What is Immunoglobulin A (IgA Antibody)?
- Immunoglobulin A (IgA) is one of the five primary immunoglobulins found in humans and is a critical component of the immune system. It is essential for maintaining mucosal homeostasis in many areas of the body, including the gastrointestinal, respiratory, and genitourinary tracts. IgA, as the main antibody in mucosal immunity, is in charge of defending these areas from antigens and infections.
- IgA is the second most prevalent immunoglobulin type in the body, producing more than all other immunoglobulin subtypes combined. It is formed by class switching of immunoglobulins, which is controlled by a variety of mechanisms. CD40-CD40L interaction and the production of particular cytokines drive Th2 cell development, resulting in class switching to diverse Ig subtypes. Furthermore, retinoic acid, a vitamin A metabolite, works synergistically with specific cytokines to promote IgA production.
- IgA is divided into two subclasses: IgA1 and IgA2. IgA can be synthesized in monomeric and dimeric forms, with the dimeric form known as secretory IgA (sIgA). sIgA is the most common type of IgA and can be found in tears, saliva, sweat, colostrum, and secretions from the genitourinary and gastrointestinal tracts, as well as the prostate and respiratory epithelium. It is also present in trace concentrations in the blood.
- One crucial feature of sIgA is its secretory component, which protects the immunoglobulin from enzyme degradation. This enables sIgA to survive in the harsh environment of the gastrointestinal tract and protect against microorganisms that grow in bodily secretions. Other immunoglobulins’ inflammatory effects can similarly be inhibited by sIgA. In comparison to other antibody classes, IgA is a poor complement activator and only faintly opsonizes microorganisms.
- In conclusion, Immunoglobulin A (IgA) is an important antibody in mucosal immunity, acting as the first line of defense against pathogens on mucosal surfaces. It is the main antibody found in mucous secretions and protects many regions of the body. Its synthesis and management are complicated, and its dimeric form, secretory IgA (sIgA), is important in avoiding infections in mucosal areas.
Definition of Immunoglobulin A (IgA Antibody)
Immunoglobulin A (IgA) is an antibody that plays a key role in the immune function of mucous membranes. It is the second most abundant immunoglobulin in the body and provides protection against antigens and pathogens in the gastrointestinal, respiratory, and genitourinary tracts.
Subclasses of Immunoglobulin A (IgA Antibody)
Immunoglobulin A (IgA) exists in two subclasses, IgA1 and IgA2, with distinct characteristics. Here is a summary of the subclasses based on the provided information:
- IgA1:
- Predominant IgA subclass found in the bloodstream, accounting for approximately 85% of the total IgA concentration in serum.
- Exhibits a strong immune response to protein antigens and displays a moderate response to polysaccharides and lipopolysaccharides.
- Predominantly produced by lymphoid tissues throughout the body, including mucosal-associated lymphoid tissues.
- IgA2:
- Represents up to 15% of total IgA in serum, with higher percentages found in secretions such as colostrum, maternal milk, tears, and saliva.
- Plays a crucial role in mucosal defense in the airways, eyes, and gastrointestinal tract.
- Particularly effective against polysaccharide and lipopolysaccharide antigens.
- Differs from IgA1 in the molecular mass of its heavy chains and its susceptibility to cleavage in the hinge region by bacterial proteases.
- Occurs in two allotypic forms, IgA2 (m1) and IgA2 (m2).
- The production of IgA2 is more prominent in secretory lymphoid tissues, such as the gut-associated lymphoid tissue (GALT).
Both IgA1 and IgA2 can be found in membrane-bound form and contribute to the body’s defense against various antigens, particularly at mucosal surfaces.
Structure of Immunoglobulin A (IgA Antibody)
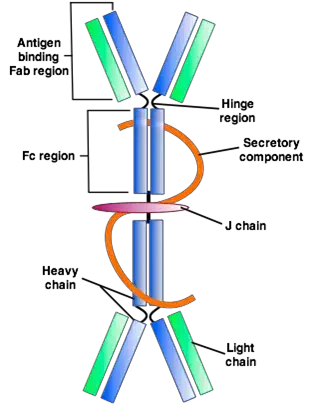
Immunoglobulin A (IgA) has a specific structure that contributes to its function and stability. Here is a summary of the structure of IgA based on the provided information:
- Overall Structure:
- IgA is a glycoprotein antibody composed of four polypeptide chains. It has two identical light chains (L) and two identical heavy chains (H).
- The H-chain type of IgA is alpha (α).
- Monomeric and Dimeric Forms:
- IgA exists in both monomeric and dimeric forms.
- In the blood, IgA is primarily found in its monomeric form.
- In body secretions, such as mucosal surfaces, IgA is present as dimeric or multimeric forms.
- Monomeric IgA in the blood can undergo polymerization to form dimeric, trimeric, and occasionally tetrameric forms.
- Additional Polypeptide Chains:
- In secretions, IgA contains two additional polypeptide chains, known as the secretory component (SC) and the J-chain (Joining chain).
- The secretory component and J-chain contribute to the stability and function of IgA.
- The secretory component helps in the transcytosis of IgA across epithelial cells, allowing it to be secreted into body fluids.
- The J-chain connects the two four-chain units of IgA through disulfide bridges, contributing to the formation of dimeric or multimeric IgA structures.
The structure of IgA, including its monomeric and dimeric forms, as well as the presence of additional polypeptide chains, plays a crucial role in its function as an antibody in mucosal immunity and protection against pathogens.
Mechanism
The mechanism of IgA antibody involves its secretion by plasma cells and its role in mucosal immunity. Here is an overview of the mechanism based on the provided information:
- Secretion of IgA:
- Plasma cells throughout the body secrete IgA into either internal fluids or external secretions.
- In internal fluids like plasma and cerebrospinal fluid, IgA remains in the monomeric form.
- In external secretions, such as mucosal surfaces, IgA is primarily released as a dimer held together by a joining (J) chain.
- Formation of Dimeric IgA:
- Plasma cells in the subepithelium of mucosal tissues secrete monomeric IgA.
- The monomeric IgA complexes with J chains through covalent bonding to form dimeric IgA.
- Transcytosis and Binding to Polymeric Ig Receptor (pIgR):
- Dimeric IgA, along with the J chain, binds to the polymeric Ig receptor (pIgR) located on the basolateral surface of intestinal epithelial cells.
- This binding allows the dimeric IgA to be transported into the cell through a process called transcytosis.
- Cleavage and Secretory Component Formation:
- Within the intestinal epithelial cells, the dimeric IgA complexed with pIgR is shuffled across the cell.
- At the apical surface of the cell, the pIgR still bound to IgA is cleaved.
- The cleavage results in the formation of the secretory component, which remains associated with the dimeric IgA.
- Release as Secretory IgA (SIgA):
- The dimeric IgA, along with the J chain and the secretory component derived from pIgR, is released into the mucosal lumen as secretory IgA (SIgA).
- SIgA functions as a protective antibody at mucosal surfaces.
- Functions of SIgA:
- SIgA plays a crucial role in preventing adhesion and penetration of antigens in the mucosal lumen.
- It neutralizes viruses and opsonizes antigens, enhancing their clearance.
In summary, IgA is secreted as a monomer or dimer depending on its location. The dimeric IgA binds to pIgR, undergoes transcytosis, and is cleaved to form the secretory component. The release of SIgA into the mucosal lumen allows it to interact with pathogens, prevent adhesion and penetration of antigens, neutralize viruses, and opsonize antigens for clearance.
Clinical Significance
IgA deficiency, IgA nephropathy, IgA vasculitis, IgA myeloma, and linear immunoglobulin A bullous dermatosis (LABD) are clinically significant conditions associated with immunoglobulin A (IgA). Here is a summary of their clinical significance based on the provided information:
- Selective IgA deficiency:
- It is the most prevalent immunodeficiency in humans, affecting 1 in 700 individuals, particularly those of the White race.
- Characterized by a decrease in IgA levels below 7 mg/dl while IgG and IgM levels remain normal.
- Individuals with severe IgA deficiency may experience repeated bouts of bacterial, enteroviral, or protozoal infections in the gastrointestinal and respiratory tracts due to the lack of mucosal immunity.
- Recurrent sino-pulmonary infections are common in IgA deficiency.
- IgA nephropathy (Berger disease):
- It is the most frequent cause of glomerulonephritis worldwide.
- IgA deposits in the kidney’s mesangium, leading to glomerular injury.
- Presents with hematuria (blood in urine) and red blood cell casts, often following an upper respiratory tract infection.
- IgA levels are increased in both serum and urine but have no prognostic significance.
- Progression to renal failure may occur in some cases.
- IgA Vasculitis (Henoch-Schonlein purpura):
- It is the most common childhood vasculitis, predominantly affecting small vessels.
- Deposition of IgA and complement protein C3 in vessel walls causes inflammation and leukocytoclastic vasculitis, resulting in purpura (skin rash).
- Symptoms include palpable purpura, joint pain, gastrointestinal pain, and renal involvement.
- Renal manifestations occur due to IgA deposition in the glomeruli.
- Typically has a good prognosis.
- IgA myeloma:
- It is the second most common subtype of multiple myeloma, characterized by a plasma cell malignancy that produces IgA.
- Presents with hypercalcemia, renal impairment, back pain (due to bone lesions), and anemia.
- Bone destruction, particularly in the skull and spine, is a hallmark feature.
- Diagnosis involves bone marrow biopsy and detection of IgA M-protein.
- Linear immunoglobulin A bullous dermatosis (LABD):
- A rare autoimmune disease affecting the subepidermis.
- Caused by IgA antibodies targeting collagen XVII and neutrophil accumulation.
- Linear deposition of IgA in the basal membrane zone leads to subepidermal cleavage.
- Presents as blisters on a reddish base in the perineum and perioral areas.
- Can cause chronic gingivitis, ulcers, and conjunctivitis.
In conclusion, clinical significance related to IgA includes selective IgA deficiency, IgA nephropathy, IgA vasculitis, IgA myeloma, and linear immunoglobulin A bullous dermatosis. These conditions have distinct manifestations and may affect different body systems, including the immune, renal, vascular, and dermatological systems. Proper diagnosis, management, and treatment are important for individuals with these conditions.
Functions of Immunoglobulin A (IgA Antibody)
Immunoglobulin A (IgA) antibody serves important functions in the immune system, particularly in protecting mucous membranes and providing local immunity. Here are the functions of IgA based on the provided information:
- Protection of Mucous Membranes:
- IgA is essential for the protection of mucous membranes in the gastrointestinal, respiratory, and genitourinary tracts.
- It has the ability to pass the epithelial layer and enter bodily secretions, providing local immunity in certain areas.
- Defense against Local Infections:
- Secretory IgA, which is rich in mucosal secretions such as saliva and tears, is the principal defense mechanism against several local infections.
- Its presence in these secretions aids in the prevention of pathogen adhesion and invasion.
- Barrier Function:
- IgA works as a barrier to prevent foreign substances from entering the circulatory system, such as infections and antigens.
- IgA protects against infection by neutralizing viruses and blocking their adhesion to host surfaces in bodily fluids.
- Resistance to Digestion and Complement Activation:
- IgA is resistant to digestion, allowing it to function in the harsh gastrointestinal and respiratory tract conditions.
- Although IgA is a weak complement pathway activator, it can activate the pathway when aggregated.
- Inhibition of Inflammatory Effects:
- Other immunoglobulins’ inflammatory effects can be inhibited by secretory IgA.
- It helps to maintain the immune system’s equilibrium and prevents excessive inflammation by moderating immunological responses.
In summary, IgA provides localized immune protection in mucosal tissues, prevents the entry of foreign substances, neutralizes viruses, and has anti-inflammatory properties. Its unique properties and functions make it a crucial component of the body’s immune defense at mucosal surfaces.
FAQ
What is Immunoglobulin A (IgA) antibody?
Immunoglobulin A (IgA) is an antibody that plays a crucial role in the immune system’s defense against pathogens. It is primarily found in mucosal secretions such as saliva, tears, respiratory and gastrointestinal fluids.
What is the structure of IgA antibody?
IgA is a four-polypeptide chain protein composed of two light chains (L) and two heavy chains (H). The H-chain type of IgA is alpha (α). IgA can exist in monomeric form or as a dimer, and it is held together by a joining (J) chain through disulfide bridges.
What are the functions of IgA antibody?
IgA antibody primarily protects mucous membranes and provides local immunity. It prevents the passage of foreign substances into the circulatory system, neutralizes viruses, inhibits inflammatory effects, and plays a role in preventing adhesion and penetration of antigens.
How is IgA antibody secreted?
IgA is secreted by plasma cells throughout the body into internal fluids or external secretions. In external secretions, it is released as a dimer held together by a J chain, while in internal fluids such as plasma, it remains in the monomeric form.
What is selective IgA deficiency?
Selective IgA deficiency is the most common immunodeficiency in humans, characterized by abnormally low levels of IgA in the blood. It can result in increased susceptibility to infections, particularly in the gastrointestinal and respiratory tracts.
What is IgA nephropathy?
IgA nephropathy, also known as Berger disease, is a kidney disorder where IgA deposits in the kidney’s glomeruli, leading to inflammation and potential kidney damage. It is the most common cause of glomerulonephritis worldwide.
What is IgA vasculitis?
IgA vasculitis, also called Henoch-Schonlein purpura, is a type of vasculitis that affects small vessels. It is characterized by the deposition of IgA and complement protein C3 in blood vessel walls, leading to inflammation and various symptoms such as skin rash, joint pain, and gastrointestinal involvement.
Can IgA deficiency lead to allergic or autoimmune diseases?
Yes, a decrease in secretory IgA can weaken the mucosal barrier, allowing more allergens to enter the bloodstream and potentially contribute to the development of allergic diseases. IgA deficiency is also associated with a higher incidence of autoimmune diseases such as rheumatoid arthritis, celiac disease, and thyroiditis.
How is IgA myeloma diagnosed?
IgA myeloma, a subtype of multiple myeloma, is diagnosed through various tests, including blood tests such as serum protein electrophoresis and immunofixation electrophoresis, which help detect abnormal levels of IgA and confirm the presence of M-proteins.
Are there any skin disorders associated with IgA antibodies?
Yes, linear immunoglobulin A bullous dermatosis (LABD) is a rare autoimmune disease where IgA antibodies target collagen XVII, leading to blistering and skin manifestations. It typically presents as blisters on a reddish base in areas like the perineum and perioral regions.