What is Salmonella?
Salmonella is a group of gram-negative bacillus bacteria that is responsible for causing food poisoning and subsequent infections in the intestinal tract. While some infections can be effectively treated, there are certain strains that have developed resistance to antibiotics, making them potentially deadly. Consequently, Salmonella infections should not be underestimated and require careful attention.
There are two major species of Salmonella: S. bongori and S. enterica. Salmonella is closely related to Escherichia coli (E. coli) bacteria, with the two diverging from a common ancestor approximately 150 million years ago. Over time, Salmonella has adapted and can now be found in various niches within the environment.
Salmonella has undergone several methods of classification, but there is no universally agreed-upon approach. However, one of the most recent classifications used by the Center for Disease Control (CDC) upon the recommendations of the World Health Organization (WHO) is as follows:
Domain: Bacteria – Salmonella are prokaryotes, meaning they have a simple cell structure without membrane-bound organelles.
Order: Enterobacteriales – Salmonella belongs to this order, which consists of gram-negative rods (Bacillus) that typically move using flagella and do not form endospores or microcysts.
Family: Enterobacteriaceae – This is the only family within the Order Enterobacteriales and comprises rod-shaped gram-negative bacteria.
Genus: Salmonella
Species: Salmonella has two main species, namely S. bongori and S. enterica.
Subspecies: S. bongori has a single subspecies referred to as Subspecies V.
In addition to subspecies, there are numerous serotypes of Salmonella, estimated to range from 2,200 to about 4,400 serotypes/serovar. Serotype grouping is based on cell surface antigens.
Some of the subspecies of Salmonella enterica are:
- S. enterica I
- S. salamae II
- S. arizonae IIIa
- S. diarizonae IIIb
- S. houtenae IV
- S. indica VI
The various serotypes and subspecies of Salmonella demonstrate its genetic diversity, which plays a significant role in its pathogenicity and ability to cause infections in humans and animals.
Overall, Salmonella is a versatile and potentially harmful group of bacteria that requires careful monitoring and control, especially in food safety and public health practices, to prevent outbreaks of foodborne illnesses.
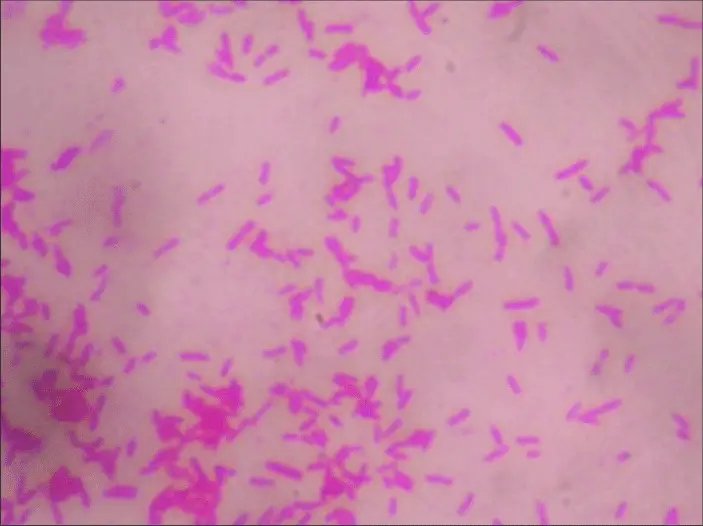
Salmonella Microscopy with Gram Stain
The source of Salmonella can be traced back to various origins, and obtaining a sample for analysis typically involves collecting specimens directly from patients or contaminated water and foods. The primary sources are as follows:
- Patient (Feces): When investigating Salmonella infections in individuals, a common approach is to obtain samples directly from patients’ feces. Salmonella can colonize the intestinal tract of infected individuals and be shed in their fecal matter. Analyzing these samples allows healthcare professionals and researchers to identify the presence of the bacteria and determine the specific strain responsible for the infection.
- Contaminated Water: Salmonella can contaminate water sources through various means, such as sewage runoff, agricultural runoffs, or inadequate sanitation practices. Drinking water contaminated with Salmonella can lead to waterborne infections and outbreaks. To investigate such cases, water samples need to be collected and tested to confirm the presence of the bacteria.
- Contaminated Foods: One of the most common ways Salmonella enters the human body is through the consumption of contaminated foods. Foods such as raw or undercooked meat (especially poultry and eggs), unpasteurized dairy products, raw fruits and vegetables, and contaminated water used for washing produce can carry the bacteria. Foodborne outbreaks of Salmonella infections can affect large numbers of people. To identify the source of such outbreaks, samples of the suspected foods must be collected and analyzed.
After obtaining samples from the potential sources mentioned above, microbiologists and laboratory professionals culture the Salmonella bacteria. This involves placing the collected samples on appropriate agar or growth media that provides the necessary nutrients for the bacteria to grow and multiply. By culturing the bacteria, the number of Salmonella cells can be increased, making it easier to detect and identify the pathogen through various laboratory techniques and tests.
It is important to identify the source of Salmonella infections to implement appropriate control measures and prevent further spread of the bacteria. Proper sanitation, food safety practices, and water treatment are essential in reducing the risk of Salmonella contamination and subsequent foodborne or waterborne illnesses. Additionally, prompt diagnosis and treatment of infected individuals are crucial to prevent severe complications and reduce the potential for further transmission.
Requirements
The term “Requirements” refers to the essential items and materials needed to perform a specific task or process. In the context provided, the requirements are related to conducting a Gram stain, a commonly used laboratory technique to differentiate bacteria into two main groups based on their cell wall composition. The Gram stain is a fundamental method in microbiology used to identify and classify bacteria.
To perform a Gram stain, the following requirements are necessary:
- Clean Glass Slide: A clean glass slide serves as the surface on which the bacterial sample will be spread. It is essential to ensure that the slide is free from any contaminants that could interfere with the staining process or affect the accuracy of the results.
- Heat (Bunsen Burner): The Bunsen burner is a heat source used in the Gram staining process. It is required for heat-fixing the bacterial sample onto the glass slide. Heat-fixing helps the bacteria adhere to the slide, kill the bacteria, and coagulate cell proteins, which aids in better staining.
- Gram Stain Reagents: The Gram stain reagents are a set of specific dyes used to stain the bacterial cells. The most commonly used Gram stain reagents include:
- a. Crystal Violet: The primary stain that imparts a purple color to both Gram-positive and Gram-negative bacteria.
- b. Iodine: The mordant that enhances the binding of the crystal violet to the bacterial cell wall, forming a complex that is retained by Gram-positive bacteria.
- c. Alcohol or Acetone (Decolorizer): The decolorizing agent that differentiates between Gram-positive and Gram-negative bacteria by removing the crystal violet-iodine complex from Gram-negative bacteria.
- d. Safranin: The counterstain that is applied after decolorization, providing a contrasting red color to Gram-negative bacteria.
- Staining Rack: A staining rack is a useful tool used to hold multiple glass slides during the staining process. It keeps the slides organized and prevents smudging or contamination.
- Sample: The sample, in this case, refers to the bacterial specimen to be analyzed. It could be a bacterial culture grown in a laboratory setting or a sample collected from a patient or an environmental source. The sample is spread onto the glass slide before the staining process begins.
These requirements are essential for successfully performing the Gram staining technique in microbiological laboratories. The Gram stain is a valuable tool that allows microbiologists to identify the morphology and Gram reaction (Gram-positive or Gram-negative) of bacteria, providing valuable information for further characterization and identification of bacterial species.
Sample Preparation and Procedure
Sample preparation and the procedure for performing a Gram stain, a common laboratory technique used to differentiate bacteria based on their cell wall composition, are outlined as follows:
- Prepare the Smear: Using a clean glass slide, place a small amount of the bacterial sample at the center of the slide. The sample can be obtained from a bacterial culture or collected from a patient or environmental source. To spread the sample, use a cotton swab stick or a wire loop. It is crucial to ensure that both the slide and the cotton swab or wire loop are clean to prevent contamination.
- Air Dry and Heat Fix: Allow the smear on the glass slide to air dry completely. Once dry, heat fix the slide by gently passing it over the flame of a Bunsen burner approximately three times. Heat fixing helps the bacterial cells adhere firmly to the slide and prevents them from getting washed off during the staining process. Be cautious not to overheat the slide, as excessive heat can lead to cell distortion or damage.
- Staining Process:
- a. Crystal Violet Stain: Place a few drops of crystal violet onto the bacterial smear. Let the stain sit on the slide for about 30 seconds to 1 minute. The crystal violet will dye the bacterial cells a purple color.
- b. Gram Iodine (Mordant): Add a few drops of Gram iodine (mordant) to the slide. Allow the mordant to react with the crystal violet for approximately 30 seconds to 1 minute. The iodine forms a complex with the crystal violet, enhancing the retention of the stain in Gram-positive bacteria.
- c. Decolorization with Alcohol: Add a few drops of alcohol (95% alcohol or acetone) to the slide. Let the alcohol sit on the slide for about 10 seconds. The alcohol acts as a decolorizer, removing the crystal violet-iodine complex from Gram-negative bacteria.
- d. Safranin Counterstain: Apply a few drops of safranin (counterstain) to the slide. Allow the counterstain to sit on the slide for a short time. Safranin will dye the Gram-negative bacteria a contrasting red color.
- e. Rinse with Water: After each staining step, gently wash the slide with water to remove excess stain or reagent.
- Remove Excess Water: Carefully blot the slide with tissue paper to remove excess water, being cautious not to disturb the bacterial smear.
- Microscopic Examination: Place the prepared slide under a microscope. Begin with the lower power objective lens to locate the bacterial cells. Observe the stained bacteria to determine their Gram reaction (Gram-positive or Gram-negative), which is based on the color they retain after staining.
Following these steps, the Gram stain allows microbiologists to observe the morphology and cell wall characteristics of bacteria, providing valuable information for bacterial identification and classification. The Gram stain is a widely used technique in microbiology and is an important tool in diagnosing bacterial infections.
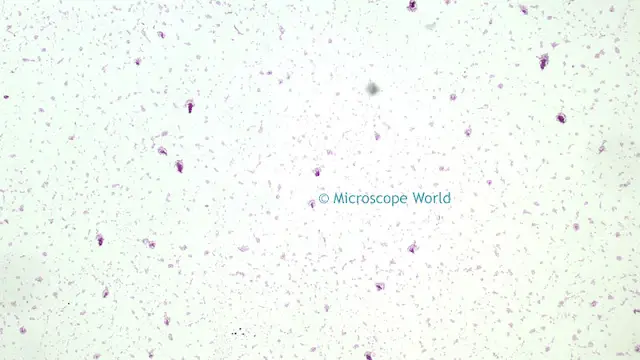
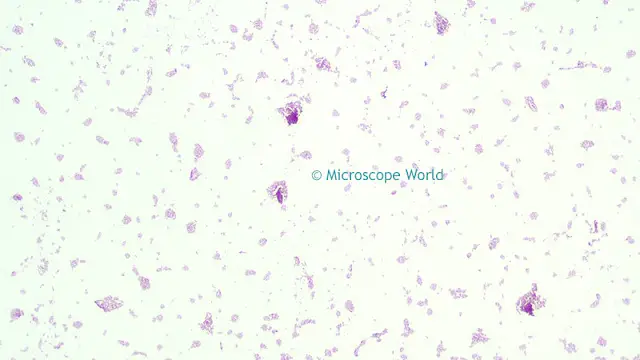
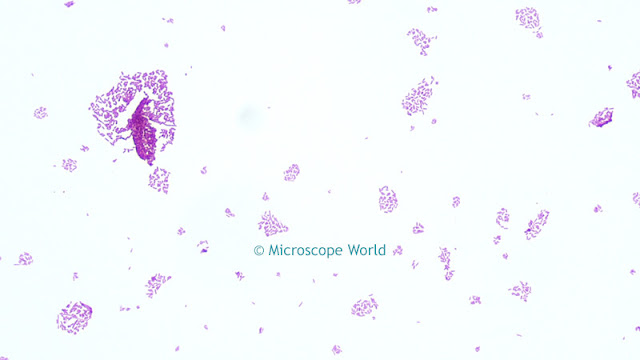
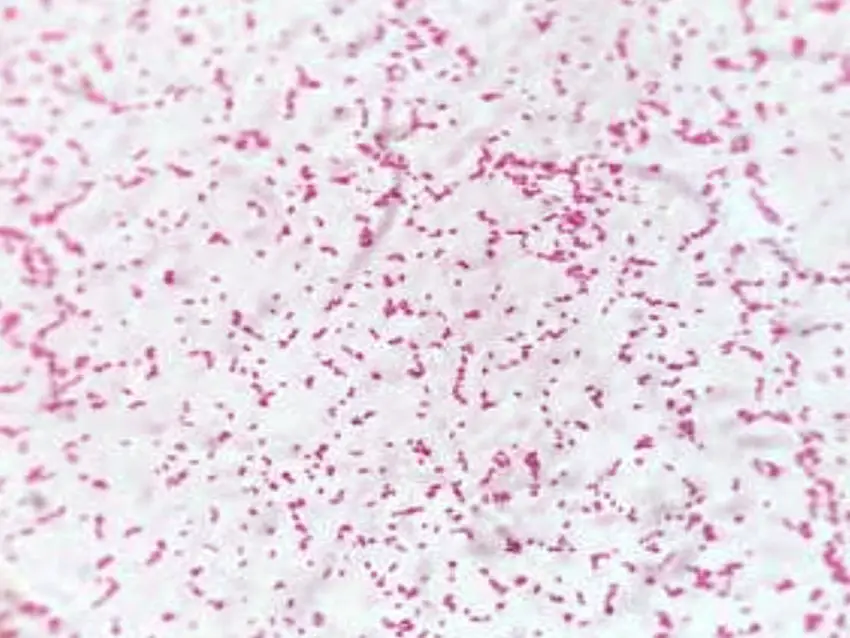
Observation of Salmonella Under Microscope

FAQ
How does Salmonella appear under a microscope?
Salmonella appears as rod-shaped bacteria, typically measuring about 2-5 micrometers in length. They have a distinct cell wall and may exhibit motility through flagella.
What staining technique is commonly used to visualize Salmonella under a microscope?
Gram staining is commonly used to visualize Salmonella under a microscope. This technique helps distinguish between Gram-positive and Gram-negative bacteria based on their cell wall properties.
Can Salmonella be seen under a regular light microscope?
Yes, Salmonella can be observed under a regular light microscope. Microbiologists use high magnification objectives (typically 100x oil immersion lens) to visualize the bacteria clearly.
What is the typical magnification required to observe Salmonella in detail?
To observe Salmonella bacteria in detail, a magnification of at least 1000x is usually necessary. This can be achieved using an oil immersion lens.
What color does Salmonella appear after Gram staining?
Salmonella will appear purple or violet after Gram staining if it is a Gram-negative bacterium.
How can you differentiate Salmonella from other similar bacteria under the microscope?
Microbiologists can differentiate Salmonella from other bacteria by its characteristic rod-shaped morphology and specific staining reaction. Additional biochemical tests are also performed for further identification.
Does Salmonella have any unique identifying features when viewed under a microscope?
While Salmonella shares a general rod-shaped morphology with other bacteria, it can often be distinguished by its motility, which is seen as movement through flagella.
Can Salmonella be easily distinguished from other bacteria, such as E. coli, under the microscope?
Distinguishing Salmonella from other bacteria like E. coli may require additional tests beyond just microscopic observation. Both bacteria have similar shapes and can be Gram-negative, making differentiation based solely on morphology challenging.
Can you see individual Salmonella cells or are they usually observed in clusters?
Salmonella cells can be observed individually or in small clusters, depending on the sample preparation and bacterial density.
How long does it take to prepare a slide and observe Salmonella under a microscope?
The time required to prepare a slide and observe Salmonella under a microscope can vary depending on the complexity of the sample and the staining process. Typically, it may take around 30 minutes to 1 hour from sample preparation to microscopic examination.
Good work done for researchers