What are Anatomical Barriers?
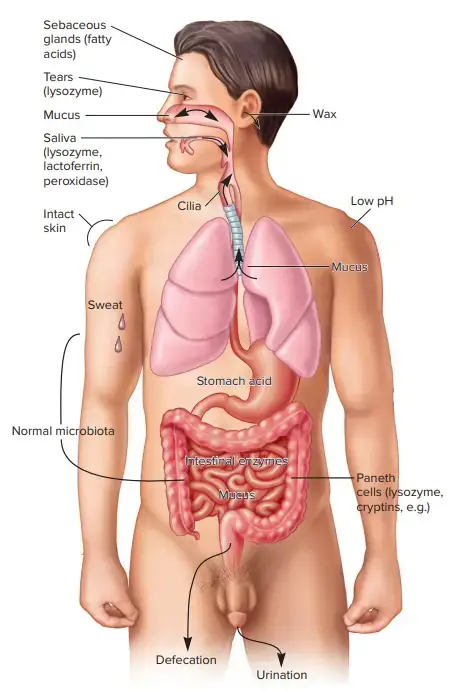
Anatomical barriers serve as the first line of defense against invading microbes or parasites, preventing them from entering the body and causing infection. These barriers consist of physical structures that organisms must attach to and penetrate before gaining entrance into the body.
Microbes or parasites can enter the body through active or passive means. Actively, they may burrow through the skin, while passively, they can be ingested through food, inhaled into the respiratory tract, or penetrate through open wounds. Regardless of the point of entry, they must overcome the external physical barriers that protect the body’s interior from the pathogens of the external environment.
The primary anatomical barriers include the skin and the mucous epithelial layers, also known as mucous membranes, which line the respiratory, gastrointestinal, and urogenital tracts, as well as the ducts of secretory glands. These barriers act like a protective shield, encapsulating and safeguarding the inner regions of the body from potential infections.
The skin and mucous membranes function as a living “plastic wrap,” creating a physical barrier that hinders the entry of pathogens. They also contribute to the body’s defense mechanisms through physical and mechanical processes. For instance, these barriers facilitate the shedding of pathogens, helping to remove them from the body’s surfaces.
Moreover, anatomical barriers actively generate chemical and biochemical defenses. They synthesize and deploy molecules that possess antimicrobial properties or induce antimicrobial activity. These active defenses aid in combating pathogens that come into contact with the skin or mucous membranes.
In summary, anatomical barriers play a crucial role in protecting the body from infections. The skin and mucous membranes form a physical barrier that prevents the entry of pathogens, while also contributing to the body’s ability to eliminate them. Additionally, these barriers produce active chemical defenses, enhancing the body’s capacity to fight against invading microbes or parasites.
What are Physiological Barriers?
Physiological barriers are natural defense mechanisms and processes within the body that help protect against infections and maintain homeostasis. These barriers are part of the body’s innate immune system and work in coordination with anatomical barriers to prevent the invasion and spread of pathogens. Unlike anatomical barriers, which are physical structures, physiological barriers encompass various biological functions and responses.
Anatomical Barriers of Immune System
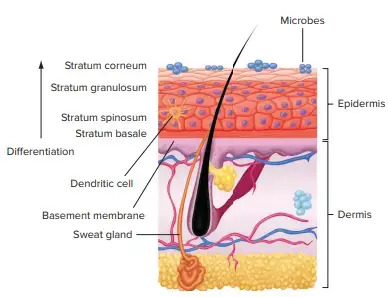
1. The Skin
- The epithelial cells of the skin are stratified and cornified (converted to keratin).
- As a highly effective mechanical barrier with accompanying microbiota, intact skin contributes significantly to the inherent resistance of the host.
- Its outer layer is composed of densely packed cells known as keratinocytes.
- These create keratins, which are insoluble proteins that make up the majority of hair, nails, and outer skin cells. These outermost skin cells continually shed.
- Sebum, a lubricating oil produced by the sebaceous glands, bathes particular regions of the skin.
- The skin’s surface is topographically, ecologically, and physiologically diverse, resulting in multiple microenvironments with varying levels of moisture, pH, temperature, and sebum.
- These niches are occupied by resident microbial communities that have adapted to flourish in the skin’s unique environment and help prevent disease colonisation.
2. Mucous Membranes
- Internal structures connected to the environment, such as the digestive, genitourinary, and respiratory tracts, are lined with mucous membranes.
- Mucous membranes, often known as mucosa, constitute a barrier that resists invasion and traps microorganisms.
- These membranes are composed of a layer of epithelial cells and a number of specialised cell types. Goblet cells, for instance, create mucus (a glycoprotein-rich aqueous fluid) that coats the membrane surface.
- Paneth cells are other specialised cells that produce antimicrobial peptides and the antibacterial enzyme lysozyme.
- Numerous germs are rendered hazardous by the presence of these chemicals in mucosal secretions such as tears and prostatic fluid.
- In addition to epithelium, goblet, and Paneth cells, three types of specialised immunological structures contain molecules and cells of both innate and adaptive immunity: Peyer’s patches, isolated lymphoid follicles, and diffuse lymphoid tissue.
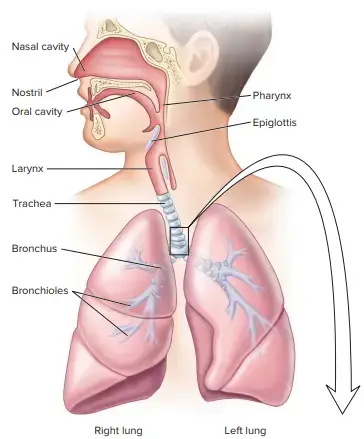
3. Respiratory System
- At least eight germs are inhaled by the average individual per minute, or 10,000 per day.
- Once breathed, a pathogen must first evade the defences of the upper and lower respiratory tract mucous membranes.
- Due to the turbulent airflow in these tracts, bacteria adhere to the moist, sticky mucosal surfaces. Microorganisms larger than 10 m are typically captured by the hairs and cilia that line the nasal canal.
- The cilia in the nasal cavity beat in the direction of the pharynx, propelling mucus containing germs toward the mouth for expulsion.
- Numerous bacteria enlarge when the nasal cavity’s air is humidified, which facilitates phagocytosis.
- Microbes smaller than 10 m (i.e., the majority of bacterial cells) are captured by the mucociliary blanket that coats the mucosal surfaces of the lower sections of the respiratory system.
- The germs are transferred from the lungs to the mouth via ciliary activity, also known as the mucociliary escalator.
- Coughing and sneezing reflexes also eliminate germs from the respiratory system. Microorganisms from the mouth and nasopharynx are washed into the stomach by salivation.
- When microorganisms reach the alveoli of the lungs, they confront a population of phagocytic cells known as alveolar macrophages. By phagocytosis, these cells consume and kill the majority of inhaled germs.
4. Gastrointestinal Tract
- The mouth and esophageal mucous membranes constitute a significant barrier to penetration.
- However, we consume thousands of germs with every snack, meal, and drink.
- There, acidic gastric secretions (pH 2 to 3) comprising a mixture of hydrochloric acid, proteolytic enzymes, and mucus kill several individuals.
- Nevertheless, certain microbes and their products (such as protozoan cysts, Helicobacter pylori, Clostridium spp., and staphylococcal toxins) can survive stomach acidity. In addition, microorganisms encased in food particles may be shielded and enter the small intestine.
- There, these microbes may be harmed by pancreatic enzymes, bile, intestinal enzymes, and cells and chemicals in the gut-associated lymphoid tissue (GALT).
- Peristalsis (Greek: ; stalsis: contraction) and the natural shedding of columnar epithelial cells work in tandem to eliminate intestinal bacteria.
- Human health and equilibrium depend on the bacteria that inhabit the GI tract.
- These bacteria are necessary for the maturity and proper function of the immune system. Additionally, gut microbes inhibit the development of prospective pathogens.
5. Genitourinary Tract
- A complicated collection of factors maintains the kidney, ureters, and urine bladder’s natural sterility.
- In addition to eliminating microorganisms by flushing, urine kills some bacteria due to its low pH, urea, and other metabolic end products (e.g., uric acid, fatty acids, mucin, enzymes).
- The anatomical length of the urethra in males (20 cm) offers a barrier that prevents bacteria from entering the urine bladder.
- This explains why women are four times more prone than men to have a urinary tract infection due to the shorter urethra in females (5 cm).
- The vagina’s innate defence is mostly composed of the normal microbiota and the protective mechanisms given by the mucous membrane.
- Lactobacillus spp. dominate nonpregnant women’s vaginal microbiome. These bacteria produce an acidic environment that is hostile to pathogens.
- Cervical mucus contains defensins, lysozyme, lactoferrin, and natural antimicrobial peptides with antibacterial activity.
Physiological barriers of immune system
Temperature, pH, and numerous soluble and cell-associated chemicals comprise the physiologic barriers that contribute to innate immunity.
1. Body temperature
- Due to the fact that their regular body temperature prevents the growth of germs, numerous species are immune to specific diseases.
- Normal body temperature of 37oC inhibits the growth of some microorganisms, but body temperature, particularly fever, limits or stops the growth of numerous microorganisms, particularly viruses.
- Additionally, the immunological response is more effective at higher body temperatures.
- For instance, chickens are naturally resistant to anthrax because their high body temperature prevents the growth of the bacteria.
2. pH
- Numerous viruses and bacteria are rendered inactive by the acidic conditions of the stomach, bladder, and kidneys, as well as the bile of the intestines. The low pH environment caused by acid production protects many tissues of the body.
- Numerous organisms in the skin convert lipids into free fatty acids, hence adding to the acidity of the skin (pH 5.5).
- Due to the acidity imparted by gastric HCl, the majority of microorganisms in the stomach are inhibited by gastric acidity (pH 1-3).
- Most pathogens are inhibited by the low pH of the female genital tract, which is approximately 4.4 due to the presence of lactic acid-producing bacteria (normal flora).
3. Secretory products of the mucosa
- Bile salts: Bile salts disrupt the bacterial cell membrane, resulting in cell death. Bile salts are cytotoxic and bacteriostatic.
- Fatty acids: Fatty acids denature bacterial proteins and provide an acidic environment that inhibits bacterial growth.
- Sebum: Sebum generates a protective acid coating on the surface of the skin, which inhibits the growth of numerous microorganisms.
- Saliva and Mucus: Enzymes in saliva degrade the cell wall and cell membrane of bacteria in saliva and mucus.
- Spermine and zinc: Spermine and zinc Spermine and zinc suppress the growth of gram-positive bacteria in sperm.
- Lactoferrin: Lactoferrin, which is abundant in numerous secretory fluids such as milk, saliva, tears, and nasal secretions, binds to iron and so prevents bacteria from acquiring iron.
- Colostrum: Colostrum contains immunoglobulins and lactoferrins that inhibit the multiplication and development of bacteria.
- Lysozyme: Tears include lysozyme, which dissolves the peptidoglycan layer in the bacterial cell wall, resulting in the lysis of the bacteria. Continuous rinsing of the eye with lysozyme-containing tears reduces the growth of bacteria in the eye.
- Gastric juice: The HCI present in gastric juice destroys microorganisms due to its low pH.
- Trypsin: Trypsin hydrolyzes bacterial proteins, resulting in cell death.
4. Other Barriers of Immune System
- Peristalsis: Intestinal microbes are entrapped in mucus or other materials present in the intestine by the gradual and rhythmic contraction of peristalsis, and then expelled from the body.
- Urination: The somewhat acidic urine flushes the urinary system and helps keep it sterile.
- Coughing and Sneezing: Reflexes like coughing and sneezing help rid the body of trapped organisms by releasing them.
- Diarrhea and Vomiting: Another way the body rids itself of an infectious agent or material is through diarrhoea and vomiting.
FAQ
What are anatomical barriers of the immune system?
Anatomical barriers refer to physical structures and mechanisms that prevent the entry of pathogens into the body. Examples include the skin, mucous membranes, and the epithelial linings of the respiratory, digestive, and genitourinary tracts.
How does the skin act as a barrier?
The skin acts as a physical barrier due to its outer layer, the epidermis, which consists of tightly packed cells that prevent pathogens from entering. Additionally, the skin produces antimicrobial substances and has a slightly acidic pH that inhibits the growth of microbes.
What are mucous membranes and how do they act as barriers?
Mucous membranes line the respiratory, digestive, and genitourinary tracts. They secrete mucus, which traps pathogens and other foreign substances. Mucus also contains antimicrobial components that help prevent infection.
What is the role of cilia in the respiratory tract?
Cilia are hair-like structures present in the respiratory tract. They move in coordinated waves and help to sweep mucus, along with trapped pathogens and debris, out of the respiratory system, preventing them from reaching the lungs.
How do tears and saliva contribute to immune defense?
Tears and saliva contain antimicrobial enzymes, such as lysozyme, that can kill or inhibit the growth of bacteria. They also help to wash away pathogens from the eyes and mouth.
What is the role of stomach acid in immune defense?
The stomach produces hydrochloric acid, which creates an acidic environment that helps to destroy ingested pathogens. It acts as a barrier against pathogens that enter the body through the digestive system.
How do beneficial bacteria in the body contribute to immune defense?
Beneficial bacteria, known as commensal bacteria, colonize various parts of the body, such as the skin, digestive tract, and vagina. They help to maintain a healthy microbial balance, preventing the overgrowth of harmful pathogens.
What is the role of mucus and cilia in the respiratory tract?
Mucus traps pathogens and particles, preventing them from reaching the lungs. Cilia, small hair-like structures, move in coordinated motions to transport the mucus along with trapped pathogens out of the respiratory system.
What are antimicrobial peptides, and how do they contribute to immune defense?
Antimicrobial peptides are small proteins produced by various cells of the immune system and other tissues. They have broad-spectrum antimicrobial activity and can directly kill pathogens or disrupt their growth.
How does the blood-brain barrier protect the central nervous system?
The blood-brain barrier is a specialized barrier formed by tight junctions between cells lining the blood vessels in the brain. It limits the passage of substances, including pathogens, from the bloodstream into the brain, protecting the central nervous system from infection.
References
- Owen, J. A., Punt, J., & Stranford, S. A. (2013). Kuby Immunology (7 ed.). New York: W.H. Freeman and Company.
- Parija S.C.(2012). Textbook of Microbiology & Immunology.(2 ed.). India: Elsevier India.
- Brooks, G. F., Jawetz, E., Melnick, J. L., & Adelberg, E. A. (2010). Jawetz, Melnick, & Adelberg’s medical microbiology. New York: McGraw Hill Medical.
- Lydyard, P.M., Whelan,A.,& Fanger,M.W. (2005).Immunology (2 ed.).London: BIOS Scientific Publishers.
- Sastry A.S. & Bhat S.K. (2016). Essentials of Medical Microbiology. New Delhi : Jaypee Brothers Medical Publishers.