What is Glycogen?
- Glycogen, a crucial component in the realm of biological energy storage, serves as a glucose polymer fundamental for various organisms. This intricate macromolecule is comprised of numerous glucose units connected through a series of chemical linkages, resulting in a vast structure containing thousands of glucose residues. The structure of glycogen is characterized by the presence of two distinct types of linkages, giving rise to its branched polymeric architecture. It’s noteworthy that these same linkages can be observed in plant starches, which perform a comparable function to glycogen.
- Glycogen’s paramount function is as a reservoir of glucose that can be readily accessed when the need arises. This storage of glucose as glycogen offers certain advantages, primarily due to the lower osmotic activity of the polymer compared to free glucose monomers. Additionally, some minor constituents of glycogen, such as covalently attached phosphate groups, play a role in its overall structure and function.
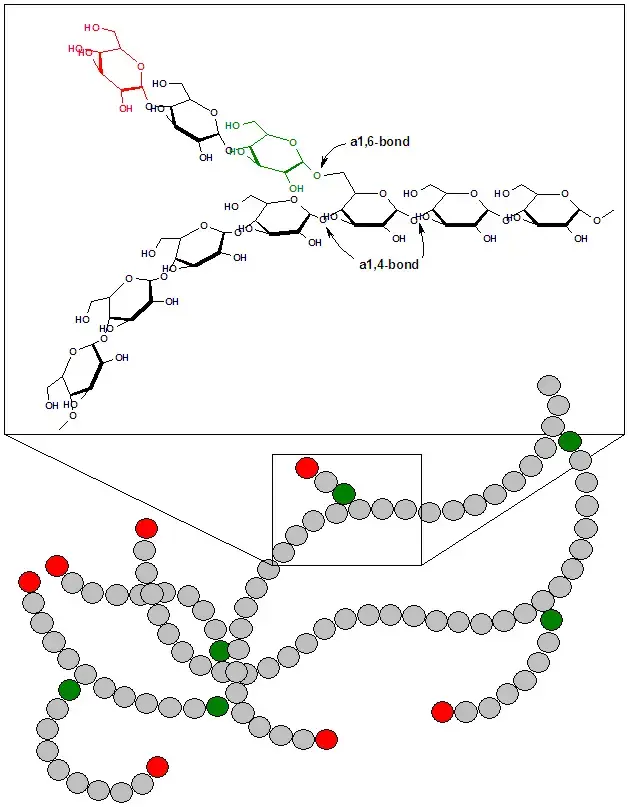
- The structural composition of glycogen is marked by its status as a branched homopolymer of glucose molecules. The majority of glucose residues are interconnected by α 1→4 linkages, creating linear chains of glucose units. However, a unique feature of glycogen is the presence of α 1→6 bonds, which connect every twelfth glucose residue to the next, resulting in branching points within the glycogen molecule. These branches are further extended by the addition of glucose residues connected by α 1→4 linkages, resembling the structure of tree branches. All enzymatic reactions involved in glycogen metabolism occur exclusively at the “non-reducing ends” of the molecule, which can be either shortened or lengthened as needed.
- In the context of animals, glycogen functions as a vital “carbohydrate storehouse.” It provides a means to release glucose when necessary, achieved through enzymatic cleavage of the glycogen structure. In the cytoplasm of virtually all cells, one can find highly hydrated glycogen granules, signifying its ubiquitous presence in the body. The human body, in particular, can store approximately 450 grams of glycogen. The liver houses a substantial portion of this reserve, containing 80-100 grams, commonly referred to as liver glycogen. The liver glycogen plays a crucial role in maintaining a constant level of glucose in the bloodstream, known as glycemia.
- The remaining 300 grams of glycogen are primarily found in muscle cells, termed muscle glycogen. Muscle glycogen serves as an essential internal energy reserve during periods of increased muscle activity. Notably, muscle cells lack the enzyme glucose-6-phosphatase, which means they cannot release pure glucose directly into the bloodstream. The remaining approximately 50 grams of glycogen are distributed among other cells throughout the human body, serving as a localized source of glucose when required.
Structure And Function Of Glycogen
The primary stores of glycogen within the human body are primarily located in skeletal muscle and the liver, although various other cells also maintain smaller glycogen reserves for their specific metabolic needs. The role of glycogen varies depending on its location, and it plays crucial functions in maintaining energy balance and glucose homeostasis.
- Muscle Glycogen Function: Muscle glycogen serves as a critical fuel reserve, particularly during periods of high-energy demand, such as muscle contraction. Its primary role is to facilitate the synthesis of adenosine triphosphate (ATP), a molecule vital for cellular energy transfer. This ensures that muscles have a readily available energy source during physical activity.
- Liver Glycogen Function: Liver glycogen, on the other hand, plays a pivotal role in regulating blood glucose concentration, especially during the early stages of fasting. It acts as a buffer, releasing glucose into the bloodstream to maintain glucose levels and support the energy needs of the body. Liver glycogen can effectively sustain blood glucose levels for a significant period, typically ranging from 10 to 18 hours.
Now, let’s delve into the quantitative aspects and structural intricacies of glycogen:
A. Amounts of Liver and Muscle Glycogen: The quantities of glycogen stored in liver and muscle tissues have distinctive characteristics. In resting muscle, approximately 400 grams of glycogen account for about 1% to 2% of its fresh weight. In a well-fed adult liver, around 100 grams of glycogen constitute up to 10% of its fresh weight. It’s essential to note that factors limiting glycogen production at these levels are not entirely clear. In certain glycogen storage diseases (GSDs), the liver and muscle may exhibit significantly higher glycogen levels. Notably, the total body mass of muscle surpasses that of the liver, leading to the majority of the body’s glycogen being housed in muscle tissues.
B. Structure of Glycogen: Glycogen is a branched-chain polysaccharide composed exclusively of α-D-glucose molecules. The primary glycosidic bond holding these glucose units together is the α(1→4) linkage. After approximately eight to ten glucosyl residues, a branch containing an α(1→6) linkage emerges, creating a branched structure (Figure 11.3). A single glycogen molecule can attain a substantial molecular weight of up to 108 Da. These polymers of glucose exist in discrete cytoplasmic granules within cells, which also harbor the necessary enzymes for glycogen synthesis and degradation.
C. Fluctuation of Glycogen Stores: Glycogen stores in the liver experience variations in response to the fed and fasting states. During well-fed conditions, liver glycogen stores increase, while fasting leads to their depletion. Muscle glycogen, however, remains largely unaffected by short-term fasting, even for a few days, and is only moderately reduced during prolonged fasting spanning weeks. Muscle glycogen plays a dynamic role, continuously undergoing synthesis and degradation processes to replenish stores after strenuous exercise or other metabolic demands. The interplay between the rates of glycogen synthesis and degradation largely determines the levels of stored glycogen during specific physiological states.
In summary, the structural complexity of glycogen, its distinctive distribution in the body, and its dynamic role in energy regulation highlight its critical importance in biological processes, allowing for the efficient utilization of glucose and the maintenance of vital physiological functions.
Synthesis Of Glycogen (Glycogenesis)
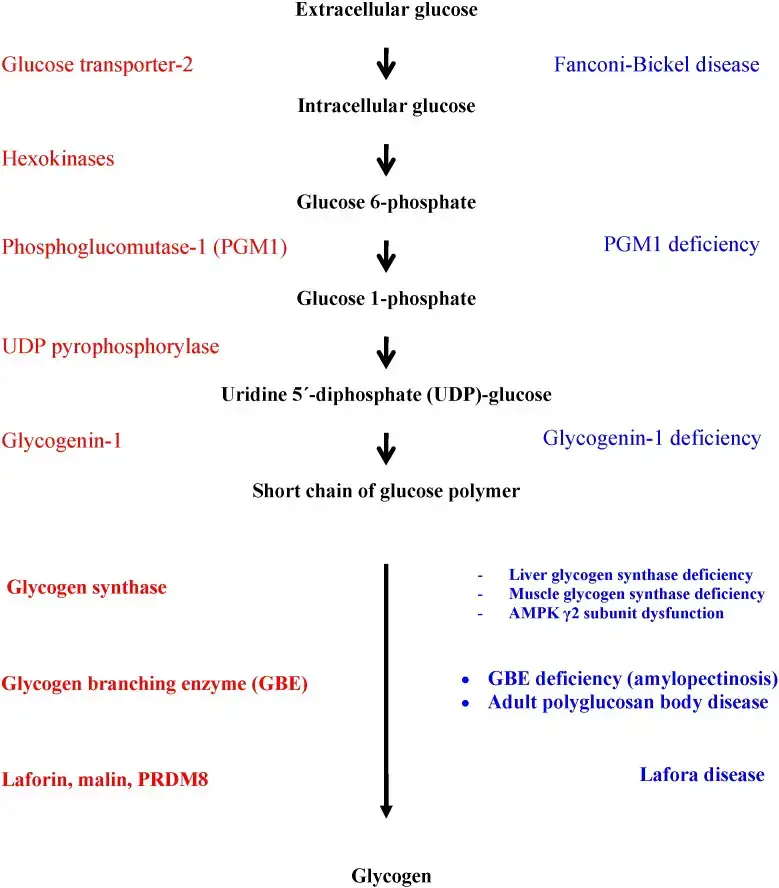
Glycogen, a fundamental energy storage molecule, is synthesized through a well-orchestrated process known as glycogenesis. This process occurs in the cytosol of cells and necessitates the input of energy supplied by adenosine triphosphate (ATP) and uridine triphosphate (UTP). Let’s delve into the sequential steps of glycogen synthesis:
A. Synthesis of Uridine Diphosphate Glucose (UDP-Glucose):
- The precursor of all glucosyl residues added to the growing glycogen molecule is α-D-glucose attached to uridine diphosphate (UDP).
- UDP-glucose is the product of a synthesis reaction involving glucose 1-phosphate and UTP, catalyzed by UDP-glucose pyrophosphorylase. This reaction also produces pyrophosphate (PPi), which is hydrolyzed into two inorganic phosphates (Pi) by pyrophosphatase.
- The exergonic nature of this reaction ensures the production of UDP-glucose from glucose 1-phosphate and UTP. Notably, glucose 1-phosphate is generated from glucose 6-phosphate via phosphoglucomutase, with glucose 1,6-bisphosphate acting as an obligatory intermediate in this reversible reaction.
B. Synthesis of a Primer to Initiate Glycogen Synthesis:
- Glycogen synthase, the enzyme responsible for forming α(1→4) linkages in glycogen, cannot initiate chain synthesis using free glucose as an acceptor of glucose molecules from UDP-glucose.
- Instead, glycogen synthase requires a primer to extend existing chains. This primer can be a fragment of glycogen, especially in cells with non-depleted glycogen stores.
- In the absence of a glycogen fragment, a protein called glycogenin can serve as an acceptor for glucose residues from UDP-glucose. Specifically, the side-chain hydroxyl group of a specific tyrosine in glycogenin serves as the attachment site for the initial glucosyl unit.
- Glycogenin catalyzes the transfer of the next few glucose molecules from UDP-glucose, generating a short α(1→4)-linked glucosyl chain that serves as a primer for glycogen synthesis. Glycogenin remains associated with and forms the core of a glycogen granule.
C. Elongation of Glycogen Chains by Glycogen Synthase:
- Glycogen synthase plays a pivotal role in extending glycogen chains. This enzyme transfers glucose from UDP-glucose to the nonreducing end of the growing chain, forming a new glycosidic bond between the anomeric hydroxyl group of carbon 1 of the activated glucose and carbon 4 of the accepting glucosyl residue.
- The enzyme facilitates the formation of α(1→4) linkages within glycogen. It’s important to note that the UDP released in this reaction can be phosphorylated to UTP by nucleoside diphosphate kinase, illustrating the dynamic nature of these reactions.
D. Formation of Branches in Glycogen:
- Unlike unbranched compounds like amylose found in plant tissues, glycogen has a highly branched, tree-like structure. On average, branches in glycogen occur every eight glucosyl residues, enhancing its solubility and efficiency.
- The formation of branches is orchestrated by the branching enzyme, amylo-α(1→4)→α(1→6)-transglucosidase. This enzyme catalyzes the removal of a set of six to eight glucosyl residues from the nonreducing end of the glycogen chain and attaches them to a non-terminal glucosyl residue via an α(1→6) linkage, thus acting as a4:6 transferase.
- The new nonreducing end formed and the old nonreducing end from which the glucosyl residues were removed can both be further extended by glycogen synthase.
- This branching process greatly enhances the rate of glycogen synthesis and contributes to the substantial size and solubility of glycogen molecules.
In summary, glycogenesis is a highly regulated and energy-dependent process that results in the formation of glycogen, a critical energy reserve used for ATP synthesis in muscle and as a glucose buffer in the liver, ensuring energy balance and glucose homeostasis in the body.
Degradation Of Glycogen (Glycogenolysis)
Glycogenolysis, the process of breaking down glycogen into glucose for energy utilization, is a well-orchestrated series of enzymatic reactions distinct from glycogenesis. Glycogenolysis primarily occurs in the liver and skeletal muscle, involving cytosolic enzymes that play a pivotal role in releasing glucose in the form of glucose 1-phosphate and free glucose.
- Shortening of Chains: The initial step in glycogenolysis involves the sequential cleavage of α(1→4) glycosidic bonds connecting glucosyl residues at the nonreducing ends of glycogen chains. This process is executed by glycogen phosphorylase, and it employs phosphorolysis, resulting in the formation of glucose 1-phosphate. Glycogen phosphorylase continues this process until only four glucosyl units remain on each chain before a branch point. At this stage, the structure is termed a limit dextrin, which cannot be further degraded by phosphorylase.
- Removal of Branches: Branches in glycogen are removed by the debranching enzyme, a multifunctional protein with two enzymatic activities. The first activity, oligo-α(1→4)→α(1→4)-glucantransferase, removes three of the four glucosyl residues at the branch point and transfers them to another chain, elongating it. This enzymatic action breaks an α(1→4) bond and forms a new α(1→4) bond, functioning as a 4:4 transferase. The remaining glucose residue attached in an α(1→6) linkage is hydrolytically removed by amylo-α(1→6)-glucosidase activity, releasing free glucose. The glucosyl chain is now available for further degradation by glycogen phosphorylase.
- Conversion of Glucose 1-Phosphate to Glucose 6-Phosphate: Glucose 1-phosphate, a product of glycogen phosphorylase, undergoes conversion into glucose 6-phosphate within the cytosol, catalyzed by phosphoglucomutase. In the liver, glucose 6-phosphate is transported to the endoplasmic reticulum (ER) via glucose 6-phosphate translocase, where it is further converted into glucose by glucose 6-phosphatase. This glucose is then transported back to the cytosol. Hepatocytes release glycogen-derived glucose into the bloodstream, assisting in maintaining blood glucose levels, especially when gluconeogenesis is not actively producing glucose. In contrast, muscle tissue does not have glucose 6-phosphatase and utilizes glucose 6-phosphate in glycolysis to provide energy for muscle contraction.
- Lysosomal Degradation of Glycogen: A minor fraction (1%–3%) of glycogen undergoes continuous degradation in lysosomes, facilitated by the enzyme α(1→4)-glucosidase, also known as acid maltase. The precise purpose of this pathway remains unclear. However, the deficiency of this enzyme leads to the accumulation of glycogen in lysosomal vacuoles, resulting in the glycogen storage disease (GSD) Type II, commonly known as Pompe disease. Pompe disease is a unique GSD as it is a lysosomal storage disease.
In summary, glycogenolysis is a well-coordinated process involving multiple enzymatic steps that ensure the efficient mobilization of glucose from glycogen stores, thus playing a critical role in maintaining energy balance and blood glucose levels in the body.
Regulation Of Glycogenesis And Glycogenolysis
The tightly regulated processes of glycogenesis (glycogen synthesis) and glycogenolysis (glycogen degradation) are essential for maintaining blood glucose levels and meeting the body’s energy demands. Regulation occurs at both hormonal and allosteric levels, ensuring that the needs of the body and specific tissues are met.
A. Activation of Glycogen Degradation: Hormonal signals, such as glucagon or epinephrine binding to G protein-coupled receptors on the plasma membrane, initiate the need for glycogen degradation, either to raise blood glucose levels or provide energy during exercise.
- Activation of Protein Kinase A (PKA): Hormone binding triggers the activation of adenylyl cyclase, which synthesizes cyclic adenosine monophosphate (cAMP). cAMP activates PKA by releasing its catalytic subunits. PKA then phosphorylates various enzymes involved in glycogen metabolism, affecting their activity.
- Activation of Phosphorylase Kinase and Glycogen Phosphorylase: Phosphorylase kinase is activated by PKA-mediated phosphorylation, converting it from the inactive “b” form to the active “a” form. This active phosphorylase kinase then phosphorylates glycogen phosphorylase “b” to its active “a” form, initiating glycogenolysis.
- Summary of Glycogen Degradation Regulation: The hormonal signal initiates a cascade of reactions, resulting in glycogenolysis. This amplification of the effect is crucial for rapid responses to hormonal signals.
- Maintenance of the Phosphorylated State: The phosphate groups added during these reactions are maintained because protein phosphatase-1 (PP1), responsible for phosphate removal, is inhibited by phosphorylation and activation in response to cAMP. Insulin, in contrast, opposes the effects of glucagon and epinephrine by activating PP1 and degrading cAMP.
B. Inhibition of Glycogen Synthesis: Glycogen synthesis is regulated by the enzyme glycogen synthase, which exists in active “a” and inactive “b” forms. Unlike phosphorylase, the active form of glycogen synthase is dephosphorylated, while the inactive form is phosphorylated. Phosphorylation is catalyzed by various protein kinases, which can be regulated by cAMP or other signaling mechanisms.
C. Allosteric Regulation of Glycogen Synthesis and Degradation: In addition to hormonal signals, these processes are influenced by metabolite levels and energy requirements of cells. Allosteric regulation allows for a rapid response to cellular needs and can override hormonal covalent regulation.
- Regulation in the Well-Fed State: Allosteric activation of glycogen synthesis in both liver and muscle occurs when glucose 6-phosphate levels are elevated. In contrast, glycogen phosphorylase “a” is allosterically inhibited by glucose 6-phosphate and ATP, signaling a high-energy state in the cell.
- Activation of Glycogen Degradation by Calcium: Calcium ions (Ca²⁺) are released into the cytoplasm during muscle contraction or in response to epinephrine. Ca²⁺ binds to calmodulin (CaM), which activates phosphorylase kinase. This activation can occur without the need for phosphorylation.
- Activation of Glycogen Degradation in Muscle: Under conditions of anoxia and ATP depletion, muscle glycogen phosphorylase is activated by the high concentrations of adenosine monophosphate (AMP). AMP binds to glycogen phosphorylase “b,” leading to its activation without phosphorylation.
In conclusion, the regulation of glycogenesis and glycogenolysis involves a complex interplay of hormonal, covalent, and allosteric mechanisms to ensure that blood glucose levels are maintained and that cells have access to the energy stored in glycogen when needed.
Glycogen metabolism in liver and skeletal muscle
Glycogen, a complex polysaccharide, is primarily stored in two key tissues: the liver and skeletal muscle. Its role and regulation in these tissues are distinct, serving essential functions within the human body. Here, we provide a detailed exploration of glycogen metabolism in both the liver and skeletal muscle, emphasizing its complexities and relevance.
1. Glycogen Metabolism in the Liver
- Glycogen Synthesis: Liver glycogen primarily undergoes restoration during the postprandial phase in healthy individuals. Glucose moieties incorporated into liver glycogen can originate from ingested food, following the direct pathway of glycogen synthesis. Alternatively, glucose 6-phosphate, a precursor for glycogen synthesis, can be generated via gluconeogenesis, constituting the indirect pathway.
- Role of Glucose Sources: In cases of congenital glucokinase deficiency, the direct pathway’s importance is diminished, as impaired glucose phosphorylation to glucose 6-phosphate hinders the utilization of food-derived glucose. Additionally, the contributions of other monosaccharides like fructose and galactose to hepatic glycogen in humans remain less clear.
- Effect of Dietary Interventions: The addition of fructose, galactose, or amino acids to the restoration of liver glycogen varies in its effectiveness. While some studies report the superiority of fructose or amino acids in comparison to glucose, others do not show significant advantages.
2. Glycogen Metabolism in Skeletal Muscle
a. Exercise-Induced Glycogen Depletion:
- Energy Source for Muscle Contraction: Glycogen stores in contracting skeletal muscles serve as a primary source of energy during high-intensity physical exercise. Consequently, rigorous physical activity leads to a marked reduction in muscle glycogen content in active muscles while leaving the inactive ones largely unaffected.
- Exercise-Related Fatigue: Muscle glycogen content plays a pivotal role in the endurance capacity of skeletal muscles. Fatigue occurs when glycogen stores in active muscles are exhausted during exercise.
b. Post-Exercise Glycogen Replenishment:
- Enhanced Storage Capacity: Prior exercise enhances the skeletal muscle’s glycogen storage capacity. The glycogen content during the recovery phase increases rapidly in previously exercised muscles, surpassing the pre-exercise levels. Additionally, training reduces muscle glycogen utilization during exercise, ultimately increasing muscle glycogen content in endurance-trained subjects.
- Effects of Dietary Modifications: In the absence of exercise, fasting or food ingestion does not significantly alter glycogen stores in resting skeletal muscle. Even with a high-carbohydrate diet, the glycogen concentration in inactive muscles remains largely unaffected.
c. Glycogen Storage Diseases and Exercise:
- Impact on Exercise Performance: Patients with glycogen storage diseases affecting skeletal muscle often experience exercise intolerance, cramps, rhabdomyolysis, and myoglobinuria. Regular exercise programs may improve muscular performance in these patients by enhancing the muscle’s ability to oxidize fatty acids and reducing reliance on glycogen.
d. Complex Interplay with Other Metabolic Pathways:
- Role of Glycogen in Fatty Acid Metabolism: Glycogen metabolism is intertwined with fatty acid metabolism. Mutations in genes related to glycogen metabolism can mimic fatty acid oxidation disorders, leading to increased plasma concentrations of medium-chain fatty acids.
- Connections with Other Organs: Altered glycogen metabolism can impact various organs and systems. Neurological effects, kidney dysfunction, and cardiac abnormalities are observed in various glycogen storage diseases.
- Impact on Glycosylation Processes: Several glycogen storage diseases, such as congenital deficiency of phosphoglucomutase-1, influence glycosylation processes, resulting in a range of clinical manifestations.
- Promising Therapeutic Avenues: Current therapies for glycogen storage diseases are limited, with enzyme replacement therapy available for some. Future therapeutic strategies, including gene therapy, offer hope for improved management of these complex disorders.
In summary, glycogen metabolism in the liver and skeletal muscle is a highly regulated and vital process that ensures the availability of glucose for energy requirements during fasting and exercise. The complex interplay between glycogen metabolism and other metabolic pathways underscores the significance of this process in maintaining overall health. Further research is essential to unveil the full potential for therapeutic interventions in glycogen storage diseases.
Glycogen Storage Diseases
Glycogen storage diseases (GSDs) encompass a group of genetic disorders caused by defects in specific enzymes crucial for glycogen metabolism. These defects result in an array of symptoms, varying in severity depending on the type of GSD and the affected tissues. In this comprehensive exploration of GSDs in humans, we provide detailed information on the various types, the affected enzymes, and their associated symptoms.
Type 0: Glycogen Synthase Deficiency
- Enzyme Affected: Glycogen synthase
- Affected Tissues: Liver
- Symptoms: Individuals with Type 0 GSD exhibit low blood glucose levels and elevated ketone bodies. This disorder often leads to early mortality.
Type Ia (von Gierke): Glucose 6-Phosphatase Deficiency
- Enzyme Affected: Glucose 6-phosphatase
- Affected Tissues: Liver
- Symptoms: Clinical manifestations include an enlarged liver and kidney failure.
Type Ib: Microsomal Glucose 6-Phosphate Translocase Deficiency
- Enzyme Affected: Microsomal glucose 6-phosphate translocase
- Affected Tissues: Liver
- Symptoms: Type Ib shares symptoms with Type Ia, including an enlarged liver and kidney complications. Additionally, patients are more susceptible to bacterial infections.
Type Ic: Microsomal Pi Transporter Deficiency
- Enzyme Affected: Microsomal Pi transporter
- Affected Tissues: Liver
- Symptoms: Similar to Type Ia, this form of GSD exhibits an enlarged liver.
Type II (Pompe): Lysosomal α-Glucosidase Deficiency
- Enzyme Affected: Lysosomal α-glucosidase
- Affected Tissues: Skeletal and cardiac muscle
- Symptoms: Pompe disease has various forms: infantile, juvenile, and adult. The infantile form often leads to death by age two. Symptoms include cardiac and muscular defects. The juvenile and adult forms display muscle weakness similar to muscular dystrophy.
Type IIIa (Cori or Forbes): Debranching Enzyme Deficiency
- Enzyme Affected: Debranching enzyme
- Affected Tissues: Liver and skeletal muscle
- Symptoms: Infants may have an enlarged liver, while cardiac myopathy is common in individuals with this GSD.
Type IIIb: Liver Debranching Enzyme Deficiency
- Enzyme Affected: Liver debranching enzyme
- Affected Tissues: Liver (muscle enzyme remains normal)
- Symptoms: Symptoms are akin to those of Type IIIa, including an enlarged liver.
Type IV (Andersen): Branching Enzyme Deficiency
- Enzyme Affected: Branching enzyme
- Affected Tissues: Liver and skeletal muscle
- Symptoms: This GSD leads to an enlarged liver and spleen, with the presence of myoglobin in urine.
Type V (McArdle): Muscle Phosphorylase Deficiency
- Enzyme Affected: Muscle phosphorylase
- Affected Tissues: Skeletal muscle
- Symptoms: Individuals with McArdle’s disease experience exercise-induced cramps and pain. Myoglobin is often detected in the urine.
Type VI (Hers): Liver Phosphorylase Deficiency
- Enzyme Affected: Liver phosphorylase
- Affected Tissues: Liver
- Symptoms: An enlarged liver is a typical symptom of this GSD.
Type VII (Tarui): Muscle PFK-1 Deficiency
- Enzyme Affected: Muscle PFK-1
- Affected Tissues: Muscle, erythrocytes
- Symptoms: This GSD is associated with exercise-induced cramps and pain, myoglobinuria (myoglobin in the urine), and hemolytic anemia.
Type VIb, VIII, or IX: Phosphorylase Kinase Deficiency
- Enzyme Affected: Phosphorylase kinase
- Affected Tissues: Liver, leukocytes, muscle
- Symptoms: Enlarged liver is a common symptom in these cases.
Type XI (Fanconi-Bickel): Glucose Transporter (GLUT2) Deficiency
- Enzyme Affected: Glucose transporter (GLUT2)
- Affected Tissues: Liver
- Symptoms: Patients with this GSD experience failure to thrive, an enlarged liver, rickets, and kidney dysfunction.
| Type | Enzyme Affected | Affected Tissues | Symptoms |
|---|---|---|---|
| Type 0 | Glycogen synthase | Liver | Low blood glucose, high ketone bodies, early death |
| Type Ia | Glucose 6-phosphatase | Liver | Enlarged liver, kidney failure |
| Type Ib | Microsomal glucose 6-phosphate translocase | Liver | Similar to Type Ia; also high susceptibility to bacterial infections |
| Type Ic | Microsomal Pi transporter | Liver | Similar to Type Ia |
| Type II | Lysosomal α-glucosidase | Skeletal and cardiac muscle | Infantile form: death by age 2; cardiac and muscular defects; juvenile and adult forms: muscle weakness similar to muscular dystrophy |
| Type IIIa | Debranching enzyme | Liver and skeletal muscle | Enlarged liver in infants, cardiac myopathy |
| Type IIIb | Liver debranching enzyme | Liver (muscle enzyme normal) | Enlarged liver in infants |
| Type IV | Branching enzyme | Liver and skeletal muscle | Enlarged liver and spleen, myoglobin in urine |
| Type V | Muscle phosphorylase | Skeletal muscle | Exercise-induced cramps and pain, myoglobin in urine |
| Type VI | Liver phosphorylase | Liver | Enlarged liver |
| Type VII | Muscle PFK-1 | Muscle, erythrocytes | Similar to Type V; also hemolytic anemia |
| Type VIb, VIII, or IX | Phosphorylase kinase | Liver, leukocytes, muscle | Enlarged liver |
| Type XI | Glucose transporter (GLUT2) | Liver | Failure to thrive, enlarged liver, rickets, kidney dysfunction |
In summary, GSDs represent a diverse group of disorders, each characterized by distinct enzymatic defects and a unique set of symptoms. While many GSDs primarily affect the liver, others target skeletal and cardiac muscle tissues, leading to a wide range of clinical presentations. Understanding the specific GSD type and its associated enzyme deficiency is crucial for effective diagnosis and management.
References
- Adeva-Andany, María M.; González-Lucán, Manuel; Donapetry-García, Cristóbal; Fernández-Fernández, Carlos; Ameneiros-Rodríguez, Eva (2016). Glycogen metabolism in humans. BBA Clinical, 5(), 85–100. doi:10.1016/j.bbacli.2016.02.001
- Roach, P.J. (2013). Encyclopedia of Biological Chemistry || Glycogen Metabolism. , (), 425–427. doi:10.1016/B978-0-12-378630-2.00042-6
- https://uh.edu/dtu/01-Glycogen-07.htm
- https://www.wikilectures.eu/w/Glycogen_metabolism