What is Entamoeba Histolytica?
- Entamoeba histolytica is a single-celled parasite that is primarily known for causing the disease amoebiasis in humans. The name of this organism derives from two parts: “Entamoeba,” which is the genus it belongs to, and “histolytica,” stemming from the Greek words for tissue (histo) and dissolution or destruction (lysis), indicating its tissue-destroying properties.
- This parasite exists in two main forms: the trophozoite and the cyst. The trophozoite stage represents the active, feeding phase of the parasite, typically found within the human host. During this stage, the parasite lives and multiplies in the intestines, absorbing nutrients and growing. On the other hand, the cyst form is the dormant, non-motile stage. Cysts are capable of surviving harsh environmental conditions outside the human body for extended periods, up to about three months, making them the primary means through which the parasite spreads.
- Infection with E. histolytica is a significant global health concern, particularly in tropical regions. While earlier estimates suggested that 10-12% of the world’s population might be infected, more recent research indicates that many of these cases are likely attributable to a different, less harmful species known as E. dispar. However, E. histolytica still infects a substantial number of people worldwide, with estimates ranging from 35 to 50 million, and it is responsible for over 55,000 deaths annually.
- The clinical manifestations of amoebiasis can vary. Many individuals infected with E. histolytica do not exhibit any symptoms. However, in cases where the organism becomes more virulent, it can cause amoebic dysentery, characterized by severe abdominal pain, diarrhea, and cramping. The infection may sometimes progress to extraintestinal amoebiasis, affecting organs beyond the intestines, most commonly the liver. In such cases, it can lead to the formation of liver abscesses, often containing a pus-like material described as having the consistency of anchovy paste. Less frequently, the infection can spread to other organs, including the spleen, lungs, and brain.
- E. histolytica is an anaerobic parasitic organism, meaning it thrives in environments without oxygen. While it predominantly affects humans, other primates can also be infected. However, other mammals like dogs and cats are less commonly affected and do not significantly contribute to the transmission of this parasite.
- Understanding the lifecycle, transmission, and impact of Entamoeba histolytica is crucial for the effective prevention and treatment of amoebiasis, particularly in regions where the parasite is prevalent.
Definition of Entamoeba Histolytica
Entamoeba histolytica is a single-celled, anaerobic parasitic organism that causes amoebiasis, a disease characterized by intestinal and sometimes extraintestinal infections. It exists in both active (trophozoite) and dormant (cyst) forms, the latter being responsible for environmental survival and transmission of the infection, particularly in tropical regions. The parasite primarily infects humans, leading to symptoms ranging from asymptomatic to severe dysentery and liver abscesses.
The Genus Entamoeba Histolytica
Entamoeba histolytica is a part of the Entamoeba genus, which encompasses various species. Within this genus, species are classified into two categories based on their impact on the host:
Commensal Species
These species typically reside in the host without causing harm:
- E. gingivalis
- E. coli
- E. hartmani
- E. dispar
Pathogenic Species
This category includes species that can cause disease:
- E. histolytica
Key Characteristics of E. histolytica
- Lifecycle Stages: E. histolytica exists in two distinct stages:
- Trophozoite Stage: The active, feeding phase within the host.
- Cyst Stage: The dormant, resilient form capable of surviving outside the host.
- Transmission Method:
- E. histolytica is primarily transmitted through its cyst form.
- Cysts are expelled from the body via the stool and can contaminate water and food sources.
- Infection and Disease:
- When cysts are ingested, they can lead to infection.
- The infection primarily targets the intestines but can spread to other organs.
- Symptomatology:
- While some infections are asymptomatic, others may lead to conditions like amoebic dysentery and liver abscesses.
- Prevalence:
- E. histolytica is more common in tropical regions where sanitary conditions may be compromised.
Comparison of the Human Enteric amoebae
The human digestive tract can host various species of amoebae, each with unique characteristics. This comparison focuses on several key species, including E. histolytica, E. coli, E. gingivalis, Endolimax nana, Iodoamoeba butschlii, and Dientamoeba fragilis.
Trophozoite Characteristics
- Size of Trophozoite:
- E. Histolytica: Approximately 25 µm (range 15-60 µm).
- E. Coli: Roughly 25 µm (range 15-40 µm).
- E. Gingivalis: About 15 µm (range 5-35 µm).
- Endolimax Nana: Typically 9 µm (range 5-14 µm).
- Iodoamoeba Butschlii: Around 10 µm (range 6-25 µm).
- Dientamoeba Fragilis: Generally 10 µm (range 6-25 µm).
- Motility of Trophozoite:
- E. Histolytica: Active, directional, and progressive.
- E. Coli: Sluggish, nondirectional, and nonprogressive.
- Others: Varying levels of activity and progression, with some resembling E. Coli.
- Nucleus Characteristics After Staining:
- Distinctive features are noted for each species, such as the size and appearance of the endosome and chromatin.
- Pseudopodes:
- Each species has a unique style of pseudopodes, ranging from finger-like and explosive in E. Histolytica to thin, leaf-like, and rapidly formed in Dientamoeba Fragilis.
Cyst Characteristics
- Size of Cyst:
- Sizes vary among species, with E. Histolytica cysts being around 12 µm and E. Coli cysts being larger at 17 µm.
- Inclusion of Glycogen:
- This characteristic varies significantly, with some species like E. Histolytica having diffuse glycogen and others like Endolimax Nana having none.
- Number of Nuclei in Cysts:
- The number of nuclei within cysts ranges from 1 to 8 depending on the species.
- Chromatoidal Bars:
- These features are present in some species, like E. Histolytica and E. Coli, often with distinct shapes.
Transmission of Entamoeba Histolytica
Entamoeba histolytica, a parasite known for causing amoebiasis, has a specific transmission cycle involving both active and dormant stages. Understanding this cycle is crucial for preventing and controlling the spread of the infection:
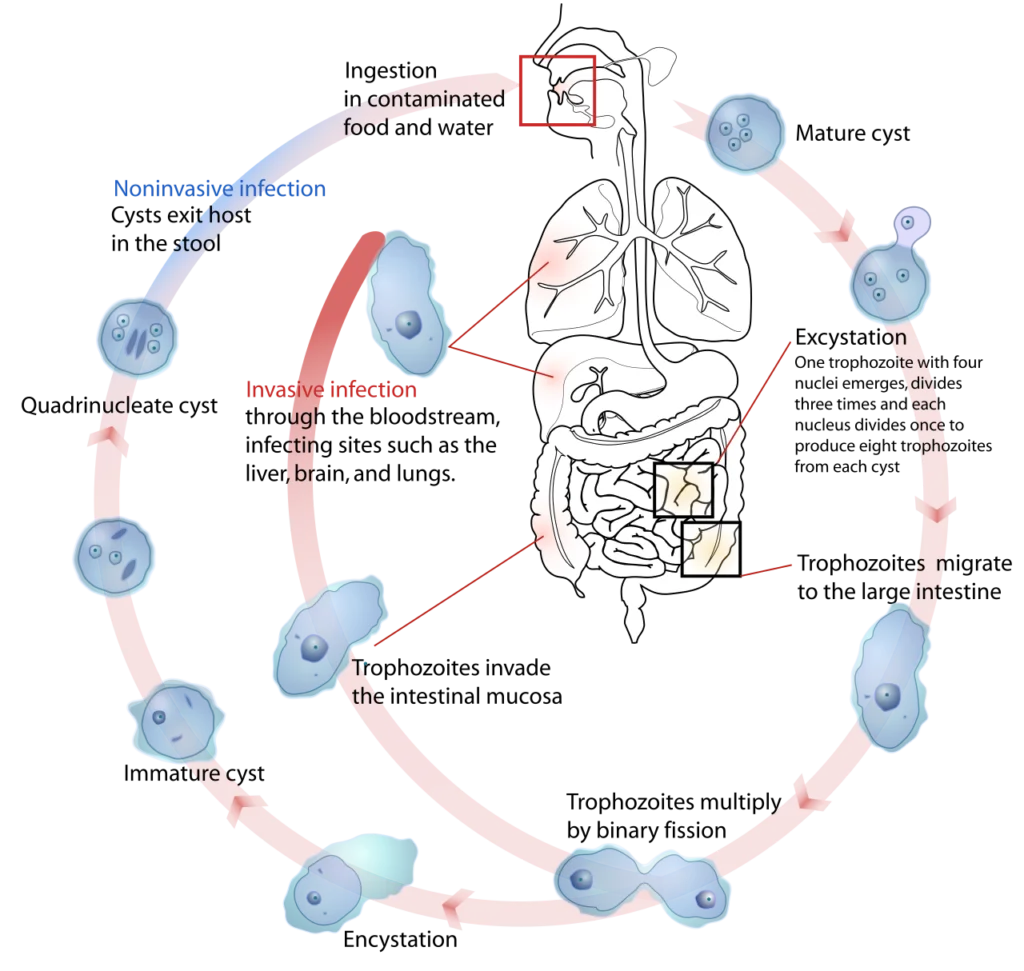
Life Cycle Stages
- Active Stage (Trophozoite):
- Exists only within the host or in fresh loose feces.
- Dormant Stage (Cyst):
- Survives outside the host in various environments, including water, soil, and on food, especially under moist conditions.
Modes of Transmission
- Fecal-Oral Route:
- Infection occurs when a person ingests something (like water or food) contaminated with E. histolytica cysts.
- Direct contact with contaminated surfaces or fingers can lead to swallowing cysts.
- Survival Outside the Host:
- Cysts are killed by heat and freezing temperatures.
- They can survive for a few months outside the host.
- Infection Process:
- Upon ingestion, cysts release trophozoites in the digestive tract.
Pathogenic Nature and Symptoms
- Discovery and Description:
- The pathogenic nature of E. histolytica was first reported by Fedor A. Lösch in 1875 and named by Fritz Schaudinn in 1903.
- Disease Manifestation:
- Infection can range from asymptomatic to causing amoebic dysentery or liver abscesses.
- Symptoms include severe dysentery, bloody diarrhea, weight loss, fatigue, abdominal pain, and amoeboma.
- Tissue Invasion:
- The amoeba can invade the intestinal wall, creating lesions and causing intestinal symptoms.
- It can reach the bloodstream or peritoneal cavity, potentially affecting vital organs like the liver, lungs, brain, and spleen.
- Liver abscesses are a common and severe outcome of tissue invasion.
- Observation in Amoeba:
- Ingested red blood cells are sometimes visible in the amoeba cell cytoplasm.
Genome of Entamoeba Histolytica
The genomic study of Entamoeba histolytica, a significant parasitic protozoan, has provided profound insights into its biology and pathogenicity. The genome sequencing and subsequent analyses have revealed various aspects of its genetic makeup. Here is an overview presented in a list and point format:
Initial Sequencing and Updates
- First Sequencing (2005):
- The E. histolytica genome was initially sequenced and annotated in 2005.
- Updated Reassembly (2010):
- The genome underwent reassembly and reannotation in 2010, enhancing the understanding of its genetic composition.
Genome Composition
- Size and Gene Prediction:
- The genome consists of approximately 20 million base pairs.
- It contains about 8,160 predicted genes.
- Transposable Elements:
- The genome includes both known and novel transposable elements.
- Major transposable elements are non-LTR retrotransposons, divided into families named EhLINEs and EhSINEs (EhLINE1,2,3 and EhSINE1,2,3).
- Functional Assignments and Pathways:
- Functional assignments have been revised and updated.
- Additional information incorporated includes metabolic pathways, Gene Ontology assignments, curation of transporters, and generation of gene families.
Unique Features
- Endonuclease Protein in EhLINE1:
- EhLINE1 encodes an endonuclease (EN) protein, alongside reverse transcriptase and nucleotide-binding ORF1.
- The EN protein shows similarity to bacterial restriction endonuclease, indicating potential horizontal gene transfer from prokaryotes.
- snoRNAs with Opisthokont-like Features:
- The genome includes snoRNAs (small nucleolar RNAs) with features resembling those in opisthokonts.
- E. histolytica U3 snoRNA (Eh_U3 snoRNA) shares sequence and structural similarities with Homo sapiens U3 snoRNA.
Oro-fecal mode of spread
The oro-fecal route of transmission is a significant pathway for various infectious diseases. This mode primarily involves the ingestion of pathogens through the mouth (oro) that have been contaminated by fecal matter. Here’s an explanation of the oro-fecal spread, particularly focusing on the lifecycle stages of a pathogen that adopts this mode, such as in the case of amoebic infections.
Cystic Stage
- Ingestion and Survival:
- Cysts are ingested and can survive in the environment for up to 3 months.
- They are resilient to various conditions, including desiccation and some chemicals.
- Environmental Resistance:
- Cysts can endure water for about a month and land-based fecal matter for over 12 days to 3 months.
- They tolerate temperatures up to 50°C and stomach acidity.
- Excystation Process:
- In the small intestine, specifically the ileum, cysts disintegrate under enzymatic influence, releasing quadrinucleate amoebae.
- These amoebae undergo division, forming trophozoites.
- Development in the Intestine:
- The resulting trophozoites migrate to the large intestine, particularly settling in the cecal area.
- They grow, feed, and reproduce in this environment.
Trophozoite Stage
- Colon Infection:
- Trophozoites establish an infection in the colon, often forming flask-shaped ulcers.
- Invasion and Feeding:
- These organisms invade intestinal crypts and can consume red blood cells (RBCs).
- They are capable of causing ulcers in the intestinal lining.
- Extraintestinal Spread:
- Trophozoites may enter the bloodstream, leading to abscesses in other parts of the body, like the liver.
- Transformation into Cysts:
- Trophozoites can transform into precysts and eventually into mature cysts, containing about four nuclei.
- These cysts are then excreted in the stool.
The oro-fecal mode of spread is a critical concept in understanding the transmission of many intestinal infections. It underscores the importance of proper hygiene and sanitation practices, especially in preventing the ingestion of water or food contaminated with fecal matter. This route of transmission is a key area of focus in public health and epidemiology, aiming to reduce the spread of infections that utilize this pathway.
Pathogenesis of amoebiasis by E. Histolytica
Amoebiasis, caused by the protozoan parasite Entamoeba histolytica, involves a complex pathogenic process. Understanding this process is crucial for diagnosing and treating the disease effectively. Here’s an overview of the pathogenesis in a list and point format:
Trophozoite Activity
- Survival and Infectivity:
- Trophozoites, the active form of E. histolytica, cannot survive outside the human body and are not directly infectious in this form.
- Movement in the Intestine:
- These trophozoites actively move within the intestine.
- Feeding Habits:
- They feed on bacteria, protozoa, and intestinal cells.
- Trophozoites can also ingest red blood cells (RBCs).
Enzymatic Action
- Secretion of Enzymes:
- E. histolytica secretes a range of enzymes, including histolysin.
- Histolysin plays a crucial role in allowing trophozoites to invade submucosal tissues.
Mucosal Ulceration
- Development of Dysentery:
- In cases where dysentery develops, mucosal ulceration becomes more severe.
- This leads to significant destruction of intestinal tissues.
- Sloughing of Epithelium:
- The overlying epithelium sloughs off, exposing the underlying necrotic areas.
- Regenerative Process:
- Following destruction, a regenerative process often occurs.
- This can lead to thickening of the intestinal wall due to fibrosis.
Organs damaged by amoeba
Amoebic infections, particularly those caused by the parasite Entamoeba histolytica, can lead to significant damage to various organs in the human body. The pathogenic process often starts in the intestines but can spread to other areas via the bloodstream. Here’s an overview of the organs commonly affected by amoebic infections:
Primary Organ Affected
- Liver:
- Trophozoites can enter the portal circulation, leading to liver abscesses.
- Conditions such as hepatic amoebiasis and amoebic hepatitis can develop.
- Hepatic abscesses can range from single to multiple formations.
Secondary Organ Involvement
- Lungs:
- The infection can spread from the liver to the lungs, potentially crossing the diaphragm.
- This can result in lung abscesses.
- Other Organs:
- The heart, brain, spleen, gonads, and skin can also be affected.
- These cases are typically considered secondary amoebiasis.
Transmission Factors
- Mechanical Vectors:
- Flies and cockroaches can act as mechanical vectors, aiding in the spread of amoebiasis.
Pathogenesis of Entamoeba Histolytica
Entamoeba histolytica, a parasitic protozoan, is known for causing amoebiasis in humans. Understanding its pathogenesis is crucial for diagnosing and managing the infection effectively. Here’s an overview of the pathogenic process:
Host-Protective Mechanism
- Serum Antibodies:
- Patients with amoebiasis often have detectable serum antibodies.
- These antibodies are used in the diagnosis of amoebiasis.
- Unclear Protective Role:
- The exact role of these antibodies in offering protection is not fully understood.
Complement System Activation
- Activation Pathways:
- E. histolytica trophozoites can activate the complement system through both alternative and classical pathways.
- Resistance to Lysis:
- While the complement system is generally amoebicidal, pathogenic strains of E. histolytica show resistance to complement-mediated lysis.
Strain Variability
- Tissue-Invasive Strain:
- About 10% of E. histolytica strains can invade tissues.
- This strain can cause diarrhea, with or without mucosal ulceration, and potentially spread to the bloodstream.
- It can lead to liver abscesses and affect other organs.
- Non-Invasive Strain:
- The more common strain of E. histolytica is usually asymptomatic or causes mild diarrhea.
- This strain is less severe and less likely to lead to serious complications.
Epidemiology of Entamoeba Histolytica
Entamoeba histolytica is a significant cause of disease worldwide, particularly in areas with poor sanitation. Its epidemiology has been studied extensively since its first description in the 19th century. Here’s an overview of the epidemiological aspects of Entamoeba histolytica:
Historical Background
- First Description:
- E. histolytica was first described in 1875, based on a case involving a young Russian peasant.
- Discovery:
- The organism was discovered by D.F. Losch in 1873 in St. Petersburg, Russia, observing amoebae in the stool of a peasant.
Global Distribution and Prevalence
- Cosmopolitan Disease:
- E. histolytica is found worldwide, but its distribution is not related to climate.
- Influence of Sanitation and Hygiene:
- The prevalence of E. histolytica is more closely related to inadequate environmental sanitation and poor personal hygiene.
- Global Infection Rates:
- It is estimated that E. histolytica infects about 10% of the global population, with actual prevalence potentially around 1%.
- Geographical Hotspots:
- The disease is more common in tropical and subtropical regions, including parts of Africa, Asia, Mexico, China, and South America.
Modes of Transmission
- Feco-oral Route:
- The primary mode of spread is feco-oral, where infective cysts are ingested through contaminated food, water, or hands.
Impact and Mortality
- Significance as a Parasitic Cause of Death:
- E. histolytica is the third most common cause of death from parasitic diseases.
- Around 500 million people are infected globally, with approximately 100,000 deaths annually.
Carriers and Active Disease
- Asymptomatic Carriers:
- Individuals can carry the parasite without symptoms, typically when cysts and trophozoites lack ingested red blood cells (RBCs).
- Active Disease:
- Active disease is indicated by trophozoites with ingested RBCs in the stool.
Clinical presentation of Entamoeba histolytica (Amoebiasis)
Amoebiasis, caused by the parasite Entamoeba histolytica, manifests in various forms, ranging from asymptomatic to severe symptomatic infections. The World Health Organization (WHO) in 1969 categorized these presentations as follows:
Asymptomatic Infection
- No Visible Symptoms:
- Individuals may carry the parasite without showing any clinical symptoms.
Symptomatic Infections
Intestinal Amoebiasis
- Dysentery:
- Characterized by severe diarrhea with blood and mucus in the stool.
- Nondysenteric Colitis:
- Presents as mild intestinal problems, with symptoms less acute than dysentery.
Extraintestinal Infection
- Hepatic Infections:
- Can manifest as acute nonsuppurative hepatitis or liver abscesses.
- Pulmonary Abscess:
- Though rare, amoebiasis can lead to pulmonary abscesses.
- Other Rare Extraintestinal Involvements:
- Involvement in areas other than the liver and lungs is uncommon.
Types of Amoebiasis Presentation
Acute Amoebic Dysentery
- Severe Diarrhea:
- Accompanied by fever (100°C to 102°C) and an incubation period of 1 to 4 weeks.
- Diagnosis:
- Based on the detection of trophozoites or cysts in the stool.
Chronic Amoebiasis
- Recurrent Symptoms:
- Periodic attacks of diarrhea interspersed with mild intestinal issues.
- Symptoms:
- Include diarrhea, dysentery, abdominal pain, cramping, flatulence, anorexia, weight loss, and chronic fatigue.
Complications and Other Symptoms
- Amoebic Liver Disease:
- Manifests as fever and abdominal pain, often leading to an amoebic liver abscess.
- Amoebic Colitis:
- Presents with non-bloody diarrhea and abdominal cramps.
- Ulceration in the large intestine can progress to granuloma formation.
- Amoeboma:
- Occurs primarily in the cecum and sigmoid colon, potentially leading to intestinal obstruction.
- Lab Findings:
- Acutely ill patients may show normal WBC and hemoglobin counts, and are usually afebrile.
- Patients with severe conditions often exhibit leukocytosis and mild anemia.
- Eosinophilia:
- Amoebiasis typically does not cause eosinophilia.
- Rare Manifestations:
- In rare cases, E. Histolytica can infect the brain, optic nerve, and face, leading to severe consequences.
Laboratory Diagnosis of Entamoeba histolytica
Diagnosing Entamoeba histolytica, the causative agent of amoebiasis, involves various laboratory techniques. These methods are crucial for accurate identification and effective treatment. Here’s an overview of the laboratory diagnosis process:
Stool Examination
- Initial Examination:
- Fresh stool is examined using direct stool smear and concentration methods like zinc sulfate flotation or formalin-ether technique.
- Identification of Trophozoites and Cysts:
- Motile trophozoites are observed in fresh, warm stool, while both trophozoites and cysts can be seen in fixed stool specimens.
- Stool samples should be examined for three consecutive days unless positive results are obtained earlier.
- Characteristics of Trophozoites:
- Size: 15 to 20 µm with a small central nucleus.
- Possible inclusion of red blood cells (RBCs) and occasionally bacteria in the cytoplasm.
- Smear Preparation:
- Use a wire loop to transfer a small amount of blood and mucus onto a slide, cover, and examine without saline.
- Another slide is prepared with eosin, which does not stain living amoeba but highlights motile amoeba against a pink background.
- Diagnostic Features:
- Trophozoites of E. histolytica show active amoeboid movements, ingested RBCs, and a single nucleus with central karyosomes.
Cyst Identification
- Characteristics of Cysts:
- Cysts are round, measuring 10 to 15 µm, with 1 to 4 nuclei, small karyosomes, and rounded chromatoidal bars.
- Immature cysts may have 1 to 2 nuclei, while mature cysts typically have 4 nuclei.
- Chromatoid bodies are usually seen in immature cysts and do not stain with iodine.
- Special Staining:
- Special stains like Burrow’s or Sargeaunt’s are required for staining chromatoid bodies.
- Differentiating from Other Species:
- E. coli cysts have 8 nuclei and splintered chromatoidal bars.
- Cysts smaller than 10 µm may belong to other species like E. nana or E. hartmanni.
Serological Tests
- EIA (Enzyme Immunoassay):
- An antibody-dependent test used for diagnosing amoebiasis.
- Antigen Detection:
- Antigen-dependent tests are also available for diagnosis.
- ELISA and Other Methods:
- Various ELISA methods are used, with high sensitivity in detecting intestinal amoebiasis and invasive cases.
Sensitivity in Different Cases
- Asymptomatic Cases:
- Detected in about 10% of cases through these tests.
- Mild Diarrhea Cases:
- Less than 50% detection rate in carriers with mild symptoms.
- Invasive Amoebiasis:
- High detection rate of 85% to 90% in patients with invasive amoebiasis.
- Comparative Sensitivity:
- ELISA, IHA (Indirect Hemagglutination), and LA (Latex Agglutination) tests are more sensitive than gel diffusion methods.
Treatment of Entamoeba histolytica
The management of infections caused by Entamoeba histolytica, a protozoan parasite responsible for amoebiasis, primarily involves pharmacotherapy. The treatment regimen is centered around specific anti-parasitic medications. Here’s a brief overview:
Primary Medication
- Metronidazole:
- Metronidazole is the primary drug of choice for treating Entamoeba histolytica infections.
- It is effective in targeting the active stages of the parasite in the body.
Supplemental Treatment
- Iodoquinol:
- Alongside Metronidazole, Iodoquinol may be used as a supplementary medication.
- This combination helps in ensuring a comprehensive treatment approach, addressing both active and dormant stages of the parasite.
The treatment strategy for amoebiasis focuses on eliminating the parasite from the patient’s system, alleviating symptoms, and preventing complications. Metronidazole, often complemented by Iodoquinol, forms the cornerstone of this therapeutic approach.
Prevention, How to control the disease
Amoebiasis, caused by the Entamoeba histolytica parasite, is a preventable disease largely influenced by environmental and personal hygiene factors. Effective prevention and control measures are crucial in reducing the spread of this infection. Here’s a comprehensive guide:
Environmental Sanitation
- Use of Closed Latrines:
- Implementing closed latrines helps prevent fecal contamination of the environment.
- Water Supply Protection:
- Ensure water sources are not contaminated with fecal material.
- Sanitary Disposal of Garbage:
- Proper garbage disposal systems are essential to maintain a clean environment.
Personal Hygiene Practices
- Hand Washing:
- Wash hands thoroughly with soap at least three times after defecation.
- Always wash hands before eating.
- Food Safety:
- Protect food from flies and cockroaches, which can carry cysts.
- Boil water to at least 55 °C to kill E. histolytica cysts.
- Avoid consuming uncooked or green salads that might contain cysts.
- Thoroughly wash fruits and vegetables before consumption.
Community Health Measures
- Health Education:
- Educate food handlers, school communities, and health centers about amoebiasis prevention.
- Avoid Use of Human Feces as Fertilizers:
- Human feces can be a source of cysts and should not be used as fertilizer.
- Screening in the Food Industry:
- Regular health checks for food industry workers to identify and treat asymptomatic carriers.
- Vector Control:
- Implement measures to control flies and other insects that can spread the disease.
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.