IGCSE Biology 118 Views 1 Answers
Sourav PanLv 9November 14, 2024
Explain how using antibiotics only when essential can limit the development of resistant bacteria such as MRSA
Explain how using antibiotics only when essential can limit the development of resistant bacteria such as MRSA
Please login to save the post
Please login to submit an answer.
Sourav PanLv 9May 15, 2025
Using antibiotics only when essential is a critical strategy in limiting the development of resistant bacteria, such as methicillin-resistant Staphylococcus aureus (MRSA). This approach is central to antimicrobial stewardship programs, which aim to optimize antibiotic use and reduce the incidence of antibiotic resistance.
Importance of Prudent Antibiotic Use
- Reducing Unnecessary Prescriptions: By prescribing antibiotics only for confirmed bacterial infections, healthcare providers can minimize exposure to these drugs. This reduces the chances of bacteria developing resistance due to selective pressure from antibiotic use. For instance, studies have shown that implementing stewardship programs can lead to significant reductions in the prevalence of MRSA and other multidrug-resistant organisms (MDROs) .
- Targeted Therapy: When antibiotics are used, they should be based on culture results and susceptibility testing whenever possible. This targeted approach ensures that the most appropriate antibiotic is selected, which not only enhances treatment efficacy but also limits the use of broad-spectrum antibiotics that can disrupt normal flora and promote resistance .
- Education and Awareness: Educating healthcare professionals and patients about the appropriate use of antibiotics is essential. Awareness campaigns can help change prescribing behaviors and encourage patients to understand when antibiotics are necessary, thereby reducing demand for unnecessary prescriptions .
Impact on MRSA Development
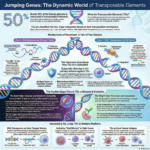
- Limiting Resistance Mechanisms: MRSA and other resistant strains develop through mechanisms such as gene mutation and horizontal gene transfer. By using antibiotics judiciously, we can slow down these processes, making it less likely for resistant strains to emerge and proliferate .
- Improving Clinical Outcomes: Effective antibiotic stewardship has been linked to improved patient outcomes, including higher cure rates for infections while simultaneously decreasing adverse effects associated with unnecessary antibiotic use .
- Cost-Effectiveness: Reducing the incidence of resistant infections not only improves patient health outcomes but also lowers healthcare costs associated with prolonged hospital stays and more complex treatments required for resistant infections
0
0 likes
- Share on Facebook
- Share on Twitter
- Share on LinkedIn
0 found this helpful out of 0 votes
Helpful: 0%
Helpful: 0%
Was this page helpful?