What is Treponema Pallidum?
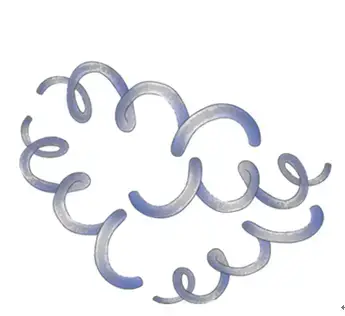
- Treponema pallidum subsp. pallidum, a member of the Treponema genus, is a microaerophilic bacterium situated within the spirochetal order. This bacterium is distinguished by its helical coil structure, typically measuring between 6–15 μm in length and 0.1–0.2 μm in width. One of its defining characteristics is its thick phospholipid membrane, which encapsulates the organism.
- Metabolically, T. pallidum exhibits a notably slow rate of activity. Lacking both a tricarboxylic acid cycle and oxidative phosphorylation, its metabolic functions are considerably limited. This results in a prolonged multiplication time, with the bacterium requiring approximately thirty hours for replication. Despite its slow metabolic rate, T. pallidum is a formidable pathogen, particularly challenging to eradicate.
- Historically referred to as Spirochaeta pallida, T. pallidum has multiple subspecies, each associated with distinct diseases. These subspecies include T. p. pallidum, T. p. endemicum, and T. p. pertenue.
- The primary disease attributed to T. p. pallidum is syphilis, a sexually transmitted infection. Meanwhile, T. p. endemicum and T. p. pertenue are responsible for bejel (or endemic syphilis) and yaws, respectively.
- One of the intriguing features of T. pallidum is its invisibility under light microscopy. To visualize this bacterium, researchers employ dark-field illumination techniques. This is primarily due to the unique structural properties of the treponemes, which comprise both a cytoplasmic and an outer membrane.
- In conclusion, Treponema pallidum is a bacterium of significant medical importance, especially given its role in causing syphilis. Its unique structural and metabolic characteristics make it a subject of continued scientific interest and study.
Definition of Treponema Pallidum
Treponema pallidum is a helical, microaerophilic bacterium responsible for causing syphilis, a sexually transmitted disease, and other related diseases such as bejel and yaws. It is characterized by its slow metabolic rate and is best visualized using dark-field microscopy.
What is Syphilis?
- Syphilis is a chronic human ailment primarily transmitted through sexual contact or vertically from an infected mother to her offspring during childbirth. This disease, often dubbed ‘The Great Pretender’, can manifest a range of symptoms that mimic other conditions, making its diagnosis challenging.
- The initial manifestation of syphilis is the chancre, a firm, round ulceration that appears at the primary site of infection. Due to its potential location in concealed areas like the vagina, mouth, throat, or anus, its early detection can be elusive. Such lesions, especially when internal, are often identified during routine clinical screenings. Populations with limited access to healthcare might overlook these primary syphilitic lesions, continuing their sexual activities and possibly childbearing without proper diagnosis or treatment.
- A chancre, though self-resolving within a month without intervention, is a crucial indicator. Initiating treatment during this primary phase is imperative to prevent the disease’s progression to its secondary stage.
- The secondary phase is marked by a distinct rash, typically rough and reddish or brownish, predominantly appearing on the soles and palms. However, it can manifest elsewhere on the body. Another hallmark of this stage is the emergence of larger lesions, termed condyloma lata, in moist regions like the armpits, mouth, and groin. Accompanying symptoms such as hair loss, swollen lymph nodes, headaches, and fatigue make medical consultation more frequent during this phase.
- Following the secondary stage, syphilis enters the latent phase, a symptom-free period where the causative bacterium, Treponema pallidum, remains in the body. Despite the absence of overt symptoms, individuals remain infectious, especially during sexual interactions or childbirth in the case of infected females. The latent stage can span several years, and its asymptomatic nature often dissuades individuals from seeking medical attention.
- If untreated, syphilis progresses to the tertiary stage, which can be life-threatening. At this juncture, T. pallidum colonizes various body regions, leading to extensive damage. The tertiary stage is categorized based on the affected area, such as neurosyphilis, cardiovascular syphilis, and ocular syphilis, among others. The disease’s ability to produce a myriad of symptoms across different body systems earned it the moniker ‘The Great Pretender’.
- Upon exposure to T. pallidum, the human immune system mounts specific responses. Typically, T-cell-mediated delayed-type hypersensitivity reactions are activated, leading to T-cell infiltration at the inoculation sites. These cells then stimulate macrophages to eliminate the treponemes through phagocytosis. However, T. pallidum has evolved mechanisms to evade this immune response, allowing it to persist and cause disease.
Classification of Treponema Pallidum
Treponema pallidum is a spirochetal bacterium that belongs to the genus Treponema. Within this genus, there are several subspecies and related organisms, each responsible for distinct diseases in humans. The classification of these organisms is based on their genetic, morphological, and pathological characteristics.
- Treponema pallidum subspecies pallidum: This is the causative agent of syphilis, a sexually transmitted disease with a global prevalence.
- Treponema pallidum subspecies pertenue: This subspecies is responsible for yaws, a tropical infection primarily affecting the skin, bones, and joints.
- Treponema pallidum subspecies endemicum: This organism leads to bejel, also known as endemic syphilis. Unlike the sexually transmitted form, bejel is primarily transmitted through close personal contact and is common in arid regions.
- Treponema carateum: This is the causative agent for pinta, a skin disease prevalent in Central and South America. It is noteworthy that T. carateum is currently designated as a separate subspecies, primarily due to the limited understanding of its genetic makeup.
Despite the differences in the diseases they cause, these pathogenic treponemes are remarkably similar. Morphologically, they are indistinguishable, showcasing the same spiral-shaped structure characteristic of spirochetes. On a genetic level, they share a high degree of DNA sequence homology, with an approximate 95% similarity as per hybridization studies (Fieldsteel & Maio, 1982). Furthermore, protein profiles across these subspecies are closely correlated, and they exhibit similar reactivity patterns when exposed to monoclonal antibodies.
In summary, the genus Treponema houses several subspecies and related organisms, each associated with specific human diseases. While they cause different conditions, these pathogenic treponemes are genetically and morphologically very similar, underscoring the importance of precise diagnostic tools in clinical settings.
Epidemiology of Treponema Pallidum
Treponema pallidum, the causative agent of syphilis, has a rich historical backdrop intertwined with global events and societal shifts. The disease, believed to have been brought to the Old World by Christopher Columbus and his crew, had firmly established its presence in Europe by the 17th century. Subsequent centuries witnessed several epidemic surges, with notable peaks during the Napoleonic wars, the industrialization era of the 19th century, and the two world wars in the 20th century.
By the 1970s, the epidemiological landscape of syphilis underwent a significant shift in North America and northern Europe, where it predominantly affected gay men. However, the late 1980s saw a resurgence in heterosexual and congenital syphilis cases, coinciding with the HIV epidemic. Despite concerted efforts, such as the National Plan to Eliminate Syphilis, the disease’s incidence did not sustainably decrease. In 2013, the USA reported a rate of 5.3 primary and secondary syphilis cases per 100,000 population, marking a significant increase from the lowest recorded rate of 2.1 in 2000. Men constituted over 90% of these cases, with 83% of early syphilis diagnoses in 2012 being among men who have sex with men (MSM). Alarmingly, up to 70% of these MSM might also be co-infected with HIV. The racial dimension of the disease’s prevalence is also noteworthy, with black men and women having significantly higher rates than their white counterparts.
The UK’s syphilis statistics from 2012 echo the US trends, with 3,316 early syphilis cases diagnosed, marking a 1% increase from the previous year. Over 90% of these cases were in men, with 80% being MSM.
Congenital syphilis, which affects infants, has also seen fluctuations in its incidence. In the USA, the annual incidence skyrocketed from 3.0 per 100,000 live births in 1980 to 107.3 in 1990. However, this dramatic increase was partly due to the introduction of a new reporting system. Post-2008, there was a decline in congenital syphilis rates, mirroring the decrease in primary and secondary syphilis among women.
On a global scale, the World Health Organization (WHO) estimated an annual syphilis incidence of approximately 12.2 million cases. The majority of these cases are found in resource-limited countries, where syphilis remains a significant cause of genital ulcer disease, stillbirths, and neonatal morbidity and mortality. In 2008, an estimated 1.4 million pregnant women worldwide had active syphilis, leading to 521,000 adverse outcomes, including stillbirths, neonatal deaths, pre-term births, and infected newborns.
In conclusion, the epidemiology of Treponema pallidum is complex and multifaceted, influenced by societal, historical, and geographical factors. Continuous monitoring, effective interventions, and global cooperation are imperative to manage and eventually eradicate this persistent disease.
Transmission of Treponema Pallidum
Treponema pallidum, the causative agent of syphilis, primarily spreads through direct contact with early mucocutaneous lesions. The transmission routes and their implications are as follows:
- Sexual Transmission: The bacterium predominantly enters the human body through minor disruptions in the epithelial surfaces found in genital, anorectal, oropharyngeal, and other cutaneous sites. The likelihood of transmitting syphilis to an uninfected partner during the early stages of the disease is notably high, with estimates suggesting a transmission probability of around 60%, though this can vary between 9% to 80%.
- Blood and Needle Sharing: While syphilis is primarily a sexually transmitted disease, there are rare instances where it can be transmitted through blood transfusion or sharing needles among intravenous drug users. However, these modes of transmission are considerably less common than sexual contact.
- Prenatal Transmission: Maternal transmission of Treponema pallidum to the fetus is particularly concerning. The risk of transmission is highest when the mother has a recent infection, but transmission can also occur during the latent stages of the disease. Manifestations of congenital syphilis in the fetus are uncommon before 18 weeks of gestation. The peak incidence of stillbirths attributed to congenital syphilis occurs between 6 to 8 months of gestation. Intriguingly, even if a woman has previously given birth to an uninfected child, subsequent pregnancies can result in offspring with congenital syphilis. Moreover, in the case of twins, it’s possible for only one twin to be affected. Fortunately, congenital syphilis is preventable through appropriate maternal treatment during pregnancy.
In conclusion, while sexual transmission remains the primary route for the spread of Treponema pallidum, other modes, including prenatal transmission, underscore the importance of early detection and treatment. Proper medical interventions can significantly reduce the risk of transmission and the associated complications.
Structure of Treponema Pallidum
Treponema pallidum, the causative agent of syphilis, possesses a distinctive structural morphology that plays a pivotal role in its pathogenicity. A detailed examination of its structure reveals the following features:
- Morphology: The bacterium exhibits a spiral shape, with a length ranging from 6 to 20 µm and a diameter of approximately 0.18 µm. This tight helical structure comprises 6 to 14 helices per cell. Upon fixation, the organism manifests a wave-like appearance, characterized by a wavelength of 1.1 µm and an amplitude between 0.2 and 0.3 µm.
- Motility: Under dark-field microscopy, fresh specimens of T. pallidum display a unique corkscrew motility. This rapid rotation around its axis is attributed to the action of flagellae, which are inserted at both ends of the bacterium and extend within the periplasmic space. The organism also exhibits flexion and reversal of rotation, characteristics that are considered distinctive of pathogenic treponemes (Clarkson, 1956).
- Flagellae: The flagellae of T. pallidum are intricate in their composition. They consist of three core proteins and a distinct sheath protein.
- Membranes: The bacterium is enveloped by an outer membrane that contains a limited number of transmembrane proteins, which are poorly immunogenic (Radolf, 1995). Directly beneath this outer membrane is a peptidoglycan layer, followed by a cytoplasmic membrane. Embedded within the periplasmic leaflet of the cytoplasmic membrane are highly immunogenic lipoproteins. Although their exact function remains uncertain, these lipoproteins are believed to be instrumental in eliciting immune responses during infection (Radolf, 1995).
- Genome: Insights from the Genome Sequencing Project completed in 1998 revealed that T. pallidum possesses a relatively small genome when compared to many other bacterial species.
In summary, the structural intricacies of Treponema pallidum, from its helical morphology to its unique flagellae and membrane components, underscore its adaptive capabilities and pathogenic potential. Understanding these structural details is crucial for deciphering the bacterium’s interactions with the host and its mechanisms of causing disease.
Genome of Treponema Pallidum
- Treponema pallidum, the causative agent of syphilis, possesses a relatively small chromosome, approximately 1.14 Mbp in size. The DNA sequences of the T. pallidum subspecies exhibit a striking similarity, with over 99.7% identical sequences. This high degree of genetic conservation underscores the close relationship among these subspecies.
- The sequencing of T. p. pallidum in 1998 marked a significant milestone in the study of this bacterium. Given the organism’s inability to grow in a pure culture, genome sequencing provided invaluable insights into its functional attributes. One of the intriguing revelations from the genomic data is the bacterium’s dependence on its host for numerous molecules, which are typically produced via biosynthetic pathways. This dependence is further exemplified by the absence of genes encoding crucial enzymes involved in oxidative phosphorylation and the tricarboxylic acid cycle. Notably, approximately 5% of T. pallidum’s genes are dedicated to coding for transport genes.
- Comparative genomic analyses, facilitated by the sequencing of various spirochetes, offer a comprehensive understanding of the similarities and differences both within this bacterial phylum and the species. T. p. pallidum’s genome, being one of the smallest among bacteria, reflects its evolutionary adaptation through genome reduction, optimizing its survival in the nutrient-rich milieu of mammalian tissues.
- Morphologically, T. pallidum is characterized by a flat, wavy structure. Its survival strategy in the host involves minimizing exposure to the host’s immune system. This is achieved by having a limited number of proteins on its outer membrane sheath, thereby reducing the chances of antibody-mediated attacks.
- The bacterium’s chromosome is circular, with a G + C content averaging 52.8%. This compact genome, comprising about 1000 kilobase pairs, is predominantly occupied by open reading frames, accounting for approximately 92.9% of its DNA. Of these, 55% have predicted biological functions. Furthermore, the genome has revealed a set of 12 proteins and potential hemolysins, which are believed to be potential virulence factors, underscoring the bacterium’s pathogenic capabilities.
- In summary, the genome of Treponema pallidum provides a window into its evolutionary adaptations, metabolic limitations, and strategies for survival within its host, offering a foundation for understanding its pathogenicity and potential therapeutic interventions.
Treponema Pallidum Antigens
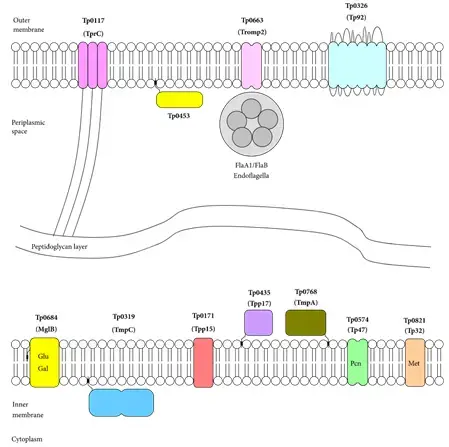
Several inner membrane lipoproteins of T. pallidum have been identified, including Tp15, Tp17, Tp47, TmpA, TmpC, Tp38, and Tp32. Additionally, other proteins such as the surface-exposed Tp0453, the putative periplasmic protein TpF1, and flagellar proteins like FlaB1 have been recognized.
- Tp17: Structurally, Tp17 is an eight-stranded β-barrel protein. It features a shallow basin on one end and an α-helix on the opposite end. This structure suggests its potential role in protein ligand binding, maintenance of treponemal membrane architecture, or syphilis pathogenesis. Notably, Tp17 has been implicated in the activation of genes like ICAM-1, E-selectin, and MCP-1 in endothelial cells.
- Tp47: Tp47 functions as a carboxypeptidase and is identified as a significant penicillin-binding protein of T. pallidum. It is involved in the host-pathogen interaction, stimulating microvessel endothelial cells to produce intercellular adhesion molecules and inducing the synthesis of vascular cell adhesion molecules.
- Tp0453: This protein, associated with the outer membrane, enhances membrane permeability.
- TpF1: TpF1 has a central role in modulating the immune response. It influences the release of specific cytokines by monocytes, thereby driving a suppressive immune reaction.
In conclusion, Treponema pallidum, with its unique structural and pathogenic features, remains a subject of intense study. The identified antigens play pivotal roles in the bacterium’s interaction with the host, offering potential targets for therapeutic interventions.
Pathogenesis and Pathology of Treponema Pallidum
Treponema pallidum is a microaerophilic bacterium, possessing a distinctive wave-like cell body that measures 6–15µm in length and 0.15–0.20µm in width. Its periplasmic flagellum gives it a characteristic movement, which can be observed under darkfield microscopy. The bacterium has a slow growth rate, with an optimal temperature range of 91–95°F (33–35°C) and a doubling time of 30–36 hours. Due to its extreme nutritional requirements and deficiencies in biosynthetic pathways, it cannot be cultured on artificial media. However, it can be propagated in organ cultures, such as rabbit testis.
Upon entering the host, Treponema pallidum triggers an inflammatory response at the site of inoculation. It rapidly disseminates, with studies in animals showing its presence in lymph nodes and blood within minutes. Remarkably, within 18 hours post-inoculation, the bacterium can be detected in the cerebrospinal fluid (CSF) of rabbits. It employs various strategies to invade deeper tissues, such as inducing the production of matrix metalloproteinase-1 in dermal cells. Furthermore, it activates endothelial cells, prompting the migration of inflammatory and immune cells to the site of infection.
Immune Response: The host’s immune system responds swiftly to the invasion of T. pallidum. Polymorphonuclear lymphocytes are among the first to arrive at the infection site, although their presence is transient. The bacterium’s microbial patterns are recognized by Toll-like receptor (TLR)-2, which plays a pivotal role in mediating the innate immune response. Dendritic cells, stimulated via the TLR2 pathway, phagocytize the bacteria and migrate to lymph nodes, where they activate T cells. Additionally, T. pallidum components stimulate macrophages to produce tumor necrosis factor (TNF) and other proinflammatory cytokines, amplifying the immune response. The humoral immune response produces IgM and IgG antibodies specific to a wide array of T. pallidum surface molecules. These antibodies can immobilize the bacteria and neutralize their pathogenicity, although they are not treponemicidal. Approximately two weeks post-infection, the bacterial count within lesions starts to decline significantly.
Evasion Mechanisms: T. pallidum has evolved several strategies to evade the host’s immune response:
- Antigenic Inertness: The surface of T. pallidum is antigenically inert, making it less recognizable to the host’s immune system.
- Low Antigenic Mass: The number of bacteria causing the disease is below the ‘critical antigenic mass’ required to stimulate a strong immune response.
- Invasion of Immune-Privileged Sites: T. pallidum can invade sites where the immune response is limited.
- Slow Generation Time: The bacterium’s slow growth rate can hinder the host’s ability to mount a rapid immune response.
- Bypassing Iron-Sequestration: T. pallidum can circumvent the host’s mechanisms that sequester iron, a vital nutrient for many pathogens.
Diagnosis of Treponema Pallidum
The diagnosis of Treponema pallidum, the causative agent of syphilis, is multifaceted, encompassing microscopic identification, serologic testing, cerebrospinal fluid examination, and neonatal evaluation.
- Microscopic Identification:
- Darkfield Microscopy: This is the gold-standard for diagnosing genital chancres of primary syphilis. It can identify T. pallidum from genital lesions, with serologic tests potentially being negative in up to 30% of patients. However, its specificity is reduced for oral or rectal mucosal lesions due to the presence of nonpathogenic treponemes.
- Direct Immunofluorescent Antibody Testing: This method is an alternative when darkfield microscopy is unavailable.
- Silver Stains and Immunofluorescent Testing: These can be used on biopsy specimens from late syphilis or atypical early lesions.
- Polymerase Chain Reaction (PCR): Though not routinely available, PCR can be used for diagnosis, targeting the 47 kDa gene.
- Serologic Testing:
- Standard Non-Treponemal Tests: These tests detect IgM and IgG antibodies to lipoidal materials from damaged host cells and T. pallidum. Examples include the VDRL slide test and the rapid plasma reagin (RPR) test. These tests are quantitative and can assess response to treatment. However, biologic false-positive reactions can occur in various conditions.
- Specific Treponemal Antibody Tests: Used for confirmatory testing, these tests detect IgG and sometimes IgM antibodies specific to treponemes. Examples include the fluorescent treponemal antibody absorption (FTA-ABS) test, the microhemagglutination assay (MHA-TP), and the T. pallidum particle agglutination (TPPA) test. Newer automated tests, such as enzyme immunoassays (EIA) and chemiluminescence assays (CIA), are also available.
- Syphilis Serologic Testing Algorithms: Testing can begin with a non-treponemal test followed by a confirmatory treponemal test or vice versa. Patients with serodiscordant results require a thorough history to determine the next steps.
- Examination of Cerebrospinal Fluid (CSF):
- Indications for CSF examination include the presence of neurologic, ophthalmic, or auditory symptoms; clinical evidence of active infection; or serologic failure post-therapy. In HIV-infected individuals, especially with certain clinical parameters, CSF examination may be considered.
- Typical CSF findings in neurosyphilis include mononuclear pleocytosis, elevated total protein, and a positive CSF VDRL. However, a negative CSF non-treponemal antibody test does not exclude neurosyphilis. Neuroimaging can also provide insights into neurosyphilis.
- Evaluation of Neonates for Congenital Syphilis:
- Neonates born to seropositive mothers, especially under certain conditions, should undergo a physical examination, radiography of long bones, CSF examination, and darkfield microscopic examination of suspicious lesions or body fluids. Infection in neonates can also be indicated if the serum non-treponemal antibody titer is significantly higher than the mother’s or if specific IgM treponemal antibody tests are positive.
In summary, the diagnosis of Treponema pallidum infection requires a combination of microscopic, serologic, and clinical evaluations. Proper diagnostic procedures are essential for timely and effective treatment.
Clinical Features of Treponema Pallidum
Treponema pallidum is the causative agent of syphilis, a sexually transmitted infection with a multifaceted clinical presentation. The clinical manifestations of syphilis can be categorized into primary, secondary, latent, tertiary, congenital, and its association with HIV infection.
- Primary Syphilis:
- Incubation Period: Following transmission, primary lesions appear after an average of 21 days, with the duration inversely proportional to the size of the spirochete inoculum.
- Chancre Formation: The primary chancre, a hallmark of this stage, emerges at the site of treponemal invasion of the dermis. These lesions, initially papular, soon ulcerate. They are typically singular, non-tender, indurated ulcers with a clean base and raised edges. Accompanying these are non-tender, rubbery inguinal lymphadenopathy, which becomes bilateral after two weeks.
- Secondary Syphilis:
- General Symptoms: Roughly 8 weeks post-infection, patients may experience fever, headache, and musculoskeletal pain.
- Dermatological Manifestations: Skin rashes, initially macular, become papular within three months. These rashes, often coppery in hue, can appear on the upper trunk, palms, soles, and extremities’ flexural surfaces. Other manifestations include condylomata lata in moist areas and mucous patches in the oral cavity.
- Systemic Features: These encompass panuveitis, periostitis, joint effusions, glomerulonephritis, hepatitis, gastritis, myocarditis, and aseptic meningitis.
- Latent Syphilis: This phase is characterized by an absence of clinical signs of active disease, though serologic tests remain positive. Early latency can see up to 25% of asymptomatic patients experiencing secondary relapses.
- Tertiary Gummatous Syphilis: Occurring 3-10 years post-infection, this stage is marked by the presence of granulomas or gummas. These granulomas can manifest as cutaneous plaques or nodules. Gummas, on the other hand, are granulomatous tissues prone to central necrosis, ulceration, and peripheral healing.
- Cardiovascular Syphilis: This involves aortitis affecting the ascending aorta, manifesting 10-30 years after infection. It can lead to aortic valve incompetence, left ventricular failure, or aneurysm formation.
- Neurosyphilis: The central nervous system is invaded by treponemes early post-infection. Clinical presentations are diverse, ranging from asymptomatic neurosyphilis to meningeal, meningovascular, gummatous, and parenchymatous neurosyphilis.
- Congenital Syphilis: Infants may be asymptomatic at birth, but early manifestations include rhinitis, vesiculobullous skin eruptions, and bone abnormalities. Late congenital syphilis can lead to skeletal developmental defects, dental abnormalities, and other gummatous and neurosyphilitic lesions.
- Syphilis and HIV Infection: A significant proportion of syphilis patients in the USA and the UK are coinfected with HIV. The coexistence of these infections can alter the clinical presentation and progression of syphilis.
In conclusion, Treponema pallidum induces a wide spectrum of clinical manifestations, necessitating a comprehensive understanding for accurate diagnosis and management.
Prevention of Treponema Pallidum
Here are some strategies to prevent the spread of this bacterium:
- Safe Sex:
- Use Condoms: While condoms do not provide 100% protection against syphilis, they significantly reduce the risk of transmission when used correctly and consistently.
- Limit Number of Sexual Partners: Reducing the number of sexual partners can decrease the risk of exposure.
- Know Your Partner’s STI Status: Before engaging in sexual activity, discuss your and your partner’s STI status and testing history.
- Regular Medical Check-ups:
- Get Tested: Regularly get tested for syphilis, especially if you have multiple sexual partners or are in a high-risk group. Early detection can prevent complications and further spread.
- Pregnancy: Pregnant women should be tested for syphilis during their first prenatal visit. If positive, they should receive treatment to prevent transmission to the baby.
- Avoid Drug Use: Sharing needles or engaging in risky sexual behaviors while under the influence can increase the risk of acquiring syphilis and other STIs.
- Education:
- Awareness: Understand the symptoms and stages of syphilis. Early-stage syphilis can manifest as sores, while later stages can have more systemic symptoms.
- Public Health Campaigns: Public health initiatives can raise awareness about syphilis and promote safe sexual practices.
- Treatment:
- Follow Treatment Protocols: If diagnosed with syphilis, it’s crucial to complete the entire course of antibiotics, usually penicillin, as prescribed by a healthcare provider.
- Notify Partners: If you’re diagnosed with syphilis, inform your recent sexual partners so they can get tested and treated if necessary.
- Avoid Contact with Sores: Syphilis can be transmitted through direct contact with a syphilis sore or rash. Avoiding contact with these sores can prevent transmission.
- Regular Screenings for High-risk Groups: Certain populations, such as men who have sex with men (MSM) or individuals with HIV, may be at a higher risk for syphilis. Regular screenings can help detect and treat syphilis early in these populations.
By following these preventive measures, the transmission of Treponema pallidum and the incidence of syphilis can be reduced.
Quiz
What is the causative agent of syphilis?
a) Escherichia coli
b) Staphylococcus aureus
c) Treponema pallidum
d) Mycobacterium tuberculosis
Which microscopy technique is considered the gold standard for diagnosing genital chancres of primary syphilis?
a) Electron microscopy
b) Darkfield microscopy
c) Light microscopy
d) Fluorescence microscopy
Which of the following is NOT a stage of syphilis?
a) Primary
b) Secondary
c) Tertiary
d) Quaternary
Approximately how large is the chromosome of T. pallidum?
a) 1.14 Mbp
b) 2.5 Mbp
c) 3.0 Mbp
d) 4.2 Mbp
Which test detects IgM and IgG antibodies to lipoidal materials from damaged host cells and T. pallidum?
a) FTA-ABS test
b) PCR
c) VDRL slide test
d) ELISA
The shape of T. pallidum is described as:
a) Spherical
b) Rod-shaped
c) Flat and wavy
d) Spiral
Which year was the genome of T. p. pallidum sequenced?
a) 1985
b) 1992
c) 1998
d) 2005
T. pallidum is known to evade the host’s immune response by:
a) Rapid replication
b) Producing toxins
c) Having few proteins exposed on its outer membrane sheath
d) Forming spores
Which of the following is NOT a typical CSF finding in neurosyphilis?
a) Elevated total protein
b) Positive CSF VDRL
c) High glucose levels
d) Moderate mononuclear pleocytosis
Which of the following conditions can give a biologic false-positive reaction in non-treponemal tests for syphilis?
a) Pregnancy
b) Diabetes
c) Hypertension
d) Asthma
FAQ
What is Treponema Pallidum?
Treponema Pallidum is a bacterium responsible for causing syphilis, a sexually transmitted infection.
How is syphilis transmitted?
Syphilis is primarily transmitted through direct contact with syphilitic sores, which can appear on the external genitals, vagina, anus, or in the rectum, lips, and mouth. It can also be transmitted from an infected mother to her baby during childbirth.
What are the stages of syphilis?
Syphilis progresses in stages: primary, secondary, latent, and tertiary. Each stage has distinct symptoms and potential complications.
How is syphilis diagnosed?
Syphilis is diagnosed through blood tests, examination of a sample from a sore, or cerebrospinal fluid tests. Darkfield microscopy is the gold standard for diagnosing genital chancres of primary syphilis.
Can syphilis be cured?
Yes, syphilis can be cured with appropriate antibiotics, typically penicillin. However, treatment will not reverse any damage that the infection has already caused.
What happens if syphilis is left untreated?
If left untreated, syphilis can progress to more severe stages, leading to complications like brain, nerve, eye, heart, blood vessel, liver, bone, and joint damage.
How can syphilis be prevented?
The most effective way to prevent syphilis is through abstinence or maintaining a monogamous relationship with a tested and uninfected partner. Using latex condoms correctly every time can reduce the risk, but it does not eliminate it entirely.
Is there a vaccine for syphilis?
As of now, there is no vaccine available to prevent syphilis.
Can syphilis reoccur after treatment?
Yes, even after successful treatment, an individual can get re-infected with syphilis if exposed to the bacterium again.
How does Treponema Pallidum evade the immune system?
T. pallidum has evolved strategies to evade the host’s immune response, one of which is having very few proteins exposed on its outer membrane sheath, minimizing the risk of antibody-mediated attacks.
References
- Radolf JD, Deka RK, Anand A, Šmajs D, Norgard MV, Yang XF. Treponema pallidum, the syphilis spirochete: making a living as a stealth pathogen. Nat Rev Microbiol. 2016 Dec;14(12):744-759. doi: 10.1038/nrmicro.2016.141. Epub 2016 Oct 10. PMID: 27721440; PMCID: PMC5106329.
- Radolf JD. Treponema. In: Baron S, editor. Medical Microbiology. 4th edition. Galveston (TX): University of Texas Medical Branch at Galveston; 1996. Chapter 36. Available from: https://www.ncbi.nlm.nih.gov/books/NBK7716/
- Varma, R., Estcourt, C., & Mindel, A. (2013). Syphilis. Sexually Transmitted Diseases, 427–462. doi:10.1016/b978-0-12-391059-2.00017-6
- Ghanem, K. G. (2017). Syphilis. Infectious Diseases, 559–566.e1. doi:10.1016/b978-0-7020-6285-8.00061-7
- https://www.creative-diagnostics.com/tag-treponema-pallidum-antigens-74.htm
- https://www.osmosis.org/learn/Treponema_pallidum_%28Syphilis%29
- https://mechpath.com/2017/12/20/treponema-pallidum/
- https://biologydictionary.net/treponema-pallidum/