- The immune system is a large network of tissues, organs, proteins, and cells.
- A properly functioning immune system can discriminate between healthy tissue and foreign things. If it identifies an unwelcome material, it will launch a complicated attack to defend the body from intruders. In addition, it identifies and eliminates damaged and dead cells.
- However, the immune system is not always trustworthy. For instance, a person’s inability to fight effectively may be from a medical condition or the use of pharmaceuticals that alter the way the body functions.
- In autoimmune illnesses and allergies, the immune system incorrectly identifies healthy tissue and launches an unwarranted attack, resulting in painful and life-threatening symptoms.
Overview of Immune System
- The immune system works as a law enforcement agency. It patrols the entire region and notifies for help whenever it detects a problem.
- This distinguishes it from other systems since it must be able to respond in any part of the body. The immune system offers two layers of protection: innate immunity and adaptive immunity.
- In general, pathogen exposure boosts the immune system. By the time they reach maturity, the majority of people will have been exposed to multiple infections and their immune systems will have been reinforced.
- When the body produces an antibody, it retains a duplicate so it can react more swiftly the next time the same antigen is encountered.
- The immune system consists of two primary components:
- The innate immune system: This immune system is intrinsic to each individual.
- The adaptive immune system: This immunity develops in response to exposure to bacteria or their byproducts.
Innate Immune System
- People are born with some immunity, allowing them to fend off invaders promptly.
- Our innate immunity includes the external barriers of our body that act as the initial line of defence against pathogens, such as the skin, gut, and throat mucous membranes.
- This response is broad and lacks specificity.
- Macrophages will engage infections if they are able to elude the innate immune system. In addition, macrophage-produced cytokines aid the body’s response to inflammation.
Adaptive (Acquired) Immune System
- Over time, the capacity to protect against infections improves.
- As a result of immunizations and disease exposure, the body creates a variety of antibodies against diverse infections. Doctors use the term immunological memory to describe this phenomenon in which the immune system recalls previous foes.
a. Active Immunity
- Active immunity is the quick response of the body to a foreign antigen. In the acquired or adaptive immune system, the body keeps note of infections it has already encountered. This is a direct result of a functioning immune system.
- When we encounter a pathogen or its antigen, we build active immunity. When a pathogen first enters the body, antibodies that oppose it are stored in case the pathogen re-enters. This is known as active natural immunity.
b. Passive Immunity
- Antibodies obtained from the outside of the body induce a form of immunity known as passive immunity. The initial response of the body to an illness is typically somewhat weak, so the first encounter with a disease is always somewhat taxing on the body.
- This immunity is temporary and is granted by a third party. For instance, a newborn obtains maternal antibodies through the placenta and breast milk before and after birth.
- This passive immunity safeguards infants against a variety of infections during their early years.
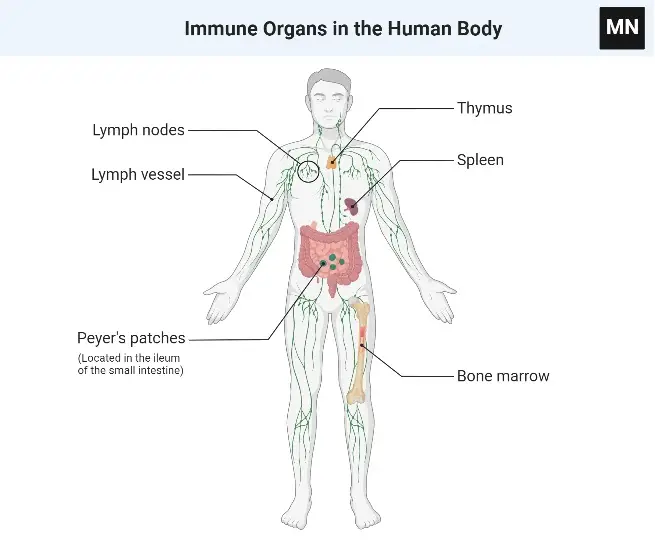
Organs of the Immune System
- Various organs and tissues with distinct morphologies and roles contribute to the development of immune responses.
- These can be categorised as major and secondary lymphoid organs based on their functions.
- The thymus and bone marrow are the primary (or central) lymphoid organs where lymphocyte maturation occurs.
- The lymph nodes, spleen, and different mucosal-associated lymphoid tissues (MALT) including gut-associated lymphoid tissue (GALT) are secondary (or peripheral) lymphoid organs that capture antigen and offer locations for mature lymphocytes to engage with that antigen.
- Additionally, during an inflammatory reaction, tertiary lymphoid tissues, which ordinarily contain fewer lymphoid cells than secondary lymphoid organs, might import lymphoid cells. The most notable of them are the lymphoid tissues linked with the skin.
- Once mature lymphocytes have been produced in the basic lymphoid organs, they circulate in the blood and lymphatic system, a network of channels that collect fluid that has escaped the capillaries of the circulatory system and return it to the blood.
Organs that function as barriers
The skin and mucous membranes are the first line of protection against pathogens entering the body from the outside. They serve as a physical barrier with the assistance of the following:
- Antibacterial chemicals can immediately eliminate microorganisms. A specific enzyme found in saliva, the airways, and tear fluid dissolves the bacterial cell wall.
- Mucus in the bronchi helps catch many of the pathogens we inhale so that hair-like structures called cilia can transport them out of the airways.
- The majority of bacteria that enter the body via the food we eat are neutralised by stomach acid.
- On our skin and in many of our mucous membranes, harmless microorganisms play a role in our immune system.
In addition, the coughing and sneezing reflexes assist clear our airways of pathogens.
Types of lymphatic system
The lymphatic system comprises the following:
- Primary lymphoid organs: The bone marrow and the thymus are examples of primary lymphoid organs. They produce immune system cells known as lymphocytes.
- Secondary lymphoid organs: Secondary lymphoid organs include the lymph nodes, spleen, tonsils, and specific tissue in the body’s numerous mucous membrane layers (for instance in the bowel). In these organs, immune system cells perform their primary function of combating pathogens and foreign substances.
A. Central (Primary) Lymphoid Organs
- The primary sites for lymphopoiesis are the central or primary lymphoid organs.
- These organs possess the capacity to generate lymphocytic progenitor cells.
- In these organs, precursor lymphocytes proliferate, mature, and differentiate from lymphoid stem cells into immunologically competent cells.
- Thymus and bone marrow comprise the principal lymphoid organs.
- T cells mature in the thymus of mammals, while B cells do so in the foetal liver and bone marrow.
- After obtaining immunological competence, lymphocytes move to secondary lymphoid organs in order to stimulate an appropriate immune response upon antigen exposure.
- In the primary lymphoid organs, immature lymphocytes created during hematopoiesis mature and commit to a particular antigenic specificity.
- Only after maturation within a main lymphoid organ is a lymphocyte immunocompetent (capable of mounting an immune response).
- T cells originate in the thymus, but in many mammals, including humans and mice, B cells originate in bone marrow.
1. Thymus
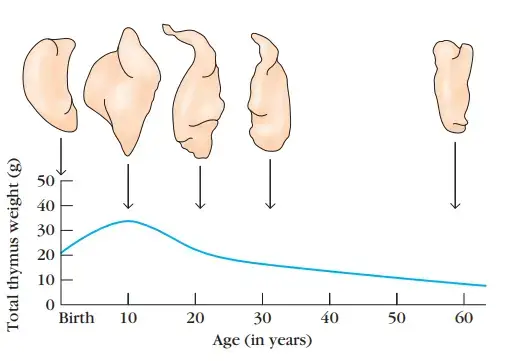
- The thymus develops first among lymphoid organs.
- It achieves its maximum size at puberty and then atrophies, with a marked drop in cortical and medullary cells and an increase in the organ’s total fat content.
- More than 95% of all thymocytes die in the thymus by apoptosis before reaching maturity.
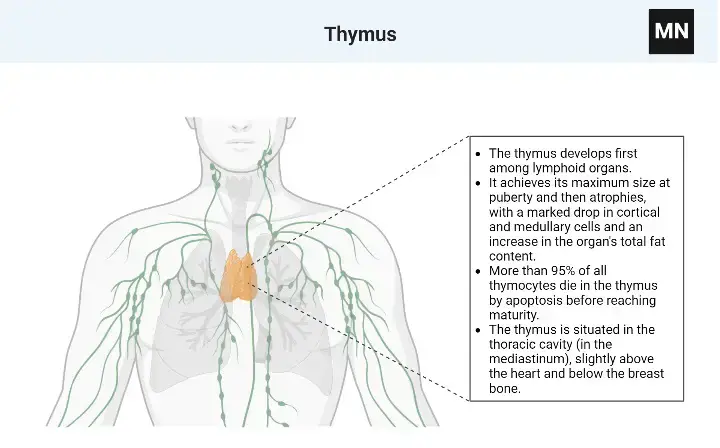
Locations
- The thymus is situated in the thoracic cavity (in the mediastinum), slightly above the heart and below the breast bone.
Origin
- The thymus is derived from the endoderm of the third and fourth pharyngeal pouches in animals.
Structure
- The thymus is a bilobed, flat organ.
- Each lobe is enclosed by a capsule and subdivided into lobules that are separated by strands of connective tissue known as trabeculae.
- Each lobule is divided into two sections: the cortex and the medulla.
- The organ’s stroma contains dendritic cells, epithelial cells, and macrophages.
- Cortex: It is primarily composed of cortical thymocytes, which are immature T lymphocytes, and a limited amount of macrophages and plasma cells. In addition, the cortex has two subpopulations of epithelial cells that form a network within the cortex: epithelial nurse cells and cortical epithelial cells.
- Medulla: It comprises primarily mature T lymphocytes and has a higher ratio of epithelial cells to lymphocytes than the cortex. Hassall’s corpuscles are concentric rings of squamous epithelial cells found solely in the medulla.
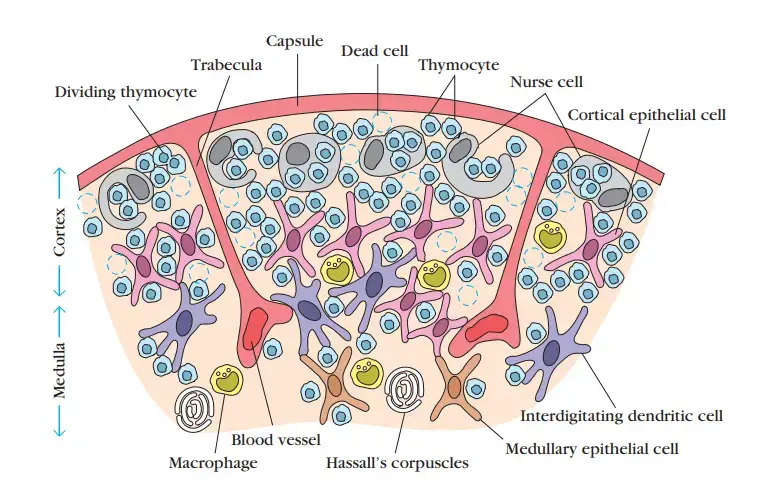
Cell types of thymus
- The thymus has four fundamental cell types: thymocytes, dendritic cells, epithelial cells, and macrophages.
- Both the cortex and medulla of the thymus are interconnected by a three-dimensional network of stromal cells.
Functions
The thymus is the only primary lymphoid organ in animals that is distinctly differentiated. It serves numerous purposes:
- Thymus is the place where a wide variety of T lymphocytes are generated, allowing them to detect and respond to a vast array of antigen–MHCs (major histocompatibility complexes).
- The thymus causes the death of T cells that are incapable of recognising antigen–MHCs.
- It also stimulates the death of T cells that react with self-antigen MHC and offer a risk for autoimmunity.
- The fundamental function of the thymus is the production of thymic lymphocytes. It is an important organ for the proliferation of lymphocytes.
- It is considered to have a crucial function in determining T lymphocyte differentiation. During maturation, lymphocytes acquire new surface antigens (Thy antigens) and are referred to as T lymphocytes or T cells (thymus dependent). During their stay in the organ, the thymus imparts immunocompetence to these cells. Unlike peripheral lymphoid organs, lymphocyte growth in the thymus is independent of antigenic stimulation.
- T cells are the primary mediators of cell-mediated immunity (CMI). The loss of thymus in neonatally thymectomized mice is related with widespread CMI deficit, causing in lymphopenia, ineffective graft rejection, and running illness. Congenital aplasia of the thymus in men with Di-George syndrome is another instance of CMI insufficiency due to thymus absence.
2. Bone marrow
- In humans and mice, B-cells originate and develop in the bone marrow.
- Immature B cells proliferate and differentiate within the bone marrow after originating from lymphoid progenitors, while stromal cells within the bone marrow interact directly with the B cells and secrete numerous cytokines essential for development.
- Similarly to thymic selection during T-cell maturation, bone marrow selection removes B cells with self-reactive antibody receptors.
- In not all species does B-cell development occur in bone marrow. The principal site of B-cell maturation in birds is the bursa of Fabricius, a lymphoid organ linked with the digestive tract.
- In mammals such as primates and rodents, there is neither a bursa nor a main lymphoid organ with a single homologue.
- Early in gestation, the foetal spleen is the major lymphoid organ in cattle and sheep that hosts the maturation, proliferation, and diversification of B lymphocytes.
- Later in gestation, this function is assumed by the ileal Peyer’s patch, a patch of tissue embedded in the intestinal wall that includes a huge number (>1010) of B cells.
- Additionally, the rabbit uses gut-associated organs such as the appendix as primary lymphoid tissue for crucial steps in the proliferation and diversity of B lymphocytes.
Location
- It is present in the cavities of the majority of the body’s bones, including the skull, ribs, sternum, femur, and spine.
- In birds, there is no bone marrow, but there is a lymphoid organ named Bursa, described by Fabricius as Bursa of Fabricius, which performs the same function as bone marrow in mammals.
Structure
- Bone marrow of various bones comprises primarily of a sponge-like reticular framework interspersed with lengthy trabeculae.
- This framework is comprised of fat cells, stromal fibroblasts, and progenitors of blood cells.
Function
- Bone marrow is the place where stem cells proliferate and where pre-B cells originate and mature into immunoglobulin-producing lymphocytes.
- In the bone marrow, immature B lymphocytes multiply and develop. Stromal cells in the bone marrow interact directly with B cells and release numerous cytokines necessary for B cell growth.
- Similarly to thymic selection during T-cell maturation, bone marrow selection removes B cells with self-reactive antibody receptors.
- B cells generate B-cell receptors (BCRs) by rearranging their DNA.
- Before leaving the bone marrow, they express auxiliary molecules such as Igα and Igβ and begin to express IgM on their surfaces.
- After maturation, B lymphocytes gain C3 and Fc receptors on their surfaces.
- B lymphocytes display IgM alone or in conjunction with IgG or IgA on their surfaces, depending on the immunoglobulin class they produce.
- The B lymphocytes become plasma cells and release antibodies. Primarily responsible for antibody-mediated immunity are B lymphocytes.
Bursa of Fabricius
Origin
- The Bursa is a lymphoepithelial organ that exclusively exists in birds as an intestinal pouch.
Location
- It is placed immediately above the cloaca and opens straight into the cloaca.
Structure
- It is a sac-like structure (about 1 cm in diameter) that contains a duct. It is bordered with epithelial cells that cover the outer cortical and inner medullary regions.
- Approximately one to two weeks after the chick’s hatching, the Bursa reaches its maximum size and then gradually atrophyes.
- Inside, folds of epithelium extend into the lumen, and lymphoid cell follicles are dispersed throughout the folds.
- Each follicle consists of a cortex and a medulla. Lymphocytes, plasma cells, and macrophages can be found in the cortex.
- At the boundary between these regions, known as the cortico-medullary juncture, a basement membrane and capillary network are present.
- Within which epithelial cells are located. Each follicle is directly attached to the epithelium that covers the fold’s surface.
Function
- The Bursa of birds serves as the microenvironment for hemopoietic induction of progenitor B-cells.
- It serves as a maturation and differentiation location for the antibody-forming system’s lymphocytes.
- They are known as B-lymphocytes or B-cells. From the Bursa, several hormones have been isolated. The most significant is bursin, a tripeptide (lys-his-glycylamide). Bursin only stimulates B-cells and not T-cells.
B. Peripheral (Secondary) Lymphoid Organs
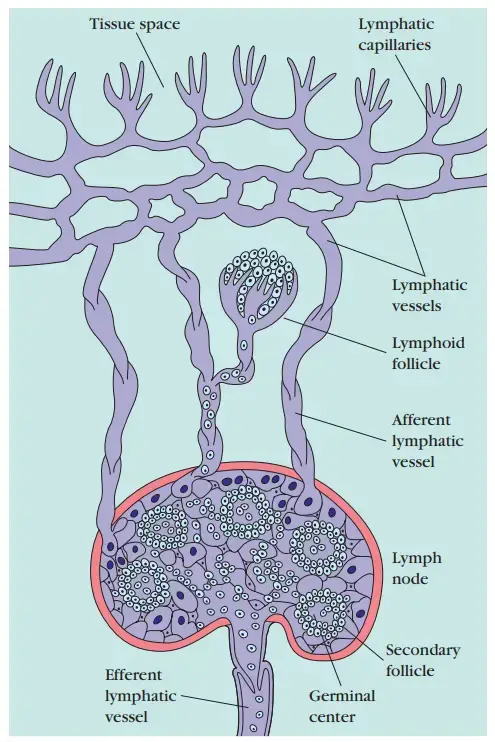
- Various forms of organised lymphoid tissues are found along the lymphatic system’s channels. Some lung lymphoid tissue and lamina propria of the intestinal wall are composed of diffuse lymphocyte and macrophage aggregates.
- Other lymphoid tissue is arranged into formations known as lymphoid follicles, which are composed of lymphoid and nonlymphoid cell aggregates surrounded by a network of lymphatic capillaries.
- A primary lymphoid follicle consists of a network of follicular dendritic cells and tiny resting B lymphocytes until it is activated by antigen.
- After an antigenic challenge, a primary follicle transforms into a larger secondary follicle, which consists of a ring of concentrically packed B lymphocytes surrounding a centre (the germinal centre) that contains a focus of proliferating B lymphocytes, a region of nondividing B cells, and some helper T cells interspersed with macrophages and follicular dendritic cells.
- In lymphoid follicles, the majority of antigen-activated B cells divide and develop into antibody-producing plasma cells, whereas few antigen-activated B cells enter germinal centres.
- Those that do endure one or more rounds of cell division, during which their antibody-encoding genes alter at an exceptionally rapid rate.
- After a period of division and mutation, there is a severe selection process in which more than 90 percent of these B cells are eliminated by apoptosis.
- In general, B cells that produce antibodies that bind antigen more firmly have a far greater probability of survival than their weaker counterparts. Emerge as plasma cells or memory cells are the few B cells that survive the germinal center’s stringent selection procedure.
- Lymph nodes and the spleen are the most organised secondary lymphoid organs; they contain lymphoid follicles as well as additional discrete zones of Tcell and B-cell activity, and are surrounded by a fibrous capsule.
- Mucosal-associated lymphoid tissue (MALT) refers to lymphoid tissue that is less structured and is present in numerous bodily regions.
- MALT consists of Peyer’s patches (in the small intestine), tonsils, and the appendix, as well as many lymphoid follicles in the lamina propria of the intestines and in the mucous membranes lining the upper airways, bronchi, and genital tract.
Peripheral or secondary lymphoid organs include lymph nodes, spleen, and nonencapsulated structures, such as mucosa-associated lymphoid tissues (MALT). These organs are the places where mature lymphocytes interact with antigens.
1. Lymph Nodes
- Lymph nodes are incredibly numerous and widely dispersed throughout the body.
- In the beginning or inductive stages of the immune response, they play a significant and dynamic role.
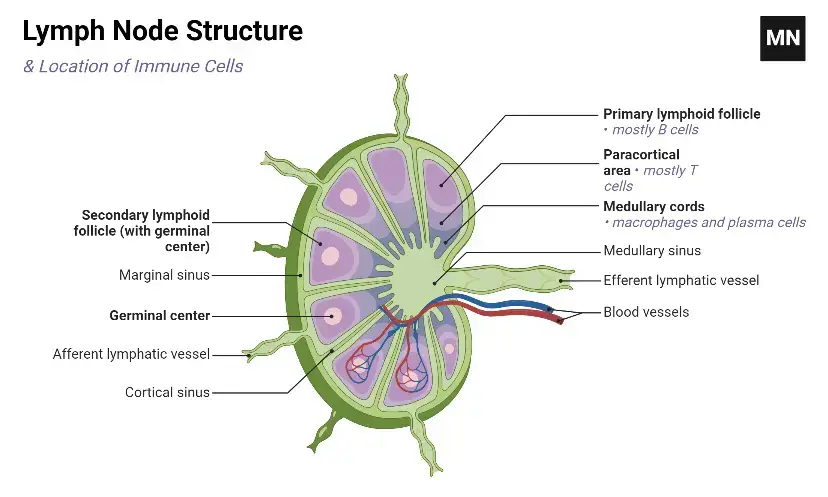
Structure of Lymph Nodes
- Lymph nodes range from 1 to 25 mm in diameter and are enclosed by a capsule of connective tissue.
- The lymph node consists of two major components: the cortex and the medulla.
- The lymph node’s reticulum or framework consists of phagocytes and specialised forms of reticular or dendritic cells.
Cortex:
- Lymphocytes occupy the brain and the deep cortex, also known as the paracortical region.
- The cortex contains roughly spherical nodules or primary lymphoid follicles containing tightly packed lymphocytes. B and T lymphocytes reside in distinct regions of the cortex.
- Primary lymphoid follicles include predominantly B lymphocytes. In addition, they include macrophages, dendritic cells, and T lymphocytes.
- The primary follicles are highly populated with tiny lymphocytes that do not participate in an immune response.
- The larger, less dense follicles, referred to as secondary follicles, are located in the cortex of a lymph node draining an infected region.
- The secondary follicles include distinct germinal centres where antigen-stimulated B cells actively divide.
- T cells are mostly present in the deep brain or paracortical region; as a result, the paracortical region is referred to as T-dependent.
- Also present in this region are interdigitating cells, which present antigen to T lymphocytes.
Medulla
- It has a lower population density and is formed primarily of medullary cords.
- These cords are extended bands of lymphocytes, plasma cells, and macrophages with branching extensions.
- They drain into the hilar lymphatic efferent arteries. Additionally, plasma cells are seen in the medullary cords.
- Following the phase of division, there is a rigorous process of selection in which more than 90 percent of these B cells die by apoptosis or cell death.
- As lymph transports antigen to a regional lymph node, interdigitating dendritic cells in the paracortex capture, process, and present it with class II MHC molecules, resulting in the activation of TH cells.
- It is also believed that the initial activation of B cells occurs in the T-cell-rich paracortex.
- Once activated, TH and B cells create tiny foci composed primarily of growing B cells near the paracortical margins.
- Certain B cells within the foci undergo differentiation into plasma cells that secrete IgM and IgG.
Functions of the lymph nodes
Lymph nodes serve the following functions:
- The lymph, fluid, and cellular components of the lymphocytic circulatory system are filtered by these cells.
- In addition, they facilitate the mixing of lymphocytes, monocytes, and dendritic cells for the start of immunological responses. In lymphoid follicles, the majority of antigen-activated B cells divide and develop into antibody-producing plasma cells, whereas few antigen-activated B cells enter germinal centres. Those that do experience one or more rounds of cell division during which their antibody-encoding genes alter at an atypically rapid rate.
- They ingest pathogenic microorganisms and other foreign material.
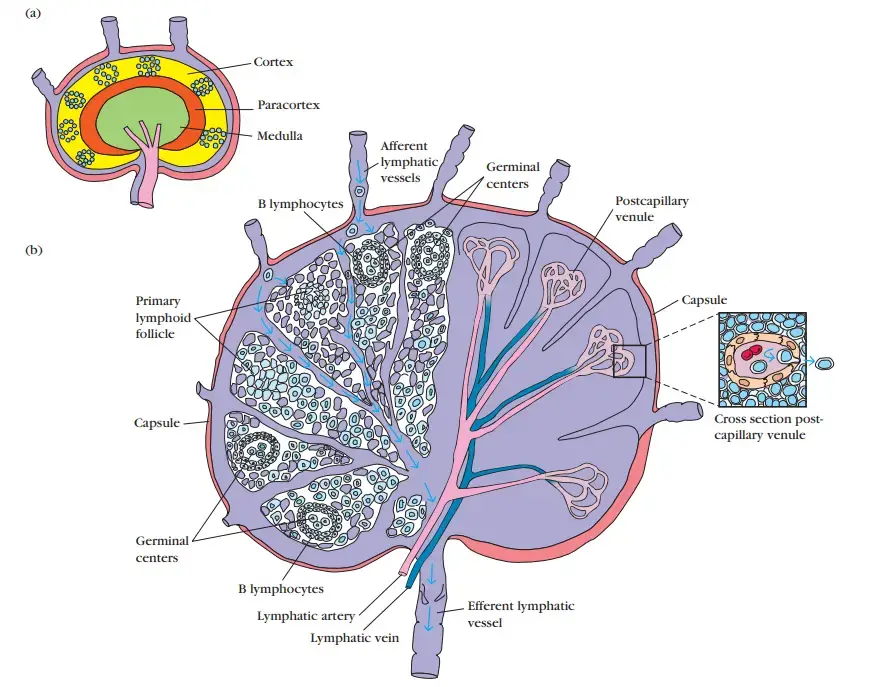
2. Spleen
- The spleen serves a crucial function in mounting immunological responses to bloodstream antigens.
- It is a big, ovoid, secondary lymphoid organ found in the upper left abdominal cavity. The spleen is specialised in filtering blood and trapping blood-borne antigens; hence, it can respond to systemic illnesses.
- The spleen is not nourished by lymphatic vessels, unlike lymph nodes. Instead, the splenic artery transports antigens and lymphocytes from the blood into the spleen.
- Experiments with radioactively labelled lymphocytes indicate that more lymphocytes recirculate through the spleen daily than through all lymph nodes combined.
Location
- Located in the upper left abdominal cavity
Structure
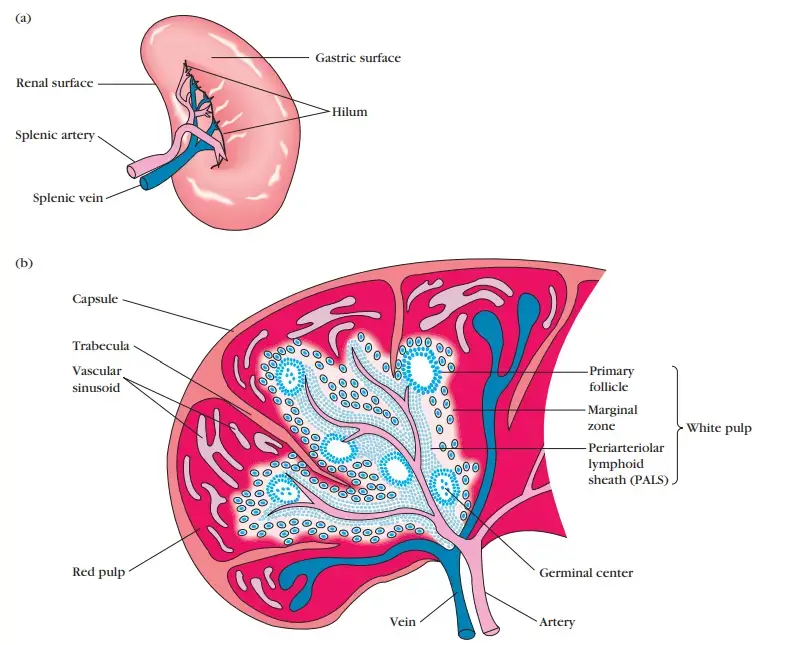
- The spleen is encircled by a capsule that forms a segmented structure by extending a number of extensions (trabeculae) into its interior.
- There are two sorts of compartments, red pulp and white pulp, separated by a diffuse border zone.
- The red pulp of the spleen consists of a network of sinusoids filled by macrophages, abundant red blood cells (erythrocytes), and few lymphocytes; it is the location where old and faulty red blood cells are destroyed and eliminated.
- Numerous macrophages within the red pulp hold ingested red blood cells or iron pigments from haemoglobin degradation.
- The white pulp of the spleen encircles the branches of the splenic artery, generating a periarteriolar lymphoid sheath (PALS) that is predominantly composed of T cells.
- The PALS are connected to lymphoid primary follicles. Some of these follicles have germinal centres and contain an abundance of B lymphocytes.
- Lymphocytes and macrophages occupy the marginal zone, which is found peripheral to the PALS.
Functions of the spleen
- Increasing immunological responses to bloodstream antigens. Antigens in circulation are captured by macrophages in the marginal zone. After processing the antigen, these macrophages travel deeper into the white pulp and activate the immune response by connecting with T and B cells.
- Filtration or removal of pathogenic organisms, old or abnormally formed components (e.g., spherocytes, ovalocytes), and particles from the peripheral circulation. Moreover, the spleen captures blood-borne antigens and microorganisms. The macrophages that line the splenic cords are responsible for the majority of filtration.
Role of Spleen in Immune system
- Antigens and lymphocytes carried in the blood enter the spleen via the splenic artery, which empties into the marginal zone.
- Antigen is captured in the marginal zone by interdigitating dendritic cells, which transport it to the PALS.
- In addition to entering sinuses in the marginal zone, blood lymphocytes move to the PALS.
- The initial activation of B and T cells occurs in the PALS, which is abundant in T cells. In this instance, interdigitating dendritic cells collect antigen and transmit it to TH cells together with class II MHC molecules.
- After activation, these TH cells are capable of activating B cells. The activated B cells, along with some TH cells, travel to the marginal zone’s primary follicles.
- Upon antigenic stimulation, these primary follicles transform into secondary follicles with germinal centres (similar to those found in lymph nodes), where rapidly dividing B cells (centroblasts) and plasma cells are surrounded by dense clusters of concentrically arranged lymphocytes.
- Depending on the age at which the spleen is removed, the consequences of splenectomy on the immunological response vary.
- In children, splenectomy frequently results in an increase in the incidence of bacterial sepsis, primarily caused by Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae.
- Adult splenectomy has fewer side effects, however it does raise the risk of blood-borne bacterial infections (bacteremia).
3. Mucosal-Associated Lymphoid Tissue
- The mucous membranes lining the digestive, respiratory, and urogenital systems have a total surface area of around 400 m2 (almost the size of a basketball court) and are the primary entrance points for the majority of infections.
- These sensitive membrane surfaces are protected by the previously stated collection of organised lymphoid tissues known together as mucosal-associated lymphoid tissue (MALT).
- These tissues range from loose, poorly organised lymphoid cell clusters in the lamina propria of intestinal villi to well-organized structures such as the tonsils, appendix, and Peyer’s patches, which are located in the submucosal layer of the intestinal lining.
- MALT’s massive population of antibody-producing plasma cells, whose number considerably exceeds that of plasma cells in the spleen, lymph nodes, and bone marrow combined, attests to its functional significance in the body’s immune system.
- There are three places for the tonsils: lingual at the base of the tongue, palatine at the sides of the rear of the mouth, and pharyngeal (adenoids) at the roof of the nasopharynx.
![Organs of Immune System – Lymphoid Organs 8 Three types of tonsils Three types of tonsils. (a) The position and internal features of the palatine and lingual tonsils; (b) a view of the position of the nasopharyngeal tonsils (adenoids). [Part b adapted from J. Klein, 1982, Immunology, The Science of Self-Nonself Discrimination, © 1982 by John Wiley and Sons, Inc.]](https://biologynotesonline.com/wp-content/uploads/2024/04/image-1484.png)
- All three tonsil groups are nodular formations composed of reticular cells, fibres, lymphocytes, macrophages, granulocytes, and mast cells.
- The B cells are arranged into follicles and germinal centres, which are bordered by T-cell-active areas.
- Antigens entering via the nasal and oral epithelial pathways are defended against by the tonsils.
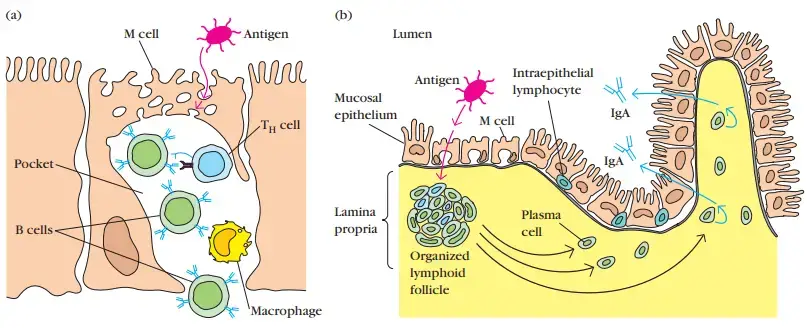
- The mucous membrane lining the digestive tract has been the subject of extensive research. As with the respiratory and urogenital tracts, this tissue has the ability to endocytose antigen from the lumen.
- Antibodies can be produced and exported to the lumen to battle invading infections.
- In numerous locations of this tissue, lymphoid cells can be detected. The mucosal epithe lial layer’s outermost layer contains intraepithelial lymphocytes (IELs).
- Numerous of these lymphocytes are T cells with uncommon antigen-binding receptors (T-cell receptors, or TCRs), which demonstrate low antigen variety. Despite the fact that this population of T cells is well-positioned to encounter antigens that enter through the intestinal mucous epithelium, their true function is poorly unclear.
- Under the epithelial layer, the lamina propria contains many B cells, plasma cells, activated TH cells, and macrophages in loose clusters.
- In the intestinal lamina propria of a healthy infant, histological sections have revealed more than 15,000 lymphoid follicles.
- Peyer’s patches, nodules of 30–40 lymphoid follicles, are located in the submucosal layer under the lamina propria.
- Peyer’s patches lymphoid follicles, like lymphoid follicles at other places, can grow into secondary follicles with germinal centres.
- By conveying small samples of foreign antigen from the lumina of the respiratory, digestive, and urogenital tracts to the underlying mucosal-associated lymphoid tissue, the epithelial cells of mucous membranes play an important role in stimulating the immune response.
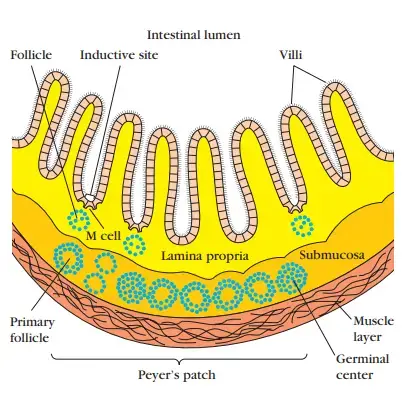
- This transport of antigen is performed by specialised M cells.
- These flattened epithelial cells lack the microvilli that are characteristic of the remainder of the mucous epithelium.
- Moreover, M cells have a deep invagination or pocket in the basolateral plasma membrane; this pocket contains a cluster of B cells, T cells, and macrophages.
- Antigens on the luminal membrane are endocytosed into vesicles that are transferred to the underlying pocket membrane.
- The vesicles subsequently fuse with the membrane of the pocket, delivering the possibly response-activating antigens to the lymphocyte clusters within the pocket.
- M cells reside in so-called inductive sites, which are tiny patches of a mucous membrane that lie over lymphoid follicles.
- Within these lymphoid follicles, antigens delivered across the mucosal membrane by M cells can activate B cells.
- The activated B cells develop into plasma cells, which exit the follicles and produce IgA-class antibodies.
- The antibodies are subsequently carried across the epithelial cells and discharged into the lumen as secretory IgA, where they can interact with antigens.
- Mucous membranes are an effective barrier against the entrance of the majority of infections, contributing to nonspecific immunity.
- This is due, in part, to the mucosal epithelial cells’ tight connections, which make pathogen penetration difficult.
- Some enteric pathogens, including bacteria and viruses, have utilised the M cell as an entry point via the mucous-membrane barrier, which is quite interesting.
- In some instances, the M cell internalises the pathogen and transports it to the pocket.
- In other instances, the pathogen binds to the M cell and destroys it, so permitting its access. Several invasive Salmonella species, Vibrio cholerae, and the polio virus are among the pathogens that exploit M cells in this manner.
Function
- MALTs serve a crucial part in the host’s defensive system. This is evidenced by the fact that the number of antibody-producing plasma cells in MALT vastly exceeds the number of plasma cells in the spleen, lymph nodes, and bone marrow combined. MALTs, in addition to the spleen and lymph nodes, promote contact between circulating leukocytes.
Cutaneous-Associated Lymphoid Tissue
- The skin is a significant anatomical barrier against the external environment, and its high surface area makes it a key component of nonspecific (innate) defences.
- The epidermal (outer) layer of skin is primarily formed of keratinocytes, which are specialised epithelial cells.
- These cells secrete a variety of cytokines that may trigger a local inflammatory response.
- In addition, keratinocytes may function as antigen-presenting cells if stimulated to express class II MHC molecules.
- Langerhans cells, a kind of dendritic cell, are dispersed throughout the epidermal cell matrix and absorb antigen by phagocytosis or endocytosis.
- From the epidermis, Langerhans cells migrate to regional lymph nodes, where they develop into interdigitating dendritic cells.
- These cells are strong activators of naive TH cells and display large quantities of class II MHC molecules.
- Additionally, the epidermis contains intraepidermal lymphocytes. Similar to the intraepithelial lymphocytes of MALT, the majority of these cells are CD8 T cells that express γδ T-cell receptors, which have limited antigen variety.
- Some immunologists believe that these intraepidermal T cells may have a role in fighting antigens that enter the body through the skin because they are ideally positioned to do so.
- CD4 and CD8 T lymphocytes and macrophages are dispersed throughout the dermal layer of the skin’s underside. The majority of these dermal T cells are either active T cells or memory T cells.
Gut-associated lymphoid tissue
- Gut-associated lymphoid tissue (GALT) is a component of the mucosa-associated lymphoid tissue (MALT) that functions in the immune system to protect the body from gastrointestinal invasion.
- Mucosal surface is thin and acts as a permeable barrier to the interior of the body due to its physiological function in food absorption.
- In addition, its fragility and permeability make it susceptible to infection; in fact, the great majority of infectious pathogens that invade the human body employ this pathway.
- The functional significance of GALT in the body’s immune system is dependent on its high population of plasma cells, which are antibody-producing cells and whose quantity exceeds that of the spleen, lymph nodes, and bone marrow combined.
- GALT constitutes approximately 70% of the immune system by weight; GALT dysfunction may have a major impact on the overall immune system’s strength.
Structure
- The lymphoid tissue associated with the gastrointestinal tract is distributed throughout the intestine, covering an area of 260–300 m2.
- The intestinal mucosa is composed of finger-like projections (villi) coated by a monolayer of epithelial cells, which separates the GALT from the lumen intestine and its contents.
- On their luminal surface, these epithelial cells have a coating of glycocalyx to protect them from the acidic pH.
- Constant production of new epithelial cells derived from stem cells at the base of the intestinal glands regenerates the epithelium (epithelial cell turnover time is less than one week).
- Although typical enterocytes are the predominant cell type in these crypts, Paneth cells are also present.
- These are found at the bottom of the crypts and emit a variety of antibacterial chemicals, including lysozyme; they are believed to have a role in the control of infections.
- Lamina propria is an underlying layer of loose connective tissue that lies beneath them. Additionally, there is lymphatic circulation in the connective tissue of the mesenteric lymph nodes.
- Due to the presence of immune cells through the epithelial cells and lamina propria, both GALT and mesenteric lymph nodes are places where the immune response is initiated.
- Human Peyer’s patches, isolated lymphoid follicles distributed throughout the intestine, and the appendix are also included in the GALT.
Peyer’s patches
- Peyer’s patch is a collection of lymphoid cells protruding into the lumen of the gut that plays a crucial role in the initiation of the immune response.
- It produces a subepithelial dome in which a significant number of B cell follicles with their germinal centres, T cell regions in a smaller number, and dendritic cells are located.
- In this region, the subepithelial dome and intestinal lumen are separated by a layer of follicle-associated epithelium.
- This contains ordinary intestinal epithelial cells and a limited number of microfold cells (M cells), which are specialised epithelial cells.
- These M cells, unlike enterocytes, have a folded luminal surface instead of microvilli, do not emit digestive enzymes or mucus, and lack a thick surface of glycocalix, allowing them to come into contact with microbiota and antigens found in the content of the gut.
Lymphatic System
- As blood flows under pressure, its fluid component (plasma) infiltrates the surrounding tissue through the capillary walls.
- A significant portion of this fluid, known as interstitial fluid, returns to the blood via the capillary membranes.
- The remainder of the interstitial fluid, now known as lymph, moves from the spaces in connective tissue into a network of lymphatic capillaries and ultimately into a number of lymphatic vessels.
- Near the heart, the main lymphatic channel, the thoracic duct, discharges into the left subclavian vein.
- In this manner, the lymphatic system recovers fluid lost from the blood and returns it to the blood, so maintaining constant fluid levels within the circulatory system.
- The lymph is not pumped through the lymphatic system by the heart; rather, muscular contractions constrict the lymph arteries to facilitate lymph passage.
- Along the lymphatic veins, a system of one-way valves guarantees that lymph flows in just one direction.
- When a foreign antigen enters the body’s tissues, it is captured by the lymphatic system (which drains all body tissues) and sent to various lymphoid tissues, such as lymph nodes, which trap the antigen.
- As lymph moves from tissues to lymphatic channels, it becomes increasingly lymphocyte-rich.
- Thus, the lymphatic system transports lymphocytes and antigen from connective tissues to organised lymphoid tissues, where the lymphocytes can interact with the trapped antigen and become activated.
References
- InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. What are the organs of the immune system? [Updated 2020 Jul 30]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279395/
- Rebelatto, M. C. (2018). Spleen, Lymph Nodes, and Thymus. Boorman’s Pathology of the Rat, 469–491. doi:10.1016/b978-0-12-391448-4.00024-1
- DELVES, P. J. (2006). Structural and Functional Aspects of the Innate and Adaptive Systems of Immunity. The Autoimmune Diseases, 11–23. doi:10.1016/b978-012595961-2/50005-6
- Biggs, J. R., & Zhang, D.-E. (2020). Molecular basis of lymphoid and myeloid diseases. Essential Concepts in Molecular Pathology, 247–269. doi:10.1016/b978-0-12-813257-9.00016-4
- https://www.sscollegejehanabad.org/study-material/1059810639Cells%20and%20organs%20of%20the%20immune%20system.pdf
- https://my.clevelandclinic.org/health/articles/21196-immune-system
- https://www.biologydiscussion.com/immunology/immune-system/organs-in-immune-system-of-humans-immunology/61727
- https://www.khanacademy.org/science/in-in-class-12-biology-india/xc09ed98f7a9e671b:in-in-human-health-and-disease/xc09ed98f7a9e671b:in-in-types-of-immunity-and-the-immune-system/a/lymphoid-organs-review
- https://www.medicine.mcgill.ca/physio/vlab/immun/backg.htm
- https://www.scientificamerican.com/article/in-autoimmune-disease-organs-may-lure-the-immune-system-into-an-attack/
- https://courses.lumenlearning.com/suny-ap2/chapter/anatomy-of-the-lymphatic-and-immune-systems/
- https://kidshealth.org/en/parents/immune.html
- https://en.wikipedia.org/wiki/Lymphatic_system
- https://www.msdmanuals.com/en-in/home/immune-disorders/biology-of-the-immune-system/overview-of-the-immune-system
- https://veteriankey.com/organs-of-the-immune-system/
- https://www.lecturio.com/concepts/primary-lymphatic-organs/
- https://www.chop.edu/centers-programs/vaccine-education-center/human-immune-system/parts-immune-system
- https://www.ndvsu.org/images/StudyMaterials/Micro/Organs-of-Immunity.pdf
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/the-immune-system