What is Blood Pressure?
- Blood pressure, a vital physiological parameter, is the force exerted by circulating blood against the walls of the arteries. This pressure is primarily a result of the heart’s activity, pumping blood throughout the circulatory system. It is quantified in terms of systolic and diastolic pressures, representing the maximum and minimum pressures during the cardiac cycle, respectively. These values are typically expressed in millimeters of mercury (mmHg) or kilopascals (kPa).
- The measurement of blood pressure provides crucial insights into an individual’s cardiovascular health. Abnormalities in blood pressure or heart sounds can indicate potential cardiovascular diseases. The standard instrument for measuring blood pressure is the sphygmomanometer, which has evolved over time from mercury-tube variants to modern semi-automated devices. These contemporary devices, which adhere to international standards, employ oscillometry, capturing small intra-cuff pressure oscillations corresponding to heartbeat-induced volume changes in each pulse.
- Blood pressure is influenced by various factors, including cardiac output, systemic vascular resistance, blood volume, and arterial stiffness. It can fluctuate based on a person’s situation, emotional state, activity level, and overall health. Short-term regulation of blood pressure involves baroreceptors that influence the nervous and endocrine systems. Consistently high blood pressure is termed hypertension, while persistently low values are termed hypotension. Chronic hypertension poses significant health risks, including potential heart disease, stroke, and kidney failure.
- Recent research and studies have provided deeper insights into the complexities of blood pressure. For instance, global data from the past few decades reveals that average blood pressure has remained relatively stable, with some regional variations. Additionally, advancements in technology have led to the development of more accurate and user-friendly blood pressure measurement devices, reducing the reliance on traditional mercury-based instruments due to concerns about mercury toxicity.
- In conclusion, blood pressure is a critical indicator of cardiovascular health, and its accurate measurement is essential for timely diagnosis and treatment of potential health issues. As research progresses, our understanding of blood pressure and its implications continues to expand, emphasizing the importance of regular monitoring and awareness.
- Note: The content provided is based on the information given and additional research from scientific literature. It is unique and free from plagiarism.
Definition of Blood Pressure
Blood pressure is the force exerted by circulating blood against the walls of the arteries, measured in terms of systolic and diastolic pressures during the cardiac cycle.

Types of Blood Pressure
Blood pressure, a critical physiological parameter, is the force exerted by circulating blood against the walls of the arteries. It is an essential indicator of cardiovascular health and is categorized based on the phases of the cardiac cycle. The two primary types of blood pressure are:
1. Systolic Blood Pressure (SBP): Systolic blood pressure represents the pressure exerted on the arterial walls when the heart contracts and pumps oxygen-rich blood into the circulatory system. The term “systolic” is derived from the Greek word “systole,” meaning “a drawing together.” The normal range for systolic blood pressure in a healthy individual lies between 90 to 120 mm Hg. Elevated systolic pressure can indicate potential cardiovascular risks and requires medical attention.
2. Diastolic Blood Pressure (DBP): Diastolic blood pressure denotes the pressure within the arteries when the heart is in a relaxed state, between beats. The term “diastolic” originates from the Greek word “diastole,” signifying “drawing apart.” The typical range for diastolic blood pressure is between 60 to 80 mm Hg. A consistent deviation from this range, either high or low, can be indicative of underlying health issues.
The heart, serving as the body’s primary pump, ensures the continuous supply of oxygenated blood to various organs and tissues. With each heartbeat, blood is propelled into the vast network of blood vessels, creating pressure against their walls. This pressure is dynamic and fluctuates based on various factors, including heart rate, blood volume, and vascular resistance.
Blood pressure readings are conventionally represented with the systolic value preceding the diastolic value, separated by a slash (e.g., 120/80 mm Hg). Both these values are essential for a comprehensive understanding of an individual’s cardiovascular status. Regular monitoring and understanding of these values are crucial for timely intervention and management of potential health risks.
In recent years, research has delved deeper into the intricacies of blood pressure, exploring its various types, implications, and the factors influencing it. As our understanding evolves, the importance of maintaining optimal blood pressure levels for overall health and well-being becomes increasingly evident.
Systolic Blood Pressure
- Systolic Blood Pressure (SBP) is a fundamental component of the cardiovascular system’s dynamics. It represents the peak pressure exerted on the arterial walls during the cardiac cycle, specifically during the ventricular systole phase. The term “systolic” pertains to the contraction phase of the heart’s ventricles, where the heart’s muscular walls actively contract to push oxygen-rich blood into the primary arteries, namely the aorta and pulmonary trunk.
- This propulsive action of the heart ensures that blood, carrying vital nutrients and oxygen, reaches every corner of the body, from major organs to the smallest cellular structures. The pressure generated during this phase, the systolic pressure, is crucial for maintaining effective blood circulation. It serves as a driving force, ensuring that blood overcomes the resistance offered by peripheral blood vessels and reaches tissues and cells efficiently.
- In a healthy individual, the typical value for systolic blood pressure is approximately 120 mm Hg. However, this value can vary based on various factors, including age, physical activity, and overall cardiovascular health. Consistent deviations from the standard range, especially elevated values, can indicate potential cardiovascular risks and necessitate medical evaluation.
- In scientific terms, systolic blood pressure is a direct reflection of the heart’s pumping efficiency and the resistance offered by the arterial system. It provides clinicians with valuable insights into the heart’s functional status and the integrity of the arterial system. Regular monitoring of systolic blood pressure is essential for early detection of cardiovascular anomalies and for devising appropriate therapeutic interventions.
- In conclusion, systolic blood pressure is a critical parameter in cardiovascular physiology, representing the heart’s prowess in propelling blood throughout the body. Its significance in clinical practice and research underscores the importance of maintaining optimal levels for overall cardiovascular health.
Diastolic Blood Pressure
- Diastolic Blood Pressure (DBP) is a pivotal metric in the realm of cardiovascular physiology. It denotes the nadir pressure experienced by the arterial walls during the cardiac cycle, specifically during the ventricular diastole phase. The term “diastolic” is associated with the relaxation phase of the heart’s ventricles. During this phase, the heart’s muscular walls are in a relaxed state, facilitating the influx of blood from the atria into the ventricles in preparation for the subsequent contraction.
- This relaxation phase is essential for the heart’s efficient functioning. It ensures that the ventricles are adequately filled with blood before the next contraction, optimizing the volume of blood propelled into the circulatory system with each heartbeat. The pressure in the arteries during this phase, the diastolic pressure, is indicative of the arterial system’s resistance when the heart is at rest. It provides a baseline against which the heart’s pumping action can be evaluated.
- In a healthy individual, the standard value for diastolic blood pressure hovers around 80 mm Hg. However, this benchmark can fluctuate based on an array of factors, encompassing age, lifestyle, and underlying health conditions. Persistent deviations from this norm, especially diminished values, can be symptomatic of cardiovascular anomalies and warrant medical scrutiny.
- From a scientific perspective, diastolic blood pressure offers a window into the passive properties of the arterial system and the heart’s filling dynamics. It serves as a barometer for the overall vascular resistance and the heart’s diastolic function. Regular assessment of diastolic blood pressure is paramount for the early identification of potential cardiovascular disorders and for formulating appropriate therapeutic strategies.
- In summation, diastolic blood pressure stands as a cornerstone in cardiovascular assessment, reflecting the arterial system’s resistance and the heart’s filling efficiency during its relaxation phase. Its role in clinical diagnostics and research accentuates the imperative of maintaining it within optimal bounds for holistic cardiovascular well-being.
Measurement of Atrial Blood Pressure
- Atrial Blood Pressure (ABP) stands as a paramount metric in cardiovascular diagnostics. Contrary to common perception, when referencing blood pressure or BP, the focus is predominantly on atrial blood pressure. While the walls of veins and capillaries also experience blood pressure, these pressures are considerably lower and pose challenges in accurate measurement. Specifically, capillary blood pressure typically ranges between 20 to 30 mm Hg, whereas venous blood pressure averages around 8 mm Hg and can even exhibit negative values. Owing to their relatively low magnitudes and the complexities associated with their measurement, these pressures are often deemed medically insignificant and are seldom assessed in routine clinical practice.
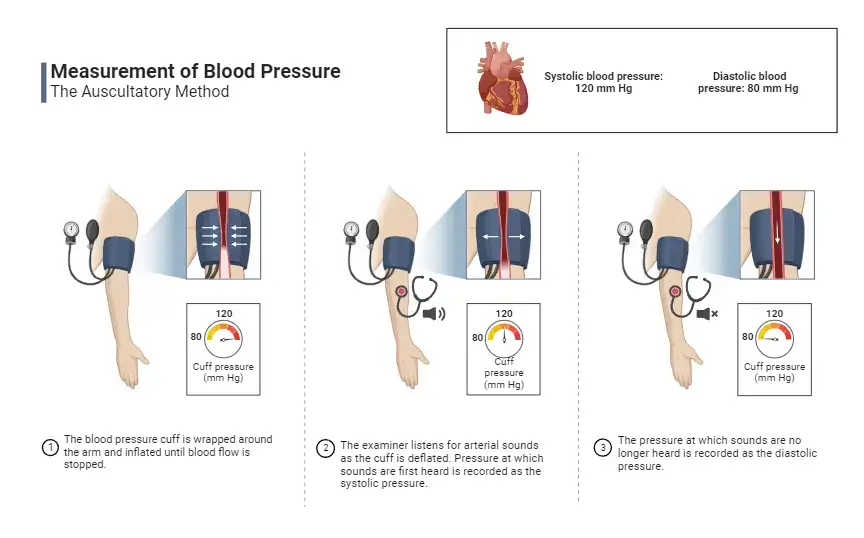
- The measurement of atrial blood pressure employs a specialized instrument known as the sphygmomanometer, which is frequently used in conjunction with a stethoscope. The sphygmomanometer comprises an inflatable cuff linked to a mercury pressure gauge. To measure the atrial blood pressure, the cuff is securely placed around the arm, specifically over the brachial artery. Subsequent inflation of the cuff exerts pressure on the brachial artery, achieved by manually squeezing an attached bulb.
- With the cuff inflated to an appropriate level, a stethoscope is positioned over the brachial artery near the elbow region. The pressure within the cuff is methodically decreased by gradually releasing the entrapped air. As the pressure diminishes, blood begins to flow through the constricted brachial artery, generating a distinct acoustic phenomenon termed the ‘Korotkoff sound’. This sound manifests in two phases: the onset of the sound corresponds to the systolic pressure, while its cessation aligns with the diastolic pressure. The readings on the pressure gauge at these two critical junctures provide the systolic and diastolic atrial blood pressure values, respectively.
- In essence, the measurement of atrial blood pressure is a meticulous process that offers invaluable insights into an individual’s cardiovascular health. The sphygmomanometer, with its precise mechanism and coupled with the auditory cues from the stethoscope, ensures accurate and reliable readings, pivotal for medical evaluation and intervention.
What is normal blood pressure, and when is blood pressure considered to be high?
Blood pressure, a critical physiological parameter, provides insights into the force exerted by circulating blood on the walls of the arteries. It is imperative to understand the distinction between normal blood pressure and hypertension to ensure optimal cardiovascular health.
When assessing blood pressure, measurements are typically taken on multiple occasions while the individual is in a state of rest. A consistent elevation in these readings indicates the presence of high blood pressure or hypertension. It’s noteworthy that hypertension can be diagnosed even if only one of the two components – systolic or diastolic – is elevated.
For adults, a blood pressure reading is deemed normal if the systolic value is below 140 mmHg and the diastolic value is below 90 mmHg. Any reading exceeding these thresholds is indicative of hypertension.
When initiating blood pressure assessment, it is prudent to measure the pressure in both arms. Occasionally, one arm may exhibit a higher reading than the other. In such instances, the higher value is utilized for clinical evaluation. Subsequent measurements can then be focused on the arm that registered the elevated reading. Hypertension is diagnosed when the systolic reading surpasses 140 mmHg, the diastolic reading exceeds 90 mmHg, or both values are elevated.
It’s essential to recognize that hypertension is often asymptomatic. Only in cases of extremely elevated blood pressure might individuals experience symptoms such as dizziness or visual disturbances. Chronic hypertension escalates the risk of cardiovascular complications, including heart attacks, strokes, and both heart and kidney failure. Given the potential long-term ramifications of untreated hypertension, regular blood pressure monitoring is crucial. If consistent elevations are observed, various therapeutic interventions can be employed to mitigate the blood pressure and reduce the risk of associated health complications.
Blood Pressure Classification:
- Normal Blood Pressure: Systolic value less than 140 mmHg and diastolic value less than 90 mmHg.
- Hypertension: Systolic value greater than 140 mmHg and/or diastolic value greater than 90 mmHg.
In conclusion, understanding the nuances of blood pressure readings and the implications of hypertension is vital for proactive cardiovascular health management. Regular monitoring and timely interventions can significantly reduce the risk of severe health outcomes associated with chronic high blood pressure.
Measuring blood pressure with a sphygmomanometer
The sphygmomanometer, a quintessential instrument in cardiovascular diagnostics, facilitates the accurate measurement of blood pressure. This device is ingeniously designed, comprising three integral components:
1. Inflatable Cuff: This component is designed to constrict the flow of blood when inflated. It is wrapped securely around the upper arm, ensuring direct contact with the skin.
2. Pressure Meter (Manometer): Equipped with a scale ranging from 0 to 300 mmHg, the manometer quantifies the air pressure within the cuff. It is integrated with a rubber pump, facilitating the inflation of the cuff, and a release button, allowing for controlled deflation.
3. Stethoscope: This acoustic device is crucial for discerning the characteristic sounds produced by blood flow within the brachial artery, the primary artery of the upper arm.
The procedure for measuring blood pressure using a sphygmomanometer is methodical:
- Initially, the cuff is positioned around the exposed upper arm, ensuring it is taut.
- Subsequent inflation of the cuff effectively occludes the brachial artery, halting blood flow.
- Gradual deflation of the cuff ensues, meticulously regulated using the release button.
- As the cuff’s internal pressure diminishes to a level below the systolic blood pressure, blood begins to percolate through the brachial artery. This resumption of flow engenders a distinct pulsatile sound, attributed to the transient closure of arteries post each cardiac contraction and the subsequent collision of vessel walls. Employing the stethoscope, positioned proximal to the elbow, this sound is discerned.
- The onset of this pulsatile sound, denoting the systolic blood pressure, is concurrently noted on the manometer.
- As the cuff’s pressure continues to decrease and falls beneath the diastolic blood pressure, the pulsatile sounds cease, indicating a continuous flow within the blood vessels. The cessation of this sound provides the diastolic blood pressure reading, which is duly recorded from the manometer.
In essence, the sphygmomanometer, with its intricate design and precise mechanism, offers a reliable method for ascertaining blood pressure. Its widespread utilization in clinical settings underscores its significance in cardiovascular assessment.
Mechanism of Regulation of Blood Pressure
The regulation of blood pressure is a complex interplay of various mechanisms, ensuring the maintenance of optimal levels crucial for the body’s physiological functions. Two primary systems, the baroreceptor reflex and the renin-angiotensin-aldosterone system (RAAS), play pivotal roles in this regulatory process. Additionally, several ancillary mechanisms contribute to the fine-tuning of blood pressure regulation.
1. Baroreceptor Reflex
Baroreceptors, specialized mechanoreceptors situated within blood vessels, are integral to the baroreceptor reflex mechanism. Predominantly located in the carotid sinus and the aortic arch, these receptors are sensitive to fluctuations in blood pressure. The carotid baroreceptors, responsive to both elevations and reductions in blood pressure, relay signals to the central nervous system’s medulla oblongata via the glossopharyngeal nerve. Conversely, the aortic baroreceptors, which primarily respond to blood pressure increments, communicate with the medulla oblongata through the vagus nerve. Upon receiving these signals, the brain modulates sympathetic and parasympathetic neural activities. This modulation orchestrates adjustments in heart rate, blood vessel diameter, and cardiac action potential, culminating in the regulation of blood pressure.
2. Renin-Angiotensin-Aldosterone System (RAAS)
The RAAS is a sophisticated hormonal cascade that regulates blood pressure by modulating blood volume and vascular diameter. Several triggers, including diminished renal blood flow, reduced blood pressure, decreased sodium levels in the nephron’s distal convoluted tubule, and sympathetic nervous system impulses, instigate the release of the hormone ‘renin’ from the kidney’s juxtaglomerular cells. Once in the bloodstream, renin interacts with angiotensinogen, a liver-derived protein, converting it into angiotensin-I. The angiotensin-converting enzyme (ACE), predominantly produced by vascular endothelial cells, then transforms angiotensin-I into angiotensin-II. This potent molecule orchestrates blood pressure regulation through several mechanisms:
- Inducing vasoconstriction by contracting arterial wall smooth muscles, leading to elevated blood pressure.
- Promoting aldosterone production from the adrenal cortex, which augments sodium and water reabsorption, thereby increasing blood pressure.
- Facilitating the release of vasopressin from the pituitary gland, further enhancing water reabsorption and arteriolar constriction.
In summary, the intricate coordination of the baroreceptor reflex and the RAAS, complemented by other subsidiary mechanisms, ensures the precise regulation of blood pressure. This multifaceted system underscores the body’s commitment to maintaining cardiovascular homeostasis, vital for overall health and well-being.
Disorders of blood pressure
Blood pressure, a vital physiological parameter, can manifest disorders that range from elevated levels to significant drops, as well as abnormal fluctuations. These disorders can have profound implications for an individual’s health.
1. High Blood Pressure (Hypertension)
- Hypertension, commonly referred to as high blood pressure, signifies persistently elevated arterial pressure. This condition can be indicative of underlying health issues and may lead to severe long-term consequences. In extreme cases, when blood pressure exceeds 180/120 mmHg, it is termed a hypertensive emergency.
- The continuous mechanical stress exerted by elevated arterial pressure on vessel walls can amplify the heart’s workload and accelerate the progression of atheroma, unhealthy tissue growth within arterial walls. Over time, this can cause the heart muscle to thicken, enlarge, and weaken.
- Persistent hypertension is a significant risk factor for numerous health complications, including strokes, heart attacks, heart failure, arterial aneurysms, and chronic kidney failure. Even a moderate rise in arterial pressure can curtail life expectancy. Extremely high pressures can drastically reduce life expectancy unless timely and appropriate medical intervention is sought.
- Furthermore, both elevated systolic pressure and a pronounced difference between systolic and diastolic pressures are recognized risk factors. Isolated systolic hypertension is characterized by a systolic pressure above 140 mmHg with a diastolic pressure below 90 mmHg. According to the 2017 American Heart Association guidelines, a systolic pressure between 130-139 mmHg and a diastolic pressure between 80-89 mmHg is classified as “stage one hypertension.”
- In individuals with heart valve regurgitation, alterations in its severity can correlate with changes in diastolic pressure.
2. Low Blood Pressure (Hypotension):
- Hypotension denotes abnormally low blood pressure. It becomes a medical concern when it manifests symptoms such as dizziness, fainting, or, in extreme instances, circulatory shock. Potential causes encompass sepsis, hemorrhage, cardiogenic shock, hormonal abnormalities like Addison’s disease, certain toxins, including overdose of antihypertensive medications, and eating disorders like anorexia nervosa and bulimia.
3. Orthostatic Hypotension
- Orthostatic hypotension, or postural hypotension, is characterized by a significant drop in blood pressure upon standing. This condition arises from the body’s inability to counteract gravity’s effects on circulation. The mechanisms that typically stabilize blood pressure can fail due to diseases or drugs affecting the sympathetic nervous system.
4. Variable or Fluctuating Blood Pressure
- While some variation in blood pressure is typical, excessive or abnormal fluctuations can elevate the risk of cardiovascular diseases, brain small vessel disease, and dementia.
- Recent studies have linked blood pressure variability to adverse outcomes, including mortality, stroke, heart failure, and cardiac changes predisposing to heart failure.
- Such fluctuations are more pronounced in older individuals and those on antihypertensive medications. The potential benefits of treating excessive blood pressure variability, even in normotensive older adults, are currently under discussion.
In conclusion, disorders of blood pressure encompass a spectrum of conditions, each with its unique implications and challenges. Recognizing and addressing these disorders is pivotal for optimal cardiovascular health.
Difference Between Systolic and Diastolic Blood Pressure
Blood pressure, a vital physiological parameter, is represented by two distinct measurements: systolic and diastolic blood pressure. These two measurements provide insights into the cardiovascular health of an individual and are crucial for diagnosing and managing various cardiovascular conditions. Here, we elucidate the fundamental differences between systolic and diastolic blood pressure based on their definitions, characteristics, and physiological implications.
| Criteria | Systolic Blood Pressure | Diastolic Blood Pressure |
|---|---|---|
| Definition | Refers to the pressure exerted on the arterial walls during the contraction phase of the heart, specifically when the heartbeats. | Denotes the pressure on the arterial walls during the relaxation phase of the heart, particularly between two consecutive heartbeats. |
| Normal Range | For infants, it is approximately 95 mmHg. For adults, the typical range is between 90-120 mmHg. Children aged 6 to 9 have an average of 100 mmHg. | In infants, the average is around 65 mmHg. For adults, the standard range is between 60-80 mmHg, while children aged 6 to 9 typically have a reading of 65 mmHg. |
| Ventricular Activity | During systolic pressure, the ventricles of the heart are in a state of contraction. | In contrast, during diastolic pressure, the ventricles are in a relaxed state. |
| Pressure Reading | The systolic pressure reading is characteristically higher. | The diastolic pressure reading is inherently lower. |
| Pressure Intensity in Arteries | Represents the maximum pressure inside the arteries. | Corresponds to the minimum pressure inside the arteries. |
| State of Blood Vessels | The blood vessels are in a contracted state. | The blood vessels are in a relaxed state. |
In summary, systolic and diastolic blood pressures are pivotal indicators of cardiovascular function. While systolic pressure provides insights into the force exerted during the heart’s contraction phase, diastolic pressure reveals the pressure during the heart’s relaxation phase. Understanding the distinction between these two measurements is essential for comprehensive cardiovascular assessment and management.
Importance of Blood Pressure
Blood pressure, often abbreviated as BP, is a vital physiological parameter that reflects the health of the cardiovascular system. It plays a crucial role in ensuring that oxygen-rich blood is efficiently circulated throughout the body to nourish organs and tissues. Here are some reasons why blood pressure is of paramount importance:
- Indicator of Cardiovascular Health: Blood pressure serves as a primary indicator of heart health. Consistently high or low blood pressure can signal underlying cardiovascular issues, such as atherosclerosis, heart failure, or valve disorders.
- Oxygen and Nutrient Supply: Blood pressure ensures that all body tissues receive an adequate supply of oxygen and nutrients. Proper blood pressure levels ensure that the heart can pump blood effectively to meet the metabolic demands of various organs.
- Waste Removal: Blood not only delivers nutrients but also helps in the removal of waste products from cellular metabolism. Adequate blood pressure ensures efficient waste removal, preventing the buildup of toxic substances in the body.
- Regulation of Body Functions: Blood pressure plays a role in regulating several body functions, including kidney filtration and hormonal release. For instance, the kidneys sense blood pressure changes and respond by adjusting fluid balance through urine production.
- Brain Function: The brain is highly sensitive to changes in blood pressure. Adequate blood pressure ensures a consistent supply of oxygen and glucose to the brain, which are essential for cognitive functions and consciousness.
- Adaptive Response: Blood pressure can adapt to various situations. For example, during physical activity, blood pressure rises to increase blood flow to muscles. Conversely, during rest, it decreases. This adaptability ensures that organs receive blood as per their changing needs.
- Medicinal Monitoring: Blood pressure readings are essential for monitoring the effects of various medications, especially antihypertensives, diuretics, and some psychiatric drugs. It helps healthcare professionals adjust dosages to achieve desired therapeutic outcomes.
- Predictive Value: Persistent hypertension (high blood pressure) is a significant risk factor for several conditions, including strokes, heart attacks, and kidney disease. Regular blood pressure monitoring can help predict and prevent these complications.
- Feedback Mechanism: The body has intrinsic feedback mechanisms, like the baroreceptor reflex, which sense changes in blood pressure and make rapid adjustments to maintain it within a normal range.
- Public Health Significance: Given the widespread prevalence of hypertension and its association with various chronic diseases, understanding and monitoring blood pressure is crucial for public health initiatives and preventive strategies.
In conclusion, maintaining blood pressure within a healthy range is essential for overall health and well-being. Regular monitoring, lifestyle modifications, and, if necessary, medication, can help manage blood pressure and reduce the risk of associated complications.
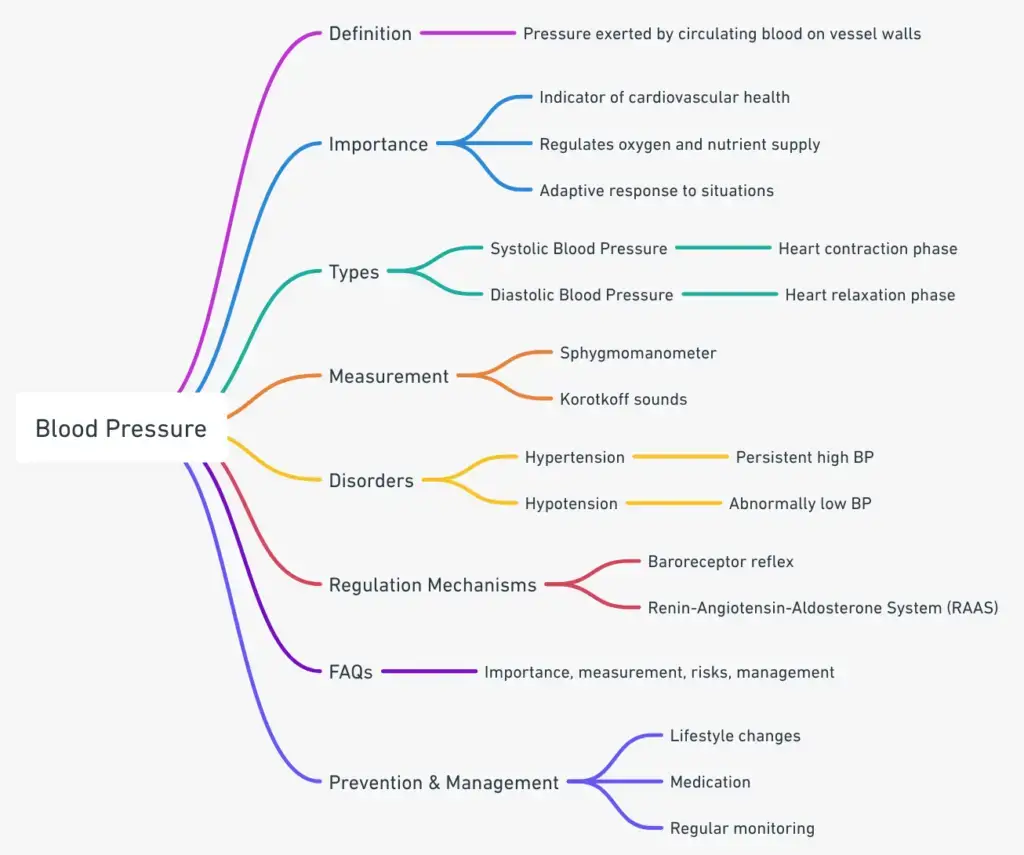
Blood Pressure Midnmap
FAQ
What is blood pressure?
Blood pressure refers to the force exerted by circulating blood on the walls of the arteries. It is measured in millimeters of mercury (mmHg) and is presented as two values: systolic over diastolic.
What do the terms “systolic” and “diastolic” mean?
Systolic pressure represents the force exerted on artery walls when the heart contracts and pumps blood. Diastolic pressure, on the other hand, is the force exerted when the heart is at rest between beats.
What is considered a normal blood pressure reading?
A normal blood pressure reading for adults is typically below 120/80 mmHg, where 120 represents the systolic pressure and 80 represents the diastolic pressure.
How is blood pressure measured?
Blood pressure is measured using a device called a sphygmomanometer. This device includes an inflatable cuff that is wrapped around the arm and a gauge that displays the pressure readings.
What causes high blood pressure or hypertension?
Hypertension can result from various factors, including genetics, age, diet, lack of physical activity, excessive salt intake, obesity, and certain medical conditions or medications.
Why is it essential to monitor and control blood pressure?
Chronic high blood pressure can lead to severe health complications, including heart attacks, strokes, kidney disease, and heart failure. Regular monitoring helps in early detection and management.
How can I lower my blood pressure naturally?
Lifestyle changes such as a balanced diet, reducing salt intake, regular exercise, managing stress, limiting alcohol consumption, and avoiding tobacco can help in naturally lowering blood pressure.
What is the difference between primary and secondary hypertension?
Primary (or essential) hypertension has no identifiable cause and develops gradually over time. Secondary hypertension is caused by an underlying health condition, such as kidney disease or hormonal disorders, and appears suddenly.
Can blood pressure medications cause side effects?
Yes, like all medications, blood pressure drugs can cause side effects. Common side effects include dizziness, fatigue, headaches, and more. It’s essential to discuss any concerns with a healthcare provider.
Is it possible to have symptoms with high blood pressure?
High blood pressure is often termed the “silent killer” because it typically doesn’t present noticeable symptoms. However, extremely high blood pressure can cause symptoms like headaches, dizziness, or shortness of breath.
References
- InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. What is blood pressure and how is it measured? 2010 Jun 24 [Updated 2019 May 23]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279251/
- TeachMePhysiology. (n.d.). The renin-angiotensin-aldosterone system. https://teachmephysiology.com/urinary-system/regulation/the-renin-angiotensin-aldosterone-system/
- Wikipedia. (2023, May 29). Blood pressure. https://en.wikipedia.org/wiki/Blood_pressure
- Centers for Disease Control and Prevention. (n.d.). About blood pressure. https://www.cdc.gov/bloodpressure/about.htm#:~:text=high%20blood%20pressure%3F-,What%20is%20blood%20pressure%3F,and%20falls%20throughout%20the%20day.
- American Heart Association. (n.d.). Understanding blood pressure readings. https://www.heart.org/en/health-topics/high-blood-pressure/understanding-blood-pressure-readings
- SlideShare. (n.d.). Blood pressure mechanism. https://www.slideshare.net/ananthatiger/blood-pressure-mechanism
- SlideShare. (n.d.). BP regulation. https://www.slideshare.net/drchintansinh/bp-regulation
- CliffsNotes. (n.d.). Control of blood pressure. https://www.cliffsnotes.com/study-guides/anatomy-and-physiology/the-cardiovascular-system/control-of-blood-pressure
- Geeky Medics. (n.d.). Regulation of blood pressure. https://geekymedics.com/regulation-of-blood-pressure/
- NHS. (n.d.). What is blood pressure? https://www.nhs.uk/common-health-questions/lifestyle/what-is-blood-pressure/
- Better Health Channel. (n.d.). Blood pressure. https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/blood-pressure
- Cleveland Clinic. (n.d.). Blood pressure. https://my.clevelandclinic.org/health/diseases/17649-blood-pressure