What is Type I Hypersensitivity Reaction?
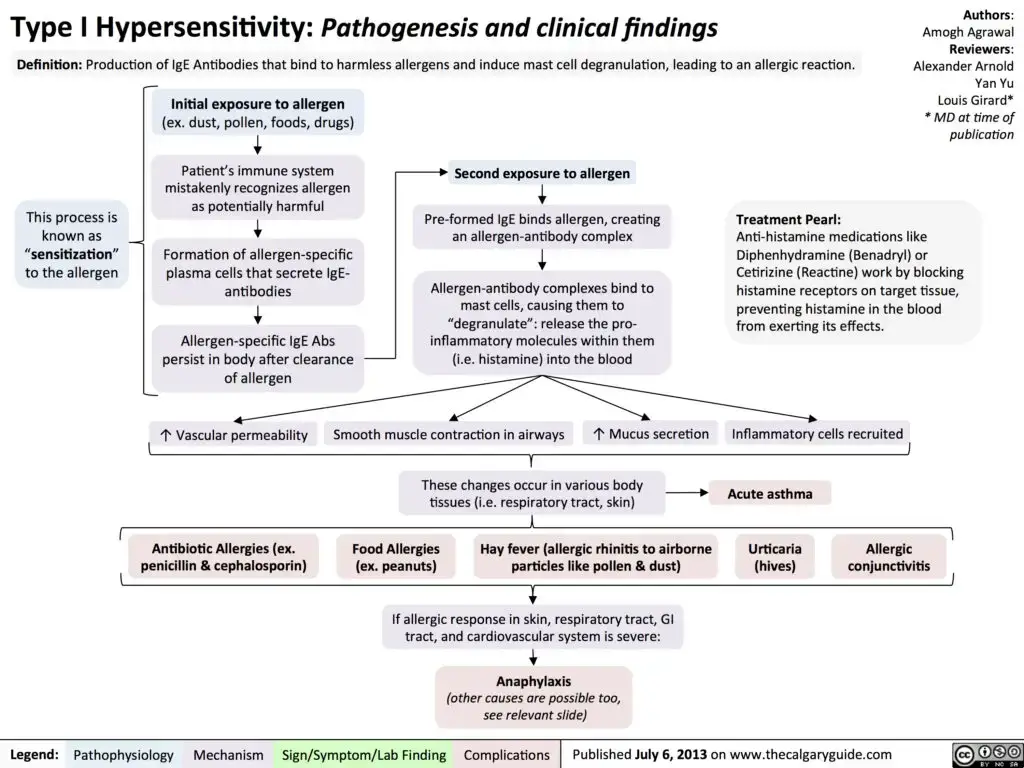
- Type I hypersensitivity reactions, also known as immediate hypersensitivity reactions, are a type of allergic response that occurs when an individual is re-exposed to a specific antigen, known as an allergen. These reactions are mediated by immunoglobulin E (IgE) and involve the degranulation of basophils or mast cells.
- The onset of type I hypersensitivity reactions is rapid, typically occurring within minutes of exposure to the allergen. This immediate response is due to the presence of preformed mediators in the mast cells, which are sensitized by IgE antibodies. IgE plays a crucial role in sensitizing mast cells and facilitating the recognition of antigens for immediate hypersensitivity reactions.
- The symptoms of type I hypersensitivity reactions can manifest in two forms: anaphylaxis and atopy. Anaphylaxis is a severe, potentially life-threatening reaction characterized by a systemic release of inflammatory mediators. It can lead to symptoms such as difficulty breathing, rapid heartbeat, low blood pressure, hives, and swelling. On the other hand, atopy refers to a genetic predisposition to allergic diseases, including hay fever, asthma, and food allergies.
- Type I reactions can be triggered through various routes of exposure, including ingestion, inhalation, injection, or direct contact with the allergen. Common allergens associated with type I hypersensitivity reactions include pollen, certain foods, insect venom, and pet dander.
- In addition to the immediate reaction, type I hypersensitivity reactions can also exhibit a late-phase reaction. This secondary response occurs 2 to 8 hours after the initial exposure and can last for 2 to 3 days. It is characterized by the recruitment of inflammatory cells and the release of additional inflammatory mediators, leading to prolonged symptoms and tissue damage.
- It is important to note that the classification of allergic reactions according to Gell and Coombs has limited utility in clinical practice. The understanding of allergies has evolved since the development of this classification, and the relevance of this system has been questioned. However, type I hypersensitivity reactions continue to be a significant area of study and clinical focus in the field of allergy and immunology.
- Overall, type I hypersensitivity reactions represent an exaggerated immune response to an allergen, mediated by IgE antibodies and resulting in the release of inflammatory mediators. These reactions can range from mild to severe, and proper management and avoidance of allergens are essential for individuals prone to these allergic responses.
Definition of Type I Hypersensitivity Reaction?
Type I hypersensitivity reaction, also known as immediate hypersensitivity, is an exaggerated immune response triggered by the re-exposure to a specific allergen. It involves the rapid release of inflammatory mediators from mast cells and basophils sensitized with IgE antibodies. This type of reaction is associated with conditions such as allergic rhinitis, asthma, and anaphylaxis, and it typically occurs within minutes of exposure to the allergen.
Mechanism of Type I hypersesnsitivity reaction
Two antigen doses are required for the development of allergy or anaphylaxis. The first dose is known as the sensitizing dosage, while the second dose is known as the shocking dose.
1. Production of IgE antibody
- During the production of IgE antibodies in the context of Type I hypersensitivity, the process begins when an antigen, also known as an allergen, enters the host’s body. Antigen-presenting cells (APCs) process and present the allergen to CD4 T cells. These CD4 T cells become activated and undergo division, resulting in the formation of T helper cells and memory cells.
- T helper cells play a crucial role in the production of IgE antibodies. They secrete a cytokine called interleukin-4 (IL-4), which promotes the differentiation and activation of B cells. Simultaneously, B cells, in the presence of APCs and IL-4, bind to the allergen and become activated.
- The activated B cells undergo division, giving rise to two types of cells: plasma cells and memory cells. Plasma cells are responsible for antibody production. In the case of Type I hypersensitivity, these plasma cells produce IgE antibodies instead of the more common IgM or IgG antibodies seen in normal immune responses.
- The production of IgE antibodies is a distinguishing feature of Type I hypersensitivity reactions. IgE antibodies bind to specific receptors on the surface of mast cells and basophils, sensitizing these cells for future encounters with the allergen. This sensitization sets the stage for subsequent allergic reactions, as the IgE-coated mast cells and basophils are ready to release inflammatory mediators upon re-exposure to the allergen.
- It’s important to note that the production of IgE antibodies is just one aspect of the complex immune response involved in Type I hypersensitivity reactions. The cascade of events that follows, including the degranulation of mast cells and the release of inflammatory mediators, leads to the characteristic symptoms associated with allergies and immediate hypersensitivity reactions.
2. Sensitization
- Sensitization refers to the process by which mast cells and basophils become bound with IgE antibodies. The Fc region of IgE antibodies contains receptors known as FcRI, which are present on the surface of tissue mast cells and blood basophils. When IgE antibodies bind to these receptors, it leads to the sensitization of mast cells and basophils.
- During sensitization, allergens or antigens trigger the production of specific IgE antibodies by activated B cells. These IgE antibodies, instead of other antibody classes like IgM or IgG, are particularly specialized in recognizing and binding to specific allergens. Once produced, these IgE antibodies travel through the bloodstream and bind to the FcRI receptors on mast cells and basophils.
- The binding of IgE antibodies to FcRI receptors on mast cells and basophils is essential for the subsequent allergic response. Sensitized mast cells and basophils become primed for reactivity to specific allergens. This means that upon re-exposure to the same allergen, the allergen can directly bind to the IgE antibodies already bound to the mast cells or basophils, triggering their activation.
- The sensitization process is a crucial step in the development of Type I hypersensitivity reactions. Sensitized mast cells and basophils act as key players in the immediate response to allergens. Upon allergen re-exposure, the cross-linking of IgE antibodies on the mast cells and basophils leads to the degranulation of these cells, resulting in the release of various inflammatory mediators such as histamine, leukotrienes, and cytokines. This release of mediators contributes to the characteristic symptoms observed in allergic reactions, such as itching, swelling, and inflammation.
- It’s important to note that sensitization occurs following the initial exposure to an allergen and subsequent production of specific IgE antibodies. Once an individual has been sensitized, they are at an increased risk of experiencing allergic reactions upon future encounters with the same allergen. Sensitization is a key component of the immune process underlying Type I hypersensitivity reactions.
3. Shocking dose of antigen
- When an antigen (allergen) enters the body for the second time in a host that has previously been sensitized, a phenomenon known as the “shocking dose of antigen” can occur. During this process, the antigen cross-links with the Fab region of IgE molecules that are already bound to the surface of mast cells or basophils.
- Upon the initial exposure to the allergen, the host’s immune system recognizes it as a foreign substance and mounts an immune response. This response includes the production of specific IgE antibodies that are capable of binding to the allergen. These IgE antibodies are then attached to the FcRI receptors on the surface of mast cells and basophils, a process known as sensitization.
- During subsequent exposures to the same allergen, the shocking dose occurs when the allergen enters the body and comes into contact with the IgE antibodies already bound to the mast cells or basophils. The allergen cross-links with the Fab regions of these IgE molecules, causing the IgE antibodies to cluster together. This cross-linking triggers a signaling cascade within the mast cells or basophils, leading to their activation and degranulation.
- The degranulation of mast cells and basophils results in the release of various mediators, including histamine, leukotrienes, prostaglandins, and cytokines. These mediators are responsible for the immediate allergic reactions observed in Type I hypersensitivity, such as itching, redness, swelling, bronchoconstriction, and vasodilation.
- The shocking dose of antigen amplifies the immune response compared to the initial exposure, as there is a higher concentration of specific IgE antibodies bound to the mast cells and basophils. This rapid and intense response is what contributes to the characteristic symptoms of immediate hypersensitivity reactions seen in allergies, such as anaphylaxis or localized allergic reactions.
- It’s important to note that the shocking dose of antigen is specific to Type I hypersensitivity reactions and occurs upon re-exposure to an allergen in an already sensitized individual. Understanding this process is crucial for managing allergies and developing strategies to prevent or mitigate severe allergic reactions.
4. Degranulation of mast cell
- The degranulation of mast cells is a critical step in the immune response during Type I hypersensitivity reactions. When an allergen cross-links with IgE antibodies bound to the surface of mast cells, it triggers the degranulation process. Degranulation refers to the release of granules containing various pharmacologically active chemicals from the mast cells.
- The cross-linking of antigen (allergen) to IgE antibodies on the mast cell surface leads to the activation of signaling pathways within the cell. This activation results in the rapid release of pre-formed granules, known as secretory granules or mast cell granules, from the cytoplasm of the mast cell.
- The released granules contain a wide array of pharmacologically active substances, including histamine, heparin, serotonin, cytokines, leukotrienes, and prostaglandins. These substances play essential roles in the allergic response and contribute to the characteristic symptoms observed in Type I hypersensitivity reactions.
- Histamine is one of the key mediators released during mast cell degranulation. It causes vasodilation, increased vascular permeability, and smooth muscle contraction. Histamine is responsible for symptoms such as itching, redness, and swelling seen in allergic reactions.
- Heparin, another component released by mast cells, acts as an anticoagulant, preventing blood clot formation. It helps to maintain blood fluidity during an allergic response.
- Serotonin, also known as 5-hydroxytryptamine, is involved in blood vessel constriction and smooth muscle contraction. It contributes to the bronchoconstriction and gastrointestinal symptoms often observed during allergic reactions.
- Cytokines released from mast cells play a role in immune regulation and inflammation. They can recruit and activate other immune cells, enhancing the immune response to the allergen.
- Leukotrienes and prostaglandins are lipid mediators that promote inflammation, smooth muscle contraction, and increased vascular permeability. They contribute to the respiratory symptoms, such as bronchoconstriction and mucus production, commonly seen in allergic asthma.
- The degranulation of mast cells and the release of these pharmacologically active chemicals are responsible for the rapid onset of symptoms in Type I hypersensitivity reactions. The combined effects of these mediators lead to local or systemic allergic responses, depending on the extent of mast cell degranulation and the distribution of the allergen.
- Understanding the degranulation process of mast cells is crucial for developing strategies to manage and treat allergic conditions. By targeting the release of these mediators, it is possible to alleviate symptoms and modulate the immune response in individuals with allergies.
5. Anaphylatic reaction
- An anaphylactic reaction is a severe and potentially life-threatening manifestation of Type I hypersensitivity. It occurs when an individual with a hypersensitivity to a particular allergen is re-exposed to that allergen, resulting in a rapid and widespread allergic response throughout the body.
- During an anaphylactic reaction, the release of active chemical mediators from mast cells and basophils, such as histamine, leukotrienes, prostaglandins, and cytokines, has a profound impact on surrounding tissues. These mediators act on various tissues and cells, leading to a range of symptoms associated with allergy.
- Vasodilation is one of the prominent effects of these chemical mediators. It causes the blood vessels to widen, resulting in increased blood flow to the affected areas. This can lead to symptoms like redness, warmth, and swelling at the site of the allergic reaction.
- Smooth muscle contraction is another significant effect. The mediators cause the smooth muscles in the airways, gastrointestinal tract, and blood vessels to contract. This can result in bronchoconstriction, leading to difficulty in breathing and wheezing, as well as gastrointestinal symptoms such as abdominal cramps, nausea, vomiting, and diarrhea.
- Increased mucus production is a common response during anaphylaxis. The chemical mediators stimulate the mucous glands, leading to excessive secretion of mucus. This can cause symptoms like a runny or congested nose, coughing, and a sensation of a “tickle” in the throat.
- Other symptoms of anaphylaxis may include itching, hives (urticaria), angioedema (swelling of deeper layers of the skin), itching or tingling sensation in the mouth or throat, and a feeling of lightheadedness or dizziness. In severe cases, anaphylaxis can cause a drop in blood pressure (hypotension) and lead to shock, which is a life-threatening condition requiring immediate medical attention.
- The allergic reaction during anaphylaxis can be localized or systemic, depending on the type of allergen and the extent of the immune response. Localized reactions typically occur at the site of allergen exposure, resulting in symptoms confined to that area. Systemic reactions, on the other hand, involve a widespread release of mediators, leading to symptoms throughout the body.
- Anaphylactic reactions require prompt and appropriate medical intervention, including the administration of epinephrine (adrenaline) to counteract the severe symptoms and stabilize the individual. It is crucial for individuals at risk of anaphylaxis to carry emergency medications, such as an epinephrine auto-injector, and to seek immediate medical help in case of exposure to known allergens.
- Managing anaphylactic reactions involves identifying and avoiding triggers, educating individuals and caregivers about allergen avoidance, and developing an emergency action plan with clear instructions on how to respond to an anaphylactic event.
Mechanism of Type I hypersesnsitivity reaction
The mechanism of Type I hypersensitivity reactions involves several key steps:
- Sensitization: The process begins with the initial exposure to an allergen. Antigen-presenting cells (APCs) process and present the allergen to CD4 T cells. The activated CD4 T cells differentiate into T helper cells, which produce interleukin-4 (IL-4). Concurrently, B cells bind to the allergen in the presence of APCs and IL-4, leading to their activation. Activated B cells divide and differentiate into plasma cells, which produce immunoglobulin E (IgE) antibodies instead of the usual IgM or IgG antibodies.
- Sensitization of Mast Cells and Basophils: The Fc region of IgE antibodies binds to the Fc receptor (FcRI) on the surface of mast cells and basophils. This binding of IgE antibodies to mast cells and basophils is known as sensitization. The mast cells and basophils become sensitized or primed for future encounters with the specific allergen.
- Second Exposure: Upon subsequent exposure to the same allergen, the shocking dose occurs. The allergen binds to the Fab region of the IgE antibodies already bound to the mast cells or basophils, cross-linking the IgE molecules.
- Degranulation of Mast Cells and Basophils: The cross-linking of the allergen to the IgE antibodies triggers the degranulation process. The mast cells and basophils release their granules, which contain various pharmacologically active chemicals such as histamine, heparin, serotonin, cytokines, leukotrienes, and prostaglandins.
- Anaphylactic Reaction: The released active chemical mediators act on surrounding tissues, leading to the manifestation of various allergy symptoms. For example, histamine causes vasodilation, increased vascular permeability, and smooth muscle contraction. These effects result in symptoms such as redness, swelling, bronchoconstriction, mucus production, sneezing, and other allergic reactions.
The severity and localization of the allergic reaction can vary, depending on the specific allergen and the individual’s immune response. The reaction may be localized to the site of allergen exposure or systemic, affecting multiple areas of the body.
Understanding the mechanism of Type I hypersensitivity reactions is crucial for the diagnosis, prevention, and management of allergic conditions. It helps in the development of targeted therapies, such as antihistamines or epinephrine, to alleviate symptoms and mitigate severe allergic reactions.
Mechanism of Activation and Degranulation of mast cell
The intracellular signaling events that ultimately result in mast cell degranulation involve the cooperation of numerous protein and lipid kinase and phosphatase, as well as cytoskeleton rearrangement. Mast cell activation and degranulation can be broken down into three biochemical phases.
- Phosphorylation
- Methylation
- Adenylation
1. Phosphorylation
Phosphorylation is a critical biochemical process involved in the signaling pathway of Type I hypersensitivity reactions. It plays a key role in the activation of downstream molecules and the subsequent cellular responses. Here is an overview of phosphorylation in the context of allergen-induced activation:
- Activation of Protein Tyrosine Kinase (PTK): When an allergen binds to the FcERI (Fc epsilon receptor I) on the surface of mast cells or basophils, it triggers the activation of protein tyrosine kinase (PTK). PTK is an enzyme responsible for adding phosphate groups to specific tyrosine residues of target proteins.
- Phosphorylation of Phospholipase C: Activated PTK phosphorylates phospholipase C (PLC). Phosphorylated PLC undergoes a conformational change and becomes enzymatically active. This active form of PLC plays a crucial role in the intracellular signaling cascade.
- Conversion of Phosphatidylinositol 4,5 Bisphosphate (PIP2): PLC converts phosphatidylinositol 4,5 bisphosphate (PIP2) into two secondary messengers: diacylglycerol (DAG) and inositol triphosphate (IP3).
- Release of Inositol Triphosphate (IP3): IP3 acts as a potent mobilizer of intracellular calcium (Ca2+). IP3 diffuses into the endoplasmic reticulum (ER), where it binds to IP3 receptors, leading to the opening of calcium channels. This results in the release of Ca2+ ions from the ER into the cytoplasm.
- Cellular Responses: The increased concentration of intracellular Ca2+ triggers various cellular responses. Calcium ions play a crucial role in the degranulation process of mast cells and basophils, leading to the release of mediators such as histamine and other pharmacologically active substances.
- Activation of Protein Kinase C (PKC): Simultaneously, diacylglycerol (DAG), the second product of PLC activity, activates protein kinase C (PKC). PKC is an enzyme involved in multiple signaling pathways and regulates various cellular processes. The activation of PKC further amplifies the intracellular signaling events, leading to the production of pro-inflammatory cytokines and other immune responses.
Phosphorylation, particularly the activation of PTK and subsequent phosphorylation events, is a critical step in the initiation and amplification of the signaling cascade in Type I hypersensitivity reactions. It leads to the release of calcium ions, activation of PKC, and ultimately, the manifestation of allergic symptoms. Understanding the phosphorylation events in this context can provide insights into the development of targeted therapies aimed at interrupting the signaling pathway and alleviating allergic reactions.
2. Methylation
- Methylation is an essential process that occurs within cells and plays a significant role in various biological pathways. One instance where methylation is involved is in the conversion of phosphatidylethanolamine (PE) to phosphatidylcholine (PC). This process is catalyzed by the enzymes phopholipid methyl transferase I and II (PMT I and PMT II).
- To understand how methylation is related to the formation of PC, we need to look at the preceding steps. Cross linkage of FcERI triggers the activation of an enzyme, which converts phosphatidyl serine (PS) into PE. Subsequently, PE undergoes methylation to form PC through the actions of PMT I and PMT II enzymes.
- The accumulation of PC on the exterior surface of the plasma membrane has notable effects on cellular function. One of the outcomes is an increased membrane fluidity, which facilitates the formation of calcium ion (Ca++) channels. These channels allow Ca++ ions to enter the cell.
- Once Ca++ ions enter the cell, they contribute to a cascade of events. The presence of Ca++ ions, along with the activation of protein tyrosine kinase (PTK), leads to the activation of Mitogen-activated protein kinase (MAPK). MAPK, in turn, plays a crucial role in various cellular processes.
- Activated MAPK further triggers the activation of phospholipase A2, an enzyme responsible for the breakdown of PC into two components: Lyso PC and Arachidonic acid. Arachidonic acid, one of the breakdown products, serves as a precursor for the production of potent mediators known as Leukotrienes and prostaglandin D2.
- Additionally, the activated MAPK pathway has implications for the immune response. MAPK induces the secretion of cytokines by increasing the transcription of cytokine genes. Cytokines are important signaling molecules involved in immune responses and various cellular processes.
- In summary, methylation plays a role in the conversion of PE to PC, a process mediated by PMT I and PMT II enzymes. The accumulation of PC on the plasma membrane affects membrane fluidity and leads to the formation of Ca++ channels. Ca++ ions, along with PTK activation, trigger the activation of MAPK, which subsequently activates phospholipase A2. The breakdown of PC by phospholipase A2 produces Lyso PC and Arachidonic acid, with the latter being converted into potent mediators such as Leukotrienes and prostaglandin D2. Furthermore, the MAPK pathway induces the secretion of cytokines by increasing the transcription of cytokine genes, affecting immune responses and other cellular processes.
3. Adenylation
- Adenylation is a crucial process that occurs in response to the cross-linkage of FcERI and plays a significant role in mast cell degranulation, which is associated with allergic symptoms. The activation of membrane adenylate cyclase enzyme, triggered by FcERI cross-linkage, leads to a transient increase in cyclic adenosine monophosphate (cAMP) levels within 15 seconds.
- However, there is a subsequent drop in cAMP levels, which is mediated by protein kinase. This decrease in cAMP is necessary for the degranulation of mast cells. The decrease in cAMP levels is achieved through the action of protein kinase, which phosphorylates granule membrane proteins. This phosphorylation alters the permeability of the granules, allowing water and calcium ions (Ca++) to enter the granules. As a result, the granules swell.
- The swelling of the granules is significant as it leads to the formation of a Soluble N-ethylmaleimide attachment receptor (SNARE) protein complex. This complex facilitates the fusion of the granule membrane with the plasma membrane of the mast cell. This fusion process enables the release of pharmacological chemical products stored within the granules.
- The release of these pharmacological chemical products, such as histamine and other inflammatory mediators, is responsible for the allergic symptoms experienced. The release of histamine, in particular, contributes to various allergic responses, including itching, swelling, and redness.
- In summary, adenylation is a process associated with FcERI cross-linkage that triggers mast cell degranulation. The activation of adenylate cyclase leads to a transient increase in cAMP levels, followed by a decrease mediated by protein kinase. This decrease in cAMP is necessary for mast cell degranulation. Protein kinase phosphorylates granule membrane proteins, altering granule permeability, resulting in the swelling of granules. The swollen granules then facilitate the formation of SNARE protein complexes, which enable the fusion of the granule membrane with the plasma membrane. This fusion process allows the release of pharmacological chemical products responsible for allergic symptoms, such as histamine.
Clinical manifestation
Clinical manifestations range from life-threatening conditions like systemic anaphylaxis and severe asthma to localised reactions like hay fever and eczema.
A. Systemic anaphylaxis
- Systemic anaphylaxis is an extremely serious and potentially fatal condition characterized by a severe allergic reaction that affects the entire body. This life-threatening state is typically initiated when an allergen enters the bloodstream directly or is absorbed from the gastrointestinal tract or skin.
- The symptoms of systemic anaphylaxis can be severe and manifest rapidly. They may include labored breathing, a sudden drop in blood pressure, smooth muscle contraction, bronchiole constriction, and a sensation of suffocation. These symptoms reflect the widespread and systemic nature of the allergic reaction.
- Labored breathing is a prominent feature of systemic anaphylaxis, often resulting from the constriction of the airways due to the body’s response to the allergen. This constriction makes it difficult for affected individuals to breathe properly, leading to shortness of breath, wheezing, and a feeling of tightness in the chest.
- The drop in blood pressure, known as hypotension, is a critical symptom of systemic anaphylaxis. It occurs due to the widespread dilation of blood vessels, which leads to a decrease in blood volume within the circulatory system. As a result, there is insufficient blood flow to vital organs, potentially causing organ damage and compromising their normal functioning.
- Smooth muscle contraction is a characteristic feature of systemic anaphylaxis. This contraction affects various organs and tissues throughout the body, leading to symptoms such as abdominal cramps, diarrhea, and uterine contractions in some cases.
- Bronchiole constriction refers to the narrowing of the small airways (bronchioles) in the lungs. This constriction is a result of the body’s immune response to the allergen, leading to difficulty in breathing, wheezing, and a sense of suffocation.
- Suffocation is a distressing sensation experienced by individuals during systemic anaphylaxis. It is a consequence of the bronchiole constriction and labored breathing, which can result in a severe and overwhelming feeling of being unable to breathe properly.
- Systemic anaphylaxis requires immediate medical attention, as it is a medical emergency. Prompt administration of epinephrine (adrenaline) is crucial to counteract the severe allergic reaction and alleviate the symptoms. It is vital for individuals at risk of anaphylaxis to carry epinephrine auto-injectors and be knowledgeable about their use in case of an allergic emergency.
- In summary, systemic anaphylaxis is a severe and potentially fatal allergic reaction that affects the entire body. It is characterized by symptoms such as labored breathing, a drop in blood pressure, smooth muscle contraction, bronchiole constriction, and a sensation of suffocation. Immediate medical intervention, including the administration of epinephrine, is essential to manage this life-threatening condition.
B. Localized hypersensitivity
Localized hypersensitivity refers to an allergic reaction that is confined to a specific target tissue or organ. This type of hypersensitivity often occurs at the epithelial surface where the allergen enters the body.
The predisposition to manifest localized hypersensitivity reactions is inherited and is known as atopy. Individuals with atopy have an increased susceptibility to develop allergic reactions when exposed to allergens.
Atopic allergies encompass a wide range of immunoglobulin E (IgE)-mediated disorders. Some common examples of atopic allergies include:
- Hay fever (allergic rhinitis): This condition involves an allergic reaction to airborne allergens such as pollen, dust mites, or animal dander. Symptoms include nasal congestion, sneezing, runny nose, and itchy/watery eyes.
- Asthma: Asthma can be categorized as allergic or intrinsic. Allergic asthma is triggered by allergens such as pollen, dust mites, or pet dander. Intrinsic asthma, on the other hand, is not triggered by allergens but by other factors such as exercise, stress, or respiratory infections. Asthma is characterized by wheezing, coughing, shortness of breath, and chest tightness.
- Food allergy: This type of allergy occurs when the immune system reacts to specific proteins present in certain foods. Common food allergens include peanuts, tree nuts, shellfish, eggs, milk, and soy. Food allergies can cause a range of symptoms, including hives, swelling, gastrointestinal discomfort, and in severe cases, anaphylaxis.
- Atopic dermatitis (eczema): Atopic dermatitis is a chronic inflammatory skin condition characterized by itchy, red, and inflamed skin. It often occurs in individuals with a personal or family history of atopic allergies. Eczema can be triggered or worsened by various factors, including allergens, irritants, dry skin, and stress.
These atopic allergies are characterized by an immune response involving the production of IgE antibodies in response to specific allergens. Upon re-exposure to the allergen, the immune system releases histamine and other inflammatory substances, leading to the characteristic symptoms of localized hypersensitivity.
Management of localized hypersensitivity involves allergen avoidance whenever possible, as well as pharmacological interventions such as antihistamines, corticosteroids, and immunomodulatory medications. In some cases, immunotherapy may be recommended to desensitize the immune system to specific allergens and reduce the severity of allergic reactions.
In summary, localized hypersensitivity refers to an allergic reaction that is limited to a specific target tissue or organ. It is often associated with atopy, an inherited tendency to manifest hypersensitivity reactions. Atopic allergies encompass a range of IgE-mediated disorders such as hay fever, asthma, food allergy, and atopic dermatitis. Proper management involves allergen avoidance, medications, and, in certain cases, immunotherapy.
Diagnosis Type 1 hypersensitivity reaction
- A thorough patient history and educated estimates may be used to identify the allergy.
- Ag skin testing with a comprehensive panel. This is accomplished through subcutaneous Ag injection or a patch test to determine wheal and flare response.
- Subcutaneous administration of the antigen results in the release of prepared mediators that increase vascular permeability, local edoema, and irritation.
- The late phase reaction is frequently neglected, and typically manifests as a painful lump on the skin that is not irritating.
- IgE level: IgE levels in the majority of patients may be elevated.
- This is a radioallergosorbent test that identifies allergen-specific IgE. It is an expensive test that is inferior to skin tests.
- Eosinophil Count:-Eosinophilia in the blood may be present in allergic disorders.
Treatment / Management of Type I Hypersensitivity
The sort of treatment administered to a patient with type I hypersensitivity varies on the patient’s symptoms and the reaction’s cause.
A. Anaphylaxis
- Anaphylaxis necessitates urgent treatment, as its onset is typically quick and it can be fatal.
- If feasible, the offending agent should be eliminated immediately, and patients should be placed in a supine position with their lower extremities elevated, unless there is a substantial blockage or airway inflammation.
- If there is significant stridor or severe respiratory distress, intubation may be required immediately.
- If the patient has a history of allergic reactions, they will be given prescriptions for emergency self-treatment, including an epinephrine IM autoinjector or 1:1,000 solution, bronchodilators, antihistamines, and/or corticosteroids.
- Epinephrine intramuscular (IM) injection is the recommended first-line treatment that should be delivered without delay, followed by the use of the following adjuvant therapies:
Epinephrine
- Epinephrine exerts agonist actions on alpha-1, beta-1, and beta-2 adrenergic receptors. Consequently, it can promote vasoconstriction and peripheral vascular resistance while decreasing airway or mucosal edoema. The beta effects result in an increase in inotropy, chronotropy, vasodilation, and a decrease in the release of inflammatory mediators from mast cells and basophils.
- The epinephrine dosage is depending on body weight and may be repeated every 5 to 15 minutes. Studies have revealed that a second dose is necessary in approximately 35% of cases.
- When possible, infants weighing less than 10 kg should be given an exact dose based on their weight (rather than an approximation). The 0.1 mg dose may be administered via autoinjector or by drawing up 0.1 mL of the 1 mg/mL solution if drawing up an accurate dose is anticipated to cause a considerable delay in a patient with severe symptoms or who is rapidly deteriorating. In the absence of the 0.1 mg autoinjector, the 0.15 mg autoinjector may be utilised.
- For weights between 10 and 25 kg, 0.15 mg of IM epinephrine is administered into the anterior-lateral thigh.
- For weights greater than 25 kilogrammes, 0.3 mg of IM epinephrine is injected into the anterior-lateral thigh.
- The dose of epinephrine solution (1 per 1,000) is 0.01 mg/kg per dose, with a maximum of 0.5 mg/dose.
- Additionally, epinephrine can be delivered via slow continuous infusion, endotracheal, and intra-osseous routes. It is recommended that blood pressure and heart rate be monitored during administration.
Bronchodilators
- Albuterol is often administered as a metered-dose inhaler (MDI), dry powder inhaler (DPI), or nebulized solution when the patient does not respond to epinephrine for the treatment of bronchospasm.
- Albuterol MDI or DPI dosing (90 mcg/actuation): Adults should provide 2 to 3 inhalations as needed for symptom alleviation; during severe exacerbations, up to 8 inhalations every 20 minutes may be required. Although the paediatric dose is 4 to 8 puffs every 20 minutes for up to 3 doses, data for kids 4 years is limited.
- Albuterol nebulization solution: (2.5 to 5 mg as needed) The nebulized solution can also be administered continuously to critically ill adult and paediatric patients at a rate of 10 to 14 mg per hour.
Antihistamines: i.e., diphenhydramine (H1 antagonist), famotidine or ranitidine (H2 antagonists)
- Antihistamines are considered second-line adjunctive therapy and can provide relief of symptoms such as hives or pruritis. However, antihistamines should not be used as monotherapy, as they do not mitigate upper or lower airway obstruction, shock, or hypotension. Although antihistamines are usually used in combination with both an H1 antagonist and an H2 antagonist in anaphylaxis, there is a lack of direct evidence to support their administration. Second-generation H1 antagonists have fewer sedative effects than first-generation agents, and as such, they may also be considered. Some studies suggest that when H2 antagonists are given intravenously (IV), they can increase hypotension.
- Diphenhydramine IV dose: 25 to 50 mg per dose in adult patients and 1 to 2 mg/kg/dose in pediatrics (maximum 50 mg/dose); dose may be repeated every 6 hours.
- Ranitidine oral (PO) or IV: 1 to 2 mg/kg per dose (maximum 75 to 150 mg of oral and IV in adults and a maximum of 50 mg/dose in pediatrics).
- Famotidine IV: 20 mg diluted to 5 ml 0.9% normal saline and pushed over two minutes in adults and 0.25 mg/kg (maximum 20 mg per dose) in pediatrics.
Glucocorticoids
- Due to their delayed start of effect, glucocorticoids do not have an acute role in the treatment of anaphylaxis, and there are no randomised, controlled trials that demonstrate the benefits of their use. However, the theoretical justification for its use is to reduce biphasic or prolonged anaphylactic reactions.
- Methylprednisolone: 1 to 2 mg/kg/day (maximum of 125 mg per dosage) for one to two days without tapering.
Additional adjuvant therapy for anaphylaxis include supplementary oxygenation, intravenous fluids for volume replacement, glucagon or vasopressors for refractory hypotension, and/or atropine for bradycardia. Ideally, the following parameters should be evaluated continuously or regularly during and after anaphylaxis: blood pressure, respiratory status, oxygenation, urine output, cardiac function, and heart rate.
B. Urticaria/Angioedema
- Treatment of urticaria is similar to anaphylaxis where the offending chemical is removed if identified, and then the patient is given an H1 antihistamine and glucocorticoids (see above for dose) (see above for dosing).
- There is not a need for epinephrine unless there is suspicion for anaphylaxis.
- Patients with chronic urticaria who are unresponsive to H1 antihistamines may benefit from omalizumab, which is a monoclonal antibody that blocks the binding of IgE to receptors on mast cells and basophils, or cyclosporine, which is an immunomodulator.
C. Allergic Asthma/Allergic Rhinitis/ Allergic Conjunctivitis/Allergic Dermatitis/Eczema/Wasp or bee venom/Drug Allergy/Food Allergy
- For allergic diseases, avoidance of the offending agent is the initial step in treatment. Oral or topical H1 antihistamine and oral or inhalation glucocorticoids may be used for symptomatic management.
- For allergic rhinitis, topical nasal or ocular decongestants can provide temporary relief of symptoms.
- For allergic asthma, patients can be provided inhaled beta-agonists with or without inhaled corticosteroids based on phases of asthma therapy recommended by the National Heart, Lung, and Blood Institute.
- Patients with considerable symptoms despite avoidance of the allergen and who have a lack of remission from adjunctive therapy can undergo allergen immunotherapy, such as desensitisation or hypo-sensitization (allergy injections).
- The patient must have a verified IgE-mediated allergy (allergic: asthma, rhinitis, conjunctivitis, dermatitis, drug allergy) prior to beginning of immunotherapy.
- The treatment is carried out in a clinical setting for the first doses, where particular allergens are supplied in a slow escalation of subclinical dosages.
- The route of delivery is either via subcutaneous immunotherapy (SCIT), sublingual/sallow immunotherapy (SLIT), or mucosal route.
- The purpose of desensitisation is to increase the synthesis of immunoglobulin G (IgG) antibodies on mast cells instead of IgE.
- This procedure is called as isotype swapping and normally lasts for three years. Desensitization treatment is successful in about 67% of patients and is usually more useful in younger individuals and those who have a sensitivity to a monovalent allergen.
- Patients need to be prescribed and instructed on the proper use of epinephrine autoinjectors prior to the commencement of immunotherapy.
Examples of Type I hypersensitivity
Type I hypersensitivity, also known as immediate hypersensitivity or allergic hypersensitivity, is characterized by an exaggerated immune response mediated by immunoglobulin E (IgE) antibodies. This immune response can lead to a wide range of allergic conditions. Here are some examples of Type I hypersensitivity:
- Allergic asthma: This condition involves the inflammation and narrowing of the airways in response to specific allergens, such as pollen, dust mites, or pet dander. It leads to symptoms like wheezing, coughing, shortness of breath, and chest tightness.
- Allergic conjunctivitis: Allergic conjunctivitis refers to inflammation of the conjunctiva, the clear tissue covering the white part of the eye and the inner surface of the eyelids. It is often triggered by allergens like pollen, dust, or pet dander, resulting in redness, itching, and watery eyes.
- Allergic rhinitis (“hay fever”): Allergic rhinitis is an allergic reaction affecting the nasal passages. It is commonly triggered by airborne allergens like pollen, dust mites, or mold spores. Symptoms include sneezing, itching, a runny or congested nose, and postnasal drip.
- Anaphylaxis: Anaphylaxis is a severe and potentially life-threatening allergic reaction that can occur within seconds or minutes of exposure to an allergen. It can manifest with symptoms such as difficulty breathing, wheezing, swelling, hives, dizziness, and a drop in blood pressure. Anaphylaxis requires immediate medical attention.
- Angioedema: Angioedema is a condition characterized by the rapid swelling of deep layers of the skin, typically affecting the face, lips, tongue, throat, or genitals. It can be caused by allergens, medications, or inherited factors and may accompany hives or occur independently.
- Urticaria (hives): Urticaria, commonly known as hives, is characterized by itchy, raised, and often red welts on the skin. Hives can be triggered by various factors, including allergens, medications, infections, or physical stimuli like pressure or temperature changes.
- Eosinophilia: Eosinophilia refers to an increased number of eosinophils, a type of white blood cell, in the blood or tissues. It can occur as a result of allergic conditions, such as asthma or parasitic infections.
- Penicillin allergy and Cephalosporin allergy: Allergies to specific antibiotics, such as penicillin or cephalosporins, are common examples of Type I hypersensitivity reactions. They can manifest as a range of symptoms, from mild skin rashes to severe systemic reactions like anaphylaxis.
- Food allergy: Food allergies involve an immune response to specific proteins present in certain foods. Common food allergens include peanuts, tree nuts, shellfish, eggs, milk, and soy. Food allergies can lead to a wide range of symptoms, ranging from mild oral itching to severe anaphylaxis.
- Sweet itch: Sweet itch, also known as summer itch or equine insect hypersensitivity, is an allergic reaction to the bites of certain insects, particularly midges. It primarily affects horses and causes itching, skin lesions, and hair loss.
These examples highlight the diverse manifestations of Type I hypersensitivity, reflecting the body’s immune response to different allergens. Proper diagnosis and management, including allergen avoidance, medications, and in some cases, immunotherapy, are important for individuals with Type I hypersensitivity conditions.
FAQ
What is Type I hypersensitivity reaction?
Type I hypersensitivity reaction, also known as immediate hypersensitivity or allergic hypersensitivity, is an exaggerated immune response triggered by the release of immunoglobulin E (IgE) antibodies in response to exposure to specific allergens.
What are the symptoms of Type I hypersensitivity?
The symptoms of Type I hypersensitivity can vary depending on the specific allergic condition, but common symptoms include itching, hives, nasal congestion, sneezing, runny nose, watery eyes, wheezing, coughing, shortness of breath, swelling, and in severe cases, anaphylaxis.
How is Type I hypersensitivity diagnosed?
Diagnosis of Type I hypersensitivity often involves a combination of clinical evaluation, medical history, and allergy testing. Allergy testing methods may include skin prick tests, blood tests for specific IgE antibodies, or in some cases, oral food challenges.
What causes Type I hypersensitivity?
Type I hypersensitivity is caused by the immune system’s response to allergens such as pollen, dust mites, pet dander, certain foods, insect venom, or medications. These allergens trigger the production of IgE antibodies, leading to the release of inflammatory substances like histamine.
Can Type I hypersensitivity be prevented?
Prevention of Type I hypersensitivity involves identifying and avoiding exposure to known allergens. For example, individuals with pollen allergies can limit outdoor activities during high pollen seasons, use air filters in their homes, and keep windows closed. Food allergies can be managed by reading food labels, avoiding cross-contamination, and being cautious while dining out.
How is Type I hypersensitivity treated?
Treatment for Type I hypersensitivity typically involves the use of medications to alleviate symptoms. These may include antihistamines to reduce itching and allergic reactions, nasal sprays to manage nasal congestion, bronchodilators for respiratory symptoms, and in severe cases, epinephrine (adrenaline) for anaphylaxis.
Can Type I hypersensitivity be cured?
There is no known cure for Type I hypersensitivity. However, symptoms can be effectively managed through avoidance of allergens, proper medical treatment, and, in some cases, allergen immunotherapy (allergy shots) to desensitize the immune system.
Are allergies and Type I hypersensitivity the same thing?
Allergies are a broad term that encompasses various types of hypersensitivity reactions, including Type I hypersensitivity. Type I hypersensitivity is specifically characterized by the production of IgE antibodies and an immediate allergic response upon re-exposure to specific allergens.
Can Type I hypersensitivity develop at any age?
Type I hypersensitivity can develop at any age. Some individuals may develop allergies in childhood and outgrow them later in life, while others may develop new allergies as adults. The tendency to develop allergies can be influenced by genetic factors and environmental exposures.
Are Type I hypersensitivity reactions life-threatening?
Type I hypersensitivity reactions can range from mild to severe, with the potential for life-threatening complications in certain cases. Anaphylaxis, a severe and potentially fatal allergic reaction, is a serious manifestation of Type I hypersensitivity that requires immediate medical attention and treatment with epinephrine.
References
- Abbas M, Moussa M, Akel H. Type I Hypersensitivity Reaction. [Updated 2022 Jul 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560561/
- King, T. C. (2007). Inflammation, Inflammatory Mediators, and Immune-Mediated Disease. Elsevier’s Integrated Pathology, 21–57. doi:10.1016/b978-0-323-04328-1.50008-5
- Sheldon, J., Wheeler, R. D., & Riches, P. G. (2014). Immunology for clinical biochemists. Clinical Biochemistry: Metabolic and Clinical Aspects, 560–603. doi:10.1016/b978-0-7020-5140-1.00030-4
- Actor, J. K. (2012). Adaptive Immune Response and Hypersensitivity. Elsevier’s Integrated Review Immunology and Microbiology, 53–59. doi:10.1016/b978-0-323-07447-6.00007-7
- Salmon, J. E. (2012). Mechanisms of Immune-Mediated Tissue Injury. Goldman’s Cecil Medicine, 226–230. doi:10.1016/b978-1-4377-1604-7.00046-4
- Sykes, J. E. (2014). Immunization. Canine and Feline Infectious Diseases, 119–130. doi:10.1016/b978-1-4377-0795-3.00012-0
- https://www.lecturio.com/concepts/type-i-hypersensitivity-reaction/
- https://labpedia.net/elementary-immunology/chapter-11-type-1-hypersensitivity-reaction-anaphylaxis-atopy-and-treatment/
- https://www.osmosis.org/learn/Type_I_hypersensitivity
- https://njms.rutgers.edu/sgs/olc/mci/prot/2009/Hypersensitivities09.pdf
- https://webpath.med.utah.edu/IMMHTML/IMM101.html
- https://www.onlinebiologynotes.com/type-i-hypersensitivity-reaction-mechanism-and-clinical-manifestation/
- https://calgaryguide.ucalgary.ca/type-i-hypersensitivity-pathogenesis-and-clinical-findings/
- https://www.microbiologybook.org/mobile/m.immuno-17.htm
- https://veteriankey.com/type-i-hypersensitivity/
- https://microbenotes.com/type-1-anaphylactic-hypersensitivity-reaction/
- https://en.wikipedia.org/wiki/Type_I_hypersensitivity
- https://portal.fmed.uniba.sk/articles.php?aid=197
- http://www.jiwaji.edu/pdf/ecourse/microbiology/Hypersensitivity%20Type%20I%20%20for%20MSc%202%20sem.%20Microbiology.pdf
- https://gpnotebook.com/simplepage.cfm?ID=127533068