What is Urinary Tract Infection (UTI)?
An illness affecting a portion of the urinary tract—that which comprises the kidneys, ureters, bladder, and urethral—is known as a urinary tract infection (UTI). Following are some salient features of urinary tract infections:
- There are several forms of urinary tract infections (UTIs), occurring in different sections of the urinary system. Bladder infections, often known as cystitis, are the most often occurring kind that targets the bladder. Other regions can also be affected by infections including the kidneys (pyelonephritis), ureters, and urethra.
- Bacteriuria is the condition whereby the urine contains bacteria. In pure culture, 105 or more organisms per millilititer (108/1) makes it noteworthy.
- Usually presenting with symptoms including frequent urination, pain or discomfort during urination (dysuria), suprapubic pain, and commonly pus in the urine (pyuria), is cystitis. In rare situations hematuria—that is, blood in the urine—may also develop.
- Even in cases when normal urine culture does not reveal any bacteria, the phrase “acute urethral syndrome” is used to characterise the symptoms of acute cystitis coupled with pyuria.
- An infection of the kidneys is called pyelonephritis. It can produce symptoms like pyuria, loin pain—that is, side or lower back pain—bacteremia, fever, and even bloodstream bacterial infection.
- Most UTIs are brought on by uropathogenic organisms colonizing the periurethral mucosa. Usually starting in the stomach or vaginal flora, these organisms can climb the urethral path to the bladder and other areas of the urinary system.
- Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis, Enterococcus faecalis, and Staphylococcus saprophyticus are the most often found common bacteria connected to urinary tract infections. Still, the particular causal organism might change based on the person and other circumstances.
- Prevalence worldwide: Affecting around 150 million persons annually, UTIs are a major public health concern globally. The great frequency underlines the need of correct diagnosis, treatment, and UTi prevention.
- Untreated UTIs can cause pain and could result in problems. Managing and avoiding UTIs depends critically on prompt medical care, suitable antibiotic treatment, and preventative actions like excellent cleanliness and regular fluid intake.
Types of Urinary Tract Infection (UTI)
UTIs can attack various urinary system segments, causing varied symptoms. Types of UTIs and their symptoms:
- Kidney Infection (Pyelonephritis)– Infection of the kidneys is called pyelonephritis.
- Kidney infection symptoms include:
- Side/back soreness (typically below ribcage)
- High fever
- Shake and chill
- Nausea, vomiting
- Kidney infection symptoms include:
- Bladder Infection (Cystitis)– Most UTIs are bladder infections (cystitis).
- Cystitis symptoms include:
- Pelvic stress
- Lower abdominal ache
- Urinating often
- Dysuria—urination pain or burning
- Hematuria (blood in urine)
- Cystitis symptoms include:
- Urethral Infection (Urethritis)- The urethra, which carries urine, is infected.
- Urethritis symptoms include:
- Dysuria—urination discomfort or burning
- Urethral discharge
- Urethritis symptoms include:
Causative Agents of UTI
Several bacteria and fungus can lead to urinary tract infections (UTIs). The following is some knowledge on the UTI causal agents:
- The most often occurring causal agent of both simple and serious urinary tract infections is Escherichia coli (E. coli). Usually present in the gastrointestinal system, this Gram-negative bacteria can also reach the urinary tract and cause an infection.
- Other Bacteria in Simple UTIs: Other bacteria typically linked to simple UTIs follow UPEC and include:
- pneumoniae Klebsiella
- Staphylococcus saprophyticus
- Group B Enterococcus faecalis GBS, or Streptococcus
- Proteus mirabilis is a
- Aeruginosa pseudo mononas
- Aureus Staphylococcus
- In Complicated UTIs, causative agents: With UPEC the most often occurring causal agent in complex UTIs, their frequency follows a similar trend to that of simple UTIs. Other species sometimes linked to complex UTIs include:
- Enterococcus species here.
- Klebsiella pneumoniae
- species of candida, or fungus
- Staphylococcus aureus.
- Proteus Mirabilis
- Aeruginosa Pseudomonas
- Group A Streptococcus GBS
- Usually equal to or more than 10^5 colony-forming units per millilititer (CFU/ml), UTIs are caused by a single bacterium present in high concentration. This great concentration points more toward an illness than towards pollution.
- While a single organism generally causes UTIs, polymicrobial infections—involving more than one microorganism—can strike people with anatomical anomalies or foreign substances in the urinary system. Multiple species in a culture might, however, also point to colonization or cultural contamination; so, much care is required to separate actual infection from alternative causes.
Risk factors of UTI
There are a number of things that can make getting a urinary tract infection (UTI) more likely. Here are some important things that put you at risk for getting a UTI:
- Gender: Women are more likely than men to get urinary tract infections. The urethras of women are shorter than those of men, which makes it easier for bacteria to get into the urine system from the rectal area.
- Previous UTI: If you’ve had a UTI before, you’re more likely to get another one.
- Sexual Activity: Having sex can bring germs into the bladder, which raises the risk of getting a UTI. Women are more likely than guys to be at this risk.
- Changes in Vaginal Flora: UTIs are more likely to happen to people who have changes in the vaginal flora, which are the germs that live naturally in the vagina. The balance of vaginal bacteria can be thrown off by things like puberty, using spermicides, or changes in hormones.
- Pregnancy– Women who are pregnant are more likely to get UTIs because their hormones change and their growing uterus puts pressure on their urinary stream.
- Age: People of certain ages are more likely to get UTIs. Older adults and young children are more likely to get it because their immune systems are weaker or they have trouble keeping themselves clean.
- Problems with the structure: Issues with the structure of the urinary system, like a male’s enlarged prostate, can make it hard for pee to move normally and lead to UTIs.
- Poor Hygiene: Bacteria can get into the urine stream more easily if people don’t clean themselves properly, especially kids who are learning to use the potty.
Symptoms of UTI
The symptoms of urinary tract infections (UTIs) vary according on the urinary tract region that is impacted. The following are typical signs of urinary tract infections:
Symptoms of a bladder infection:
- Dysuria, or pain or burning during urinating
- Urinating a lot
- urge to urinate despite not having a full bladder
- Blood in the pee, or hematuria
- Lower abdominal or groin pressure or cramps
Symptoms of a kidney infection:
- Fever chills
- Pain on the side of the back or lower back
- Vomiting or feeling queasy
It’s crucial to remember that younger kids could find it hard to communicate their symptoms. Fever, however, is the most typical symptom of UTIs in young children. Since the majority of children who have a fever do not have a UTI, it is important to see a doctor if you think your kid may have one.
Pathogenesis of UTI
UTIs are caused by bacteria entering the urine system, attaching to the bladder wall, and infecting. Here are some UTI pathogenesis steps:
- Entry of Bacteria – The urethra is the main pathway for germs into the urinary system. The circulation or lymphatic system can potentially carry germs to the urinary tract. Due to the closeness of the urethra to the anus, females are more likely to get UTIs from gut bacteria.
- Attachment to the Bladder Wall – Bacteria can adhere to the bladder wall once they reach there. Bacterial surface processes and sticky structures aid adhesion. This adhesion permits the germs to resist being washed away during urine.
- Biofilm Formation- Many UTI-causing bacteria create biofilms on bladder walls after adhesion. Biofilms are complex structures made of bacteria and polysaccharides and proteins. The biofilm shields germs from the human immune response and renders them antibiotic-resistant, making infection removal difficult.
- Infection and Symptoms – Bacteria in the bladder and biofilm development cause immune system inflammation. Localized inflammation from this immune response can produce pain, frequent urination, and bladder discomfort. Untreated infection can move to the kidneys, worsening symptoms and consequences.
Diagnosis of UTI
Urinary tract infections (UTIs) are diagnosed by assessing the symptoms of the patient and running particular diagnostic investigations. Here is some information about the diagnosis of UTIs:
- simple UTI Diagnosis: In situations of simple UTIs, an accurate diagnosis may typically be obtained based on usual symptoms alone. Urinalysis and urine culture are not frequently needed, and patients may be treated empirically without additional testing.
- Diagnostic Tests for Complicated UTI – Diagnostic tests including urinalysis and urine culture should be conducted for suspected complex UTIs, or when pyelonephritis (kidney infection) is present.
- Urinalysis: Urinalysis can be done using a dipstick or microscopic examination of the urine sample. Positive findings for leukocyte esterase and nitrite responses on the dipstick suggest the presence of infection. Common findings are proteinuria and hematuria (presence of blood in the urine), and most UTI sufferers have pyuria, or white blood cells in the urine.
- Gram Stain: Gram staining of urine samples may be useful in detecting significant bacterial growth. However, its sensitivity is restricted and it is not suggested for routine usage in urine specimens.
- Routine urine culture – Routine urine culture is the method of objectively evaluating bacterial growth by spreading a urine sample onto agar plates. Usually speaking, the lowest limit of detection is 10^3 colony-forming units per millilititer (cfu/mL). The level of subsequent testing, such as identification and susceptibility testing, relies on criteria such as the kind of material, the number of species isolated, and the pathogenic potential of the isolates.
- Culture for Possible complex UTI: For individuals at risk of complex UTI, such as those with symptoms and lesser bacterial numbers (<10^3-10^4 cfu/mL), culture methods utilizing a 10-microliter inoculum can identify substantial infections. The degree of workup follows comparable standards applied in standard cultures.
- Other Laboratory Testing: Based on the clinical presentation, more or less suitable laboratory testing is advised. Women with simple urinary tract infections could be advised pregnancy testing. Patients with complex UTIs who show symptoms of systemic infection—such as fever, hypotension, or sepsis—should get blood cultures.
Treatment of UTI
The primary approach to treating urinary tract infections (UTIs) involves the use of antibiotics. Here is some information about the treatment of UTIs:
- Uncomplicated and Complicated UTIs: For uncomplicated UTIs, the first-line treatment is typically oral trimethoprim. If trimethoprim is contraindicated or not suitable, oral nitrofurantoin can be used as a second-line option. In pregnancy, oral cephalexin is often prescribed.
- Pyelonephritis (Kidney Infection): Pyelonephritis, which is a more severe form of UTI involving the kidneys, usually requires intravenous (IV) antibiotics. The first-line treatment is IV co-amoxiclav (a combination of amoxicillin and clavulanic acid) along with IV gentamicin. If the first-line treatment is not suitable, oral or IV ciprofloxacin in combination with IV gentamicin can be used as a second-line option. In pregnancy, IV cefuroxime is often administered.
- Urethral Syndrome: Urethral syndrome, which is characterized by symptoms of dysuria and pyuria but without the presence of bacteria, does not respond well to antibiotics. The primary treatment approach for urethral syndrome is to increase fluid intake to flush out bacteria from the urethra.
- Complicated UTIs: Complicated UTIs are more challenging to treat and often require a more aggressive evaluation, treatment, and follow-up. The underlying complication contributing to the UTI needs to be identified and addressed along with appropriate antibiotic therapy.
- Concerns of Antibiotic Resistance: Increasing antibiotic resistance is a significant concern in the treatment of complicated and recurrent UTIs. It is important to monitor and address antibiotic resistance patterns to ensure effective treatment options are available in the future.
Treatment of Urinary Tract Infections with D-Mannose
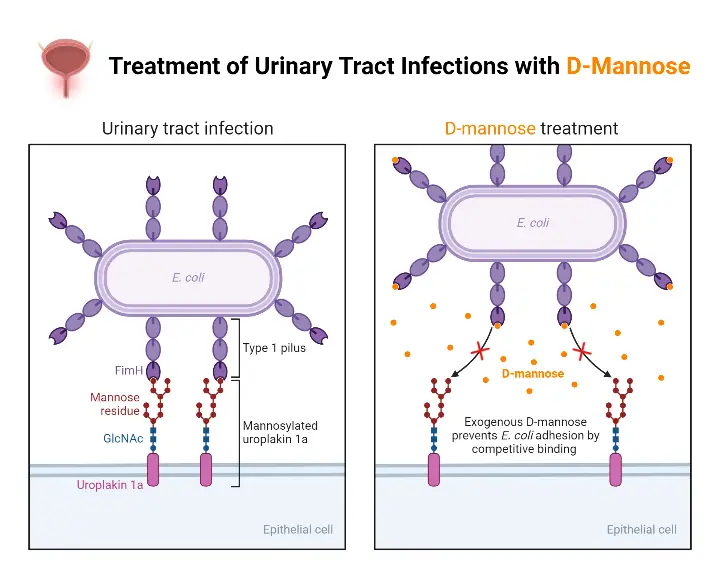
D-Mannose is a type of sugar that is commonly used as a natural remedy for urinary tract infections (UTIs). It is believed to work by preventing bacteria from attaching to the walls of the urinary tract and flushing them out of the body. Here’s some information about the treatment of UTIs with D-Mannose:
- Mechanism of action: UTIs are primarily caused by the colonization of bacteria, typically Escherichia coli (E. coli), in the urinary tract. D-Mannose is a simple sugar that is not metabolized by the body and is excreted through the urinary system. It is thought that D-Mannose attaches to the E. coli bacteria, preventing them from binding to the urinary tract walls, allowing them to be flushed out during urination.
- Effectiveness: D-Mannose has gained popularity as a natural remedy for UTIs, and some people report positive results. However, the scientific evidence supporting its effectiveness is limited. There have been a few small-scale studies and anecdotal reports suggesting that D-Mannose may help prevent or treat UTIs. Further research is needed to establish its true efficacy.
- Usage: D-Mannose is available as a supplement in the form of powder or capsules. The typical recommended dosage for treating UTIs is 1 to 2 grams of D-Mannose taken every few hours, followed by a maintenance dose of 0.5 to 1 gram taken once or twice daily. It is essential to follow the instructions provided by the manufacturer or consult with a healthcare professional for proper dosage and usage.
- Safety: D-Mannose is generally considered safe with minimal side effects. It is well-tolerated by most individuals, and there are no known drug interactions. However, it is a sugar, so people with diabetes should be cautious and monitor their blood sugar levels when using D-Mannose. As with any supplement or medication, it is recommended to consult with a healthcare professional before starting D-Mannose, especially if you have any pre-existing medical conditions or are taking other medications.
- Limitations: D-Mannose may be more effective in preventing UTIs rather than treating active infections. It is not considered a substitute for conventional antibiotic treatment in severe or recurrent UTIs. If you suspect you have a UTI, it is essential to seek medical attention for diagnosis and appropriate treatment. Your healthcare provider can determine the most suitable course of action based on your individual circumstances.
Animation Video
Prophylaxis and Prevention of UTI
Prophylaxis and prevention strategies are important in reducing the risk of urinary tract infections (UTIs). Here is some information on UTI prophylaxis and prevention:
- Prophylactic Antibiotics: In children with recurrent UTIs, prophylactic antibiotics may be prescribed to prevent further infections and protect renal function. The use of prophylactic antibiotics should be guided by a healthcare professional.
- Hydration: Staying well hydrated is crucial in preventing UTIs. Drinking plenty of fluids, especially water, helps dilute urine and promotes frequent urination. This helps flush out bacteria from the urinary tract before an infection can develop.
- Urination After Sexual Activity: Emptying the bladder soon after sexual activity can help flush out bacteria that may have entered the urethra during intercourse. Additionally, drinking a full glass of water after sexual activity can further assist in flushing out bacteria.
- Personal Hygiene: Practicing good personal hygiene can reduce the risk of UTIs. Here are some recommendations:
- Wipe from front to back after urinating and after a bowel movement to prevent the spread of bacteria from the anus to the urethra and vagina.
- Minimize the use of potentially irritating feminine products such as deodorant sprays, douches, and powders, as they can irritate the urethra.
- Showering Instead of Bathing: Taking showers instead of baths can help reduce the risk of UTIs. Baths can increase the likelihood of bacteria entering the urethra, while showers promote better hygiene and reduce the chance of bacterial contamination.
- Consider Cranberry Juice: While the evidence on cranberry juice preventing UTIs is not conclusive, it is generally considered safe to consume and may have some benefit. Drinking cranberry juice may help inhibit bacterial adherence to the urinary tract, potentially reducing the risk of infection.
- Birth Control Methods: Certain birth control methods, such as diaphragms, unlubricated condoms, or condoms treated with spermicide, can contribute to bacterial growth. If recurrent UTIs are an issue, discussing alternative birth control options with a healthcare professional may be beneficial.
FAQ
What is a urinary tract infection (UTI)?
A urinary tract infection is an infection that affects any part of the urinary system, including the kidneys, bladder, ureters, and urethra.
Can UTIs be prevented?
While UTIs cannot always be prevented, there are steps you can take to reduce the risk. These include staying hydrated, urinating after sexual activity, practicing good hygiene, avoiding irritating products in the genital area, and considering cranberry juice or supplements.
Who is at a higher risk of developing UTIs?
Women are more prone to UTIs due to their shorter urethra, which allows bacteria to reach the bladder more easily. Other risk factors include sexual activity, menopause, urinary tract abnormalities, catheter use, weakened immune system, and certain medical conditions.
How are UTIs diagnosed?
UTIs are typically diagnosed based on symptoms, a physical examination, and a urine sample analysis. Urinalysis and urine culture may be conducted to confirm the presence of bacteria and determine the specific type of bacteria causing the infection.
What is the treatment for a UTI?
The mainstay of UTI treatment is antibiotics prescribed by a healthcare professional. The specific antibiotic and duration of treatment depend on the type and severity of the infection. It is important to complete the full course of antibiotics as prescribed.
Can UTIs be recurrent?
Yes, UTIs can recur, especially in individuals with risk factors such as urinary tract abnormalities, frequent sexual activity, or a history of UTIs. Recurrent UTIs may require further evaluation and management by a healthcare professional.
Are there any complications associated with UTIs?
If left untreated or inadequately treated, UTIs can potentially lead to more serious complications, such as kidney infections (pyelonephritis), bloodstream infections (sepsis), and recurrent infections.
What are the common symptoms of a UTI?
Common symptoms of a UTI may include frequent urination, pain or burning sensation during urination, cloudy or bloody urine, strong-smelling urine, pelvic pain, and a feeling of urgency to urinate.
Can men get UTIs?
Although less common, men can also develop UTIs. In men, UTIs are often associated with underlying urinary tract abnormalities, such as an enlarged prostate or urinary stone.
When should I seek medical attention for a suspected UTI?
If you experience symptoms of a UTI, it is recommended to seek medical attention. Prompt diagnosis and treatment can help alleviate symptoms and prevent potential complications.
References
- https://www.mayoclinic.org/diseases-conditions/urinary-tract-infection/symptoms-causes/syc-20353447
- https://www.cdc.gov/antibiotic-use/uti.html
- https://my.clevelandclinic.org/health/diseases/9135-urinary-tract-infections
- https://www.urologyhealth.org/urology-a-z/u/urinary-tract-infections-in-adults
- https://www.nhsinform.scot/illnesses-and-conditions/kidneys-bladder-and-prostate/urinary-tract-infection-uti
- https://www.niddk.nih.gov/health-information/urologic-diseases/bladder-infection-uti-in-adults
- https://www.webmd.com/women/your-guide-urinary-tract-infections
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/urinary-tract-infections-uti
- https://www.nhs.uk/conditions/urinary-tract-infections-utis/
- https://www.healthline.com/health/urinary-tract-infection-adults