| Domain: | Bacteria |
| Phylum: | Actinomycetota |
| Class: | Actinomycetia |
| Order: | Mycobacteriales |
| Family: | Corynebacteriaceae |
| Genus: | Corynebacterium |
| Species: | C. diphtheriae |
- Diphtheroids, also known as Corynebacterium species, are a group of bacteria related to the diphtheria-causing bacterium, Corynebacterium diphtheriae. In contrast to C. diphtheriae, however, diphtheroids are typically nonpathogenic or have a low pathogenic potential.
- Diphtheroids are gram-positive bacteria commonly found on the epidermis, mucous membranes, and other body surfaces as part of the normal microbial flora. They are also present in the soil and water of the environment. Diphtheroids have a rod- or club-like appearance and can form irregular clusters or arrangements.
- Infrequently, diphtheroids can cause opportunistic infections, despite the fact that they are generally regarded as innocuous microorganisms. Individuals with compromised immune systems or those who have endured invasive medical procedures are more susceptible to these infections. Infections such as wound infections, urinary tract infections, bloodstream infections, and endocarditis have been linked to diphtheroids.
- When diphtheroids cause infections, treatment may be required, and susceptible bacteria-specific antibiotics are prescribed. However, diphtheroids are typically not cause for concern and do not necessitate special treatment.
- Importantly, if you have specific concerns or symptoms related to diphtheroids, you should consult a healthcare professional for an accurate diagnosis and appropriate treatment.
What is Diphtheroids? (Corynebacterium diphtheriae)
- Due to the characteristics of pseudomembrane generated by the organism itself at the site of colonization, the term “diphtheria” is derived from the Greek word “diphtheria” which means “hide or leather.”
- It is a potentially fatal infection of the upper respiratory tract that is vaccine-preventable. The disease may manifest as an asymptomatic carrier, a cutaneous infection, or as pharyngitis manifested by aching throat, fever, malaise, and cervical lymphadenopathy.
- Corynebacterium diphtheria is typically club-shaped, anaerobic, Gram-positive, non-motile, non-spore-forming, non-capsulated, toxin-producing coccobacillus.
- It has four biotypes based on biochemical properties and colony morphology: gravis, mitis, intermedius, and belfanti. C. mitis causes moderate disease, C. intermedius causes intermediate disease, and C. gravis causes severe disease.
- Infection susceptibility and transmission are influenced by substandard living conditions, low socioeconomic status, immunocompromised states, and insufficient immunization.
- The disease is distinguished by the formation of a pseudomembrane at the site of colonization. The most prevalent sites of involvement are the anterior tonsillar pillars and posterior pharyngeal walls.
- Prior to the introduction of universal vaccination in the 1940s and 1950s, measles was the leading cause of disease and mortality among children and adolescents.
- However, since the introduction of universal immunization, the incidence of the disease has been drastically reduced to approximately 5,000 cases per year globally.
- Frequent sporadic outbreaks of the disease have been caused by various factors, including low socioeconomic status, inadequate income, inaccessibility to public health, conflict and displacement, and ineffective monitoring of the immunization schedule. The purpose of this section is to provide a refresher on Corynebacterium diphtheria.
Characteristics of Diphtheroids/Corynebacterium diphtheriae
The infectious disease known as diphtheria is caused by the bacterium Corynebacterium diphtheriae. Key characteristics of Corynebacterium diphtheriae are as follows:
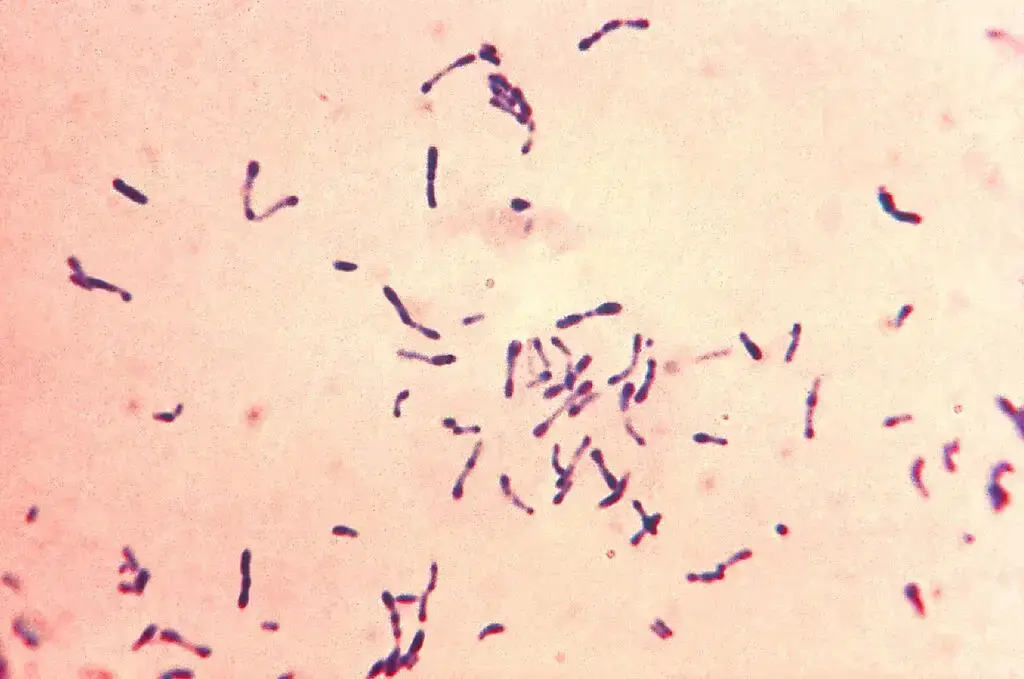
- Both diphtheroids and Corynebacterium diphtheriae are Gram-positive, non-sporulating, non-motile, pleomorphic bacteria. Typically, they are 1 to 3 micrometers long and 0.2 to 0.5 micrometers wide. Corynebacterium diphtheriae can be linear, curved, or branched. Diphtheroids have a club-shaped morphology.
- The cell wall of diphtheroids and Corynebacterium diphtheriae consists of peptidoglycan, teichoic acids, and lipoteichoic acids. Additionally, the cell wall contains several proteins, including the diphtheria toxin.
- Diphtheroids and Corynebacterium diphtheriae share a circular chromosome containing approximately 2.8 million base pairs. The genome of Corynebacterium diphtheriae contains a prophage, a DNA fragment that can be incorporated into the chromosome. The prophage contains the diphtheria toxin gene.
- Diphtheroids and Corynebacterium diphtheriae are aerobic bacteria, requiring oxygen for growth. Additionally, they are catalase-positive and oxidase-positive, indicating that they produce the respective enzymes catalase and oxidase.
- Diphtheroids and Corynebacterium diphtheriae are fermentative bacteria, which can convert carbohydrates into energy. They ferment numerous carbohydrates, such as glucose, sucrose, and lactose.
- Diphtheroids and Corynebacterium diphtheriae are susceptible to numerous antibiotics, such as penicillin, erythromycin, and vancomycin. However, certain strains of Corynebacterium diphtheriae have developed antibiotic resistance.
Due to pervasive vaccination programs, diphtheria is now uncommon in many regions of the globe. In areas with low vaccination rates or during outbreaks, however, the disease remains a significant health risk. If you suspect you have been exposed to diphtheria or are experiencing its symptoms, you must seek immediate medical care for diagnosis and treatment.
Epidemiology of Diphtheroids/Corynebacterium diphtheriae
- Humans are the only known reservoir for C. diphtheriae. Diphtheria is transmitted from person to person through either acute cases or asymptomatic carriers. Principal modes of transmission include respiratory droplets, direct contact with respiratory tract secretions, and exudation from infected epidermis.
- Fomites and dust are not significant transmission vectors, but the organism is resistant to drying and can be isolated from floor dust in a ward or room where an infected patient is being cared for. Milk contaminated by a human carrier has been the cause of epidemics.
- Occasionally, some patients become carriers and continue to harbor C. diphtheriae for weeks or months, or even a lifetime. In the last 50–75 years, the incidence of diphtheria in the Western world has decreased (from 152 cases per 100,000 population in 1920 to 0.002 cases per 100,000 population in 1980 in the United States).
- In 2008, the European Union reported 47 cases. Sixty-two percent were reported by Latvia. Despite the fact that diphtheria is uncommon in the EU, indigenous transmission of the disease persists in certain countries, suggesting that epidemic diphtheria remains a potential threat to the EU.
- Despite the limited number of cases, it is necessary to maintain a high vaccination rate, increase the number of adults who receive a booster shot, and maintain epidemiological surveillance and laboratory capacity.
- As diphtheria began to decline before immunization programmes were implemented and epidemics have occurred even in well-immunized populations, it appears that additional unidentified factors contribute to the low incidence of diphtheria in prosperous nations.
- Although there has been a significant decline in the incidence of the disease in affluent nations (to the point where most physicians in these nations have never seen a case of diphtheria), it remains a significant problem in many developing nations.
Classification of Diphtheroids/Corynebacterium diphtheriae
Diphtheroids, also known as Corynebacterium species, and Corynebacterium diphtheriae can be classified based on various characteristics, including their serotype, biotype, and genomic characteristics. Here are the common classification methods:
- Serotype: Corynebacterium diphtheriae can be classified into different serotypes based on the presence of specific antigens on their cell surface. The most important serotypes are gravis, mitis, and intermedius. Serotyping is primarily used for epidemiological purposes.
- Biotype: Corynebacterium diphtheriae can be further classified into different biotypes based on biochemical characteristics. The most common biotypes are gravis, mitis, intermedius, and belfanti. Biotyping is important for understanding the pathogenicity and epidemiology of different strains.
- Genomic Classification: Corynebacterium diphtheriae strains can also be classified based on their genomic characteristics. Molecular techniques, such as DNA sequencing, allow for a more precise classification and identification of strains. This approach helps in understanding the genetic diversity and evolution of different isolates.
It’s important to note that diphtheroids, which include other Corynebacterium species besides Corynebacterium diphtheriae, can also be classified based on their biochemical properties, genomic characteristics, and other factors. Different species within the diphtheroids group may have specific characteristics that distinguish them from each other.
Classification and identification of diphtheroids and Corynebacterium diphtheriae strains are important for epidemiological surveillance, understanding disease transmission patterns, and selecting appropriate treatment strategies. These classifications help researchers and healthcare professionals study and monitor the bacteria and develop effective preventive measures and treatments.
Structure of Diphtheroids/Corynebacterium diphtheriae
The unique structures of diphtheroids, including Corynebacterium species and specifically Corynebacterium diphtheriae, contribute to their characteristics and pathogenicity. Here is a summary of their organization:
- Cell Shape: As gram-positive bacteria, diphtheroids retain the crystal violet stain during the Gram staining procedure. Typically, Corynebacterium diphtheriae is described as being rod-shaped or bacillary. The cells may be linear or slightly curved and are frequently arranged in clusters or palisades that are irregular in shape.
- Cell Wall: Similar to other gram-positive bacteria, diphtheroids have a thick peptidoglycan layer that provides structural support and rigidity in their cell wall. Alternating N-acetylglucosamine (NAG) and N-acetylmuramic acid (NAM) residues make up the peptidoglycan layer.
- Capsule: Corynebacterium diphtheriae is capable of producing a capsule, a polysaccharide layer that surrounds the bacterial cell for protection. The capsule aids the bacterium in evading the host’s immune system and increases its capacity to colonize and cause disease.
- Flagella: Diphtheroids are typically non-motile, lacking flagella for movement. Therefore, they do not demonstrate motility in standard laboratory experiments.
- Pili and Adhesins: Diphtheroids, such as Corynebacterium diphtheriae, can have pili or fimbriae, which are hair-like appendages on the surface of bacteria. These structures serve a role in adhesion, allowing bacteria to adhere to cells and tissues of the host.
- Toxin Production: Corynebacterium diphtheriae is recognized for producing the potent exotoxin known as diphtheria toxin. This toxin is encoded within the bacterial genome by a bacteriophage. The toxin is released from the bacterial cells and can cause tissue injury in the host, leading to the diphtheria symptoms.
- Proteins: Contain Numbers of Proteins;
- Surface proteins: Numerous proteins cover the surface of both diphtheroids and Corynebacterium diphtheriae. These proteins play multiple roles, including attachment to host cells, quorum sensing, and virulence.
- Membrane proteins: Membrane proteins are present in the membranes of diphtheroids and Corynebacterium diphtheriae. These proteins play a multitude of roles, including nutrient transport, energy production, and signal transduction.
- Cytoplasmic proteins: A number of proteins are present in the cytoplasm of diphtheroids and Corynebacterium diphtheriae. These proteins play a multitude of roles, including metabolism, cell structure, and virulence.
- Chromosome: Diphtheroids and Corynebacterium diphtheriae have a circular chromosome with approximately 2.8 million base pairs. There are numerous genes on the chromosome, including genes for proteins involved in metabolism, cell structure, and virulence.
Understanding the structure of diphtheroids and Corynebacterium diphtheriae is essential for identifying and distinguishing them from other bacteria, studying their pathogenicity, and devising suitable treatments and preventative measures.
Toixn Produced by Diphtheroids/Corynebacterium diphtheriae
The production of toxins plays a pivotal role in the development of the disease, serving as the primary factor responsible for its virulence. The gene that governs the creation of this toxin is encoded by corynebacteriophage, a genetic element that, upon integration into the bacterial genome, has the potential to convert a non-toxigenic strain into a highly virulent toxigenic strain.
This toxin comprises a single polypeptide chain, which spans 535 amino acids. Further examination of the toxins, utilizing X-ray crystallography, as well as genetic and biochemical analysis, has revealed its composition of three distinct functional domains:
- Catalytic domain: This domain possesses ADP ribosyl transferase activity at its N-terminal end.
- Transmembrane domain: This domain aids in the transportation of the catalytic domain across the cell membrane.
- Cell receptor binding domain: Once the diphtheria exotoxin binds to the host cell receptor, it initiates receptor-mediated endocytosis.
After endocytosis, the toxin undergoes acidification. Subsequently, the transmembrane domain inserts itself into the membrane, facilitating the delivery of the catalytic domain to the cytosol. Within the cytosol, the catalytic domain catalyzes the NAD+-dependent ribosylation of elongation factor 2, effectively inhibiting protein synthesis. Although the bacteria acquire the toxin-producing gene from the bacteriophage, the regulation of toxin production is controlled by the bacteria itself. The diphtheria toxin repressor gene (DtxR) resides on the bacterial chromosome, and the expression of tox and bacterial iron metabolism determines the production of the toxin.
Pathogenesis of Diphtheroids/Corynebacterium diphtheriae – What is the mechanism of action of Corynebacterium diphtheria?
Corynebacterium diphtheriae is the bacterium responsible for causing diphtheria, a potentially life-threatening infection. Diphtheroids, also known as non-toxigenic Corynebacterium species, are related bacteria that are similar to C. diphtheriae but do not produce the diphtheria toxin. While they are generally considered to be harmless colonizers of the skin, mucous membranes, and other body sites, they can occasionally cause opportunistic infections.
The pathogenesis, or the process by which these bacteria cause disease, involves several key factors:
- Adherence: Corynebacterium diphtheriae and diphtheroids possess adhesins, which are surface molecules that allow them to attach to host cells. This adherence enables the bacteria to colonize and establish themselves in the host.
- Invasion: After adhering to the host’s epithelial cells, the bacteria can invade deeper tissues, although the mechanisms are not fully understood. It is believed that factors such as enzymes and toxins produced by the bacteria facilitate tissue invasion.
- Toxin production (specific to C. diphtheriae): This is a critical factor in the pathogenesis of diphtheria caused by C. diphtheriae. The bacteria produce a potent exotoxin called the diphtheria toxin. The toxin is encoded by a gene present on a bacteriophage (a virus that infects bacteria) within the bacterial genome. The toxin binds to receptors on host cells, enters them, and interferes with protein synthesis, leading to cell death. The diphtheria toxin is responsible for the characteristic pseudomembrane formation in the throat and can also affect other organs, such as the heart and nervous system.
- Immune response: As the bacteria proliferate and cause tissue damage, the host’s immune system mounts a response. The immune cells recognize the bacteria and their products as foreign and activate an inflammatory response to control the infection. The immune response involves the recruitment of white blood cells, production of antibodies, and other immune mechanisms aimed at eliminating the bacteria.
In the case of diphtheroids, since they do not produce the diphtheria toxin, the disease manifestations are typically milder or absent. However, in individuals with weakened immune systems or underlying medical conditions, diphtheroids can cause opportunistic infections such as bloodstream infections, endocarditis, or infections in surgical sites.
Diagnosis Methods of Diphtheroids
The diagnosis of diphtheroids, or non-toxigenic Corynebacterium species, typically involves several laboratory methods to accurately identify and differentiate these bacteria from other microorganisms. Here are the commonly used diagnosis methods:
- Microbiological culture: This is the primary method used to isolate and grow diphtheroids in the laboratory. A sample is collected from the suspected site of infection, such as wounds, respiratory secretions, or blood, and is streaked onto specific culture media, such as blood agar or chocolate agar. The plates are then incubated at an appropriate temperature to encourage bacterial growth. Diphtheroids typically appear as small, grayish-white colonies.
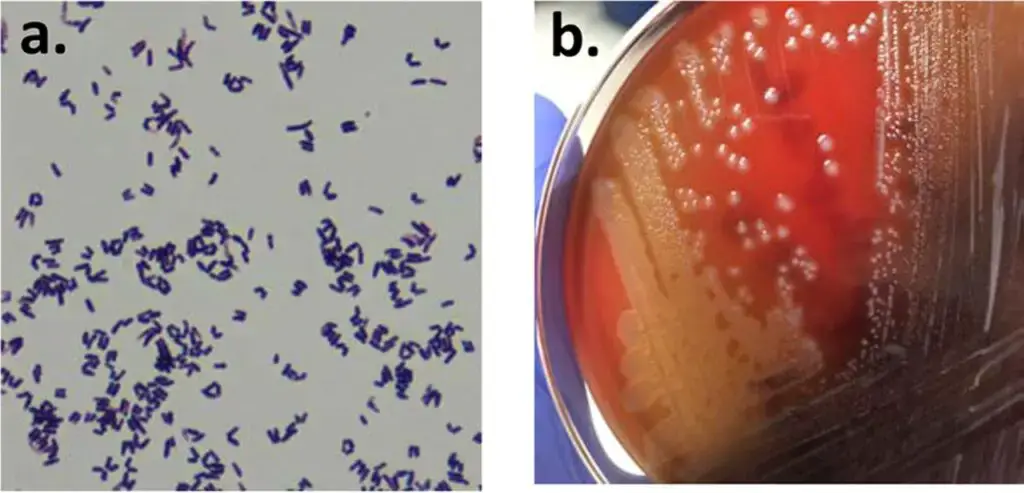
- Gram staining: Gram staining is a rapid technique used to visualize the characteristics of bacteria under a microscope. Diphtheroids are Gram-positive bacteria, meaning they retain the purple crystal violet stain after the staining process. Gram staining can provide a preliminary identification of diphtheroids based on their Gram-positive nature and cellular morphology.
- Biochemical tests: Various biochemical tests can be performed to confirm the identity of diphtheroids and differentiate them from other bacteria. These tests assess the metabolic activities and characteristics of the bacteria. Commonly employed biochemical tests include catalase test (to determine the presence of catalase enzyme), oxidase test (to assess the presence of oxidase enzyme), and sugar fermentation tests (to determine the utilization of specific sugars). These tests help in narrowing down the identification of the specific species of diphtheroids.
- Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS): This is an advanced and rapid diagnostic technique increasingly used in clinical laboratories. It involves the creation of a mass spectrum for each bacterial species, allowing for accurate identification. MALDI-TOF MS can rapidly and reliably identify diphtheroids to the species level, aiding in appropriate treatment decisions.
- Molecular techniques: Polymerase chain reaction (PCR) assays can be employed to detect and identify diphtheroids based on the presence of specific genetic markers or virulence factors. PCR can provide rapid and sensitive results, allowing for early detection and identification of diphtheroids.
Clinical Manifestations of Diphtheroids
Diphtheria is primarily a pediatric disease.15,16 Depending on the location of the pseudomembrane, diphtheria manifests in a variety of forms after an incubation period of 2 to 5 days. The membrane is the defining characteristic of the infection. It is caused by the toxin’s cytotoxic effects on epithelial cells. The membrane is composed of leukocytes, bacteria, cellular detritus, and fibrin, which form a coagulum. It adheres to the tissues beneath it and seeps if separated. In clinical practice, the disease can be separated into the following subtypes: cutaneous, nasal, faucial, tracheolaryngeal, and malignant. In endemic areas, facial diphtheria is more prevalent than cutaneous diphtheria; however, in areas where the disease is uncommon, cutaneous diphtheria is more prevalent.
Clinical Manifestations of Acute Infection
ANTERIOR NASAL DIPHTHERIA
- The most prevalent symptom is nasal discharge (100 percent). This is typically unilateral, initially thin, then purulent and hemorrhagic, with nasal and upper lip skin excoriations. In infants, nasal diphtheria is relatively prevalent. It is typically mild, unless nasopharyngeal or faucial variants co-exist.
FAUCIAL DIPHTHERIA
- Diphtheria, the most prevalent form, typically manifests with a gradual onset characterized by moderate fever, malaise, and a sore throat (around 80% of cases). Additional symptoms may include nausea, vomiting, and painful dysphagia.
- Notably, one or both tonsils exhibit patchy greyish-yellow membranes encompassed by a dull red inflammation zone. Initially, diphtheria can resemble various forms of tonsillitis, often displaying a mere speck of membrane on a single tonsil.
- Subsequently, the membrane may extend to the uvula, soft palate, oropharynx, nasopharynx, or larynx. Alongside this, swollen and tender lymph nodes in the neck and slight neck swelling can be observed.
- It is worth mentioning that the fetor associated with diphtheria is distinctive and was formerly one of the four clinical diagnostic criteria, alongside membrane presence, lymphadenitis, and edema.
TRACHEOLARYNGEAL DIPHTHERIA
- Laryngeal diphtheria is typically secondary to faucial diphtheria (85%). Occasionally, the pharynx has no membrane at all.
- The initial symptoms are moderate fever (75%), hoarseness (100%), a nonproductive cough, and dyspnea. Breathing is progressively obstructed by the expanding membrane and associated oedema over the course of 24 hours.
- Occasionally, the membrane detaches, resulting in severe respiratory obstruction. The severely affected child appears fearful and agitated, but is silent, perspiring, and cyanotic, which is an ominous sign.
- On inspiration, the ancillary muscles of respiration are utilized, with the supraclavicular, substernal, and intercostal tissues retracting. Without a tracheostomy, the child will perish of suffocation.
MALIGNANT DIPHTHERIA
- This is the worst case of diphtheria. The onset is more abrupt compared to other types. The patient swiftly develops ‘toxic’ symptoms, including high fever, rapid pulse, low blood pressure, and cyanosis.
- Typically, the membrane spreads rapidly from the tonsils to the uvula, then creeps across the hard palate, up the nasopharynx, and occasionally down the nostrils.
- Cervical adenitis and oedema produce the classic ‘bull neck’ appearance. The patient may experience bleeding from the mouth, nose, or epidermis.
- Within a few days of the onset, cardiac involvement with heart block occurs. Over fifty percent of malignant diphtheria cases are fatal, and this high mortality rate has not decreased significantly despite treatment.
CUTANEOUS DIPHTHERIA
- In the West, C. diphtheriae skin infections are now more prevalent than nasopharyngeal disease. This affects vagrants and alcoholics living in unsanitary conditions in particular.
- Clinical manifestations vary from a simple pustule to a chronic, non-healing ulcer with a dirty, grey membrane. Infrequently do these infections result in toxic complications, and when they do, they are more likely to manifest as neuritis than myocarditis.
OTHER SITES
- C. diphtheriae can occasionally cause clinical infections at sites such as the ears, conjunctiva, and vagina. Otitis media ear discharge swabs may occasionally grow C. diphtheriae, but toxic manifestations are uncommon.
Toxic Complications
Extreme diphtheria is an awful disease. Even if patients survive the acute destructive phase of the infection, it is likely that they will perish as a result of the toxin’s distant effects. Patients recovering from diphtheria are susceptible to sudden death up to eight weeks after the acute disease. Myocarditis and neuritis are the two most common toxic complications of diphtheria. Risk and severity of toxin injury are proportional to the extent of the pseudomembrane and the delay in antitoxin administration. The frequency of cardiac involvement following laryngeal and malignant diphtheria is 3–8-fold greater than that of tonsillar diphtheria, and 2–3-fold greater if antitoxin is administered 48 hours or later after the onset of disease.
MYOCARDITIS
- Approximately 10% of diphtheria patients develop myocarditis; however, two-thirds of patients with severe infection will exhibit cardiac involvement.
- On admission, myocarditis can be foretold by the extent of the pseudomembrane, and it is virtually inevitable if there is a bull neck. Typically, the first signs of cardiac toxicity appear during the second week of illness.
- Clinical symptoms include soft heart sounds, a gallop cadence, and, less frequently, congestive heart failure symptoms. As the ventricles dilate, dysfunctional murmurs may develop. Diphtheritic myocarditis is associated with a mortality rate of approximately 50%.
- The echocardiogram reveals dilated ventricles with inadequate contraction. Electrocardiographic (ECG) abnormalities are more prevalent than clinical symptoms of myocarditis, and they include frequent supraventricular and ventricular ectopics, bursts of tachyarrhythmia, broadening of the QRS complex, ST and T wave alterations, varying degrees of heart block, and bradyarrhythmias.
- The absence of anterior R waves or the development of complete heart block are both ominous indicators. The mortality rate for patients with bundle branch block and complete heart block is extremely high (over 80%).
- Creatine phosphokinase MB, myoglobin, and troponin levels rise proportionally to the severity of cardiac injury. Although early reports suggested that diphtheria could induce post-recovery conduction disturbances, this has not been confirmed by more recent studies.
NEUROPATHY
- In 10–20% of cases, neurotoxicity is visible. As with myocardial injury, the extent and severity of nervous system involvement are determined by the extent and severity of the primary infection (typically oropharyngeal).
- Exotoxin causes segmental myelin sheath degeneration and, in severe cases, axon cylinder degeneration. In mild diphtheria, polyneuritis is uncommon, but occurs in 7–10% of moderate and severe cases.
- Neurological complications develop late, typically 3 to 8 weeks after the onset of local symptoms, and frequently when other severe manifestations are improving. Paralysis of the soft pharynx is an early and characteristic sign of neuropathy.
- It does not occur with cutaneous diphtheria and is therefore likely caused by the dissemination of oropharyngeal tissue toxin.
- This results in a congested voice and nasal regurgitation of swallowed fluids. Later, impaired vision may result from paralysis of the accommodation muscles, as well as the pharynx, larynx, and respiratory muscles.
- Most frequently affected are the IXth and Xth cranial nerves, followed by the VIIth nerve and the nerves to the external ocular muscles (III, IV, and VI). The cause of mortality from respiratory failure in quadriparesis is frequently paralysis of the respiratory muscles or paralysis of the larynx.
- Approximately fifty percent of neuropathy sufferers experience limb weakness. Specifically, sensory deficits affect proprioception.
- Autonomic dysfunction is common, and between the fourth and seventh weeks of disease, abrupt hypotension may occur. Frequently, the evolution of a neurological deficit is asynchronous, with cranial nerve deficits resolving while peripheral nerve deficits worsening.
- Diphtheric polyneuropathy is more likely than Guillain–Barré syndrome (GBS) to have a bulbar onset, to induce respiratory failure, to progress more slowly, to have a biphasic course, and to result in death or long-term disability.
- In a recent series of diphtheria patients from Latvia, 41% of those with limb impairment were still unable to work one year later. If administered after the second day of diphtheritic symptoms, antitoxin seems ineffective in preventing neuropathy.
OTHER COMPLICATIONS
- Acute tubular necrosis, disseminated intravascular coagulation, endocarditis, and secondary pneumonia are uncommon complications of diphtheria.
- The overall mortality rate of diphtheria is between 5 and 10%, with greater rates in infants and the elderly.
Transmission of Diphtheroids
The transmission of diphtheroids can occur through various routes:
- Direct contact: Diphtheroids can spread from person to person through direct physical contact. This can include shaking hands, hugging, or other forms of close contact with an infected individual.
- Indirect contact: Diphtheroids can also be transmitted indirectly through contact with contaminated surfaces or objects. If an infected person touches a surface or object and then someone else touches the same surface or object, the bacteria can be transferred.
- Airborne transmission: Although diphtheroids are not typically airborne pathogens, some studies have suggested that they can be present in the respiratory droplets of infected individuals. This means that in rare cases, diphtheroids could potentially be transmitted through respiratory droplets when an infected person coughs, sneezes, or talks closely to another person.
Diphtheroids treatment
Diphtheroids are a group of bacteria that are typically harmless and do not require specific treatment. They are commonly found on the skin and mucous membranes of humans and are part of the normal microbial flora.
However, in some cases, diphtheroids can cause infections, particularly in individuals with weakened immune systems or in specific clinical settings. Treatment for diphtheroid infections may vary depending on the type and severity of the infection. Some general treatment approaches include:
- Antibiotics: If a diphtheroid infection requires treatment, antibiotics may be prescribed. The choice of antibiotic depends on the specific bacteria involved and their susceptibility to different antibiotics. Commonly used antibiotics include penicillin, erythromycin, clindamycin, or vancomycin.
- Wound care: In cases where diphtheroids cause skin infections or wound infections, proper wound care is essential. This may involve cleaning the affected area, applying topical antiseptics or antibiotics, and keeping the wound clean and covered.
- Supportive care: In severe cases, supportive care may be necessary, especially if the infection has spread or caused complications. This can include measures such as intravenous fluids, pain management, and monitoring of vital signs.
It’s important to note that diphtheroids are generally resistant to the diphtheria antitoxin, which is specific to the bacteria that cause diphtheria. Therefore, the diphtheria antitoxin is not effective in treating diphtheroid infections.
What antibiotics treat diphtheroids? – Antibiotics for diphtheroids
Diphtheroids, also known as Corynebacterium species, are generally susceptible to a range of antibiotics. The choice of antibiotics depends on the specific strain of diphtheroid and its susceptibility profile. Some commonly used antibiotics to treat diphtheroid infections include:
- Penicillins: Penicillin is often effective against diphtheroids. Examples of penicillin antibiotics include penicillin G and amoxicillin.
- Cephalosporins: Cephalosporin antibiotics, such as cephalexin or ceftriaxone, may be prescribed for diphtheroid infections.
- Macrolides: Macrolide antibiotics, such as erythromycin, clarithromycin, or azithromycin, are commonly used to treat diphtheroids.
- Clindamycin: Clindamycin is another antibiotic that can be effective against diphtheroids.
- Vancomycin: Vancomycin is a potent antibiotic that may be used in cases of more severe or resistant diphtheroid infections.
Diphtheroids gram stain
- Diphtheroids, also known as Corynebacterium species, are Gram-positive bacteria. Gram staining is a common laboratory technique used to classify bacteria into two major groups: Gram-positive and Gram-negative.
- When diphtheroids are subjected to Gram staining, they retain the crystal violet dye, which stains them purple or blue. The Gram-positive nature of diphtheroids indicates that they have a thick peptidoglycan layer in their cell wall, which traps the crystal violet dye during the staining process.
- In contrast, Gram-negative bacteria do not retain the crystal violet dye and instead take up the counterstain, which is usually safranin or fuchsin, appearing pink or red under a microscope.
- Gram staining is a useful diagnostic tool in microbiology laboratories as it provides valuable information about the cellular structure of bacteria and helps in determining appropriate treatment options.
Diphtheroids gram stain Step by stpe Procedure
- Prepare a heat-fixed smear: Take a clean microscope slide and using a sterile loop or swab, transfer a small amount of the bacterial culture (grown on an agar plate or broth) onto the slide. Spread the culture evenly on the slide to create a thin film.
- Air dry the smear: Allow the smear to air dry completely to ensure that the bacterial cells adhere to the slide.
- Heat-fix the smear: Pass the slide through a flame a few times to heat-fix the bacterial cells. This helps to kill the bacteria, adhere them to the slide, and improve their staining properties.
- Flood the slide with crystal violet: Place the heat-fixed smear on a staining rack or holder, and flood the slide with crystal violet stain. Allow the stain to cover the entire smear for about 1 minute.
- Rinse with water: Gently rinse the slide with water to remove excess crystal violet stain.
- Apply iodine solution: Flood the slide with Gram’s iodine solution (iodine and potassium iodide). The iodine acts as a mordant and forms a complex with crystal violet, enhancing its retention by the bacterial cells. Leave the iodine on the slide for about 1 minute.
- Rinse with water: Rinse the slide gently with water to remove excess iodine solution.
- Decolorize with alcohol or acetone: Gently pour a few drops of alcohol or acetone (a decolorizing agent) onto the slide and tilt it slightly to allow the liquid to flow over the smear. Decolorize for a few seconds or until the runoff appears colorless. It is crucial to monitor the decolorization process carefully as over-decolorization may lead to false-negative results.
- Rinse with water: Rinse the slide gently with water to remove the decolorizing agent.
- Counterstain with safranin: Flood the slide with safranin (counterstain) and allow it to cover the smear for about 1 minute. Safranin stains Gram-negative bacteria and any Gram-positive bacteria that may have lost the crystal violet stain during decolorization.
- Rinse with water: Rinse the slide gently with water to remove excess safranin.
- Blot and air dry: Gently blot the slide with bibulous paper or allow it to air dry.
- Examine under a microscope: Once the slide is completely dry, place it on a microscope stage and examine it using a light microscope. Look for purple or blue-stained cells, indicating Gram-positive diphtheroids.
What is diphtheroids in urine?
- Diphtheroids in urine refer to the presence of Corynebacterium species, also known as diphtheroids, in a urine sample. Diphtheroids are a group of bacteria that are commonly found on the skin and mucous membranes of humans and are part of the normal microbial flora.
- While diphtheroids are generally harmless and do not cause significant health issues, their presence in urine can sometimes be a cause for concern. In some cases, it may indicate a urinary tract infection (UTI) or another underlying condition. However, it’s important to note that the significance of diphtheroids in urine depends on the specific clinical context and the presence of accompanying symptoms.
- When diphtheroids are identified in a urine sample, further investigation is usually required to determine if they are playing a role in the patient’s symptoms or if they are merely contaminants. This may involve evaluating the patient’s medical history, conducting additional diagnostic tests, and assessing the presence of symptoms such as urinary frequency, urgency, pain, or other signs of infection.
- If a urinary tract infection is suspected, appropriate treatment with antibiotics may be prescribed based on the susceptibility of the specific strain of diphtheroid bacteria. It’s important to consult a healthcare professional for an accurate diagnosis and appropriate management if diphtheroids are detected in the urine sample.
Diphtheroids in urine treatment/diphtheroids uti treatment
The treatment for diphtheroids in urine depends on the clinical context and the presence of symptoms. If diphtheroids are identified in a urine sample without any accompanying symptoms or signs of infection, treatment may not be necessary as they are often considered contaminants or part of the normal flora.
However, if diphtheroids in urine are associated with symptoms or indicative of a urinary tract infection (UTI), treatment may be required. In such cases, the treatment approach typically involves:
- Antibiotics: The choice of antibiotics depends on the specific strain of diphtheroid bacteria and its susceptibility to different antibiotics. Commonly used antibiotics for treating UTIs caused by diphtheroids include penicillins, cephalosporins, or macrolides. The selection of the appropriate antibiotic should be based on the results of antimicrobial susceptibility testing.
- Duration of treatment: The duration of antibiotic treatment may vary depending on the severity of the infection, the patient’s overall health, and other factors. Typically, UTIs caused by diphtheroids are treated for a duration of 7 to 14 days, but the exact duration will be determined by the healthcare professional.
Diphtheroids antibiotic susceptibility
- The antibiotic susceptibility of diphtheroids, specifically Corynebacterium species, can vary depending on the strain and individual characteristics. It’s important to perform antimicrobial susceptibility testing to determine the specific susceptibility profile of the isolated strain. This testing helps identify which antibiotics are most effective against the particular diphtheroid strain causing the infection.
- The susceptibility testing is typically conducted in a laboratory using standardized methods, such as the disk diffusion method or broth microdilution method. These tests involve exposing the bacteria to different antibiotics and measuring their growth inhibition or minimum inhibitory concentration (MIC).
- The susceptibility results will indicate whether the diphtheroid strain is susceptible, intermediate, or resistant to specific antibiotics. Commonly tested antibiotics for diphtheroids include penicillins (e.g., penicillin G, amoxicillin), cephalosporins (e.g., cephalexin, ceftriaxone), macrolides (e.g., erythromycin, clarithromycin), clindamycin, and vancomycin.
- It’s important to note that antibiotic susceptibility patterns can vary, and it is crucial to follow the guidance of a healthcare professional and rely on the specific susceptibility testing results for accurate treatment decisions.
Rare diphtheroids
Diphtheroids, also known as Corynebacterium species, encompass a diverse group of bacteria. While some strains of diphtheroids are commonly found on the skin and mucous membranes of humans and are considered part of the normal microbial flora, there are also rare or less common strains of diphtheroids that may be encountered in specific clinical contexts or environments.
These rare diphtheroid strains may have unique characteristics, including differences in their virulence, antibiotic susceptibility patterns, or potential to cause infections. Examples of rare diphtheroids include:
- Corynebacterium diphtheriae: While not a rare diphtheroid in the strict sense, it is worth mentioning that the strains of Corynebacterium diphtheriae that cause diphtheria are less commonly encountered today due to widespread vaccination against the disease.
- Corynebacterium jeikeium: This species is an opportunistic pathogen that can cause infections, particularly in immunocompromised individuals or those with underlying medical conditions. It is often associated with bloodstream infections, surgical site infections, and device-related infections.
- Corynebacterium striatum: This species has been implicated in various infections, including bloodstream infections, pneumonia, urinary tract infections, and skin and soft tissue infections. It is often associated with multidrug resistance.
- Corynebacterium accolens: This species is commonly found on the skin and mucous membranes. While it is generally considered harmless, there have been rare reports of it causing infections, such as endocarditis and bloodstream infections.
Diphtheroids in abscess
Diphtheroids, specifically Corynebacterium species, can be occasionally isolated from abscesses. An abscess is a localized collection of pus that forms as a result of an infection, often caused by bacteria.
When diphtheroids are found in an abscess, their clinical significance and role in the infection need to be carefully evaluated. Diphtheroids are part of the normal microbial flora, and their presence alone does not necessarily indicate a pathogenic role in abscess formation. In many cases, diphtheroids may be contaminants or part of the normal skin flora that enter the abscess during the infection process.
The treatment approach for an abscess that contains diphtheroids depends on several factors, including the severity of the infection, the presence of symptoms, and the overall clinical picture. Here are some general considerations:
- Abscess drainage: The primary treatment for an abscess is often drainage. This involves making an incision to allow the pus to drain out. Drainage helps relieve symptoms, promotes healing, and reduces the bacterial burden in the abscess.
- Antibiotics: In some cases, especially if there are signs of spreading infection, systemic symptoms, or immunocompromised individuals, antibiotics may be prescribed. The choice of antibiotics depends on the specific circumstances and should be guided by the results of any relevant culture and susceptibility testing. Commonly used antibiotics for treating abscesses caused by diphtheroids include penicillins, cephalosporins, or clindamycin.
Diphtheroids in wound culture treatment
When diphtheroids are isolated from a wound culture, the treatment approach depends on several factors, including the clinical presentation, severity of the wound infection, presence of symptoms, and the overall health status of the patient. It’s important to note that diphtheroids are often part of the normal skin flora and may be present as contaminants in wound cultures. Therefore, the clinical significance of their presence needs to be carefully evaluated.
If the wound shows signs of infection and symptoms such as redness, swelling, pain, or discharge, treatment may be necessary. The following approaches are generally considered:
- Wound care: Proper wound care is crucial for promoting healing and preventing further infection. This may involve cleaning the wound with sterile saline or an antiseptic solution, removing any dead tissue or debris, and applying appropriate wound dressings. Regular cleaning and dressing changes should be maintained as per healthcare professional’s instructions.
- Antibiotics: In some cases, if there are signs of an active infection, systemic symptoms, or compromised immune system, antibiotics may be prescribed. The choice of antibiotics depends on the severity of the infection, the suspected or identified pathogens, and their susceptibility patterns. Commonly used antibiotics for treating wound infections caused by diphtheroids include penicillins, cephalosporins, or clindamycin. The decision to use antibiotics should be guided by the clinical evaluation and, if available, the results of culture and susceptibility testing.
Diphtheroids examples
Diphtheroids, also known as Corynebacterium species, encompass a diverse group of bacteria. Here are some examples of diphtheroids:
- Corynebacterium diphtheriae: This is the most well-known species among the diphtheroids. It is the causative agent of diphtheria, a potentially serious respiratory infection. Vaccination against diphtheria has significantly reduced its incidence in many parts of the world.
- Corynebacterium jeikeium: This species is an opportunistic pathogen commonly found in hospital environments. It can cause infections in immunocompromised individuals, particularly bloodstream infections, surgical site infections, and device-related infections.
- Corynebacterium striatum: This species has been associated with various infections, including bloodstream infections, pneumonia, urinary tract infections, and skin and soft tissue infections. Some strains of C. striatum have shown multidrug resistance, posing challenges in treatment.
- Corynebacterium accolens: This species is part of the normal skin flora. While it is generally considered harmless, there have been rare reports of it causing infections, such as endocarditis and bloodstream infections.
- Corynebacterium pseudodiphtheriticum: This species is commonly found in the upper respiratory tract and may be associated with respiratory tract infections, particularly in individuals with underlying conditions or compromised immune systems.
FAQ
What are diphtheroids?
Diphtheroids, also known as Corynebacterium species, are a group of bacteria that are commonly found on the skin and mucous membranes of humans. They are part of the normal microbial flora and generally do not cause significant health issues. However, in certain circumstances, they can be associated with infections, particularly in immunocompromised individuals or when they enter sterile areas of the body.
What are the symptoms of a diphtheroid infection?
Symptoms of a diphtheroid infection depend on the site of infection. Infections caused by diphtheroids can occur in various areas, such as the respiratory tract, skin, soft tissues, or other body sites. Common symptoms may include redness, swelling, pain, discharge, and inflammation at the site of infection. Systemic symptoms such as fever, chills, and malaise may also be present, especially in more severe infections.
How are diphtheroids transmitted?
Diphtheroids are generally transmitted through direct contact. They can be passed from person to person through close physical contact or by sharing contaminated objects or surfaces. However, it’s important to note that diphtheroids are commonly present on the skin and mucous membranes of healthy individuals and do not always cause infection or require specific precautions.
How are diphtheroids diagnosed?
Diagnosis of diphtheroids typically involves obtaining a clinical specimen, such as a wound swab, respiratory secretions, or a blood sample, depending on the suspected site of infection. The specimen is then sent to a laboratory for culture and identification of the bacteria. Additional tests, such as Gram staining and antimicrobial susceptibility testing, may be performed to determine the characteristics of the isolated bacteria.
How are diphtheroids treated?
The treatment of diphtheroids depends on the site and severity of the infection. In some cases, no specific treatment may be required if the diphtheroids are considered contaminants or part of the normal flora. However, if the infection is significant or causing symptoms, antibiotics may be prescribed. The choice of antibiotics depends on the specific strain and its susceptibility to different drugs. Proper wound care and other supportive measures may also be implemented, if applicable.
Can diphtheroids be prevented?
Preventing diphtheroid infections primarily involves practicing good hygiene. Regular handwashing, maintaining clean and healthy skin, and following proper wound care procedures can help reduce the risk of infection. In healthcare settings, adherence to infection control protocols, such as appropriate sterilization techniques and barrier precautions, can also minimize the transmission of diphtheroids.
What are the complications of a diphtheroid infection?
Complications of a diphtheroid infection can vary depending on the site and severity of the infection. Possible complications include the spread of infection to surrounding tissues, deep-seated infections, development of abscesses, or the involvement of other body systems. In immunocompromised individuals or those with underlying health conditions, the risk of complications may be higher.
What are the risk factors for a diphtheroid infection?
Risk factors for diphtheroid infections may include immunocompromised states, underlying medical conditions, recent surgeries or invasive procedures, prolonged hospital stays, the presence of indwelling medical devices, poor wound care, and compromised skin integrity. These factors can increase the susceptibility to infection and colonization by diphtheroid bacteria.
What is the prognosis for a diphtheroid infection?
The prognosis for a diphtheroid infection is usually good, especially when prompt and appropriate treatment is administered. Infections caused by diphtheroids are generally localized and do not tend to spread extensively or cause severe complications. However, the prognosis may be influenced by factors such as the overall health of the individual, the presence of underlying conditions, the site of infection, and the presence of any complications. In immunocompromised individuals or those with significant comorbidities, the prognosis may be more variable and require close monitoring and comprehensive management.
What are the latest research findings on diphtheroids?
As of my knowledge cutoff in September 2021, research on diphtheroids continues to focus on various aspects, including their role in healthcare-associated infections, antimicrobial resistance patterns, and the clinical significance of different species and strains. Additionally, research efforts aim to enhance diagnostic techniques, refine treatment strategies, and explore the mechanisms of pathogenicity and virulence factors associated with diphtheroids. It’s important to consult recent scientific literature or seek updated information from reputable sources to learn about the latest research findings on diphtheroids as new studies and advancements are continually emerging in the field.
References
- Chandran R, Puthukkichal DR, Suman E, Mangalore SK. Diphtheroids-Important Nosocomial Pathogens. J Clin Diagn Res. 2016 Dec;10(12):DC28-DC31. doi: 10.7860/JCDR/2016/19098.9043. Epub 2016 Dec 1. PMID: 28208859; PMCID: PMC5296432.
- Murphy JR. Corynebacterium Diphtheriae. In: Baron S, editor. Medical Microbiology. 4th edition. Galveston (TX): University of Texas Medical Branch at Galveston; 1996. Chapter 32. Available from: https://www.ncbi.nlm.nih.gov/books/NBK7971/
- Chaudhary A, Pandey S. Corynebacterium Diphtheriae. [Updated 2022 Aug 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559015/
- Cavalieri, S. J., & Knoop, F. C. (2014). Corynebacterium Infections☆. Reference Module in Biomedical Sciences. doi:10.1016/b978-0-12-801238-3.04943-6
- Hien, T. T., & White, N. J. (2014). Diphtheria. Manson’s Tropical Infectious Diseases, 416–420.e1. doi:10.1016/b978-0-7020-5101-2.00036-4
- Tiwari, T. S. (2013). Diphtheria. Hunter’s Tropical Medicine and Emerging Infectious Disease, 402–406. doi:10.1016/b978-1-4160-4390-4.00037-0
- Smith, K. F., & Oram, D. M. (2009). Corynebacteria (including diphtheria). Encyclopedia of Microbiology, 94–106. doi:10.1016/b978-012373944-5.00216-9
- https://gpnotebook.com/en-gb/simplepage.cfm?ID=-650837939
- https://www.ajo.com/article/0002-9394(89)90114-1/pdf
- http://www.lhp.leedsth.nhs.uk/detail.aspx?id=4111
- https://www.merriam-webster.com/dictionary/diphtheroid
- https://casereports.bmj.com/content/2012/bcr.10.2011.4894
- https://www.jcdr.net/article_fulltext.asp?id=7002
- https://www.usmslab.com/coryneform-bacilli/
- https://jamanetwork.com/journals/jama/article-abstract/236746