What is Blood grouping?
- Blood grouping, commonly referred to as blood typing, is a method used to categorize blood based on the presence or absence of specific antigens on the surface of red blood cells (RBCs) and the corresponding antibodies in the plasma. This classification is essential because it determines the compatibility of blood for transfusions and various medical procedures.
- The concept of blood grouping was first introduced in 1901 by Karl Landsteiner, who identified the A, B, and O blood groups. Since then, the understanding of blood groups has expanded significantly. The International Society of Blood Transfusion (ISBT) now recognizes 43 distinct blood group systems. However, the ABO and Rh systems remain the most widely used and clinically significant.
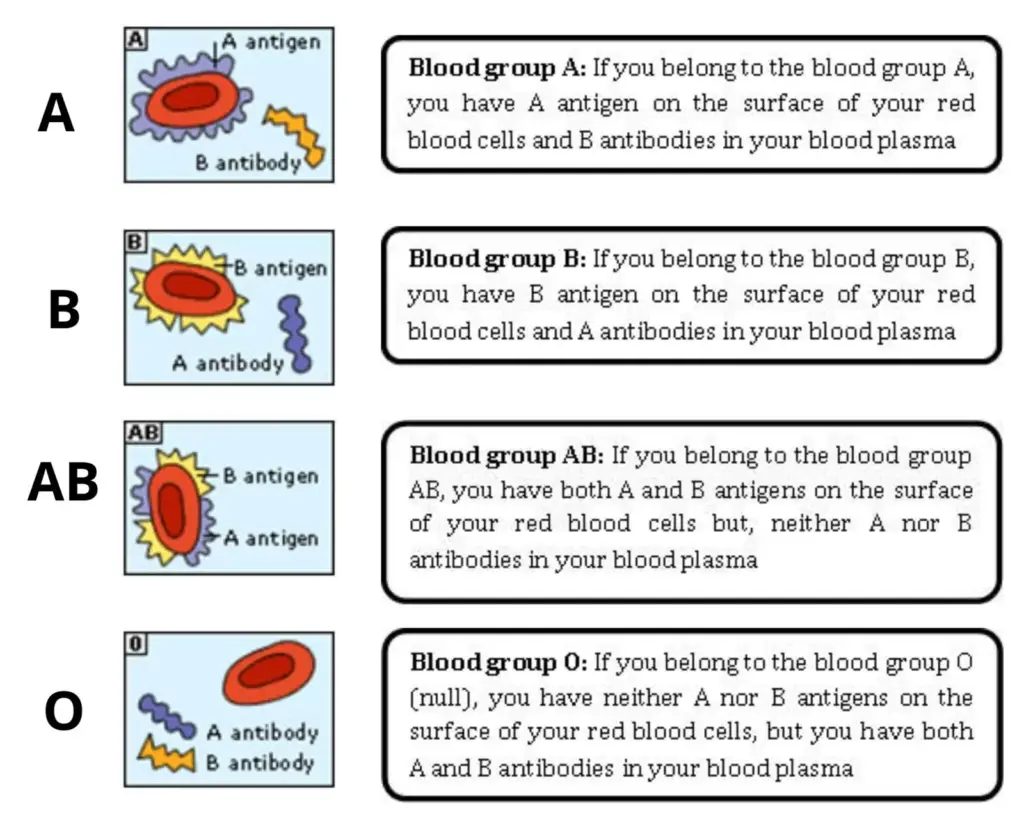
- In the ABO system, blood is classified into four primary types: A, B, AB, and O. This classification is based on the presence or absence of two antigens, A and B, on the surface of the RBCs and their corresponding antibodies, anti-A and anti-B, in the plasma. Therefore, a person with type A blood has A antigens on their RBCs and anti-B antibodies in their plasma. Similarly, someone with type B blood has B antigens and anti-A antibodies. Type AB individuals have both A and B antigens but lack both antibodies, while type O individuals lack both antigens but have both antibodies.
- The process of identifying an individual’s blood type is known as blood typing. It involves mixing a sample of the person’s blood with known antisera. If agglutination (clumping) occurs, it indicates the presence of the corresponding antigen in the blood. For instance, if a person’s blood agglutinates when mixed with anti-A serum but not with anti-B serum, then they have type A blood.
- Besides the ABO system, the Rh system is another crucial blood grouping system. It is based on the presence or absence of the Rh factor, also known as the D antigen. Individuals who have this antigen are termed Rh-positive, while those without it are Rh-negative.
- Understanding blood groups is vital for various medical procedures, especially blood transfusions. Transfusing incompatible blood can lead to severe reactions, which can be fatal. Therefore, before any transfusion, both the donor and the recipient’s blood types are tested to ensure compatibility.
- In conclusion, blood grouping is a fundamental concept in medicine that ensures the safe administration of blood and blood products. With advancements in science, our understanding of blood groups has expanded, leading to the identification of numerous blood group systems. However, the ABO and Rh systems remain the cornerstone of blood transfusion medicine.
Common Blood Group Systems
The blood grouping system is a methodical classification of blood based on the presence or absence of specific antigens and antibodies in the red blood cells and serum. This system is pivotal for various medical procedures, especially transfusions, to ensure compatibility and prevent adverse reactions. Here’s an in-depth exploration of the various blood grouping systems:
- ABO Blood Group System: The ABO system is the most prevalent and clinically significant blood grouping system. It is based on three genes: A, B, and O, located on chromosome 9. The presence or absence of these genes determines an individual’s blood group:
- Blood group A: Individuals with genotypes AA or AO possess the A antigen on their red blood cells and have anti-B antibodies in their serum.
- Blood group B: Those with genotypes BB or BO have the B antigen on their red blood cells and anti-A antibodies in their serum.
- Blood group AB: Individuals with this genotype have both A and B antigens on their red blood cells but lack both anti-A and anti-B antibodies in their serum.
- Blood group O: Those with genotype OO lack both A and B antigens on their red blood cells but have both anti-A and anti-B antibodies in their serum.
- Rh Blood Group System: The Rh system, also known as the Rhesus system, is the second most important blood grouping system. It comprises six genes: C, c, D, d, E, and e. The D gene is particularly significant in this system:
- Rh positive: Individuals with the D-antigen present on their red blood cells.
- Rh negative: Individuals lacking the D-antigen on their red blood cells.
Notably, unlike the ABO system, anti-D antibodies do not naturally circulate in those lacking the D-antigen. However, they can develop if an Rh-negative individual receives a transfusion with Rh-positive blood.
- Lewis Blood Group System: The Lewis system is characterized by the Lewis antigen, which is produced in tissues, secreted into body fluids, and then absorbed onto the red blood cell membrane. As it is secreted, it’s also termed as secretor antigens. This system has been linked to growth delays in children and occasional transfusion reactions. The primary phenotypes in this system are Le (a+ b-), Le (a- b+), and Le (a- b-).
- MNS Antigen Blood Group System: Introduced by Landsteiner and Levine in 1927, this system revolves around two genes, glycophorin A and glycophorin B. It is governed by an autosomal locus on chromosome 4 with alleles LM and LN. Typically, the antibodies anti-M and anti-N in this system are of the IgM type and are infrequently associated with transfusion reactions.
- Lutheran Grouping System: This system encompasses four allelic antigens, each representing a single amino acid substitution in the Lutheran glycoprotein located on chromosome 19. It holds minimal clinical significance since antibodies against this blood group are rare.
- P Blood Group System: This system classifies blood based on P-type carbohydrate antigens. Significant antigens in this system include P1, P2, and PK, which can lead to transfusion reactions and erythroblastosis fetalis under specific circumstances.
- Kell Blood Group System: The Kell system, third in clinical significance after ABO and Rh, has 25 known antigens. Of these, six (K, k, Kpa, Kpb, Jsa, and Jsb) are of particular clinical importance due to their potential to cause transfusion reactions and erythroblastosis fetalis.
- Duffy Blood Group System: The Duffy system, identified in 1950, is based on Fy glycoprotein antigens. While antibodies against these antigens are rare, they can occasionally lead to transfusion reactions and erythroblastosis fetalis.
- Kidd Blood Group System: Discovered in 1951, the Kidd system is based on Kidd (Jk) glycoprotein antigens. Antibodies against these antigens can cause severe hemolytic transfusion reactions.
- Yt Blood Group System: Also known as the Cartwright system, the Yt system is based on Yt antigens. Antibodies against these antigens can lead to delayed-type transfusion reactions.
- Xg Blood Group System: Identified in 1962, the Xg system is based on Xg protein antigens. This system is not associated with any known transfusion reactions.
- Dombrock Blood Group System: The Dombrock system, discovered in 1965, is based on Do antigens. Severe transfusion reactions have been reported in association with Dombrock antigen-antibody interactions.

The ABO Blood Group System
The ABO blood group system stands as a cornerstone in the realm of human blood classification. This pivotal system was unveiled by Karl Landsteiner in 1901, a groundbreaking discovery that stemmed from his observation of agglutination, or clumping, when mixing blood from different individuals. By 1900, Landsteiner had discerned that the agglutination was due to the interaction between specific antigens present on red blood cells (RBCs) and antibodies in the plasma. This led to the initial classification of blood into groups A, B, and C. However, by 1910, the designation “C” was replaced with “O” by Ludwik Hirszfeld and Emil Freiherr von Dungern.
The essence of the ABO system lies in the presence or absence of two specific antigens, A and B, on the surface of RBCs, and their corresponding antibodies, anti-A and anti-B, in the plasma. These antigens are glycoproteins encoded by the ABO gene.
To elucidate further:
- Type A Blood: RBCs possess A antigens on their surface and the plasma contains anti-B antibodies.
- Type B Blood: RBCs display B antigens, while the plasma is rich in anti-A antibodies.
- Type AB Blood: RBCs exhibit both A and B antigens, but the plasma lacks both sets of antibodies.
- Type O Blood: RBCs are devoid of both A and B antigens, but the plasma contains both anti-A and anti-B antibodies.
The genetic underpinning of this system is governed by three alleles: i, IA, and IB. Both IA and IB are dominant over i, but they exhibit co-dominance with each other. Consequently, individuals with IAIA or IAi alleles manifest type A blood, those with IBIB or IBi alleles display type B blood, IAIB allele carriers have type AB blood, and those with ii alleles present with type O blood.
The significance of the ABO system is underscored by the potential for severe hemolytic reactions if incompatible blood types are transfused. Such reactions arise from the violent interaction between A and B antigens with their respective antibodies, leading to RBC clumping and blood clotting. Without prompt intervention, these reactions can be fatal. Therefore, the ABO blood group system remains paramount in ensuring the safety of blood transfusions and other medical procedures involving blood.
The Rh Blood Group System
The Rh blood group system, a pivotal classification in human blood typing, was unveiled by Karl Landsteiner and A.S. Weiner in 1940. This discovery was rooted in their identification of Rh antigens present on the membrane of human red blood cells (RBCs). The nomenclature “Rh” is derived from the Rhesus monkeys, whose blood played a crucial role in the initial identification of these antigens in human RBCs.
To date, researchers have identified 49 distinct Rh antigens, also termed Rh factors. However, of these, only five – D, C, c, E, and e – hold clinical significance. Among them, the Rh (D) antigen stands out due to its highly immunogenic nature, making it the most extensively studied and tested Rh antigen. This is primarily because of its association with hemolytic reactions. These antigens are integral to transmembrane proteins, predominantly functioning as ion channels. The genetic blueprint for these antigens is encoded by two genes: the RHD gene and the RHCE gene.
Classification within the Rh system is straightforward:
- Rh Positive (Rh +ve): Blood that contains the Rh (D) antigen on its RBCs.
- Rh Negative (Rh -ve): Blood devoid of the Rh (D) antigen on its RBCs.
Interestingly, individuals with Rh (D) antigens on their RBCs inherently lack anti-D Rh antibodies in their plasma. However, when Rh (D) antigen is introduced into a bloodstream that lacks this antigen, the body promptly synthesizes anti-D Rh antibodies in response.
Among the antibodies associated with the Rh system, anti-D, anti-C, anti-c, and anti-e are known to trigger hemolytic transfusion reactions. The anti-D antibody, in particular, is renowned for its potency, capable of inducing severe, sometimes fatal, immune reactions. Consequently, it is imperative to determine the Rh type of blood prior to any transfusion or medical procedure to ensure compatibility and patient safety.
Prevalence/Frequency of ABO and Rh Blood Type
The distribution of blood types across the global population varies, with some blood types being more common than others. The ABO and Rh systems are the primary determinants for classifying these blood types.
- Type O+ Blood: This blood type stands out as the most prevalent globally. Approximately 42% of the world’s population possesses O+ blood, making it the most common blood type.
- Type A Blood: A+ blood is found in roughly 31% of individuals worldwide. On the other hand, A- blood is considerably rarer, with only about 2.5% of the global population having this blood type.
- Type B Blood: B+ blood is present in around 15% of people globally. In contrast, B- blood is less common, with a mere 1% of the world’s population having this type.
- Type AB Blood: AB+ blood is found in about 5% of the global populace. Its counterpart, AB-, is the least common of all blood types, with only 0.5% of people worldwide possessing it.
- Rh Factor: The presence or absence of the Rh factor further classifies these blood types into positive (+) or negative (-). The Rh factor, specifically the Rh (D) antigen, is a significant determinant. A staggering 95% of the global population has Rh+ blood, indicating the presence of the Rh (D) antigen in their red blood cells (RBCs). Conversely, only about 5% lack this antigen, classifying them as Rh-.
It’s crucial to note that the distribution of these blood types can vary significantly based on ethnicity and geographic location. Such variations can influence medical practices, especially in areas like blood transfusion, where compatibility is paramount.
| Blood Type (ABO and Rh system) | Percentage Prevalence Globally |
|---|---|
| A+ | 31% |
| A- | 2.5% |
| B+ | 15% |
| B- | 1% |
| AB+ | 5% |
| AB- | 0.5% |
| O+ | 42% |
| O- | 3% |
The objective of Blood Grouping
- To determine the blood group and Rh factor of an individual
Blood Grouping Principle
Blood grouping is a fundamental concept in immunohematology, based on the principle of agglutination. Agglutination is an immunological reaction that occurs when specific antigens on the surface of red blood cells (RBCs) interact with their corresponding antibodies in the serum. This interaction results in the clumping or aggregation of the RBCs, which is visible to the naked eye.
The ABO blood grouping system classifies blood based on the presence or absence of two primary antigens, A and B, on the surface of RBCs and their corresponding antibodies, anti-A and anti-B, in the serum. Therefore:
- Blood group A individuals possess A antigens on their RBCs and have anti-B antibodies in their serum.
- Blood group B individuals have B antigens on their RBCs and anti-A antibodies in their serum.
- Blood group AB individuals carry both A and B antigens on their RBCs, but lack both anti-A and anti-B antibodies in their serum.
- Blood group O individuals lack both A and B antigens on their RBCs but have both anti-A and anti-B antibodies in their serum.
The discovery of the ABO blood grouping system can be credited to Karl Landsteiner in 1901. His groundbreaking work paved the way for safer blood transfusions by ensuring compatibility between the donor and recipient. Before this discovery, attempts at blood transfusion often resulted in adverse reactions, sometimes even leading to the patient’s death. Landsteiner’s contribution to medicine was so significant that he was awarded the Nobel Prize in Physiology or Medicine in 1930.
Besides the ABO system, another pivotal discovery was the Rhesus (Rh) blood grouping system. This system is based on the presence or absence of the Rh factor on the surface of RBCs. The Rh system was elucidated through the combined efforts of Levine and Stetson in 1939, and Landsteiner and Weiner in 1940. With the establishment of reliable tests for Rhesus grouping, transfusion reactions became exceedingly rare.
In essence, the principle of blood grouping revolves around the agglutination reaction. The antigens present on the RBCs’ surface, whether from the ABO or Rh system, interact with their corresponding antibodies in the serum. This interaction results in visible clumping, which is the basis for determining an individual’s blood group. Understanding this principle is crucial for various medical procedures, especially blood transfusions, to ensure the safety and well-being of patients.
Material Required
- Anti A Sera
- Anti B Sera
- Anti RhD Sera
- Cavity slide
- Disposable Mixing Stick
- Blood Lancet
- 70% Alcohol/ Spirit
- Cotton
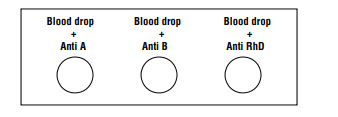
ABO blood Grouping Procedure
The determination of the ABO blood group is a fundamental procedure in immunohematology. It involves identifying the specific antigens present on the surface of an individual’s red blood cells (RBCs). There are two primary methods employed for this purpose: the tube method and the tile method. Both methods rely on the principle of agglutination, where the interaction between specific antigens on RBCs and their corresponding antibodies results in visible clumping of the cells. Here’s a detailed and sequential explanation of both procedures:
Tube Method:
- Begin by taking two glass tubes.
- Add 1 volume (typically 1 drop) of a 3-5% RBC suspension from the patient into each tube.
- Into the first tube, add 1 ml of anti-A serum. In the second tube, introduce 1 ml of anti-B serum.
- Gently tap the base of the tubes to mix the contents thoroughly.
- Allow the tubes to stand at room temperature for approximately five minutes.
- Subsequently, centrifuge the tubes at the lowest setting for one minute.
- After centrifugation, carefully observe the tubes for any signs of agglutination or clumping of the RBCs.
Tile Method:
- Start with a clean, grease-free tile.
- Place a drop of anti-sera A on one end of the tile and a drop of anti-sera B on the opposite end.
- Next, place a drop of the RBC suspension onto each drop of antiserum.
- Using a clean applicator, mix the RBC suspension with the antiserum thoroughly.
- Gently rock the tile back and forth for about 2 minutes.
- Observe the tile for any visible agglutination or clumping of the RBCs. This can be seen with the naked eye, but for a more detailed observation, a microscope can be used.
Result of ABO blood Grouping
Slide Method
- Blood Group A: Agglutination observed at the end with antiserum A indicates the presence of A antigens on the RBCs, confirming the blood group as A.
- Blood Group B: If agglutination is seen at the end with antiserum B, it signifies the presence of B antigens on the RBCs, determining the blood group as B.
- Blood Group AB: When agglutination occurs at both ends (those with antiserum A and antiserum B), it indicates the presence of both A and B antigens on the RBCs, confirming the blood group as AB.
- Blood Group O: In the absence of any agglutination at both ends, it suggests that neither A nor B antigens are present on the RBCs, determining the blood group as O.
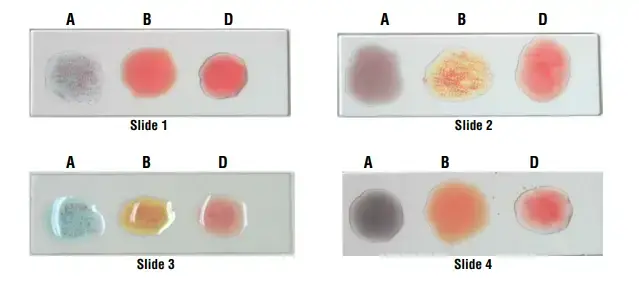
| S. No. | Anti A | Anti B | Anti RhD | Blood Group |
| Slide 1 | Agglutination | No agglutination | Agglutination | A +ve |
| Slide 2 | No agglutination | Agglutination | Agglutination | B +ve |
| Slide 3 | Agglutination | Agglutination | Agglutination | AB +ve |
| Slide 4 | No agglutination | No agglutination | Agglutination | O +ve |
Tube Method
- Blood Group A: Agglutination is observed in the tube containing antiserum A. This indicates the presence of A antigens on the RBCs and confirms the blood group as A.
- Blood Group B: If agglutination occurs in the tube with antiserum B, it signifies the presence of B antigens on the RBCs, determining the blood group as B.
- Blood Group AB: When agglutination is seen in both tubes (those containing antiserum A and antiserum B), it indicates the presence of both A and B antigens on the RBCs. This confirms the blood group as AB.
- Blood Group O: In the absence of any agglutination in both tubes, it suggests that neither A nor B antigens are present on the RBCs. This determines the blood group as O.
Blood grouping tube method interpretations:
| Tube 1 | Tube 2 | Tube 3 | Tube 4 | Tube 5 | Blood group |
| anti-A | anti-B | anti-AB | A1- red blood cells | B-red blood cells | |
| Negative | Negative | Negative | Positive | Positive | O |
| Positive | Negative | Positive | Negative | Positive | A |
| Negative | Positive | Positive | Positive | Negative | B |
| Positive | Positive | Positive | Negative | Negative | AB |
False results in ABO blood grouping
Procedural Mistakes:
- Dirty Glassware: Unclean apparatus can interfere with the test results.
- Improper Cell-to-Serum Ratio: This can lead to either false-positive or false-negative outcomes.
- Contaminated or Expired Reagents: These can produce false-positive results.
- Over-Centrifugation: This can lead to false-positive outcomes.
- Under-Centrifugation: This can result in false-negative outcomes.
- Missed Hemolysis: Overlooking hemolysis can turn a positive result into a negative one.
- Careless Reading: A hasty or inattentive reading can be interpreted as a negative result.
- Absence of Optical Aid: Not using an optical aid might lead to false-negative readings.
- Misidentification: Incorrectly identifying samples or reagents can yield both false-positive and false-negative results.
- Incorrect Interpretation: Misreading or misinterpreting results can lead to both false-positive and false-negative outcomes.
Other Causes of False-Positive Results:
- Antibody-Coated RBCs: These cells may agglutinate in a high-protein medium.
- Recent Blood Transfusion: This can result in a mixed cell appearance during testing.
- Unusual Genotype Antigen: Blood groups like A2B and A3B might react weakly with reagent anti-sera anti-A.
- Diseases: Conditions like acute leukemia or non-malignant hemolytic disorders can weaken ABO antigens.
- Polyagglutinable RBCs: These cells can agglutinate due to genetic or acquired surface abnormalities.
- Gram-Negative Bacteria: These can mimic group B activity.
- High Levels of Proteins: This can cause rouleux formation, which might be mistaken for agglutination.
- Blood Group-Specific Substances: These can neutralize anti-A and anti-B when unwashed RBCs are used.
- Unwashed RBCs in Multiple Myeloma: This can lead to false-positive results due to rouleux formation.
- Certain Drugs: Drugs like dextran and contrast media can cause cellular aggregation, mimicking agglutination.
- Age-Related Effects: Newborns might not have developed antibodies yet, while older adults might have weakened antibody levels.
Rh Blood Grouping Procedure/Determination of Rh Factor
The determination of the Rh factor, commonly referred to as the Rhesus factor, is a crucial aspect of blood typing in immunohematology. This factor is characterized by specific antigens present on the surface of red blood cells (RBCs). The presence or absence of these antigens plays a significant role in blood transfusions and various other medical procedures.
The Rh factor was first discovered by Landsteiner and Wiener in the “Rhesus” monkey, from which the name “Rhesus factor” was derived. Among the various Rh antigens, antigen D stands out due to its high antigenicity. This means that antigen D has a strong ability to induce an immune response, making it the primary focus when determining the Rh factor in blood.
The procedure to determine the Rh factor involves exposing a blood sample to antiserum D. If agglutination or clumping of the RBCs occurs upon exposure to this antiserum, it indicates the presence of the D antigen on the RBCs, and the individual is termed “Rh-positive.” Conversely, if no agglutination is observed, it suggests the absence of the D antigen, and the individual is termed “Rh-negative.”
In conclusion, the determination of the Rh factor is an essential procedure in the field of blood typing. It provides valuable information about the presence or absence of specific Rh antigens, primarily the D antigen, on an individual’s RBCs. This information is vital for ensuring the compatibility of blood during transfusions and for understanding potential complications in medical scenarios, such as pregnancies where the mother and fetus have different Rh statuses.
Principle for Determination of Rh Factor
The determination of the Rh factor, often referred to as the Rhesus factor, is a fundamental procedure in immunohematology. This factor is characterized by specific antigens present on the surface of red blood cells (RBCs). The principle behind determining the Rh factor revolves around the presence or absence of the D antigen, which is the most prominent among the genes responsible for producing the Rh factor.
The D antigen, secreted by the D gene, is a key component in the RBCs of humans. Its presence or absence plays a pivotal role in classifying an individual’s Rh status. When conducting the determination procedure, a blood sample is exposed to antiserum D, which specifically reacts with the D antigen.
If, upon exposure to antiserum D, agglutination or clumping of the RBCs is observed, it indicates that the D antigen is present on the RBCs. In such cases, the individual is classified as “Rh-positive.” On the other hand, if no agglutination occurs, it suggests that the D antigen is absent from the RBCs, and the individual is termed “Rh-negative.”
In conclusion, the principle for the determination of the Rh factor is centered on the interaction between the D antigen on RBCs and antiserum D. This interaction, resulting in either agglutination or the lack thereof, provides a clear and concise method to ascertain an individual’s Rh status, which is crucial for various medical applications, especially blood transfusions.
Requirement for Determination of Rh Factor
- Patient’s Blood: The primary requirement is the blood sample from the patient or individual whose Rh status needs to be determined. This sample serves as the source from which the presence or absence of the D antigen will be identified. The blood sample is pivotal as it provides the actual material for testing and interaction with the antisera.
- Monoclonal Antisera D: The next essential component is the monoclonal antisera D. This antiserum contains antibodies that specifically react with the D antigen present on the surface of RBCs. The interaction between the antisera D and the D antigen results in agglutination or clumping of the RBCs, which is the basis for determining the Rh factor. To facilitate easy identification and prevent any potential confusion during the procedure, this antiserum is color-coded red. This color-coding ensures clarity and accuracy during the testing process.
- Tile/Tube: The final requirement is a tile or tube, which serves as the platform where the blood sample and antisera D are mixed and observed for any agglutination reactions. The choice between a tile and a tube often depends on the specific method or protocol being followed in the laboratory. Regardless of the chosen platform, its primary function is to provide a clear view of the interaction between the blood sample and the antisera, allowing for accurate observation and interpretation of results.
Procedure for Determination of Rh Factor
The determination of the Rh factor, often referred to as the Rhesus factor, is a pivotal procedure in immunohematology. This process identifies whether an individual’s red blood cells (RBCs) possess the D antigen, classifying them as either Rh-positive or Rh-negative. The procedure for determining the Rh factor is similar to that of the ABO blood grouping system and can be conducted using either the tube or tile method. Here’s a detailed and sequential explanation of both procedures:
Tube Method:
- Sample Preparation: Begin by taking a glass tube and adding 1 volume (typically 1 ml) of the patient’s blood.
- Addition of Antisera: To the same tube, add an equal volume of antisera D. This antiserum contains antibodies that specifically react with the D antigen present on RBCs.
- Mixing and Centrifugation: After adding the antisera, mix the contents of the tube thoroughly. Then, centrifuge the tube at a low speed for approximately 1 minute. This step ensures that any potential agglutination reactions are easily observable.
- Observation: After centrifugation, carefully inspect the tube for any signs of agglutination or clumping of the RBCs. This can be observed with the naked eye. For a more detailed observation, a microscope can be used.
Tile Method:
- Sample Placement: Start by placing a drop of the patient’s blood at one end of a clean, grease-free tile.
- Addition of Antisera: Gently place a drop of antisera D on top of the blood drop. This antiserum will interact with any D antigens present on the RBCs.
- Mixing: Using a clean toothpick or a specialized mixer, mix the blood sample and the antisera D thoroughly.
- Observation: Allow the mixture to sit for about 2 minutes. After this duration, inspect the tile for any visible agglutination or clumping of the RBCs.
Rh Blood Grouping Result
General Observation:
- Rh Positive: If agglutination or clumping of the RBCs is observed, it indicates the presence of the D antigen on the RBCs. Therefore, the individual is classified as “Rh positive.”
- Rh Negative: Conversely, if no agglutination is seen, it suggests the absence of the D antigen on the RBCs. In such cases, the individual is termed “Rh negative.”
Result for Slide Method:
- Positive Result: A positive result is indicated when agglutination is observed in the patient’s sample, while the control sample remains in suspension. This outcome confirms the presence of the D antigen, classifying the individual as Rh positive.
- Negative Result: A negative result is denoted when both the patient’s sample and the control sample show a smooth suspension without any agglutination. This outcome confirms the absence of the D antigen, classifying the individual as Rh negative.
Result for Tube Method:
- Rh-D Positive: A positive result for the Rh-D antigen is indicated by the presence of agglutination in the patient’s tube, while the control tube displays a smooth suspension. This observation confirms the presence of the D antigen on the RBCs, classifying the individual as Rh-D positive.
- Rh-D Negative: A negative result for the Rh-D antigen is denoted when both the patient’s tube and the control tube show a smooth suspension without any agglutination. This observation confirms the absence of the D antigen, classifying the individual as Rh-D negative.
False positive and negative result in slide and Tube method
In the realm of blood grouping, both the slide and tube methods are widely employed. However, like any scientific procedure, they are not without potential pitfalls. Understanding the causes of false results in these methods is crucial for accurate interpretation and subsequent medical decisions. Here’s a detailed exposition on the false-positive and false-negative results in both methods:
Slide Method
False-Positive Results:
- Drying of the Slide: If the slide dries out during the procedure, it can create an appearance similar to agglutination, leading to a false-positive result.
- Presence of Microclots: These tiny clots can mimic the appearance of agglutination. It’s essential to rule them out during interpretation.
- Inadequate Anticoagulant: An insufficient amount of anticoagulant can lead to clotting, which can be mistaken for agglutination.
False-Negative Results:
- Saline Suspension Issues: A saline suspension of the red blood cells (RBCs) might react weakly or not at all, leading to a false-negative result.
- Anemic Patients: In individuals with anemia, there are fewer RBCs available for testing, which can affect the outcome.
- Premature Reading: Interpreting the result in less than 2 minutes can yield a false-negative, especially with weak RBCs.
- Incorrect Reagents: Using the wrong reagents can lead to inaccurate results.
Tube Method
False-Positive Results:
- Extended Incubation: Leaving serum and RBCs together for an extended period can lead to rouleux formation due to the high protein medium. This formation can be mistaken for agglutination.
- Contaminating Antibodies: The anti-Rho (D) serum might contain antibodies with different specificities, leading to false results.
- Polyagglutinable RBCs: These RBCs can agglutinate in the presence of any serum protein reagents.
- Abnormal Serum Proteins: If a patient’s serum contains abnormal proteins, it can lead to false-positive results.
False-Negative Results:
- Improper Reagents: Using incorrect or expired reagents can yield inaccurate results.
- Rouleux Formation: If serum and cells are left together for too long, rouleux formation can occur, which might be misinterpreted as agglutination.
- Variant Antigens: RBCs with variant antigens, such as Cw or ces, might not react with standard reagents, leading to false-negative results.
Interpretation
- Blood Group A: When a blood sample is mixed with Anti A reagent, and agglutination is observed, it indicates the presence of A antigens on the RBCs. Therefore, the individual’s blood group is identified as “A.”
- Blood Group B: If agglutination is observed when the blood sample is mixed with Anti B reagent, it signifies the presence of B antigens on the RBCs. As a result, the individual’s blood group is determined to be “B.”
- Blood Group AB: In cases where agglutination is observed upon mixing the blood sample with both Anti A and Anti B reagents, it indicates the simultaneous presence of both A and B antigens on the RBCs. Consequently, the individual is classified as having blood group “AB.”
- Blood Group O: If no agglutination is observed when the blood sample is mixed with both Anti A and Anti B reagents, it suggests the absence of both A and B antigens on the RBCs. This result classifies the individual as having blood group “O.”
- Rh Factor Positive (+ve): The Rh factor, also known as the Rhesus factor, is another critical antigen present on RBCs. If agglutination is observed when the blood sample is mixed with Anti RhD reagent, it indicates the presence of the D antigen, which is a component of the Rh factor. Therefore, the individual is said to have a positive (+ve) Rh factor.
- Rh Factor Negative (-ve): Conversely, if no agglutination is observed upon mixing the blood sample with Anti RhD reagent, it signifies the absence of the D antigen. As a result, the individual is classified as having a negative (-ve) Rh factor.
| Reaction with Antisera | Agglutination Observed | Blood Group/Rh Factor |
|---|---|---|
| Anti A reagent | Yes | A |
| Anti B reagent | Yes | B |
| Anti A and Anti B reagent | Yes | AB |
| Anti A and Anti B reagent | No | O |
| Anti RhD reagent | Yes | Rh Positive (+ve) |
| Anti RhD reagent | No | Rh Negative (-ve) |
Importance of Blood Grouping
- Identification of Blood Type: One of the primary reasons for blood grouping is to ascertain an individual’s blood type. This knowledge is crucial, especially in emergency situations where a person might require an immediate blood transfusion. Besides, being aware of one’s blood group is essential for those who wish to donate blood. For potential donors, certain criteria must be met, including being between the ages of 17 and 66, maintaining good health, and weighing at least 50 Kg.
- Ensuring Safe Blood Transfusions: Blood transfusions are life-saving procedures, but they come with inherent risks if not conducted correctly. Therefore, before any transfusion, it’s imperative to perform cross-matching. This process ensures that the donor and recipient blood types are compatible. Incompatible transfusions can lead to severe complications, including the hemolysis of blood cells, which can be fatal.
- Significance During Pregnancy: Blood grouping gains added importance during pregnancy, especially concerning the Rh factor. It’s essential to determine the Rh factor of pregnant mothers. If an Rh-negative mother is carrying an Rh-positive child, there’s a potential risk of Rh sensitization. This condition can lead to various complications during pregnancy, affecting both the mother and the fetus. To mitigate this risk, Rh-negative pregnant women are typically administered Rh immunoglobulin (RhIg) around the 28th week of pregnancy. This intervention prevents the production of Rh antibodies for the remainder of the pregnancy, ensuring the safety of both the mother and the child.
Application of blood grouping
- Blood Transfusions: One of the primary applications of blood grouping is ensuring the safety of blood transfusions. Before any transfusion, it’s imperative to match the donor’s and the recipient’s blood types to prevent adverse reactions. Incompatible transfusions can lead to severe complications, emphasizing the importance of accurate blood grouping.
- Paternity Disputes: Blood grouping can be a tool in resolving paternity disputes. By comparing the blood groups of a child with potential parents, it can provide evidence to support or refute claims of biological relationships. However, it’s worth noting that while blood grouping can exclude certain individuals as biological parents, DNA testing is more definitive in confirming paternity.
- Hemolytic Disease of the Newborn: Blood grouping plays a crucial role in detecting and managing the hemolytic disease of the newborn (HDN). This condition arises when there’s an incompatibility between the blood types of the mother and the fetus, leading to the mother’s immune system attacking the fetus’s red blood cells. Early detection and intervention can prevent severe complications.
- Disease Susceptibility: Interestingly, one’s blood group can influence susceptibility to certain diseases. For instance, individuals with blood group O have been found to be more susceptible to peptic ulcers. Understanding this correlation can aid in preventive healthcare measures.
- Health Check-ups and Licensing: Blood grouping is often a part of routine health check-ups. Moreover, certain professions or activities, like driving, might require individuals to provide their blood group information during the licensing process. This information can be crucial in emergencies, ensuring that individuals receive compatible blood transfusions if needed.
Precautions
- Thorough Procedure Review: Before initiating the experiment, it’s essential to read the entire procedure. This ensures that the individual is well-prepared and familiar with each step, reducing the likelihood of mistakes.
- Safety First: Wearing gloves during the experiment is crucial. Gloves act as a barrier, protecting the individual from potential contaminants in the blood sample and ensuring that the sample remains uncontaminated.
- Slide Preparation: The slide, a primary tool in this procedure, must be clean and dry. Any contaminants or moisture on the slide can interfere with the results, leading to inaccurate readings.
- Handling of Antisera Reagent: Care must be taken to avoid touching the dropper of the antisera reagent directly to the blood sample. Direct contact can contaminate the reagent, compromising its efficacy in subsequent tests.
- Immediate Interpretation: Once the blood and antisera are mixed, the reaction should be interpreted immediately. Delaying interpretation can lead to changes in the sample, potentially skewing the results.
- Avoid Intermixing of Reagents: Precision is key in blood grouping. Therefore, it’s vital to ensure that antisera reagents do not get mixed up during the experiment. Intermixing can lead to false results, which can have serious implications, especially in clinical settings.
Blood Compatibility
Blood compatibility is a crucial aspect of transfusion medicine. It refers to the harmonious coexistence of donor and recipient blood without any adverse reactions. The human body has specific antigens and antibodies in the blood, and when incompatible blood types are mixed, it can lead to harmful reactions, including agglutination or clotting of the blood.
The ABO and Rh systems play pivotal roles in determining blood compatibility. These systems classify blood based on the presence or absence of specific antigens on the surface of red blood cells and corresponding antibodies in the plasma. Therefore, before any blood transfusion or organ transplantation, it’s imperative to ensure that the donor and recipient blood types are compatible.
In the Rh system, Rh-positive blood can only be transfused to another Rh-positive individual. Conversely, Rh-negative blood is compatible with both Rh-positive and Rh-negative recipients. When it comes to the ABO system, specific rules apply. For instance, individuals with type A blood cannot receive type B blood and vice versa. Those with type O blood can only receive type O, but they can donate to any blood type, earning them the title of “universal donors.” On the other hand, individuals with type AB blood are “universal recipients” as they can accept blood from any ABO group.
To further elucidate, here’s a compatibility chart:
| Donor Blood Type | A+ | A- | B+ | B- | AB+ | AB- | O+ | O- |
|---|---|---|---|---|---|---|---|---|
| A+ | √ | |||||||
| A- | √ | √ | ||||||
| B+ | √ | |||||||
| B- | √ | √ | ||||||
| AB+ | √ | |||||||
| AB- | √ | √ | ||||||
| O+ | √ | √ | √ | √ | ||||
| O- | √ | √ | √ | √ | √ | √ | √ | √ |
In the chart, “√” denotes compatibility between the donor and recipient blood types.
In conclusion, understanding blood compatibility is paramount to prevent severe transfusion reactions. Proper cross-matching and adherence to compatibility guidelines ensure the safety and efficacy of blood transfusions.
Transfusion Reactions Due to Incompatibility
Transfusion reactions are a significant concern in the medical field, particularly when there’s a mismatch between the donor and recipient’s blood. Such reactions can have varying degrees of severity, ranging from mild symptoms to life-threatening conditions. Here’s an in-depth look at transfusion reactions due to incompatibility:
Transfusion reactions arise from the adverse response of the recipient’s body to the transfusion of incompatible or mismatched blood. Specifically, a reaction takes place when the donor’s red blood cells (RBCs) interact with the recipient’s plasma. This adverse response is most likely to occur when the recipient’s plasma contains a high concentration of agglutinins against the donor’s RBCs. Depending on the severity, reactions can manifest as mild symptoms like hives and a slight fever or escalate to more severe conditions such as renal failure, shock, and even death. Broadly, these reactions are classified into two categories: non-hemolytic and hemolytic transfusion reactions.
Non-hemolytic Transfusion Reaction: This type of reaction can manifest anywhere from a few minutes to hours post-transfusion in cases of ABO incompatibility, or even a month later in instances of Rh incompatibility. Symptoms are generally mild and may include:
- Fever
- Difficulty in breathing
- Severe itching
Hemolytic Transfusion Reaction: Hemolytic reactions, associated with the breakdown of RBCs, can be acute or delayed:
- Acute Hemolytic Reaction: This reaction is typically a consequence of ABO incompatibility. It is characterized by the rapid hemolysis of the donor’s RBCs. Symptoms can include:
- Fever and chills
- Increased heart rate
- Shortness of breath
- Nausea and vomiting
- Reddish urine
- Low blood pressure
- Bronchospasm
- Rigor and back pain
- In severe cases, pulmonary edema and congestive cardiac failure might develop.
- Delayed Hemolytic Transfusion Reaction: This reaction can manifest between 1 to 5 days post-transfusion due to ABO blood group incompatibility. The breakdown of RBCs leads to an elevated presence of hemoglobin in the plasma, resulting in:
- Jaundice
- Cardiac shock
- Renal shutdown
In cases of Rh incompatibility, the delayed reactions typically commence when incompatible blood is transfused for the second time. The complications mirror those observed in ABO transfusion reactions.
In conclusion, ensuring blood compatibility is paramount to prevent these adverse reactions. Proper screening, testing, and adherence to transfusion protocols are essential to safeguard patients’ health and well-being.
Components of Blood
Blood, the vital fluid that circulates throughout the human body, plays a pivotal role in transporting nutrients, oxygen, and waste products. Comprising both liquid and cellular components, blood is a complex mixture that serves various functions essential for survival. Delving deeper into its composition, we can categorize blood into two primary segments: Plasma and Blood Cells.
- Plasma: Plasma is the liquid component of blood, making up about 60% of its total volume. Predominantly composed of water, plasma acts as a solvent, carrying a myriad of substances. These include proteins, enzymes, glucose, fat particles, salts, hormones, and antibodies. These constituents play crucial roles in various physiological processes, from immunity to metabolism.
- Blood Cells: Produced in the bone marrow by hematopoietic stem cells, blood cells can be broadly classified into three main types:
- Erythrocytes (Red Blood Cells or RBCs): Erythrocytes, responsible for the characteristic red hue of blood, are the most abundant cells in the bloodstream. Approximately 5 million RBCs are present in just 1 ml of blood. These biconcave, nucleus-lacking cells have a lifespan of around 120 days. Their primary function is oxygen transport, facilitated by the iron-rich protein, hemoglobin. Hemoglobin binds oxygen in the lungs and delivers it to tissues throughout the body. As RBCs age, they are systematically broken down, with certain organs like the liver processing their remnants.
- Leukocytes (White Blood Cells or WBCs): Leukocytes are the sentinels of the immune system. They exist in various forms, including neutrophils, lymphocytes, eosinophils, monocytes, and basophils. Each type has a specific role in defending the body against pathogens. An adult human typically has between 4,000 to 11,000 leukocytes per ml of blood. Their primary role is to combat infections, remove cellular debris, and eliminate aberrant or old cells.
- Thrombocytes (Platelets): Thrombocytes, or platelets, are instrumental in the blood clotting process. When an injury occurs, they act on clotting proteins, transforming fibrinogen into fibrin. This creates a meshwork where RBCs accumulate, forming a clot that halts bleeding and prevents pathogen entry. An adult’s blood usually contains between 200,000 to 500,000 platelets per ml.
References
- https://himedialabs.com/TD/HTI008.pdf
- https://vlab.amrita.edu/?sub=3&brch=69&sim=192&cnt=1
- https://w¯ww.labpedia.net/blood-banking-part-1-blood-groups-abo-and-rh-system-blood-grouping-procedures/
- http://www.histopathology.guru/academics/undergraduate-academics/rbc-bleeding-disorders-transfusion-medicine/blood-grouping/
- https://www.apollodiagnostics.in/blog/blood-types-and-blood-group-testing
- https://www.labtestsguide.com/blood-group-test-procedure
- https://www.healthline.com/health/how-to-find-out-your-blood-type#_noHeaderPrefixedContent