What is an inflammation?
- Inflammation, also known as the inflammatory response, is a biological reaction initiated by the immune system, particularly in vascular tissues, as a defense mechanism against harmful stimuli. These stimuli can range from microorganisms to foreign substances that pose a threat to the body. When tissues endure injury from microbes, trauma, toxins, heat, or any other cause, inflammation serves as the body’s natural protective response.
- The process of inflammation involves the migration of immune system cells to the site of injury or infection. This migration gives rise to four characteristic signs of inflammation: warmth, redness, swelling, and pain. Initially, within the first 24 hours, neutrophils are the primary inflammatory cells recruited. After 48 hours, macrophages become the predominant cell type involved in the inflammatory response.
- When a wound becomes swollen, turns red, and causes discomfort, it may indicate the presence of inflammation. In a broad sense, inflammation is the immune system’s reaction to an irritant. While this irritant could be a germ causing an infection, it could also be a foreign object like a splinter lodged in your finger.
- It’s important to note that inflammation doesn’t solely manifest when a wound has already become infected, showing signs of pus or poor healing. Instead, the inflammatory response commences as soon as the body recognizes the presence of a harmful irritant and initiates the process to combat it. Inflammation acts as a crucial defense mechanism, safeguarding the body against potential threats and aiding in the recovery process.
Definition of inflammation
Inflammation is the immune system’s response to injury or infection, characterized by redness, swelling, warmth, and pain at the affected site.
Causes of inflammation
Inflammation can be triggered by a variety of factors, each capable of initiating an inflammatory response. The following are among the most common causes:
- Pathogens: Infections caused by bacteria, viruses, or fungi can provoke an inflammatory reaction in the body. When the immune system detects these pathogens, it launches an inflammatory response to eliminate the invaders and protect the body from further harm.
- External Injuries: Physical injuries, such as cuts, scrapes, or puncture wounds resulting from foreign objects like thorns, can induce inflammation. The body’s immune system responds to these injuries by initiating an inflammatory process to facilitate healing and prevent infection.
- Effects of Chemicals or Radiation: Exposure to certain chemicals or radiation can provoke an inflammatory response in tissues or organs. The body recognizes these substances as harmful and triggers an inflammation to repair the damage and mitigate any potential harm.
- Inflammatory Diseases or Medical Conditions: Many diseases or medical conditions are associated with chronic inflammation, often identifiable by names ending in “-itis.” Examples include cystitis, which involves inflammation of the bladder, bronchitis, which affects the bronchi, otitis media, characterized by inflammation of the middle ear, and dermatitis, a condition where the skin becomes inflamed.
Types of inflammation
There are several types of inflammation that can occur in the body, each with its own characteristics and underlying causes. Here are some common types of inflammation:
- Acute Inflammation: This is the most common and immediate form of inflammation that occurs in response to an injury or infection. Acute inflammation typically develops rapidly and is characterized by symptoms such as redness, heat, swelling, pain, and loss of function. It is a short-lived response aimed at eliminating the harmful stimulus and initiating the healing process.
- Chronic Inflammation: Unlike acute inflammation, chronic inflammation persists over a longer period, often lasting for months or even years. It can result from a persistent infection, prolonged exposure to irritants or toxins, or an autoimmune response where the immune system attacks healthy tissues. Chronic inflammation can lead to tissue damage and is associated with various diseases, including rheumatoid arthritis, inflammatory bowel disease, and chronic respiratory conditions.
- Granulomatous Inflammation: Granulomatous inflammation is characterized by the formation of granulomas, which are small clusters of immune cells called macrophages. These clusters form in response to persistent or difficult-to-eliminate irritants, such as certain infections (e.g., tuberculosis) or foreign substances (e.g., certain types of dust or particles). Granulomatous inflammation is often seen in diseases like sarcoidosis and Crohn’s disease.
- Serous Inflammation: Serous inflammation is characterized by the accumulation of watery fluid in body cavities or on the surface of tissues. It can occur in response to burns, bacterial infections, or other forms of tissue injury. Serous inflammation often leads to the formation of blisters or the production of excessive fluid in body cavities, such as pleural effusion (fluid in the lungs) or ascites (fluid in the abdominal cavity).
- Suppurative (Purulent) Inflammation: Suppurative inflammation, also known as purulent inflammation, is associated with the formation of pus. Pus consists of dead white blood cells, bacteria, and tissue debris. It is typically seen in bacterial infections, such as abscesses, boils, or infected wounds. The presence of pus is a sign that the body is actively fighting off the infection.
- Allergic Inflammation: Allergic inflammation occurs in response to exposure to allergens, such as pollen, dust mites, or certain foods. In susceptible individuals, the immune system overreacts to these harmless substances, leading to the release of inflammatory mediators like histamine. Allergic inflammation can manifest as allergic rhinitis (hay fever), asthma, or allergic skin conditions like eczema or hives.
Differences between acute and chronic inflammation
| Aspect | Acute | Chronic |
|---|---|---|
| Causative agent | Bacterial pathogens, injured tissues | Persistent acute inflammation due to non-degradable pathogens, viral infection, persistent foreign bodies, or autoimmune reactions |
| Major cells involved | Neutrophils (primarily), basophils (inflammatory response), and eosinophils (response to helminth worms and parasites), mononuclear cells (monocytes, macrophages) | Mononuclear cells (monocytes, macrophages, lymphocytes, plasma cells), fibroblasts |
| Primary mediators | Vasoactive amines, eicosanoids | IFN-γ and other cytokines, growth factors, reactive oxygen species, hydrolytic enzymes |
| Onset | Immediate | Delayed |
| Duration | Few days | Up to many months, or years |
| Outcomes | Resolution, abscess formation, chronic inflammation | Tissue destruction, fibrosis, necrosis |
Acute inflammation
- Acute inflammation is an immediate and short-term response that occurs upon injury, typically lasting only a few days. It involves the activation of immune cells, such as neutrophils and macrophages, which are attracted to the site of inflammation by cytokines and chemokines. Pathogens, allergens, toxins, burns, and frostbite are common causes of acute inflammation. Toll-like receptors (TLRs) play a role in recognizing microbial pathogens.
- Acute inflammation serves as a defensive mechanism to protect tissues from further injury. It is characterized by five cardinal signs: redness (rubor), swelling (tumor), heat (calor), pain (dolor), and loss of function (functio laesa). These signs reflect the body’s response to the inflammatory process. Redness and heat result from increased blood flow to the inflamed area, while swelling is caused by fluid accumulation. Pain is triggered by the release of chemicals that stimulate nerve endings.
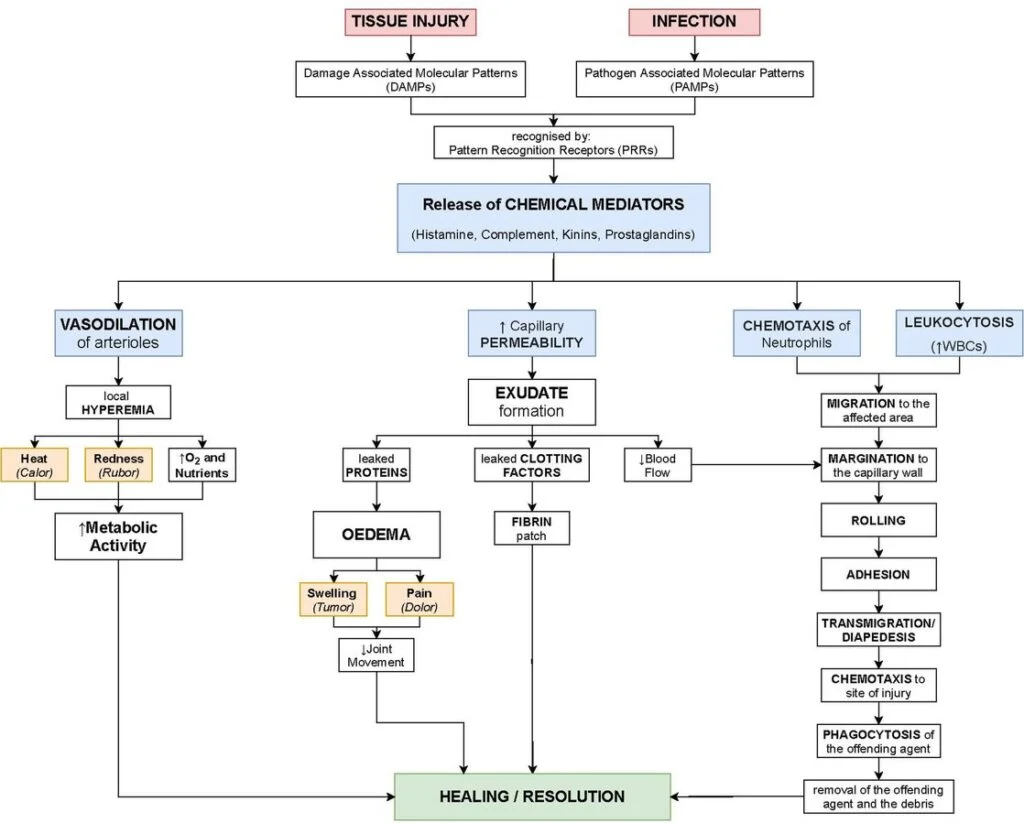
- The process of acute inflammation is initiated by resident immune cells already present in the affected tissue, such as macrophages and mast cells. These cells possess pattern recognition receptors (PRRs) that recognize pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs). Upon activation, these cells release inflammatory mediators that lead to the clinical signs of inflammation.
- Vasodilation and increased blood flow contribute to redness and heat, while increased vessel permeability leads to the leakage of plasma proteins and fluid into the tissue, resulting in swelling. Inflammatory mediators also increase sensitivity to pain and promote the migration of leukocytes, primarily neutrophils and macrophages, from the blood vessels into the tissue.
- Acute inflammation involves both cell-derived mediators and acellular biochemical cascade systems. Cell-derived mediators, such as cytokines, are released by immune cells and play a crucial role in coordinating the inflammatory response. Biochemical cascade systems, such as the complement system and coagulation system, act in parallel to initiate and propagate inflammation.
- Acute inflammation is the body’s initial line of defense against injury. It requires continuous stimulation to be sustained, and once the triggering stimulus is removed, the inflammatory response begins to subside. The resolution of acute inflammation involves the clearance of pathogens or harmful agents and the initiation of tissue repair processes.
Process of Acute inflammation
The process of acute inflammation involves a series of coordinated events that occur in response to tissue injury or infection. Here is an overview of the steps involved:
- Recognition of the insult: The immune system recognizes the presence of harmful stimuli, such as pathogens or tissue damage, through pattern recognition receptors (PRRs) located on immune cells. These receptors detect specific molecules associated with the insult, known as pathogen-associated molecular patterns (PAMPs) or damage-associated molecular patterns (DAMPs).
- Vasodilation: Upon recognition of the insult, immune cells release chemical signals, including histamine and prostaglandins, which cause blood vessels in the affected area to widen (vasodilation). This increased blood flow leads to redness (rubor) and heat (calor) at the site of inflammation.
- Increased vascular permeability: The immune cells also promote the loosening of the junctions between endothelial cells lining the blood vessels, allowing fluid, proteins, and immune cells to leak out of the blood vessels and into the surrounding tissue. This extravasation of fluid causes swelling (tumor) at the site of inflammation.
- Migration of immune cells: Chemotactic factors released at the site of inflammation attract immune cells, especially neutrophils, from the bloodstream to the affected tissue. These immune cells migrate along the concentration gradient towards the source of the chemotactic signals, guided by cell adhesion molecules expressed on the endothelial cells lining the blood vessels.
- Phagocytosis and destruction: Once at the site of inflammation, neutrophils and other phagocytic cells engulf and destroy pathogens or damaged cells through a process called phagocytosis. They release antimicrobial substances and enzymes to break down the engulfed material.
- Release of inflammatory mediators: Immune cells, such as macrophages and mast cells, release various inflammatory mediators, including cytokines, chemokines, and prostaglandins. These mediators amplify the inflammatory response, recruit more immune cells to the site of inflammation, and promote the repair and healing processes.
- Resolution or chronic inflammation: In most cases, acute inflammation subsides once the insult is removed or neutralized. The immune system resolves the inflammation by clearing the pathogens or debris and initiating tissue repair. However, if the insult persists or the immune response is dysregulated, acute inflammation can transition into chronic inflammation, which lasts for a longer duration and can lead to tissue damage and fibrosis.
Chronic inflammation
Chronic inflammation is a persistent and prolonged inflammatory response that can last for months or even years. Unlike acute inflammation, which is characterized by the presence of neutrophils, chronic inflammation is characterized by the dominance of macrophages, lymphocytes, and plasma cells. It is associated with various diseases such as diabetes, cardiovascular disease, allergies, and chronic obstructive pulmonary disease (COPD).
Several factors contribute to the development of chronic inflammation. Lifestyle factors like obesity, smoking, chronic stress, and an inadequate diet can promote a chronic inflammatory state in the body. In fact, a study conducted in 2014 found that a significant percentage of Americans, around 60%, had at least one chronic inflammatory condition, and 42% had multiple conditions.
Chronic inflammation manifests through a range of signs and symptoms that can affect different parts of the body. Some common manifestations include:
- Body pain, arthralgia, and myalgia: Individuals with chronic inflammation may experience persistent pain in their joints and muscles, which can significantly impact their daily activities.
- Chronic fatigue and insomnia: Fatigue is a common symptom of chronic inflammation, often accompanied by sleep disturbances such as insomnia. The ongoing inflammatory response can disrupt normal sleep patterns, leading to feelings of exhaustion.
- Depression, anxiety, and mood disorders: Chronic inflammation has been linked to changes in mood and mental well-being. Individuals may experience symptoms of depression, anxiety, and other mood disorders as a result of the persistent inflammatory state.
- Gastrointestinal complications: Chronic inflammation can affect the gastrointestinal system, leading to issues such as constipation, diarrhea, and acid reflux. These gastrointestinal disturbances can cause discomfort and disrupt normal digestive functions.
- Weight gain or loss: Chronic inflammation can impact metabolism and lead to weight fluctuations. Some individuals may experience unexplained weight gain, while others may have difficulty maintaining a healthy weight.
- Increased susceptibility to infections: Chronic inflammation weakens the immune system, making individuals more susceptible to frequent infections. This compromised immune response can result in recurrent infections or difficulty recovering from infections.
Process of Chronic inflammation
The process of chronic inflammation is complex and involves a persistent and prolonged immune response in the body. Unlike acute inflammation, which is a short-term protective response to injury or infection, chronic inflammation persists over an extended period. It is characterized by the infiltration of immune cells, tissue destruction, and ongoing release of inflammatory mediators.
The process of chronic inflammation can be summarized in the following steps:
- Initial Trigger: Chronic inflammation can be triggered by various factors, including persistent infections, long-term exposure to harmful substances (such as cigarette smoke or environmental pollutants), autoimmune disorders, or repeated episodes of acute inflammation that fail to resolve completely.
- Recruitment of Immune Cells: In response to the ongoing stimulus, immune cells, particularly macrophages and lymphocytes, are continuously recruited to the site of inflammation. These cells release cytokines, chemokines, and other signaling molecules that perpetuate the inflammatory response.
- Tissue Damage and Repair: Chronic inflammation is characterized by a cycle of tissue damage and repair. The continuous presence of immune cells and inflammatory mediators can lead to collateral damage to healthy tissues, resulting in structural changes and fibrosis.
- Angiogenesis: In chronic inflammation, the formation of new blood vessels (angiogenesis) is a common feature. This process is stimulated by factors released by immune cells and is intended to supply nutrients and oxygen to the inflamed area. However, excessive angiogenesis can contribute to tissue dysfunction and perpetuate inflammation.
- Immune Cell Activation: Within the inflamed tissue, immune cells such as macrophages and lymphocytes remain activated for an extended period. These cells release a variety of pro-inflammatory substances, including cytokines, growth factors, and reactive oxygen species. These molecules further contribute to tissue damage and the recruitment of additional immune cells.
- Prolonged Inflammatory Mediator Release: In chronic inflammation, the release of inflammatory mediators persists over time. These mediators include cytokines, such as tumor necrosis factor-alpha (TNF-α), interleukins, and chemokines, which maintain the inflammatory environment and perpetuate immune cell activation.
- Fibrosis and Scar Formation: As chronic inflammation persists, the excessive deposition of extracellular matrix components, particularly collagen, may occur. This leads to fibrosis and scar formation, which can disrupt normal tissue architecture and impair organ function.
- Systemic Effects: Chronic inflammation can have systemic effects on the body. It may contribute to the development of conditions like metabolic syndrome, cardiovascular disease, neurodegenerative disorders, and certain types of cancer. The constant activation of the immune system and the release of inflammatory molecules can have widespread effects on various organs and systems.
Signs of inflammation
Numerous factors can contribute to the development of inflammation, leading to a range of symptoms. Here are some common causes of inflammation:
- Infections: Pathogens such as bacteria, viruses, or fungi can trigger an inflammatory response as the immune system works to combat the invading organisms. Inflammatory symptoms like redness, heat, swelling, pain, and loss of function may manifest.
- Injuries: External injuries, such as cuts, scrapes, or wounds caused by foreign objects, can result in inflammation. The body responds by initiating the inflammatory process to promote healing and protect against infection. The affected area may exhibit symptoms like redness, swelling, pain, and impaired function.
- Chemical or Environmental Factors: Exposure to certain chemicals, allergens, or irritants can stimulate an inflammatory reaction. For example, contact with an allergen can lead to dermatitis, characterized by skin inflammation. Similarly, exposure to irritants in the lungs can cause bronchitis, resulting in inflammation of the bronchial tubes and symptoms like difficulty breathing.
- Autoimmune Disorders: In conditions such as rheumatoid arthritis or lupus, the immune system mistakenly attacks healthy tissues, triggering chronic inflammation. This ongoing immune response can lead to symptoms such as joint pain, swelling, and loss of function.
- Chronic Conditions: Some medical conditions, such as inflammatory bowel disease or chronic sinusitis, can result in persistent inflammation. These conditions may exhibit symptoms like abdominal pain, diarrhea, sinus pressure, or nasal congestion.
General reactions in body during inflammation
In cases of severe inflammation, the body can exhibit general responses that indicate the heightened activity of the immune system. These responses may encompass the following signs and symptoms:
- Feeling Ill and Exhaustion: When inflammation becomes pronounced, individuals may experience a general sense of illness and fatigue. This is an indication that the immune system is actively engaged and requires substantial energy resources, potentially diverting energy from other bodily functions. The increased metabolic rate during fever can facilitate the production of more antibodies and immune cells.
- Blood Changes: In response to inflammation, alterations in the blood may occur. This can include an elevated number of immune system cells as the body mobilizes its defense mechanisms to combat the underlying cause of inflammation.
- Septicemia (Blood Poisoning): Although rare, septicemia is a serious and potentially life-threatening complication of an infection. Its symptoms may include chills, a profound feeling of illness, and an exceptionally high fever. Septicemia arises when bacteria rapidly multiply in a localized area of the body and subsequently enter the bloodstream in significant quantities. This can happen if the body’s ability to contain the infection locally is compromised, if the infecting microbes are highly virulent, or if the immune system is significantly weakened. Septicemia requires urgent medical attention and should be treated by a doctor without delay.
What happens when you have an inflammation
- When inflammation occurs in the body, it involves the participation of various immune system cells that release specific substances called inflammatory mediators. Among these mediators are hormones like bradykinin and histamine. These substances have significant effects on the affected tissue.
- One of the primary actions of inflammatory mediators is to cause the dilation, or widening, of the small blood vessels within the tissue. This dilation allows for an increased blood flow to reach the injured area. Consequently, the inflamed region appears red and feels hot. The enhanced blood flow also facilitates the transportation of more immune system cells to the site of injury, where they contribute to the healing process. Additionally, these hormones can irritate nerves, leading to the transmission of pain signals to the brain. This pain response serves a protective purpose, as it prompts individuals to safeguard the affected part of their body.
- Furthermore, the inflammatory mediators play an important role in enabling immune system cells to exit the small blood vessels and enter the affected tissue more easily. This increased migration of immune cells into the inflamed tissue is accompanied by a greater accumulation of fluid. Consequently, swelling often occurs in the affected area. Over time, the excess fluid is eventually transported out of the tissue, leading to a reduction in swelling.
- In the case of mucous membranes, such as those lining the nasal passages, inflammation triggers an increase in fluid production. For example, when the membranes in your nose become inflamed, causing nasal congestion, the additional fluid serves to flush viruses out of your body more efficiently.
- Understanding the processes that occur during inflammation helps shed light on the body’s intricate defense mechanisms and the ways in which it strives to heal and protect itself in the face of injury or infection.
Outcomes of inflammation
The outcome of inflammation can vary depending on the specific circumstances and the type of tissue involved. Here are the possible outcomes:
- Resolution: In cases where inflammation is limited or short-lived, the inflamed tissue can undergo complete restoration, returning to its normal state. The inflammatory processes, such as vasodilation, chemical production, and infiltration of immune cells, cease. Damaged cells regenerate, and the tissue heals without any lasting effects.
- Fibrosis: When there is significant tissue destruction or damage in tissues that are unable to regenerate fully, the body’s healing response involves the formation of fibrous scar tissue. This scar, primarily composed of collagen, replaces the damaged tissue. However, since the scar lacks specialized structures like parenchymal cells, functional impairment may occur in the affected area.
- Abscess Formation: In some cases, particularly when there is a localized infection, an abscess may form. An abscess is a cavity filled with pus, which consists of dead white blood cells, bacteria, and cellular debris from destroyed tissues. Abscesses can develop in response to severe infections or as a means for the body to contain and isolate the infection.
- Chronic Inflammation: If the injurious agent persists or if the body’s immune response is dysregulated, acute inflammation can transition to chronic inflammation. Chronic inflammation is characterized by inflammation that lasts for an extended period, ranging from days to months or even years. This prolonged inflammation can lead to the formation of chronic wounds. In chronic inflammation, macrophages play a dominant role in the injured tissue. While these immune cells are meant to defend the body, their prolonged presence and release of toxins, including reactive oxygen species, can cause damage to both the invading agents and the body’s own tissues. Consequently, chronic inflammation is often accompanied by tissue destruction and can result in long-term functional impairment.
Disorders associated with inflammation
There are several disorders associated with inflammation, encompassing a wide range of medical conditions. These disorders can affect various parts of the body and involve different mechanisms of inflammation. Here are some examples:
- Acne vulgaris: A common skin disorder characterized by inflammation of the sebaceous glands and hair follicles, leading to the formation of pimples and blemishes.
- Asthma: A chronic respiratory condition characterized by inflammation and narrowing of the airways, resulting in breathing difficulties, wheezing, and coughing.
- Autoimmune diseases: Conditions where the immune system mistakenly attacks healthy cells and tissues in the body, leading to chronic inflammation. Examples include rheumatoid arthritis, systemic lupus erythematosus, and multiple sclerosis.
- Autoinflammatory diseases: Inherited disorders characterized by recurrent episodes of systemic inflammation, often without an autoimmune component. Examples include familial Mediterranean fever and periodic fever syndromes.
- Celiac disease: An autoimmune disorder triggered by the ingestion of gluten, causing inflammation and damage to the small intestine in individuals with a genetic predisposition.
- Chronic prostatitis: Inflammation of the prostate gland, often leading to persistent pelvic pain, discomfort, and urinary symptoms.
- Colitis: Inflammation of the colon, which can be caused by various factors, including inflammatory bowel diseases like Crohn’s disease and ulcerative colitis.
- Diverticulitis: Inflammation or infection of small pouches (diverticula) that develop along the wall of the colon, leading to abdominal pain and digestive issues.
- Glomerulonephritis: Inflammation of the glomeruli, the filtering units of the kidneys, resulting in impaired kidney function and various symptoms like blood in the urine and fluid retention.
- Hidradenitis suppurativa: A chronic skin condition characterized by recurrent painful nodules and abscesses in the skin folds, often leading to scarring and chronic inflammation.
Diagnosis of inflammation
The diagnosis of inflammation typically involves a comprehensive evaluation that includes:
- Medical history: The healthcare provider will inquire about your symptoms, their duration, any triggering factors, previous medical conditions, and any relevant family history.
- Physical examination: The healthcare provider will conduct a physical examination to assess signs of inflammation such as redness, swelling, warmth, and tenderness in the affected area. They may also examine other parts of the body for systemic signs of inflammation.
- Laboratory tests: Blood tests can be conducted to measure specific markers of inflammation, such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). These markers indicate the presence and severity of inflammation in the body.
- Imaging studies: Depending on the suspected site of inflammation, imaging techniques like X-rays, ultrasound, computed tomography (CT), magnetic resonance imaging (MRI), or positron emission tomography (PET) scans may be ordered. These tests can help visualize and assess the extent of inflammation in tissues and organs.
- Biopsy: In some cases, a biopsy may be necessary to obtain a sample of the affected tissue for further examination under a microscope. This can help identify the underlying cause of inflammation, such as infections, autoimmune disorders, or cancer.
- Other specific tests: Depending on the suspected cause of inflammation, additional tests may be ordered, such as allergy testing, autoimmune antibody testing, cultures to identify infectious agents, or genetic testing for certain inherited conditions.
Treatment of inflammation
The treatment of inflammation depends on the underlying cause and severity of the condition. Here are some common approaches used in the treatment of inflammation:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs such as ibuprofen, naproxen, and aspirin are commonly used to reduce pain, inflammation, and fever. They work by inhibiting the production of certain chemicals called prostaglandins, which contribute to the inflammatory response.
- Corticosteroids: Corticosteroids, such as prednisone and dexamethasone, are powerful anti-inflammatory medications that mimic the effects of hormones naturally produced by the body. They are often prescribed for more severe or chronic inflammatory conditions to reduce swelling, redness, and immune system activity.
- Disease-Modifying Anti-Rheumatic Drugs (DMARDs): DMARDs are a class of drugs used primarily for the treatment of autoimmune diseases such as rheumatoid arthritis and psoriasis. They work by suppressing the immune system and reducing inflammation associated with these conditions. Examples of DMARDs include methotrexate, sulfasalazine, and hydroxychloroquine.
- Biologic Response Modifiers: Biologic drugs are a newer class of medications that target specific molecules involved in the inflammatory response. They are often used for autoimmune conditions such as rheumatoid arthritis, Crohn’s disease, and psoriasis. Biologics include medications like adalimumab, etanercept, and infliximab.
- Immunosuppressants: In some cases, medications that suppress the immune system may be prescribed to reduce inflammation. These medications, such as azathioprine, cyclosporine, and tacrolimus, are often used for conditions like inflammatory bowel disease or certain types of arthritis.
- Lifestyle Modifications: Making certain lifestyle changes can help manage inflammation. These may include maintaining a healthy diet rich in fruits, vegetables, and omega-3 fatty acids, regular exercise, stress management, getting enough sleep, and avoiding smoking and excessive alcohol consumption.
FAQ
What is inflammation?
Inflammation is a natural response of the body’s immune system to injury, infection, or irritation. It involves a series of biological processes aimed at removing harmful stimuli, initiating tissue repair, and restoring normal functioning.
What causes inflammation?
Inflammation can be caused by various factors, including infections (such as bacterial or viral), injuries, autoimmune reactions, exposure to toxins, chronic diseases, and lifestyle factors like smoking and poor diet.
What are the signs and symptoms of inflammation?
Common signs of inflammation include redness, swelling, heat, pain, and loss of function in the affected area. Systemic symptoms like fever, fatigue, and malaise can also occur in some cases.
Is inflammation always bad?
No, inflammation is a vital defense mechanism of the body. It helps to remove pathogens, repair damaged tissues, and promote healing. However, chronic or excessive inflammation can contribute to the development of various diseases.
What are the complications of chronic inflammation?
Prolonged inflammation can lead to tissue damage, scarring, organ dysfunction, and an increased risk of developing chronic conditions like cardiovascular disease, diabetes, autoimmune disorders, and certain cancers.
How is inflammation diagnosed?
Inflammation is diagnosed through a combination of medical history, physical examination, and laboratory tests. Blood tests measuring inflammatory markers, imaging studies, and biopsies may be used to evaluate the extent and severity of inflammation.
How is inflammation treated?
Treatment depends on the underlying cause and severity of inflammation. It may include medications like nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, immunosuppressants, lifestyle modifications (such as a healthy diet and regular exercise), and specific interventions targeted at the underlying condition.
Can diet influence inflammation?
Yes, certain foods can either promote or reduce inflammation in the body. A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats (such as omega-3 fatty acids) is generally recommended to help reduce inflammation. On the other hand, a diet high in processed foods, refined sugars, and unhealthy fats may contribute to increased inflammation.
Are there natural remedies for inflammation?
Several natural remedies and complementary therapies, such as herbal supplements, acupuncture, and mind-body techniques like meditation and yoga, are thought to have anti-inflammatory properties. However, it is important to consult with a healthcare professional before trying any natural remedies, as they may interact with medications or have adverse effects.
Can lifestyle choices affect inflammation?
Yes, lifestyle choices play a significant role in inflammation. Factors like regular exercise, stress management, adequate sleep, maintaining a healthy weight, and avoiding smoking and excessive alcohol consumption can help reduce inflammation and promote overall well-being.
References
- InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. What is an inflammation? 2010 Nov 23 [Updated 2018 Feb 22]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279298/
- Parija S.C.(2012). Textbook of Microbiology & Immunology.(2 ed.). India: Elsevier India.
- Lydyard, P.M., Whelan,A.,& Fanger,M.W. (2005).Immunology (2 ed.).London: BIOS Scientific Publishers.
- Sastry A.S. & Bhat S.K. (2016). Essentials of Medical Microbiology. New Delhi : Jaypee Brothers Medical Publishers.
- https://dundeemedstudentnotes.wordpress.com/2015/11/15/acute-inflammation/
- http://www.simplynotes.in/medical/inflammation-definition-causes-types/