What is Pseudomonas putida?
- Pseudomonas putida is a Gram-negative, rod-shaped bacterium that is commonly found in soil environments. It is non-pathogenic and exhibits remarkable metabolic versatility, which makes it an important subject of study in various scientific fields. It belongs to the genus Pseudomonas, a group known for its ability to metabolize a wide range of organic and inorganic compounds. P. putida’s genetic adaptability also makes it a useful organism in research, particularly in bioremediation and industrial applications.
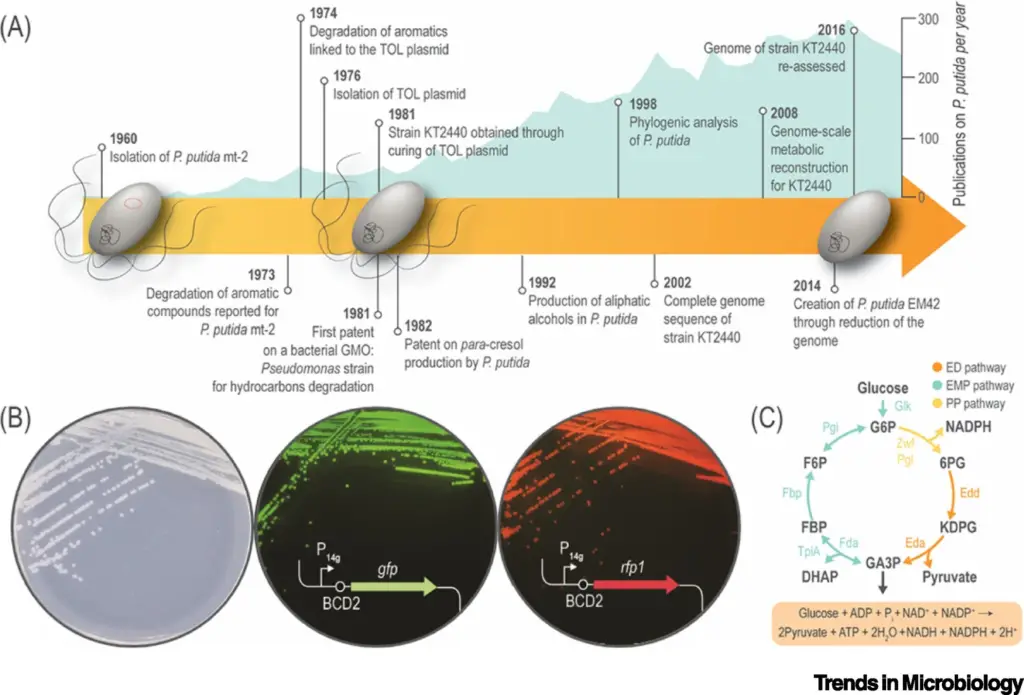
- One of the most significant traits of P. putida is its ability to degrade complex organic solvents, including hydrocarbons like toluene. This metabolic characteristic has been harnessed in bioremediation, where P. putida is employed to degrade pollutants in contaminated environments. Its ability to break down toxic substances is also why it was the first microorganism to be patented, though the patenting of a living organism raised significant legal questions. The landmark case, Diamond v. Chakrabarty, confirmed the organism’s patentability, marking a pivotal moment in biotechnology history.
- P. putida’s ability to adapt to diverse environments is attributed to its unique genetic makeup. Its genome is not monophyletic; it forms part of a larger group of Pseudomonas species known as the putida group. This group includes species such as P. alkylphenolia and P. alloputida, all sharing similar metabolic capabilities. While P. putida itself is non-pathogenic, its close relatives, like P. aeruginosa, can be harmful, particularly to immunocompromised individuals. The classification of P. putida has been refined through advanced genomic analyses, which have helped clarify its evolutionary position among other Pseudomonas species.
- Beyond its role in environmental cleanup, P. putida also has industrial applications, including in the production of bio-based chemicals. Its metabolism enables the synthesis of various compounds, making it a valuable organism in biotechnology. The bacterium is also used as a biocontrol agent to combat pathogenic microorganisms, further highlighting its versatility.
- P. putida’s interactions with its environment are also of interest in ecological studies. It is commonly found in rhizospheric soils and freshwater habitats, where it can interact with plant roots and contribute to nutrient cycling. Although P. putida is rarely associated with infections, it has been isolated from clinical samples, particularly in immunocompromised patients, though such cases are uncommon.
- Distinct from other species in the Pseudomonas genus, P. putida does not produce gelatinase, a key enzyme that differentiates it from P. aeruginosa. It also does not produce phenazine pigments, a characteristic that distinguishes it from P. fluorescens. These differences, along with its inability to grow at higher temperatures and its lack of denitrifying capabilities, help microbiologists distinguish P. putida from closely related species.
- The name Pseudomonas putida derives from the Latin word “putida,” meaning “stinking,” reflecting the bacterium’s presence in decomposing organic matter and its characteristic odor in laboratory cultures. Discovered by Trevisan in 1889, P. putida has since become a model organism for studying bacterial metabolism and environmental remediation.
Scientific classification of Pseudomonas putida
| Domain: | Bacteria |
| Phylum: | Pseudomonadota |
| Class: | Gammaproteobacteria |
| Order: | Pseudomonadales |
| Family: | Pseudomonadaceae |
| Genus: | Pseudomonas |
| Species: | P. putida |
Habitat of Pseudomonas putida
Pseudomonas putida is a versatile bacterium found in a wide range of environments, thriving in both natural and man-made habitats. Its adaptability to various ecological niches is a result of its diverse metabolic capabilities and ability to survive under different abiotic conditions.
- Common Habitats:
- Soil (Rhizosphere): P. putida is commonly found in the soil, particularly in the rhizosphere, where it interacts with plant roots. This environment provides a rich source of organic compounds for the bacterium to break down.
- Fresh and Saltwater: It is present in both freshwater and saltwater, adapting to changes in salinity and other environmental conditions.
- Sewage and Wastewater: P. putida thrives in sewage and wastewater, making it a frequent inhabitant of household drains. Its ability to survive in these polluted environments highlights its metabolic flexibility.
- Plant and Animal Surfaces: It is also found on the surfaces of plants and animals, as well as in human habitats, though it is generally non-pathogenic in these settings.
- Temperature Sensitivity:
- P. putida is not well-suited to high-temperature environments. Unlike species such as P. fluorescens and P. aeruginosa, which can tolerate higher temperatures, P. putida struggles to survive at temperatures above 42°C.
- Adaptability to Environmental Stress:
- P. putida’s broad environmental tolerance is linked to its ability to metabolize a wide range of compounds. This allows the bacterium to thrive in diverse habitats, from the nutrient-rich rhizosphere to polluted water systems.
- It can withstand various abiotic challenges, such as fluctuating pH levels and varying nutrient availability, which enhances its competitive edge in diverse ecosystems.
- Global Distribution:
- Most strains of P. putida have a broad geographical range, with some being isolated from extreme environments, such as soil samples around lakes in Antarctica.
- Some strains exhibit more restricted distributions, which are typically due to less versatile metabolic pathways, limiting their ability to survive in diverse conditions.
- Aerobic Requirements:
- As an obligate aerobe, P. putida requires oxygen-rich environments for growth and development. This means it is typically found in habitats with abundant oxygen, such as the surface of water bodies and the roots of plants.
- Opportunistic Pathogenesis:
- Though P. putida is generally non-pathogenic in healthy individuals, it can act as an opportunistic pathogen in immune-compromised individuals, such as newborns and cancer patients.
- Role in Plant Environments:
- Certain strains of P. putida are part of the natural microbial flora of plants, inhabiting their roots and leaves. This suggests that P. putida may play a role in plant health or protection, though it is not considered pathogenic under normal conditions.
Morphology of Pseudomonas putida
Pseudomonas putida exhibits a distinctive morphology that contributes to its functional versatility. Its structure allows it to adapt to various environments and perform a range of biochemical processes.
- Shape and Size:
- P. putida cells are Gram-negative and rod-shaped, typically ranging from 0.5 to 1.0 µm in length.
- The length of the cells can vary depending on the age and growth conditions. Younger cells tend to be longer compared to older ones.
- Under certain conditions, some cells may become filamentous, appearing longer and broader due to changes in the width-to-length ratio.
- Cell Arrangement:
- Most P. putida cells exist as single units, but there are occasional pairings observed. These pairs form in an end-to-front fashion.
- Flagella and Motility:
- As a motile bacterium, P. putida has flagella on its surface. The number of flagella can vary, with cells sometimes having just one or multiple flagella.
- These flagella enable the bacterium to move toward favorable conditions or away from harmful ones.
- Fimbriae (Pili):
- P. putida cells are equipped with fimbriae (also known as pili), which are hair-like structures on the surface.
- These structures assist in attachment to surfaces and contribute to the bacterium’s motility, facilitating its ability to move across various environments.
- Cell Envelope:
- The cell envelope of P. putida consists of three distinct layers:
- Outer membrane: This serves as the outer boundary of the cell, offering protection.
- Peptidoglycan layer: Situated beneath the outer membrane, this layer provides structural integrity and helps protect the cell against external threats, including antibacterial agents.
- Cell membrane: The innermost layer consists of a lipid bilayer, which can adjust its fluidity depending on the surrounding environmental conditions, allowing the bacterium to remain adaptable.
- The cell envelope of P. putida consists of three distinct layers:
- Genome and Protein Content:
- P. putida’s genome is composed of a substantial number of proteins, ranging from 3,748 to 6,780 proteins.
- The GC content of its genome is approximately 60%, a feature that plays a role in the bacterium’s genetic stability and adaptability.
- Fluorescent Pigment:
- P. putida belongs to the fluorescent group of Pseudomonas species, meaning it produces the fluorescent pigment pyoverdine.
- Unlike some other members of the genus, P. putida does not produce phenazine pigments, which distinguishes it from certain related species.
Virulence Factors of Pseudomonas putida
Pseudomonas putida, though typically non-pathogenic, can exhibit virulence under certain conditions, particularly in immunocompromised individuals. While it is not as virulent as other Pseudomonas species like P. aeruginosa, it still possesses several factors that enable it to cause infections.
- Temperature Tolerance:
- One of the key virulence factors is its ability to survive at 37°C, the human body temperature, which allows it to thrive in clinical environments.
- It can also endure low temperatures (as low as 4°C), enabling survival in stored clinical samples like blood.
- Antibiotic Resistance:
- Similar to other Pseudomonas species, P. putida is known for its antibiotic resistance. This resistance plays a crucial role in its ability to evade treatment, contributing to its virulence.
Key Virulence Factors
- Flagella and Pili:
- P. putida is motile, equipped with flagella that aid in its movement. These flagella move in a helical manner, allowing the bacteria to swim through the tissues.
- Pili, another surface structure, help in the adhesion of bacteria to host cells.
- Together, flagella and pili play a significant role in colonization of host tissue, movement through the body, and the formation of biofilms.
- Quorum Sensing and Biofilm Formation:
- Quorum sensing is a communication mechanism that allows P. putida to coordinate the behavior of bacterial cells, which aids in the progression of disease.
- This system triggers the production of alginates, which contribute to the formation of biofilms. Biofilms protect bacteria from the host immune system and antibiotic treatment.
- Biofilm formation is particularly significant in environments where medical devices (such as catheters and respirators) are present, providing a safe harbor for bacteria to persist and multiply.
- Secondary Metabolites:
- P. putida produces secondary metabolites like hydrogen cyanide and rhizoxin, which have antibacterial properties. These metabolites help the bacterium compete with other microorganisms in its environment.
- Hydrogen cyanide disrupts the water and mineral intake of competing microbes, particularly plant pathogens. It is regulated by specific genes (hcnABC), with production increasing in low oxygen conditions.
- Lipopolysaccharides (LPS):
- The outer membrane of P. putida contains lipopolysaccharides (LPS), which protect it from the immune system by preventing phagocytosis and lysis.
- The lipid A component of LPS induces cytotoxic activity, further helping P. putida evade immune responses. It also causes the immune system to release inflammatory cytokines such as IL-8 and TNF-α, leading to an excessive inflammatory response. This inflammation is often a primary cause of organ damage.
- Proteases:
- P. putida produces proteases like elastases and phospholipases. These enzymes degrade tissue components, facilitating the spread of bacteria within the body.
- Phospholipases break down phospholipids, which are key components of cell membranes. One byproduct, diacylglycerol, has toxic effects on host cells. It induces the production of inflammatory mediators like protein kinase and arachidonic acid, which drive further tissue damage.
Pathogenesis of Pseudomonas putida
Pseudomonas putida is typically a non-pathogenic bacterium, thriving in environmental settings. However, in individuals with weakened immune systems, it can cause infections, primarily in the lungs and bloodstream. The process of infection is not fully understood, but it is known to involve several key virulence factors that help the bacteria invade, colonize, and damage host tissues.
Key Steps in the Pathogenesis of P. putida
- Entry and Colonization:
- P. putida can enter the body through contaminated blood (e.g., during transfusions) or sterile body sites like wounds or burns.
- Flagella allow the bacteria to move through tissues, while pili enable attachment to target cells. These structures are critical for initial colonization.
- The bacterium avoids phagocytosis by utilizing its lipopolysaccharide (LPS) layer, which provides protection against immune cells like macrophages.
- Once attached, P. putida starts to extract essential nutrients and minerals from the host to survive and reproduce.
- Tissue Damage:
- As P. putida establishes itself, it produces various proteins, enzymes, and toxins to degrade host tissues and spread throughout the body.
- Elastase, a protease, breaks down elastin, facilitating the bacteria’s movement and spreading to adjacent tissues.
- Phospholipase degrades phospholipids in host cell membranes, causing the release of toxic cell components and leading to necrosis.
- The byproducts of this degradation trigger an inflammatory response, which leads to further tissue damage and contributes to the spread of infection.
- Biofilm Formation:
- Biofilm formation is a key defensive mechanism for P. putida. This structure protects the bacteria from both the host immune system and antimicrobial agents.
- The production of alginates and the extracellular matrix by the bacteria helps to form the biofilm, providing a nutrient-rich environment and preventing dehydration.
- Pili, along with metabolic products, also play a vital role in biofilm formation. The biofilm offers a shielding layer that makes it harder for the immune system to eliminate the bacteria.
Clinical Manifestation of Pseudomonas putida
Infections caused by Pseudomonas putida often affect specific sites in the body where the bacteria can colonize and thrive. While these infections can range from mild to severe, they are particularly concerning in individuals with compromised immune systems or underlying conditions.
Common Infections and Symptoms
- Bacteremia:
- Bacteremia is the most serious and common manifestation of P. putida infection.
- The bacteria enter the bloodstream, often following soft tissue infections or through transfusion of contaminated blood.
- Symptoms include periodic fever and chills, as bacteria reproduce and release into the bloodstream.
- In severe cases, bacteremia can progress to fulminant sepsis-induced multiorgan failure, which can be fatal.
- The risk is higher in immunocompromised patients, particularly those with underlying conditions like HIV, renal insufficiency, or advanced age.
- Soft Tissue Infections:
- Skin and soft tissue infections are relatively uncommon but still observed, especially in individuals with weakened immune systems.
- These infections typically target cartilage and connective tissues and can lead to ulcerative lesions.
- The bacteria usually enter the body through trauma or breaks in the skin.
- Without appropriate antimicrobial treatment, the infection can spread, leading to bacteremia and potentially fatal complications.
- Patients with conditions like HIV or renal insufficiency are particularly at risk.
- Respiratory Infections:
- P. putida can also cause hospital-acquired respiratory infections, often originating from contaminated medical equipment like bronchoscopes.
- These infections can be transmitted from one patient to another, particularly in healthcare settings.
- Diagnosing respiratory infections involves isolating the bacteria from tracheal aspirates or sputum samples.
- It is essential to distinguish P. putida from other respiratory pathogens to ensure proper treatment.
Lab Diagnosis of Pseudomonas putida
Diagnosing Pseudomonas putida infections requires isolating and identifying the bacteria from clinical samples. The methods used depend on the type of sample and the severity of the infection. While some traditional approaches focus on bacterial morphology and biochemical tests, newer methods like immunological and molecular techniques are providing more precise results.
Methods of Laboratory Diagnosis
- Preliminary Identification:
- Isolation of P. putida begins by growing bacteria on artificial growth media.
- Colony morphology helps give an initial indication of the bacteria’s identity.
- Microscopic observation reveals bacterial shape and size.
- Biochemical tests are essential for confirming P. putida. Two key tests are:
- Gelatin hydrolysis test: Differentiates P. putida from other Pseudomonas species.
- Growth at 41°C: P. putida can grow at this higher temperature, which is not typical for all Pseudomonas strains.
- Immunological Methods:
- Immunoassays identify proteins or enzymes specific to P. putida. These tests use techniques such as ELISA (Enzyme-Linked Immunosorbent Assay) and Western Blotting.
- Rapid diagnostic tests can detect specific antigens or other structures unique to P. putida.
- These methods provide quicker results compared to traditional culturing techniques.
- Molecular Methods:
- Modern diagnostic labs increasingly rely on molecular methods like PCR (Polymerase Chain Reaction) and DNA sequencing for identifying P. putida.
- These methods target unique DNA segments or rRNA fragments that are specific to the bacteria.
- While these techniques are more reliable, they tend to be more time-consuming and require specialized equipment.
Prevention of Pseudomonas putida
Preventing Pseudomonas putida infections is mostly about minimizing the bacteria’s transmission, especially in hospital settings where the risk is high. Strict adherence to guidelines and protocols can reduce the spread of the bacteria, particularly in environments with vulnerable individuals.
Key Prevention Strategies
- Hospital Infection Control:
- Transmission often occurs in hospital environments, making infection control essential.
- Health workers should adhere to strict hygiene practices, including wearing gloves and coats when interacting with patients.
- Blood testing is vital before blood transfusions to ensure the blood is free from contamination.
- Regular cleaning and disinfection of hospital equipment, particularly bronchoscopes, can prevent cross-contamination between patients.
- Avoid Contaminated Items:
- Items like contaminated food and flowers can be vehicles for bacteria transmission. Hospitals should monitor such items carefully.
- Prompt Treatment of Skin Infections:
- Since the infection often starts with topical skin infections, any cuts, wounds, or lesions should be treated immediately to prevent the bacteria from spreading deeper into the body.
- Regular monitoring of patients for signs of infection, especially those with compromised immunity, can help catch early symptoms before they worsen.
Industrial Uses of Pseudomonas putida
Pseudomonas putida has found its way into various industrial applications due to its versatile metabolic capabilities. This bacteria plays a significant role in areas such as bioremediation, agriculture, and the production of biodegradable plastics, thanks to its ability to break down complex substances and survive in harsh environments.
- Bioremediation:
- P. putida is commonly used in bioremediation processes. It breaks down non-degradable compounds, helping to clean up polluted environments.
- Its versatile metabolism allows it to thrive in unfavorable conditions, making it an ideal choice for degrading environmental pollutants.
- The bacteria has been used to reduce naphthalene contamination in soil, demonstrating its effectiveness in environmental cleanup.
- Biodegradable Plastic Production:
- P. putida can convert styrene oil into biodegradable plastic known as PHA (polyhydroxyalkanoates).
- This process supports sustainable plastic alternatives that are decomposed by other microorganisms, reducing plastic waste.
- Agriculture and Biocontrol:
- Many strains of P. putida produce antibiotic secondary metabolites, which can be used in biocontrol to protect plants from harmful pathogens.
- The bacteria has been isolated from rhizospheric regions of plants, indicating its potential use as a plant growth-promoting rhizobacteria.
- As a soil inoculant, P. putida contributes to enhancing plant growth by creating a beneficial environment for plants and suppressing disease-causing microorganisms.
- Topley and Wison’s Microbiology and Microbial Interactions; Bacteriology, 2 Vol. Tenth Edition. John Wiley and Sons Ltd.
- Textbook of Microbiology and Immunology – Textbook by Parija SC
- Volke, D. C., Calero, P., & Nikel, P. I. (2020). Pseudomonas putida. Trends in Microbiology. doi:10.1016/j.tim.2020.02.015
- Peter, S., Oberhettinger, P., Schuele, L. et al. Genomic characterisation of clinical and environmental Pseudomonas putida group strains and determination of their role in the transfer of antimicrobial resistance genes to Pseudomonas aeruginosa . BMC Genomics 18, 859 (2017). https://doi.org/10.1186/s12864-017-4216-2
- Weimer, A., Kohlstedt, M., Volke, D.C. et al. Industrial biotechnology of Pseudomonas putida: advances and prospects. Appl Microbiol Biotechnol 104, 7745–7766 (2020). https://doi.org/10.1007/s00253-020-10811-9
- Purtschert-Montenegro, G., Cárcamo-Oyarce, G., Pinto-Carbó, M. et al. Pseudomonas putida mediates bacterial killing, biofilm invasion and biocontrol with a type IVB secretion system. Nat Microbiol 7, 1547–1557 (2022). https://doi.org/10.1038/s41564-022-01209-6
- Baykal H, Çelik D, Ülger AF, Vezir S, Güngör MÖ. Clinical features, risk factors, and antimicrobial resistance of pseudomonas putida isolates. Medicine (Baltimore). 2022 Dec 2;101(48):e32145. doi: 10.1097/MD.0000000000032145. PMID: 36482647; PMCID: PMC9726331.
- Loeschcke A, Thies S. Pseudomonas putida-a versatile host for the production of natural products. Appl Microbiol Biotechnol. 2015 Aug;99(15):6197-214. doi: 10.1007/s00253-015-6745-4. Epub 2015 Jun 23. PMID: 26099332; PMCID: PMC4495716.
- Pseudomonas putida Volke, Daniel C. et al. Trends in Microbiology, Volume 28, Issue 6, 512 – 513
- https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-017-4216-2
- https://en.wikipedia.org/wiki/Pseudomonas_putida
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.