Epstein-Barr Virus (EBV), also known as Human Herpesvirus 4, is a virus that belongs to the herpesvirus family. It is one of the most common viruses in humans and is estimated to infect over 90% of people worldwide at some point in their lives. EBV is primarily transmitted through contact with infected saliva, such as through kissing, sharing food or drinks, or other close contact with an infected person.
While most people infected with EBV show no symptoms, the virus can cause a range of illnesses, from mild to severe, including:
- Infectious mononucleosis (mono): This is a common illness caused by EBV that can cause symptoms such as fever, sore throat, swollen lymph nodes, fatigue, and body aches.
- Burkitt’s lymphoma: EBV is strongly associated with this type of cancer, which primarily affects children and young adults in Africa.
- Nasopharyngeal carcinoma: EBV is also strongly associated with this type of cancer, which primarily affects people in Asia and Africa.
- Hodgkin’s lymphoma: EBV is found in some cases of Hodgkin’s lymphoma, a type of cancer that affects the lymphatic system.
- Other illnesses: EBV has also been associated with other illnesses, such as chronic fatigue syndrome, multiple sclerosis, and autoimmune diseases.
EBV can be diagnosed through blood tests that look for specific antibodies to the virus. Treatment for EBV varies depending on the illness and severity of symptoms. For infectious mononucleosis, treatment usually involves managing symptoms, such as rest, pain relief, and fluids to prevent dehydration. For more severe illnesses, such as Burkitt’s lymphoma or nasopharyngeal carcinoma, treatment may involve chemotherapy, radiation therapy, and other cancer treatments.
Prevention of EBV infection can be challenging as the virus is highly contagious, but measures can be taken to reduce the risk of transmission, such as avoiding close contact with infected individuals, not sharing food or drinks, and practicing good hygiene, such as washing hands frequently and thoroughly.
The Epstein–Barr virus (EBV), also known as Human gammaherpesvirus 4, is one of the nine known varieties of human herpesviruses and one of the most prevalent viruses in humans. EBV is classified within the Herpesviridae family, Gammaherpesvirinae subfamily, and Lymphocryptovirus genus. It is most well-known for causing infectious mononucleosis (“mono” or “glandular fever”). In addition, it is associated with various non-malignant, premalignant, and malignant Epstein–Barr virus-associated lymphoproliferative diseases and, according to some evidence, an increased risk of developing specific autoimmune diseases. Approximately 200,000 cases of malignancy per year are attributed to EBV worldwide. In 2022, a large study (population of 10 million over 20 years) suggested that EBV is the primary cause of multiple sclerosis, with a recent EBV infection increasing the risk of developing the disease by 32-fold.
EBV has an 184 kilobase pair double-stranded DNA genome that encodes nearly 100 proteins. The DNA is surrounded by a protein nucleocapsid, which is surrounded by a protein tegument, which is surrounded by an envelope containing lipids and surface projections of glycoproteins that are essential for infecting the host cell. The structure of the Epstein–Barr virus is depicted in Figure 1.
Structure of Epstein-Barr Virus (EBV)
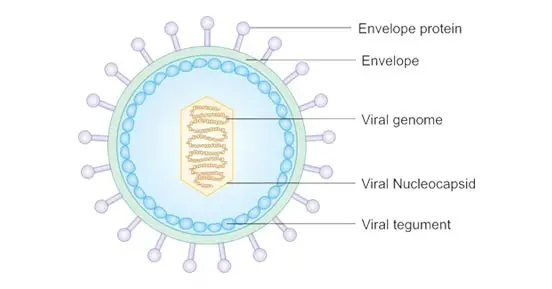
- Epstein-Barr virus has a diameter of 122–180 nm and consists of a double helix of deoxyribonucleic acid (DNA) containing approximately 172,000 base pairs and 85 genes.
- DNA is surrounded by a protein nucleocapsid, which is surrounded by a protein tegument, which is surrounded by an envelope containing lipids and surface projections of glycoproteins, which are essential for infecting the host cell.
- EBV has a structure similar to other herpesviruses, consisting of a double-stranded DNA enclosed in an icosahedral protein capsid with 162 capsomers.
- A protein tegument is also present between the capsid and envelope, which is embedded with glycoproteins that play a crucial role in cell tropism, host range, and cell recognition. The mature virions have a diameter of approximately 120 to 180mm.
- Currently, EBV has two recognized subtypes, Type 1 and Type 2 (also known as Type A and Type B), which differ from each other at the EBV nuclear antigen loci (EBNA).
Genome structure of Epstein-Barr Virus (EBV)
- The genome of herpesviruses is double-stranded linear DNA ranging from 120 to 250 kilobase pairs.
- The variation in size of the DNA genome is due to the arrangement of their DNA sequences.
- The genomes have terminal and internal repeat sequences bounded by a unique long (UL) and a unique short (US) region.
- Some members of the herpesvirus family can undergo genomic rearrangement due to the repeats, leading to different genomic isomers.
- Spontaneous deletions occur due to the high incidence of rearrangement, resulting in defective viral particles being common.
- There is little DNA homology among the different species in the herpesvirus family.
- HSV types 1 and 2 share 50% sequence homology, and herpesvirus 6 and 7 share 30–50% homology.
- Digestion of the genome with restriction endonucleases will yield a characteristic fragment pattern specific for each family member, allowing for rapid epidemiologic tracing of a given strain.
- The genome of the typical herpesvirus encodes for at least 100 different proteins, many of which are structural in nature.
- Herpesviruses encode for a number of virus-specific enzymes involved in nucleic acid metabolism, which are expressed only during replication within the host cell.
Epidemiology of Epstein-Barr Virus (EBV)
- Almost 95% of the world’s adult population is infected with the Epstein Barr virus. In the United States, 66.5% of children and adolescents between the ages of 6 and 19 were EBV-positive.
- Children aged 6 to 8 years had a prevalence of approximately 54 percent, whereas adolescents aged 18 to 19 years had a prevalence of 82.9%.
- More females were infected than males, but the difference was negligible. Epstein Barr virus was more prevalent among Mexican-American children and adolescents than among non-Hispanic Negroes and Whites.
- Children and adolescents with larger households, lesser household incomes, less parental education, and foreign birth were more likely to be infected with Epstein Barr virus.
- The prevalence of Epstein Barr virus varies globally. In England, the prevalence of Epstein Barr virus among minors aged 11 to 24 was 74.6%. In comparison to older adolescents, the prevalence of Epstein Barr virus was lower among 11- to 14-year-old patients.
- 93% of young adults ages 22 to 24 were seropositive. In a study population from Tehran, Iran, Epstein Barr virus IgG antibody seroprevalence was 81.4%. Nearly 95% of subjects older than 40 were seropositive.
- The prevalence of seropositive subjects increased with age, with the exception of infants. Infants had elevated levels of Epstein Barr virus IgG antibodies that decreased with age, most likely due to the gradual loss of maternal antibodies.
- According to a study, the prevalence rate in China is greater than fifty percent before the age of three and over ninety percent between the ages of eight and nine.
- One study found that infection rates tend to rise between June and August, presumably as a result of increased human contact during the summer months.
Replication of Epstein-Barr Virus (EBV)
Entry to the cell
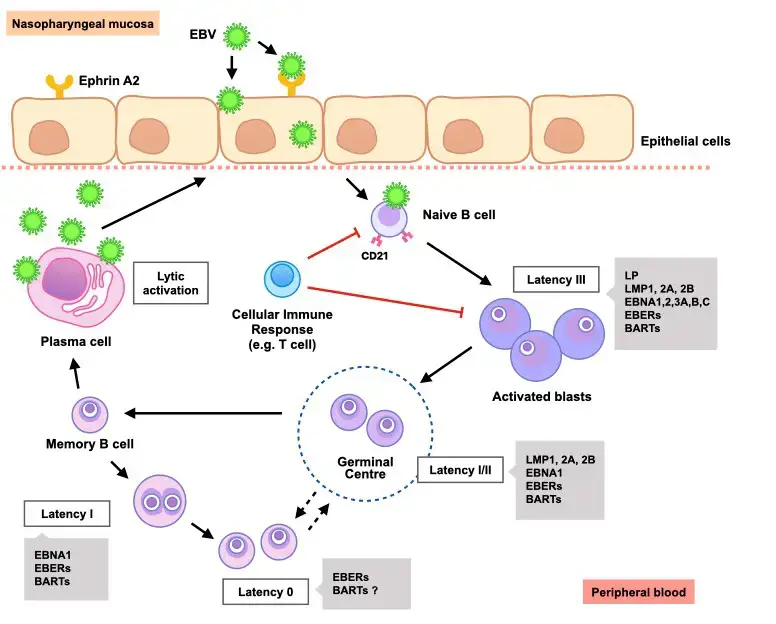
- EBV is capable of infecting both B and epithelial cells.
- Viral glycoprotein gp350 binds to cellular receptor CD21 in order to enter B cells (also known as CR2).
- Viral glycoprotein gp42 then interacts with cellular MHC class II molecules, activating fusion of the viral envelope with the cell membrane and permitting EBV entry into the B cell.
- Human CD35, also known as complement receptor 1 (CR1), is an additional attachment factor for gp350/220 that allows EBV to enter CD21-negative cells, such as immature B-cells.
- CD35 expression is downregulated by EBV infection.
- The viral protein BMRF-2 interacts with cellular 1 integrins in order to penetrate epithelial cells.
- Viral protein gH/gL interacts with cellular v6/v8 integrins, triggering fusion of the viral envelope with the epithelial cell membrane and permitting EBV entry into the epithelial cell.
- Unlike B-cell entry, viral glycoprotein gp42 actually impedes epithelial-cell entry.
- As soon as EBV penetrates a cell, the viral capsid disassembles and the viral genome is transported to the cell nucleus.
Lytic replication
- EBV can produce infectious virions during the lytic cycle, also known as productive infection.
- Lytic replication can occur in both B cells and epithelial cells, but in B cells it usually happens after reactivation from latency.
- The viral genome must be linear for lytic replication to take place, which contrasts with the circular latent EBV genome.
- During lytic replication, viral DNA polymerase copies the viral genome instead of host-cell DNA polymerase during latency.
- Lytic gene products are produced in three stages: immediate-early, early, and late.
- Immediate-early lytic gene products enhance the expression of later lytic genes and include BZLF1 and BRLF1.
- Early lytic gene products have various functions, including replication, metabolism, and blockade of antigen processing. BNLF2 is an example of early lytic gene products.
- Late lytic gene products tend to have structural roles such as VCA, which forms the viral capsid, and BCRF1, which helps EBV evade the immune system.
- EGCG, a polyphenol in green tea, has shown to inhibit EBV spontaneous lytic infection at different levels in a time- and dose-dependent manner in a study.
- Specific inhibitors suggest that the Ras/MEK/MAPK pathway contributes to EBV lytic infection through BZLF1 and PI3-K pathway through BRLF1.
- Activation of some genes is being studied to induce immune destruction of latently infected B-cells by use of either TPA or sodium butyrate.
Replication of Epstein-Barr Virus (EBV)
- Attachment/Adsorption
- Virus attaches to host cells through receptors like CD21 and integrin proteins
- Interaction of receptors with viral glycoproteins
- Penetration
- EBV virus penetrates host cells through fusion
- gp42 interacts with HLA class II molecule of B cell
- EBV gH/gL envelope protein interacts with αvβ6/8 integrins of epithelial cells
- Fusion allows entry of viral particle
- Uncoating
- Capsid separated from viral genome by host lysosomal enzymes
- Viral DNA released into cytoplasm and enters nucleus
- Biosynthesis
- Linear dsDNA converted to circular DNA and replicated through rolling circle mechanism
- During viral latency, latent genes transcribed and circular DNA can persist for decades
- In lytic phase, intermediate-early, early, and late mRNA synthesized and leave nucleus
- Synthesized mRNA translated to proteins in free ribosomes or ribosomes on endoplasmic reticulum
- Assembly
- Capsid proteins enter nucleus and form nucleocapsid with viral genome
- Bud off nuclear membrane with single membrane envelope
- Maturation
- Maturation of virus takes place in endoplasmic reticulum and Golgi bodies
- Released back to cytoplasm
- Release
- Viruses released from infected host cells through lysis of host cell membrane.
Pathogenesis of Epstein-Barr Virus (EBV)
- Different classes of cells are infected by the Epstein-Barr virus (EBV) via distinct mechanisms. EBV is capable of infecting both B and epithelial cells.
- The viral glycoprotein gp350 binds to a cellular receptor in order to penetrate B cells. The viral glycoprotein gp42 then interacts with MHC class II molecules in the host cell.
- This causes the viral envelope to fuse with the cell membrane, thereby allowing EBV to penetrate the B cell.
- Human CD35 is an additional attachment factor for gp350/220 and can facilitate EBV entry into CD21-negative cells, such as immature B cells. Once the initial lytic infection of EBV is brought under control, the virus remains latent in the individual’s B cells for life.
- The viral protein BMRF2 interacts with 1 integrins to penetrate epithelial cells. The viral proteins gH/gL then interact with v6/v8 integrins. This causes the viral envelope to fuse with the epithelial cell membrane, permitting EBV to penetrate the epithelial cell.
Clinical Manifestations of Epstein-Barr Virus (EBV)
- Infectious mononucleosis (IM): Also known as glandular fever or kissing disease, IM is the most common clinical manifestation of EBV infection. Symptoms include fever, sore throat, swollen lymph nodes, fatigue, and enlarged spleen and liver.
- Burkitt’s lymphoma: A type of non-Hodgkin’s lymphoma, Burkitt’s lymphoma is associated with EBV infection in endemic areas, such as Africa. It typically presents as a rapidly growing mass in the jaw, facial bones, or abdomen.
- Nasopharyngeal carcinoma (NPC): NPC is a rare cancer of the nasopharynx that is strongly associated with EBV infection, especially in Southeast Asia. Symptoms include a lump in the neck, nasal congestion, hearing loss, and facial numbness.
- Hodgkin’s lymphoma: A type of lymphoma characterized by the presence of Reed-Sternberg cells, Hodgkin’s lymphoma is associated with EBV infection in a subset of cases.
- Chronic active EBV infection (CAEBV): CAEBV is a rare complication of EBV infection characterized by persistent fever, lymphadenopathy, and abnormal liver function tests.
- Oral hairy leukoplakia (OHL): OHL is a white patch on the tongue or cheek that is seen in HIV-infected individuals and is strongly associated with EBV infection.
- Other less common manifestations: EBV infection has been associated with various other clinical manifestations, such as hepatitis, pneumonitis, encephalitis, and autoimmune diseases.
Diagnosis of Epstein-Barr Virus (EBV)
Diagnosis of Epstein-Barr Virus (EBV) typically involves laboratory testing to detect either the virus itself or antibodies produced by the immune system in response to the virus. Common methods of diagnosis include:
- Blood tests: These can detect the presence of antibodies to EBV, including IgM and IgG antibodies, and can help determine whether a person is currently infected or has been infected in the past.
- Viral culture: This involves collecting a sample of blood or other bodily fluid and attempting to grow the virus in a laboratory setting.
- Polymerase chain reaction (PCR): This method can detect the presence of viral DNA in a blood or tissue sample.
- Imaging tests: These may be used to detect any potential complications or abnormalities associated with EBV infection, such as enlarged lymph nodes or an enlarged spleen.
It is important to note that a positive result on one of these tests does not necessarily indicate active disease or illness, as many people have been exposed to EBV at some point in their lives and carry antibodies against the virus without experiencing symptoms.
Treatment of Epstein-Barr Virus (EBV)
Currently, there is no specific treatment available for EBV infection. Most cases of EBV infection are self-limiting and do not require any specific therapy. However, antiviral drugs such as acyclovir, ganciclovir, and valacyclovir can be used to treat severe or prolonged EBV infections. In addition, corticosteroids may be used to control symptoms such as fever and pharyngitis in patients with infectious mononucleosis.
Some alternative therapies may also be helpful in managing symptoms of EBV infection. These may include:
- Rest and adequate hydration
- Pain relievers such as acetaminophen or ibuprofen for fever and sore throat
- Gargling with salt water or using throat lozenges to relieve sore throat
- Warm compresses to relieve swollen lymph nodes
- Herbal remedies such as echinacea, licorice root, and astragalus may help boost the immune system and relieve symptoms
It is important to note that alternative therapies should not be used as a substitute for conventional medical treatment. Patients with severe or persistent symptoms should consult a healthcare provider for appropriate evaluation and management.
Prevention and Control of Epstein-Barr Virus (EBV)
- Practice good hygiene: Regular hand washing and avoiding close contact with infected individuals can help prevent the spread of EBV.
- Avoid sharing personal items: EBV can spread through contact with infected saliva, so avoid sharing personal items such as toothbrushes, utensils, and drinking glasses.
- Strengthen your immune system: A healthy immune system can help prevent EBV infection, so maintaining a healthy lifestyle, including regular exercise, a balanced diet, and getting enough sleep, can help boost immunity.
- Avoid contact sports: Avoid contact sports that may lead to bodily fluids exchange, like football and wrestling, that may increase the chances of catching EBV.
- Vaccination: While there is no vaccine available to prevent EBV infection, the hepatitis A vaccine has been shown to reduce the risk of developing infectious mononucleosis, which is often caused by EBV.
- Early diagnosis and treatment: Early detection and treatment of EBV can help reduce the severity and duration of symptoms and prevent complications.
Transmission of Epstein-Barr Virus (EBV)
- EBV is typically transmitted through bodily secretions, particularly saliva. EBV is transmitted by saliva through kissing, sharing beverages and food, using the same cups, eating utensils, or toothbrushes, and coming into contact with drooling children’s toys. The virus probably persists on a surface for as long as the surface is moist.
- EBV can spread via blood and sperm during sexual contact, blood transfusions, and organ transplants.
FAQ
What is Epstein-Barr Virus (EBV)?
EBV is a type of herpesvirus that infects human beings, and is also known as Human Herpesvirus 4 (HHV-4).
How is EBV transmitted?
EBV is primarily transmitted through contact with saliva from an infected person, either through direct contact like kissing, or through sharing objects like utensils or toothbrushes.
What are the symptoms of EBV infection?
Symptoms of EBV infection can include fatigue, fever, sore throat, swollen lymph nodes, and sometimes a rash. In some cases, EBV can also cause more severe symptoms like hepatitis or an enlarged spleen.
How is EBV diagnosed?
EBV can be diagnosed through a blood test that detects antibodies to the virus, or through a test that looks for the virus’s DNA in a sample of blood.
Is there a cure for EBV?
There is no cure for EBV, but the symptoms can be managed through rest, hydration, and over-the-counter pain relievers. In some cases, antiviral medication may also be prescribed.
Can you get EBV more than once?
While it’s rare, it is possible to get EBV more than once. However, once a person has been infected, they typically develop immunity to the virus that lasts for the rest of their life.
Are there any long-term effects of EBV infection?
In some cases, EBV infection can lead to the development of certain types of cancer, like Hodgkin’s lymphoma or nasopharyngeal carcinoma. However, this is relatively rare.
Can you prevent EBV infection?
There is no vaccine to prevent EBV infection, but certain precautions like avoiding close contact with infected individuals and not sharing personal items can help reduce the risk of transmission.
Can EBV be transmitted through blood transfusions?
Yes, EBV can be transmitted through blood transfusions, although this is rare.
Is EBV related to COVID-19?
No, EBV is not related to COVID-19. They are caused by different viruses and have different symptoms and modes of transmission.
References
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Biological Agents. Lyon (FR): International Agency for Research on Cancer; 2012. (IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, No. 100B.) EPSTEIN-BARR VIRUS. Available from: https://www.ncbi.nlm.nih.gov/books/NBK304353/
- Hoover K, Higginbotham K. Epstein Barr Virus. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559285/
- Padgett, D. A., Bailey, M. T., & Sheridan, J. F. (2007). Herpesviruses. Encyclopedia of Stress, 305–311. doi:10.1016/b978-012373947-6.00193-8
- Young, L. S. (2008). Epstein–Barr Virus: General Features. Encyclopedia of Virology, 148–157. doi:10.1016/b978-012374410-4.00391-5
- Young, L. S. (1999). EPSTEIN-BARR VIRUS(HERPESVIRIDAE) | General Features. Encyclopedia of Virology, 487–494. doi:10.1006/rwvi.1999.0086
- Hadi, Assist. Prof. Dr. Ameer & Mohammed, Shakir & Jebor, Mohammed. (2015). Molecular Study of Epstein Barr Virus, P16 and Bcl2 Gene Expression in Tissues from Nasopharyngeal Carcinoma Patients.
- https://www.creative-diagnostics.com/tag-epstein-barr-virus-antigens-15.htm
- https://aurametrix.weebly.com/topics/epstein-barr-virus
- https://labpedia.net/epstein-barr-virus-ebv-infectious-mononucleosis/
- https://www.cusabio.com/infectious-diseases/epstein-barr-virus.html