What is Pseudomonas aeruginosa?
- Pseudomonas aeruginosa is a Gram-negative, rod-shaped bacterium with significant medical importance due to its resistance to antibiotics and its role as an opportunistic pathogen. It is widely distributed across the environment, found in soil, water, plants, animals, and as part of the normal human flora. Though it is typically harmless in healthy individuals, it can cause serious infections in those with weakened immune systems, such as patients with cystic fibrosis, burns, or other compromised conditions.
- P. aeruginosa is highly versatile, capable of thriving in both aerobic and low-oxygen environments. It can infect various tissues, particularly in critical organs like the lungs, urinary tract, and kidneys. The bacterium’s ability to form biofilms on surfaces, including medical devices like catheters, contributes to its resistance to treatments and its role in hospital-acquired infections. Common infections associated with P. aeruginosa include ventilator-associated pneumonia and sepsis.
- One of the most distinctive features of P. aeruginosa is its pigmentation, which results from the production of two secondary metabolites, pyocyanin (blue) and pyoverdine (green). These pigments give the bacterium a characteristic blue-green color, which is often observed in laboratory cultures. The name “Pseudomonas” comes from the Greek word “pseudēs,” meaning false, and “monas,” referring to a single unit. The species name “aeruginosa” refers to the verdigris or greenish-blue color, indicative of the bacterium’s pigmentation.
- A key challenge in managing P. aeruginosa infections is its intrinsic resistance to many antibiotics. This bacterium has developed several mechanisms to evade treatment, including the ability to block antibiotic penetration through its outer membrane. It can also produce enzymes that break down antibiotics. Consequently, infections with P. aeruginosa often require the use of more potent or specialized antibiotic therapies, which can carry the risk of adverse effects.
- The bacterium’s ability to break down hydrocarbons has also made it useful in environmental applications, such as oil spill cleanup. Despite its medical challenges, P. aeruginosa’s capacity to degrade pollutants has led to its use in bioremediation efforts.
Scientific classification of Pseudomonas aeruginosa
| Domain: | Bacteria |
| Phylum: | Pseudomonadota |
| Class: | Gammaproteobacteria |
| Order: | Pseudomonadales |
| Family: | Pseudomonadaceae |
| Genus: | Pseudomonas |
| Species: | P. aeruginosa |
Morphology of Pseudomonas aeruginosa
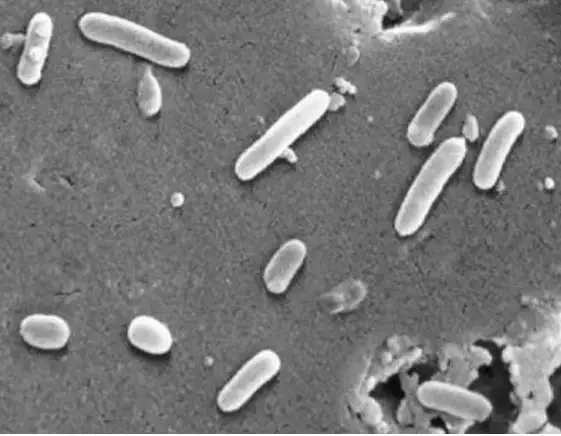
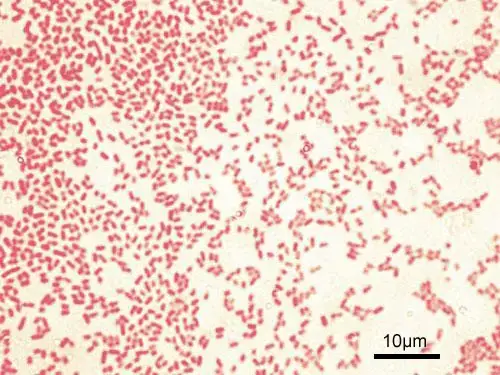
Pseudomonas aeruginosa is a Gram-negative bacterium with several distinctive morphological features that contribute to its pathogenicity and ability to thrive in various environments. Below is a breakdown of the key characteristics:
- Shape and Size:
P. aeruginosa is a rod-shaped bacterium (bacillus), typically measuring 0.5 to 0.8 µm in width and 1.5 to 3.0 µm in length. Some strains can grow up to 1.5–5.0 µm long. The cells usually appear as single units, in pairs, or occasionally in short chains. - Motility:
The bacterium is motile due to the presence of a single polar flagellum inserted at the tip of the cell. Some strains may have two or three flagella at the pole. This flagellum plays a role in movement and also contributes to heat-labile antigens, which are important for virulence. - Fimbriae and Pili:
P. aeruginosa also produces polar fimbriae or pili. These appendages are around 6 nm wide and are retractable. Fimbriae are essential for the bacterium’s ability to adhere to surfaces and can serve as receptors for bacteriophages. They also contribute to the bacterium’s pathogenicity by enabling adhesion to host cells. - Capsule and Slime Layer:
While P. aeruginosa is non-capsulated, many strains produce an abundant extracellular polysaccharide, which is primarily composed of alginate polymers. This forms a loose capsule or glycocalyx, giving certain strains a mucoid appearance. This feature is especially common in strains isolated from patients with cystic fibrosis, where the mucoid strain helps in colonization of the lungs and evasion of immune responses. - Pigmentation:
P. aeruginosa is known for producing water-soluble pigments, which diffuse through the media. These pigments give the bacterium a characteristic blue-green color, primarily due to pyocyanin (blue) and pyoverdine (green). The phenazine blue pigment is the most commonly observed and contributes to the distinctive appearance of infected tissues. - Cell Envelope:
The structure of the cell envelope is similar to other Gram-negative bacteria, consisting of three distinct layers:- Outer membrane: Contains a lipopolysaccharide layer that provides the bacterium with rigidity and contributes to its resistance against some antibiotics.
- Peptidoglycan layer: Situated between the inner and outer membranes, providing structural support.
- Inner cytoplasmic membrane: A lipid bilayer that adjusts its fluidity in response to environmental changes, helping the bacterium adapt to different conditions.
- Sporulation and Fimbriation:
Pseudomonas aeruginosa is non-sporing, meaning it does not form spores for survival in harsh conditions. It does, however, produce fimbriae, which help in adhesion and colonization, enhancing its ability to infect various host tissues.
Geographical Distribution and Habitat of Pseudomonas aeruginosa Infection
Pseudomonas aeruginosa is a widespread opportunistic pathogen that can be found in various environments, particularly in healthcare settings. Its ability to thrive in diverse locations and colonize different parts of the human body makes it a significant concern in hospital-related infections. Here’s how its distribution and habitat look:
- Global presence:
Pseudomonas aeruginosa is found nearly everywhere. It’s a part of the natural microbial environment, but it’s also a common culprit in infections, especially in hospital settings.
It is not limited to a specific region or climate. It can thrive in both tropical and temperate climates. - In the hospital:
Hospitals provide ideal conditions for the spread of P. aeruginosa due to their high humidity, crowded areas, and frequent use of medical devices.
The bacteria are commonly found in places like:- Toilets
- Bathtubs
- Wash basins
- Respiratory equipment
- Dialysis machines
- Kitchens
- Antiseptic or disinfectant solutions
- Habitat in the human body:
Outside of environmental surfaces, P. aeruginosa can also colonize parts of the human body, especially in hospital patients.
It is commonly found in:- Respiratory tract
- Gastrointestinal tract
- Colonization in vulnerable patients:
For patients with weakened immune systems or those on long-term medical treatments, P. aeruginosa has a higher chance of becoming an opportunistic pathogen. This colonization can lead to serious infections, especially in those already dealing with other underlying health conditions.
Culture and Biochemical Reactions of Pseudomonas aeruginosa
Pseudomonas aeruginosa is a strict aerobe that thrives in various environments. It is capable of growing on a wide range of media and can be identified through several distinct biochemical reactions. Below is a breakdown of its cultural and biochemical characteristics:

Culture Characteristics:
- Aerobic Growth:
P. aeruginosa requires oxygen to grow and is considered a strictly aerobic bacterium. - Temperature Range:
It grows effectively between 5°C and 32°C, with an optimal temperature of 37°C for best growth. - Growth on Common Media:
- Nutrient Agar:
After 24 hours of incubation at 37°C, P. aeruginosa forms large, 2-3 mm diameter colonies that are opaque, translucent, and irregularly round. These colonies emit a musty to fruity odor due to the production of aminoacetophenone from the amino acid tryptophan. The bacterium shows hemolytic activity on blood agar. - MacConkey Agar:
On MacConkey agar, P. aeruginosa produces colorless colonies as it does not ferment lactose. - Cetrimide Agar:
This selective medium supports the growth of P. aeruginosa and helps isolate it from other bacteria. - Nutrient Broth:
In nutrient broth, P. aeruginosa forms a dense turbidity and a surface pellicle due to its growth pattern.
- Nutrient Agar:
- Pigments Produced:
P. aeruginosa is known for producing a variety of pigments that contribute to its characteristic appearance:- Pyocyanin: A blue pigment produced only by P. aeruginosa, which diffuses into the surrounding medium. It is soluble in chloroform and water.
- Pyoverdin (Fluorescein): A yellow pigment common to Pseudomonas species, visible under ultraviolet light. It is water-soluble but insoluble in chloroform.
- Pyorubin: A red pigment, soluble in water but insoluble in alcohol.
- Pyomelanin: A brown pigment produced by some strains.
Biochemical Reactions:
- Oxidase Test:
P. aeruginosa is oxidase-positive, with a positive result appearing within 30 seconds. This test is crucial for identification. - Non-Fermentative Metabolism:
P. aeruginosa is a non-fermenter and uses oxygen as the terminal electron acceptor for sugar metabolism. In oxidation-fermentation (OF) media, P. aeruginosa shows a low acid production when glucose is oxidized. - Sugar Utilization:
- It does not ferment lactose or maltose.
- Glucose is utilized, but it forms only acid during its oxidative breakdown.
- Nitrate Reduction:
P. aeruginosa can reduce nitrates to nitrites, which are then further converted into gaseous nitrogen compounds. - Catalase and Arginine Dihydrolase:
- P. aeruginosa is catalase-positive, meaning it produces the enzyme catalase that breaks down hydrogen peroxide.
- It is also arginine dihydrolase-positive, showing activity with the enzyme that breaks down arginine.
- Other Negative Reactions:
P. aeruginosa is indole-negative, methyl red-negative, Voges-Proskauer-negative, and H2S-negative.
Cell Wall Components and Antigenic Structure of Pseudomonas aeruginosa
Pseudomonas aeruginosa has a complex cell wall structure and unique antigenic components that play key roles in its pathogenicity. The components of the cell wall include pili, slime layer, lipopolysaccharide (LPS), and pyocyanin, each contributing to the bacterium’s ability to cause infection and evade the host immune system.
Cell Wall Components:
- Pili:
P. aeruginosa contains pili similar to those found in Neisseria gonorrhoeae. These pili are essential for adhering to epithelial cells, facilitating colonization and infection. - Slime Layer (Alginate Coat or Glycocalyx):
Surrounding the bacterial cell wall is a loose slime layer, which provides protection against phagocytosis. It also shields the bacteria from the effects of many antibiotics, including aminoglycosides.
The slime layer’s production is regulated by genes that become active in specific conditions, such as in patients with cystic fibrosis or chronic respiratory diseases. This mucoid layer helps the bacteria to persist in the lungs of affected individuals. - Lipopolysaccharide (LPS):
The cell wall of P. aeruginosa, like other Gram-negative bacteria, contains LPS.
LPS acts as an endotoxin and contributes to the toxic effects seen in infections, particularly sepsis. It plays a critical role in the bacterium’s ability to cause severe infections. - Pyocyanin:
Pyocyanin is a pigment produced by P. aeruginosa. It catalyzes the production of superoxide and hydrogen peroxide, which contribute to tissue damage.
This pigment is not only important for the bacteria’s ability to damage host tissue but also plays a role in triggering inflammation in infected areas.
Antigenic Structure:
P. aeruginosa has two major antigenic components—O antigens and H antigens—that are crucial for identifying and classifying the bacterium.
- O Antigen:
The O antigens are somatic antigens that are group-specific. P. aeruginosa has 19 distinct O antigens, which have been used to classify the bacterium into 19 serogroups. These antigens are heat-stable and can be extracted using acid or formamide.- Detection: O antigens are typically detected through precipitation reactions or agglutination tests, where specific antisera are used to recognize the O antigens.
- Some O antigens, like serogroups O2 and O5, show cross-reactivity, which can complicate identification.
- Common Serogroups: O6 and O11 are frequently isolated from clinical specimens, with O11 being particularly associated with hospital-acquired infections caused by P. aeruginosa.
- H Antigen:
The H antigens are located in the flagella of P. aeruginosa. These are heat-labile antigens, meaning they are sensitive to heat and may lose their reactivity when exposed to high temperatures.
Two types of H antigens have been identified, which can be demonstrated using slide agglutination tests and specific antibodies against these antigens.
Virulence Factors of Pseudomonas aeruginosa
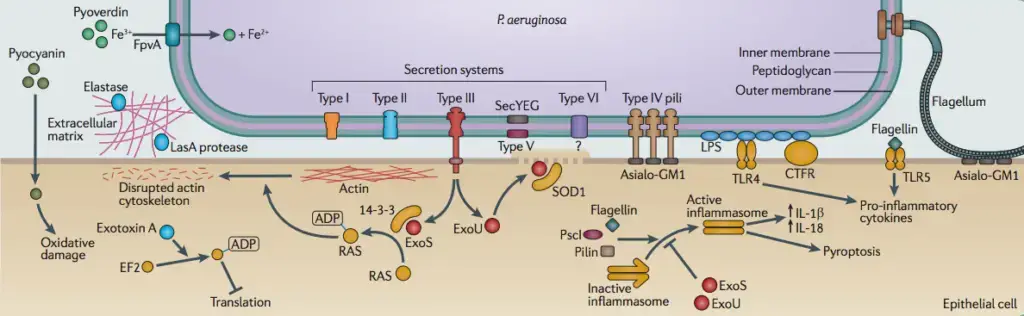
Pseudomonas aeruginosa is equipped with an array of virulence factors that help it establish infection, evade the host immune system, and cause tissue damage. These factors include toxins, enzymes, and various cell wall components. Here’s how each contributes to the pathogen’s ability to infect and cause disease.
Toxins:
- Exotoxin A:
Exotoxin A is a critical virulence factor for P. aeruginosa. It inhibits protein synthesis in eukaryotic cells, similar to the diphtheria toxin.
While less potent than the diphtheria toxin, Exotoxin A contributes to severe tissue damage in chronic pulmonary infections, dermatonecrosis in burn wounds, and destruction of the cornea in ocular infections. It also suppresses the immune response of the infected host, further complicating recovery. - Exotoxins S and T:
These two toxins also exhibit adenosine diphosphate ribosyl transferase activity.
They are believed to aid in the spread of P. aeruginosa by causing damage to epithelial cells. This facilitates the bacterium’s invasion of tissues, leading to necrosis and worsening the infection.
Enzymes:
- Elastase:
Elastase comes in two forms: serine protease (LasA) and zinc metalloprotease (LasB).
Together, they break down elastin, a major component of skin, lung tissue, and blood vessels, leading to significant tissue damage.
Elastase also helps P. aeruginosa spread by degrading complement proteins and inhibiting neutrophil chemotaxis, impairing the immune response in both acute and chronic infections. - Alkaline Protease:
This enzyme contributes to tissue destruction and the progression of P. aeruginosa infections.
It can interfere with the immune response by inactivating proteins like interferon, which play a role in immune defense. - Phospholipase C:
A heat-labile hemolysin, Phospholipase C breaks down lipids and lecithin, causing tissue destruction and facilitating the bacterium’s spread. - Rhamnolipid:
A heat-stable hemolysin, Rhamnolipid also contributes to the breakdown of lecithin-containing tissues, further aiding in tissue destruction and the spread of infection.
Cell Wall Components:
- Pili:
Pili are important for adhesion of P. aeruginosa to epithelial cells, allowing the bacteria to establish a foothold in host tissues. - Loose Slime Layer:
The slime layer, also known as the alginate coat or glycocalyx, serves as a protective barrier. It shields the bacteria from the immune system, inhibits antibiotic activity, and promotes persistence in chronic infections, especially in patients with cystic fibrosis. - Lipopolysaccharide (LPS):
LPS is a major component of the outer membrane of P. aeruginosa. It exhibits endotoxic activity, contributing to sepsis and further enhancing the bacterium’s ability to cause severe infections. - Pyocyanin:
Pyocyanin is a pigment that damages tissues by catalyzing the production of harmful molecules like superoxide and hydrogen peroxide. It also induces inflammation, playing a role in the bacterial pathogenicity. - Alginate-like:
The production of this substance is associated with the mucoid phenotype, which helps P. aeruginosa resist host defenses and persist in infected tissues.
Pathogenesis of Pseudomonas aeruginosa
The pathogenesis of Pseudomonas aeruginosa infections is driven by a variety of virulence factors that allow the bacteria to infect host tissue, evade immune defenses, and cause persistent infections. These factors contribute to tissue damage, bacterial invasion, and the spread of infection throughout the body. The infection process follows a distinct path, from initial colonization to the development of chronic and invasive disease.
- Bacterial Attachment and Colonization
- The infection starts when P. aeruginosa enters the host, typically through breaches in the skin or mucous membranes, such as during hospital-acquired infections.
- The bacteria rely on flagella for movement through the body, directing them toward target sites where infection can take hold.
- Once at the target site, the bacteria use Type IV pili to bind to host epithelial cells. These pili attach to glycosphingolipids on the cell surface, aiding in initial colonization.
- Proteolytic enzymes like elastase help to break down host tissue, specifically elastin, creating pathways for the bacteria to spread further.
- Invasion
- Following colonization, P. aeruginosa releases the Type III secretion system, a critical mechanism that injects proteins directly from the bacterial cytoplasm into the host cells.
- This system delivers a range of cytotoxins, including Exo S and Exo T, which are potent toxins with two main activities: Rho GTPase-activating and ADP ribosyltransferase activities.
- These toxins disrupt the actin cytoskeleton, preventing phagocytosis and interfering with cell signaling and adhesion.
- Exo U, another toxin, directly contributes to cytotoxicity, particularly against epithelial cells and macrophages, facilitating further tissue damage.
- Other toxins from P. aeruginosa promote the activation of adenylate cyclase, affecting cAMP levels and causing further reorganization of the host’s cytoskeleton.
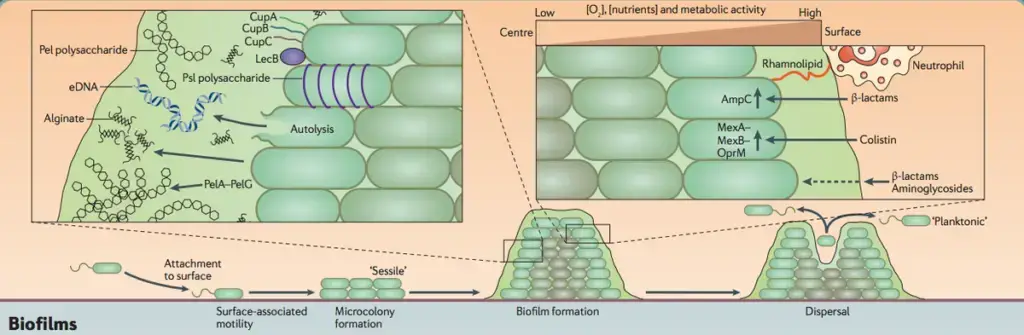
- Biofilm Formation
- The ability of P. aeruginosa to form biofilms is a crucial factor in the persistence and chronicity of infections.
- Exopolysaccharides, rhamnolipids, pyoverdine, and surface appendages contribute to the formation and structure of the biofilm.
- As the biofilm matures, it develops oxygen and water-filled channels that allow the deeper layers of the biofilm to receive nutrients, protecting the bacteria from hostile conditions.
- Cells within the biofilm are significantly more resistant to antimicrobial agents. Studies show that biofilm-associated cells can be up to 1000 times more resistant to antibiotics compared to free-swimming cells.
Clinical Syndromes of Pseudomonas aeruginosa Infection
Pseudomonas aeruginosa is a versatile pathogen that can cause a range of infections. It acts as both a true pathogen in patients with underlying diseases and an opportunistic pathogen in immunocompromised individuals. The infection can occur in various organs, manifesting in different clinical syndromes depending on the patient’s health status and the site of infection.
Respiratory Tract Infections:
- P. aeruginosa primarily infects the lower respiratory tract in patients with malignancies or immunodeficiencies.
- It is commonly associated with cystic fibrosis, other chronic diseases, and neutropenia, often following earlier colonization of the respiratory tract.
- Infection manifests as bilateral, diffuse bronchopneumonia, typically accompanied by pleural effusion.
- Mortality in these cases is high, with a 70% mortality rate.
- Factors that increase susceptibility:
- Use of respiratory instruments during therapy, which may introduce the bacteria to the lungs.
- Broad-spectrum antibiotics, which can disrupt normal microbial flora, making the respiratory tract more vulnerable to infection.
Skin Infections:
- P. aeruginosa is notorious for causing various skin infections, especially in burn wounds, chronic paronychia, infected toe webs, and pseudomonal folliculitis.
- Burn wound infections are the most common, presenting with dark brown eschar, edema, and hemorrhagic necrosis.
- Infections are more common in individuals exposed to moisture or contaminated water, such as in swimming pools or hot tubs.
- Pseudomonal toe web infection is frequently seen in children who are exposed to contaminated water, and paronychia (nail infections) often occurs in people whose hands are frequently in water.
Urinary Tract Infections:
- P. aeruginosa can cause urinary tract infections (UTIs) in individuals with indwelling urinary catheters or those undergoing urinary tract surgery.
- These infections are typically hospital-acquired and are considered iatrogenic, meaning they result from medical intervention.
Ear Infections:
- P. aeruginosa is a common cause of external otitis (outer ear canal infection), particularly in patients with a history of swimming.
- It can also cause malignant external otitis, a severe infection that occurs mainly in patients with diabetes, AIDS, or the elderly.
- This form of ear infection is aggressive and can lead to complications if not treated promptly.
Eye Infections:
- Pseudomonal endophthalmitis, an infection of the inner eye, is caused by P. aeruginosa, often following trauma, intraocular surgery, or corneal ulcers.
- Individuals who wear contact lenses are at an increased risk of developing P. aeruginosa infections of the eye.
Endocarditis:
- Pseudomonal infectious endocarditis involves infection of the heart valves, including the tricuspid, aortic, and mitral valves.
- This condition leads to valve destruction and heart failure and is more commonly seen in individuals who abuse intravenous drugs, particularly those using pentazocine and triphenylamine.
Nosocomial Infections:
- P. aeruginosa is a major cause of nosocomial (hospital-acquired) infections, especially in immunocompromised hosts.
- Vulnerable populations include patients with conditions like AIDS, cystic fibrosis, neutropenia, and those with immune deficiencies such as complement deficiency or hypogammaglobulinemia.
- Nosocomial infections also occur in patients who have undergone medical procedures that cause skin and mucosal membrane injuries, such as burns, and those with indwelling devices like catheters, dialysis lines, and endotracheal tubes.
- P. aeruginosa can lead to bacteremia and conditions resembling Gram-negative bacteremia in immunocompromised individuals.
- Pseudomonal meningitis is another severe infection seen in patients who have undergone neurosurgery or are immunocompromised.
Reservoir, Source, and Transmission of Pseudomonas aeruginosa Infection
Pseudomonas aeruginosa thrives in specific environments, and its ability to spread makes it a major concern in healthcare settings. It can be transmitted in several ways, leading to infections that are difficult to control. Here’s how it works:
- Primary Reservoir:
The hospital environment is the primary reservoir for P. aeruginosa.
This is where the bacteria can persist and spread easily. It can live on various surfaces, especially in places like toilets, wash basins, bathtubs, and medical equipment.
The hospital setting provides the right conditions for its survival and transmission. - Source of Infection:
P. aeruginosa can be found in:- Aerosols: The bacteria can be aerosolized, especially in settings where respiratory therapy is involved.
- Infectious materials: This includes contact with contaminated surfaces or medical equipment, which can harbor the bacteria.
- Medical devices: Equipment like catheters, ventilators, and dialysis machines can serve as vectors for spreading the infection.
- Transmission Pathways:
The most common ways the infection spreads are:- Aerosols: When contaminated air is inhaled or when particles are dispersed through activities like mechanical ventilation.
- Direct contact: This occurs when an individual touches surfaces or instruments contaminated with the bacteria, leading to infection.
- Healthcare procedures: Procedures involving invasive equipment, such as intubation or catheterization, provide easy access for the bacteria to enter the body.
- Hospital-associated Infections:
P. aeruginosa is responsible for 5–15% of hospital-acquired infections.
Its ability to spread in healthcare environments makes it a common cause of nosocomial infections.
Laboratory Diagnosis of Pseudomonas aeruginosa
Diagnosing Pseudomonas aeruginosa infections in the lab requires careful isolation and identification processes. The bacteria’s presence in clinical samples must be confirmed through multiple steps to ensure accuracy. Here’s how it’s done:
- Isolation from Clinical Specimens:
- Pseudomonas aeruginosa is commonly found in clinical specimens, including feces, which may contain mixed microbial flora.
- To identify it, the sample is cultured on selective media like cetrimide agar, which helps inhibit the growth of other microorganisms and promotes the growth of P. aeruginosa.
- Since P. aeruginosa can often be a contaminant, repeated isolation is necessary to confirm that the bacterium is the actual causative agent of the infection.
- Identification of Bacteria:
Once isolated, the bacteria’s characteristics help in identifying it:- Non-lactose fermenting: P. aeruginosa does not ferment lactose, which helps distinguish it from other common pathogens.
- Beta-hemolytic: It produces beta-hemolysis on blood agar, indicating its ability to break down red blood cells.
- Green pigmented colonies: The bacteria typically produce a distinctive green color, often due to the production of pyocyanin, a pigment that gives it a characteristic green hue.
- Oxidase positive: P. aeruginosa gives a positive reaction in the oxidase test, which is another key feature in its identification.
- Further Characterization:
To confirm the identity, additional techniques can be used:- Biochemical properties: A range of tests can help identify P. aeruginosa based on its metabolic activity.
- Pyocin production: The bacteria may produce specific bacteriocins known as pyocins, which can help differentiate it.
- Phage typing: This involves testing the bacterium’s susceptibility to specific bacteriophages.
- Serotyping and molecular typing: These methods identify the strain of P. aeruginosa based on antigenic differences and genetic markers.
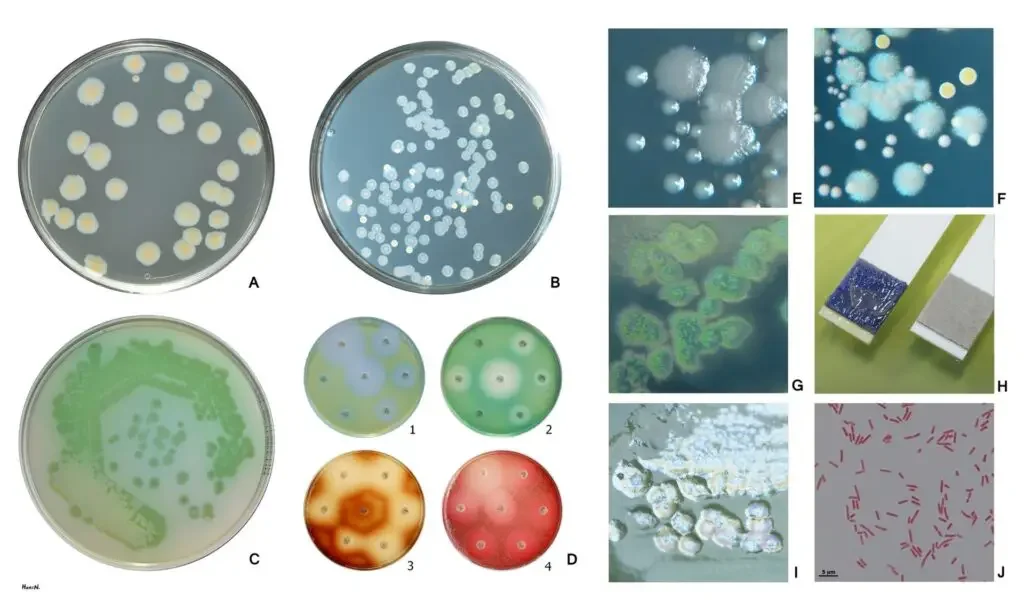
![Pseudomonas aeruginosa - Habitat, Diagnosis, Pathogenesis, Treatment 7 Examples of antibiotic susceptibility testing of P. aeruginosa. The disk diffusion test (A) and the MIC test (B). P. aeruginosa is intrinsically resistant to ampicillin/sulbactam, tigecycline and trimethoprim/sulfamethoxazole (no breakpoints in Img. B). [HansN., CC BY-SA 4.0, via Wikimedia Commons]](https://biologynotesonline.com/wp-content/uploads/2024/03/image-789.png)
Treatment of Pseudomonas aeruginosa Infection
Treating a Pseudomonas aeruginosa infection requires a targeted approach due to the bacterium’s resistance to many common antibiotics. Here’s how the treatment process typically works:
- Antimicrobial Therapy:
- Pseudomonas aeruginosa is known for its resistance to several commonly used antibiotics, so the treatment usually involves specific antipseudomonal drugs.
- The bacterium is generally susceptible to a few antibiotics, such as:
- Cefotaxime
- Ceftazidime
- Gentamicin
- Tobramycin
- Carbenicillin
- Azlocillin
- Ticarcillin
- Most Commonly Used Antibiotic:
- Ciprofloxacin is often the go-to choice because it’s effective in treating P. aeruginosa in various tissues.
- It’s frequently used due to its broad activity against the bacteria.
- Combination Therapy:
- Combination therapy is typically the best approach, particularly using two antipseudomonal antibiotics.
- Aminoglycosides or quinolones paired with another antipseudomonal drug provide greater efficacy in treating P. aeruginosa infections.
- This combination targets the bacteria from multiple angles, improving treatment outcomes.
- Exceptions to Combination Therapy:
- For certain infections, single antibiotic therapy might be enough:
- Urinary tract infections
- Local skin infections
- Febrile leukopenic patients
- In these cases, combination therapy is generally avoided unless other complications are present.
- For certain infections, single antibiotic therapy might be enough:
- Additional Treatments:
- Hyperimmune globulin and granulocytic transfusion may be helpful in some cases.
- These treatments can bolster the body’s immune response, aiding in the fight against the infection.
- Supportive Care:
- Treating any underlying conditions and providing supportive therapy is crucial for the success of the treatment.
- Managing the patient’s overall health can enhance the body’s ability to recover from the infection.
Prevention and Control of Pseudomonas aeruginosa Infections
Preventing Pseudomonas aeruginosa infections, especially in hospital settings, is a complex task that demands a focused approach. The bacteria are highly adaptable, and their resistance to many antibiotics makes control even more challenging. Here’s a breakdown of key measures to reduce the spread and impact of these infections:
- Infection Control Practices:
- Strict aseptic techniques are essential to preventing infection transmission.
- Constant monitoring of hospital environments helps identify potential sources of infection early.
- Limiting Cross-Infection:
- Careful attention is needed to prevent the cross-infection of patients.
- This involves ensuring that medical and paramedical personnel follow proper hygiene protocols and use personal protective equipment (PPE) when interacting with patients.
- Regular hand washing and disinfecting are critical to reduce transmission risk.
- Preventing Equipment Contamination:
- Medical equipment, especially dialysis machines and respiratory instruments, must be regularly cleaned and disinfected.
- Contaminated equipment is a common source of Pseudomonas transmission, so it’s crucial to follow manufacturer guidelines for sterilization.
- Antibiotic Management:
- Restricting the use of broad-spectrum antibiotics can help control Pseudomonas infections.
- Overuse of these antibiotics suppresses normal microbial flora, making it easier for resistant Pseudomonas strains to thrive.
- Ensuring that antibiotics are only prescribed when absolutely necessary is key to preventing resistance.
- Vaccination:
- Research has explored Pseudomonas vaccines, particularly for individuals at high risk of infection.
- Cystic fibrosis patients, for example, are highly susceptible to P. aeruginosa infections and may benefit from specialized vaccines designed to reduce infection rates.
FAQ
What is Pseudomonas aeruginosa, and where is it commonly found?
Pseudomonas aeruginosa is a bacterium commonly found in soil, water, and vegetation. It is also present on the skin of some healthy individuals and can be isolated from the throat and stool of nonhospitalized patients.
What are the common infections caused by Pseudomonas aeruginosa?
Pseudomonas aeruginosa can cause a wide range of infections, including respiratory tract infections, urinary tract infections, skin and soft tissue infections, bacteremia, endocarditis, and central nervous system infections.
How is Pseudomonas aeruginosa transmitted in healthcare settings?
In healthcare settings, P. aeruginosa can spread through contaminated medical equipment, sinks, taps, food, and even on the hands of healthcare personnel. Patients can also acquire the bacterium from fruits, vegetables, and other environmental sources.
Why is Pseudomonas aeruginosa often resistant to antibiotics?
Pseudomonas aeruginosa has developed resistance to many commonly used antibiotics due to its ability to adapt and produce various mechanisms of resistance. This resistance poses challenges in treating Pseudomonas infections effectively.
What are some risk factors for Pseudomonas aeruginosa infections?
Immunocompromised individuals, such as those with HIV/AIDS, cancer patients undergoing chemotherapy, diabetics, and those with severe burns, are at higher risk of developing Pseudomonas infections.
Can Pseudomonas aeruginosa infections be prevented?
Yes, certain measures can help prevent Pseudomonas infections in healthcare settings, such as proper isolation procedures, aseptic techniques, and regular cleaning and monitoring of medical equipment.
What are some common symptoms of Pseudomonas aeruginosa infections?
Symptoms vary depending on the site of infection, but common symptoms may include fever, respiratory difficulties, painful urination, skin redness, and inflammation.
How is Pseudomonas aeruginosa diagnosed?
Diagnosis is typically made by collecting samples from the infected site, such as sputum, urine, blood, or wound exudate, and subjecting them to laboratory analysis, including culture and sensitivity testing.
Are there any effective vaccines against Pseudomonas aeruginosa?
As of now, there are no widely available vaccines against Pseudomonas aeruginosa. Several types of vaccines are being studied, but none have been approved for general use.
What is the mortality rate associated with Pseudomonas aeruginosa infections?
Pseudomonas aeruginosa infections can be serious, especially in immunocompromised individuals. The combination of antibiotic resistance, weakened host defenses, and the production of extracellular enzymes and toxins can contribute to a high mortality rate in severe cases.
- Textbook of Microbiology and Immunology – Textbook by Parija SC
- Al-Dahmoshi, H., D. Al-Obaidi, R., & Al-Khafaji, N. (2021). Pseudomonas aeruginosa: Diseases, Biofilm and Antibiotic Resistance. IntechOpen. doi: 10.5772/intechopen.95251
- https://www.microscopemaster.com/pseudomonas-aeruginosa.html
- https://microbeonline.com/pseudomonas-aeruginosa-infection-mortality-pathogenesis-and-diagnosis
- https://www.cdc.gov/hai/organisms/pseudomonas.html
- https://microbewiki.kenyon.edu/index.php/Pseudomonas_aeruginosa_infection
- https://textbookofbacteriology.net/pseudomonas.html
- https://en.wikipedia.org/wiki/Pseudomonas_aeruginosa