What are Blood Cells?
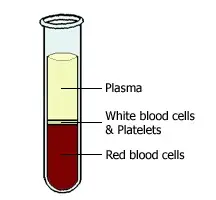
- Blood cells, also known as hematocytes or hemocytes, play an important role in the circulatory system’s operation. They are predominantly created in the red bone marrow via a process known as hematopoiesis. These cells account for approximately 45% of total blood volume, with blood plasma accounting for the remaining 55%.
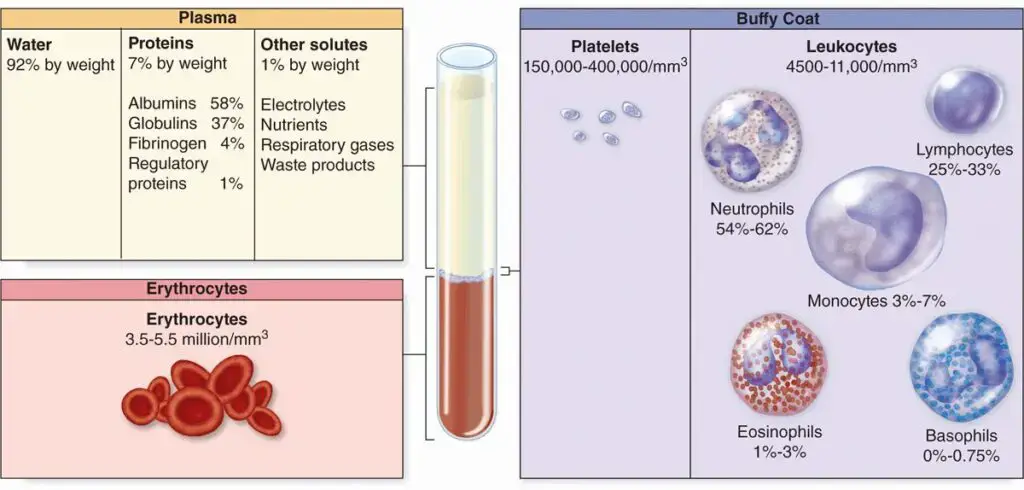
- Blood cells are classified into three types: red blood cells (erythrocytes), white blood cells (leukocytes), and platelets (thrombocytes). Red blood cells transfer oxygen from the lungs to the body’s tissues while also eliminating carbon dioxide, a waste product, from the tissues. They contain hemoglobin, a protein that binds to oxygen and gives them their characteristic red hue.
- White blood cells, on the other hand, play an important role in the immune system. They protect the body from pathogens such as bacteria and viruses, as well as other dangerous chemicals. White blood cells are classified into three types: lymphocytes, monocytes, and granulocytes. Granulocytes are further subdivided into three groups: neutrophils, eosinophils, and basophils. Each type of white blood cell plays a distinct role in fighting infections and supporting general body health.
- Platelets are required for blood coagulation, which is necessary to prevent excessive bleeding. When a blood vessel is injured, platelets clump together and form a plug to stop the bleeding. They also release molecules that start the coagulation process, which results in the creation of a clot that seals the wound.
- Hematology, or the study of blood cells, has made substantial contributions to our understanding of numerous blood illnesses and diseases. The discovery of diverse types of blood cells and their roles dates back to the 17th century, when scientists began examining blood samples with microscopes.
- The initial observation of red blood cells under a microscope by Jan Swammerdam in 1658 and the discovery of platelets by Alfred Donné in 1842 were significant milestones in the study of blood cells. The discovery of leukocytes in 1843 by Gabriel Andral and William Addison added to our understanding of the immune system. These breakthrough discoveries established the area of hematology as a medical speciality.
- Paul Ehrlich’s invention of staining techniques in 1879 enabled the careful examination and differentiation of distinct blood cell types. This aided in the detection and monitoring of disorders such as anemia, infections, and cancer using blood tests that assess the quantity and qualities of various blood cells.
- The study of blood cells is evolving as a result of technical advances and continuous research. Scientists and healthcare practitioners are better equipped to detect, treat, and manage a wide range of blood-related disorders as they unravel the complexity of blood cells, thereby improving patient outcomes and general health.
Blood Cells Definitions
Red blood cells (erythrocytes): Blood cells responsible for transporting oxygen from the lungs to the body’s tissues and removing carbon dioxide.
White blood cells (leukocytes): Blood cells involved in the body’s immune response, defending against infections and diseases.
Platelets (thrombocytes): Blood cells essential for blood clotting, preventing excessive bleeding by forming clots at the site of injuries or wounds.
Characteristics of Blood cells
Blood cells possess several distinct characteristics that contribute to their vital role in the body’s functioning:
- Red Blood Cells (RBCs): RBCs are small, biconcave, disk-shaped cells that lack a nucleus and other organelles. This unique structure allows them to efficiently transport oxygen from the lungs to the body’s tissues and remove carbon dioxide as waste.
- White Blood Cells (WBCs): Unlike RBCs, WBCs have a nucleus and other organelles. They are larger than RBCs and play a crucial role in the immune response, defending the body against infections and diseases.
- Platelets: Platelets are small cell fragments without a nucleus. They are essential for blood coagulation, forming clots to prevent excessive bleeding when a blood vessel is damaged.
- Bone Marrow: Blood cells are produced in the spongy tissue called bone marrow, located within the bones. It serves as the primary site for the generation and maturation of blood cells.
- Lifespan: Blood cells have a finite lifespan, ranging from a few days to a few months. They are constantly replenished by the bone marrow, ensuring a continuous supply of fresh blood cells.
- Disease Impact: Various diseases, infections, genetic abnormalities, and cancers can affect blood cells, leading to abnormal cell counts or compromised function.
- Diagnostic Tool: Blood tests are commonly used in medicine to evaluate a patient’s health by analyzing their blood cells. Abnormalities in cell counts or characteristics can provide important diagnostic information.
- Blood Transfusions: In certain medical conditions that affect blood cells, such as severe anemia or blood disorders, blood transfusions may be performed to introduce healthy blood cells or blood products from donors.
- Factors Influencing Blood Cells: Age, sex, and overall health can influence the composition and quantity of blood cells circulating in the body. Hormones, diet, and physical activity also impact blood cell synthesis and function.
- Cellular Movement: Blood cells are in constant motion, circulating throughout the body’s vascular system to deliver oxygen, nutrients, hormones, and other essential materials to various tissues and organs.
- Laboratory Methods: Microscopy, flow cytometry, and other laboratory techniques enable the visualization and study of blood cells, aiding in diagnostics, research, and monitoring of blood-related conditions.
- Collaboration and Communication: Blood cells collaborate with each other and with other cell types and tissues, playing essential roles in processes such as inflammation, wound healing, and immunological responses.
- Environmental Influence: Blood cells can be affected by environmental factors such as toxins, radiation, and diseases, which can disrupt their development, function, or survival.
- Research and Therapies: Blood cells, containing genetic material, offer valuable insights for research and diagnostics. Advances in studying blood cells have contributed to the discovery of therapies for various blood diseases and disorders, such as leukemia, lymphoma, and myeloma.
Contents of Blood Cells
Blood is composed of various components, each with its own unique role and characteristics. Here are the contents of blood cells:
- Plasma: Plasma is a straw-colored fluid that constitutes approximately 60% of blood volume. It is mostly water but also contains essential substances such as proteins (including albumin, clotting factors, antibodies, enzymes, and hormones), sugars (such as glucose), lipids (fat particles), electrolytes, and waste products. Plasma acts as a carrier for nutrients, hormones, and other molecules, and plays a role in regulating body temperature and maintaining blood pressure.
- Red Blood Cells (RBCs): Red blood cells, also known as erythrocytes, make up the bottom layer of blood when left undisturbed. They account for approximately 99% of blood cells and are responsible for transporting oxygen from the lungs to the body’s tissues and carrying carbon dioxide waste back to the lungs. RBCs are specialized cells that lack a nucleus and other organelles, allowing for maximum space to carry oxygen and giving them their characteristic red color.
- White Blood Cells (WBCs): White blood cells, also called leukocytes, are found in the middle white layer of blood when it separates. They play a crucial role in the body’s immune response, protecting against infections and diseases. There are several types of WBCs, including lymphocytes, monocytes, and granulocytes. Granulocytes further include neutrophils, eosinophils, and basophils. Each type of WBC has unique functions in identifying and eliminating pathogens, producing antibodies, and regulating immune responses.
- Platelets (Thrombocytes): Platelets are small cell fragments present in the middle layer of blood. They lack a nucleus and are crucial for blood clotting (coagulation). When a blood vessel is damaged, platelets gather at the site to form a plug and release substances that initiate clotting, preventing excessive bleeding.
- Bone Marrow: Bone marrow, located within the bones, is the primary source of all blood cells. It is a spongy tissue where stem cells differentiate and mature into specific blood cell types. Red blood cells, white blood cells, and platelets all originate from these stem cells in the bone marrow.
- Centrifugation: Centrifuging a blood sample can separate its components based on density. The denser elements, such as red blood cells, settle at the bottom due to the centrifugal force. This technique allows for the isolation of specific blood cell types or proteins. For example, plasma can be obtained by separating it from the other components and can be used to treat immunological deficiencies with antibodies or clotting problems with clotting factors. Red blood cells can also be isolated for transfusions.
Types of Blood cells
There are three main types of blood cells:
- Red blood cells (RBCs): RBCs, or erythrocytes, are the body’s most common type of blood cell. They are responsible for delivering oxygen to the body’s tissues from the lungs and returning carbon dioxide to the lungs from the rest of the body. Red blood cells (RBCs) are coloured red because of a protein called haemoglobin that binds to oxygen.
- White blood cells (WBCs): White blood cells (WBCs), sometimes called leukocytes, are an integral element of the immune system that works to ward off illness and infection. Lymphocytes, neutrophils, monocytes, eosinophils, and basophils are just few of the white blood cell kinds. Several types of white blood cells perform specialised tasks include making antibodies, fighting off invaders, and controlling inflammation.
- Platelets: When blood clots, it’s thanks in part to platelets, also called thrombocytes, which are pieces of larger cells. Platelets immediately clump together at the site of a blood vessel injury to form a plug and halt bleeding. In addition, they secrete substances that stimulate blood clotting, which ultimately leads to the creation of a firm clot that effectively closes the incision.
Red blood cells (RBC) or Erythrocytes
- Red blood cells (RBCs), also known as erythrocytes, play a vital role in the human body by transporting oxygen and carbon dioxide throughout the bloodstream. These small, disc-shaped cells lack a nucleus and most other organelles, allowing them to efficiently carry out their specialized functions.
- The unique structure and composition of red blood cells enable them to fulfill their essential role in oxygen transport. The presence of the protein hemoglobin, which is packed within RBCs, allows for the binding and transport of oxygen from the lungs to various tissues and organs in the body. Simultaneously, red blood cells collect carbon dioxide, a waste product, and transport it back to the lungs for elimination.
- The production of red blood cells occurs in the red bone marrow, a spongy tissue found within bones. The kidneys release a hormone called erythropoietin when they detect low oxygen levels in the body. Erythropoietin stimulates the production and maturation of red blood cells, ensuring an adequate supply to meet the body’s oxygen demands.
- The average lifespan of red blood cells is approximately 120 days. As they age and become less efficient, they are removed from circulation and metabolized by the liver and spleen. The constant renewal of red blood cells is crucial to maintaining a healthy blood supply.
- Medical professionals can assess the quantity and quality of red blood cells through blood tests like the complete blood count (CBC) and hematocrit. These tests provide valuable information about the overall health of the blood and can help diagnose conditions related to red blood cell abnormalities.
- Several disorders can arise from issues with red blood cells. Anemia, characterized by a deficiency in the number or quality of red blood cells, can lead to fatigue, weakness, and other symptoms. Conditions like sickle cell disease and thalassemia are genetic disorders that affect the structure or synthesis of hemoglobin, resulting in abnormal red blood cells.
- Environmental factors, such as exposure to toxins or radiation, can adversely affect red blood cells. Nutritional deficiencies, particularly in iron or vitamin B12, can also impair their production and function.
- In cases of severe anemia or bleeding disorders, transfusions of red blood cells may be necessary to address the resulting blood loss or lack of oxygen-carrying capacity. These transfusions provide a temporary boost to the red blood cell count and help restore normal oxygen transport.
- Advancements in research and technology have opened up new possibilities in the field of red blood cell therapy. For instance, gene therapy shows promise in treating conditions like sickle cell disease, offering potential long-term solutions to inherited blood disorders.
- In conclusion, red blood cells are essential components of the bloodstream responsible for transporting oxygen and carbon dioxide throughout the body. Their unique structure, function, and production are vital for maintaining overall health. Ongoing advancements in understanding red blood cells continue to drive progress in the diagnosis, treatment, and management of blood-related disorders.
Structure of Erythrocytes or Red blood cells (RBC)
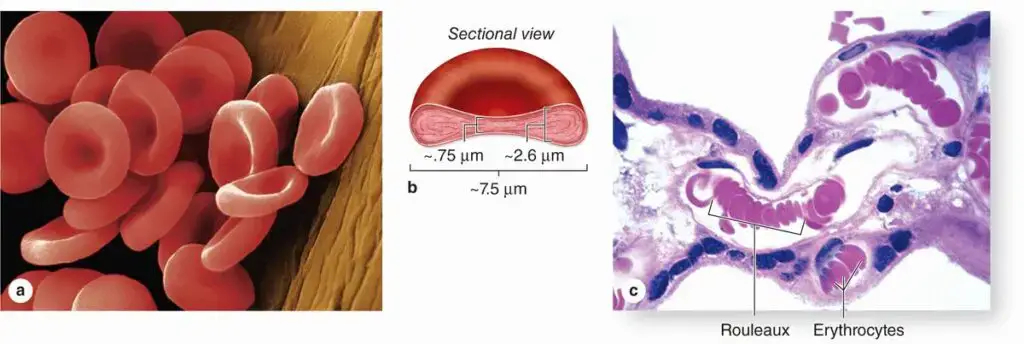
- Erythrocytes, or red blood cells (RBCs), possess a distinct structure that enables them to carry out their crucial role in oxygen transport. These specialized cells exhibit a biconcave, discoid shape and lack a nucleus. With a diameter of approximately 7.5 μm, they are thicker at the rim, measuring around 2.6 μm, while the center is much thinner, measuring only 0.75 μm.
- The biconcave shape of erythrocytes serves an important function in facilitating gas exchange. This unique structure provides a large surface area in relation to the volume of the cell, allowing for efficient uptake and release of oxygen and carbon dioxide.
- In a healthy individual, the concentration of erythrocytes in the blood varies slightly between genders. On average, women have approximately 3.9-5.5 million erythrocytes per microliter (μL or mm3) of blood, while men have around 4.1-6.0 million erythrocytes per μL.
- One notable characteristic of erythrocytes is their flexibility. This flexibility enables them to deform and adapt to the narrow dimensions and irregular shapes of blood vessels, ensuring smooth circulation throughout the body.
- The plasmalemma, or plasma membrane, of erythrocytes is well-studied and renowned for its properties. Comprising approximately 40% lipid, 10% carbohydrate, and 50% protein, it plays a crucial role in maintaining the integrity and functionality of the cell. The plasmalemma consists of a phospholipid bilayer, which provides support to the overall structure of the red blood cell. It also houses a network of proteins that form the cytoskeleton.
- The cytoskeleton is a complex arrangement of proteins within the erythrocyte that contributes to its structural integrity and flexibility. Key proteins in the cytoskeleton include spectrin, actin, band 3, protein 4.1, and ankyrin. These proteins maintain the shape and stability of the cell while allowing it to undergo deformations and maneuver through blood vessels.
- The cytoplasm of erythrocytes lacks organelles, such as the nucleus, mitochondria, and endoplasmic reticulum, to make room for a high concentration of hemoglobin. Hemoglobin, a protein responsible for oxygen transport, densely fills the cytoplasm of erythrocytes. It binds to oxygen in the lungs and releases it to tissues throughout the body, ensuring the proper delivery of oxygen for cellular respiration.
- In summary, the structure of erythrocytes is characterized by their biconcave shape, lack of a nucleus, and high concentration of hemoglobin. This unique structure, coupled with the flexibility provided by the cytoskeleton, allows red blood cells to efficiently transport oxygen and carbon dioxide throughout the body, ensuring proper cellular function and overall physiological well-being.
Functions of Erythrocytes or Red blood cells (RBC)
Erythrocytes, or red blood cells (RBCs), play vital functions in the human body. Their main role is the transport of oxygen from the lungs to peripheral tissues and the collection of carbon dioxide from the tissues to be eliminated from the body. However, erythrocytes have several other important functions as well:
- Oxygen transport: Erythrocytes contain a protein called hemoglobin, which binds to oxygen in the lungs and carries it to the body’s tissues. This oxygen is essential for cellular respiration and the production of ATP, the energy currency of cells.
- Carbon dioxide transport: As erythrocytes deliver oxygen to tissues, they also pick up carbon dioxide, a waste product of cellular respiration. Erythrocytes transport carbon dioxide back to the lungs, where it is expelled from the body during exhalation.
- Acid-base balance: Erythrocytes contain an enzyme called carbonic anhydrase, which facilitates the conversion of carbon dioxide and water into carbonic acid. This helps regulate the body’s acid-base balance and maintains proper pH levels in the blood.
- Blood viscosity: Erythrocytes contribute significantly to the viscosity, or thickness, of the blood. Their high concentration gives blood its characteristic consistency, which is crucial for maintaining optimal blood pressure and circulation throughout the body.
- Iron storage: Erythrocytes store a substantial amount of iron in the form of heme molecules. When erythrocytes are destroyed, this iron can be recycled and reused in the body or stored for later use in the production of new erythrocytes or other iron-dependent processes.
- Immune function: While erythrocytes are not primarily involved in the immune response, they can transport antigens on their surface. These antigens can stimulate the production of antibodies, which are critical in fighting against infections and diseases.
- Nutrient transport: In addition to oxygen, erythrocytes are capable of transporting other essential nutrients, such as glucose and amino acids, to cells throughout the body. This ensures that cells have a constant supply of nutrients necessary for their normal functioning.
RBC Summery
- Red blood cells (RBC), also known as erythrocytes, are the functional component of blood that carries oxygen and nutrients across the body. These specialized cells are able to perform their crucial roles because of their distinct structure and makeup.
- Erythrocytes play an important part in the study of disease processes across many organ systems.
- The mature erythrocyte is biconcave, discoid, and anucleated.
- The cell is able to perform its function because of the design’s flexibility and the increased surface area that ensures adequate gas exchange.
- The cytoskeleton is a protein network that supports the phospholipid bilayer membrane that defines this special type of cell. Spectrin, actin, band 3 protein 4.1, and ankyrin make up the cytoskeleton, which gives cells their rigidity and flexibility.
- Structures that are both sturdy and malleable are supported by the interactions between these compounds.
- The average lifespan of a red blood cell is only 120 days. With such a limited amount of time, the circulatory system must transport oxygen from the lungs to the rest of the body’s tissues, where it can be used in metabolic processes like ATP synthesis, and then bring back the waste carbon dioxide to be exhaled.
- When oxygen-starved blood reaches the lungs, it carries hemoglobin containing ferrous heme (Fe), which has a strong attraction to oxygen. As heme reaches deoxygenated tissues, the low pH and low partial pressure of oxygen lead it to lose its affinity for the oxygen and release it into the tissue.
- Carbonic anhydrase then incorporates the CO2 into the cellular environment, where it reacts with H2O to produce bicarbonate and hydrogen. A large portion of the CO2 will be recycled to the lungs as bicarbonate and exhaled.
- Changes in erythrocyte size, shape, and distribution may provide insight into a variety of diseases and pathologies seen in the clinic. For instance, acanthocytes may form during the process of eryptosis, the controlled and gradual degeneration and death of erythrocytes.
- Tabulated cell death is observed in anemia and hypercalcemia. Red blood cell agglutination may suggest a hypercoagulable state, while microcytosis, or abnormally small red blood cells, is linked to microcytic anemias including iron shortage and thalassemia.
- The severity of the disease is also affected by the shape of the red blood cells. The severity of erythrocyte sickling, for instance, is linked to the amount of hereditary hemoglobin S. Blood smears can reveal the presence of these cells, which contribute to many of the disease’s clinical symptoms, such as vaso-occlusive crises and associated pain.
- In addition, erythrocytes’ susceptibility to pro-inflammatory states and physiological alterations has been documented in the scientific literature.
- Non-discoid or atypical erythrocyte morphologies are common in inflammatory disease conditions such systemic lupus erythematosus, but were reversible after inflammatory product chelation was administered.
- The role of inflammation and oxidative stress on erythrocytes in the development of chronic inflammatory illness is further supported by this finding.
- In addition, the analysis of a patient’s red blood cells can shed light on their overall health and the physiological processes taking place in their body.
- Leukemias and other malignancies may involve the presence of nucleated red blood cells, which might be a sign of hemolysis, bleeding, or hypoxia.
White blood cells (WBC) or Leukocytes
- White blood cells (WBCs), also known as leukocytes, are a diverse group of nucleated cells that circulate in the bloodstream. They play a crucial role in various immune-related activities and are vital for defending the body against infections. WBCs can be divided into two main categories: granulocytes and agranulocytes, based on the presence or absence of cytoplasmic granules.
- Granulocytes, as the name suggests, have granules in their cytoplasm. There are three types of granulocytes: neutrophils (or polymorphonuclear granulocytes), eosinophils, and basophils. Neutrophils are the most abundant type and are involved in bacterial phagocytosis. They undergo a complex process of engulfing bacteria, absorbing them into their cytoplasm, and fusing with lysosomes to destroy the bacteria using enzymes.
- Eosinophils and basophils are less numerous. Eosinophils are typically found in the gastrointestinal tract, lungs, and skin. While their specific function is not fully understood, they are thought to contribute to defense against multicellular parasites and help limit inflammation. Basophils contain heparin and histamine in their granules, and they play a role in allergic reactions and immune responses associated with IgE antibodies.
- Agranulocytes include monocytes and lymphocytes. Monocytes are part of the mononuclear leukocytes and have the ability to transform into macrophages when they enter tissues. Macrophages play important roles in phagocytosis, inflammation, antigen analysis, and communication with T lymphocytes. Monocytes can also secrete interleukins and contribute to fibrinolysis.
- Lymphocytes are key players in both cellular and humoral immunity. They account for a significant portion of WBCs in the bloodstream. B lymphocytes (B cells) are responsible for antibody production. When appropriately activated, B cells multiply and differentiate into plasma cells, which produce specific antibodies. T lymphocytes (T cells) govern the cellular immune system and have various subsets with specialized functions. Helper T cells assist B cells, while suppressor T cells inhibit their activity. Some T cells are involved in cell-mediated cytotoxicity, and natural killer (NK) cells have a role in nonspecific cell lysis.
- The proportions of B cells and T cells in the peripheral blood can vary. B cells typically make up around 15-25% of lymphocytes, while T cells range from 40-75%. The B and T cells are morphologically similar but have distinct roles in the immune system.
- In summary, white blood cells or leukocytes are a diverse group of nucleated cells that are essential for immune function. They are categorized into granulocytes (neutrophils, eosinophils, basophils) and agranulocytes (monocytes, lymphocytes). These cells collectively play a crucial role in phagocytosis, immune response, defense against infections, and maintaining overall health and well-being.
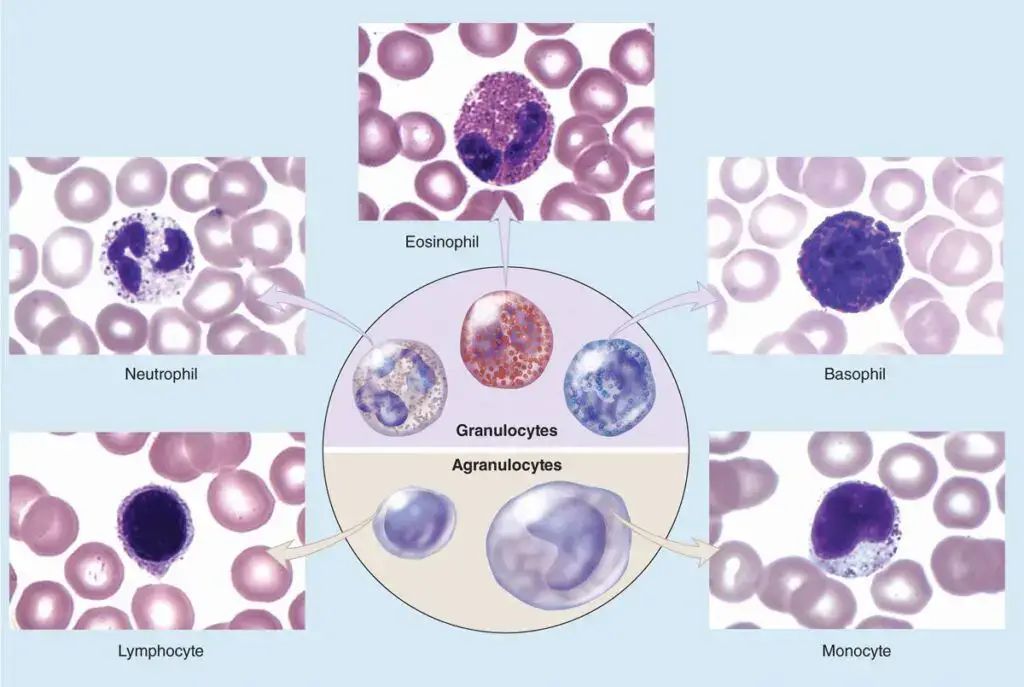
1. Granulocytes
- Granulocytes are a crucial type of white blood cell that plays a significant role in the immune system. These cells are produced in the bone marrow and then released into the bloodstream to fulfill their various functions. The distinguishing feature of granulocytes is the presence of granules in their cytoplasm, which can be visualized when stained and examined under a microscope.
- There are three main types of granulocytes: neutrophils, eosinophils, and basophils. Neutrophils are the most abundant type and serve as the body’s first line of defense against microorganisms. They are highly efficient at phagocytosis, the process of engulfing and digesting foreign particles or organisms. Neutrophils contain enzymes and other chemicals within their granules that help in destroying invaders.
- Eosinophils are involved in the immune system’s defense against parasite infections and are also implicated in the development of allergic reactions. They have specific receptors on their surface that allow them to recognize and target parasites, and they release toxic substances from their granules to eliminate these invaders.
- Basophils are the rarest form of granulocyte, and their main role is in allergic reactions. When exposed to allergens, basophils release histamine from their granules, which contributes to the inflammatory response and leads to symptoms such as itching, swelling, and redness.
- Granulocytes, in general, are equipped with specialized granules that contain enzymes, antimicrobial peptides, and other chemicals that are harmful to invading microorganisms. These granules enable granulocytes to effectively combat infections and contribute to the body’s immune response.
- The count of granulocytes in the blood can provide valuable information about a person’s health. An increase or decrease in granulocyte count may indicate an infection or an autoimmune condition, respectively. Monitoring the granulocyte count is an important diagnostic tool for healthcare professionals.
- In response to injury or infection, granulocytes can migrate to the affected site as part of the inflammatory response. They release additional substances that help recruit other immune cells to the area and contribute to the elimination of pathogens.
- In conclusion, granulocytes are a diverse group of white blood cells with granules in their cytoplasm. Neutrophils, eosinophils, and basophils are the three main types of granulocytes, each with its own unique functions in the immune system. These cells play a crucial role in defending the body against infections, participating in phagocytosis, and contributing to the inflammatory response.
a. Eosinophils
- Eosinophils are a specific type of granulocyte or white blood cell that plays a significant role in the body’s immune system. They are characterized by the presence of large granules in their cytoplasm that can be stained with eosin, a red dye commonly used in laboratory settings.
- These cells are produced in the bone marrow and then circulate throughout the body via the bloodstream. Eosinophils make up a small percentage, typically between 1% and 6%, of the total leukocytes in a person’s blood.
- Eosinophils have distinct features that differentiate them from other leukocytes. They possess a bilobed nucleus and contain abundant large, acidophilic specific granules that stain pink or red. The granules are structurally characterized by oval shapes with flattened crystalloid cores that contain major basic proteins.
- One of the primary functions of eosinophils is their involvement in the immune response to both parasitic infections and allergic reactions. These cells are particularly abundant in the connective tissue of the intestinal lining and can be found in increased numbers at sites of chronic inflammation, such as the lung tissues of individuals with asthma.
- In the context of allergic responses, eosinophils play a crucial role in modulating inflammatory responses. They release chemokines, cytokines, and lipid mediators that contribute to the allergic inflammatory cascade. Eosinophils are known to be involved in the pathogenesis of various allergic conditions, such as asthma, allergic rhinitis, and eosinophilic esophagitis.
- While eosinophils primarily reside in the blood, they can also migrate to other tissues depending on the specific situation. They can remain in the bloodstream for several hours to a few days before moving on to sites of inflammation or infection where they exert their immune functions.
- In summary, eosinophils are a distinct type of granulocyte characterized by their large eosinophilic granules. They play a crucial role in the immune system, being involved in both the defense against parasitic infections and the inflammatory response to allergies. Their ability to release various mediators contributes to the modulation of inflammation and allergic reactions in the body.
Structure
Eosinophils have a distinct cellular structure that sets them apart from other types of white blood cells. Their structure is closely related to their specific functions in the immune response. Here are some key features of the structure of eosinophils:
- Nucleus: Eosinophils possess a bilobed nucleus, which means that their nucleus is divided into two lobes connected by a thin strand of chromatin. The bilobed nucleus gives eosinophils a characteristic appearance under the microscope.
- Cytoplasm: The cytoplasm of eosinophils is filled with numerous large granules. These granules are one of the defining features of eosinophils and are responsible for their name, as they can be stained with eosin, a red dye commonly used in laboratory settings. The granules give the cytoplasm a distinct appearance.
- Granules: The granules present in eosinophils are essential for their function in the immune response. These granules contain various substances that can combat invading infections. Among the components stored in the granules are enzymes, proteins, and toxic chemicals that can be released to kill parasites and pathogens.
- Major basic protein (MBP): One of the prominent components found in eosinophil granules is the major basic protein. MBP is an enzyme that has potent toxic effects on parasites. When released, it can damage the surface of parasites and disrupt their vital functions, ultimately leading to their destruction.
- Eosinophil peroxidase (EPO): Another enzyme found in eosinophil granules is eosinophil peroxidase. This enzyme is involved in generating reactive oxygen species, which have antimicrobial properties. EPO helps in the defense against invading infections by enhancing the ability of eosinophils to kill pathogens.
The unique structure of eosinophils, including the bilobed nucleus and the presence of large granules filled with enzymes and toxic chemicals, enables them to effectively combat parasites and participate in the immune response against various infections. Understanding the structure of eosinophils provides insights into their specialized functions and their role in maintaining the body’s defense mechanisms.
Functions
Eosinophils play important roles in various physiological processes and immune responses in the body. Here are some key functions of eosinophils:
- Defense against parasitic infections: Eosinophils are crucial in combating parasitic infections. When eosinophils encounter parasites, they release toxic granules containing enzymes and proteins such as major basic protein (MBP) and eosinophil peroxidase (EPO). These substances can directly damage and kill parasites, providing a defense mechanism against these invaders.
- Modulation of allergic reactions: Eosinophils contribute to the complex immune response involved in allergic reactions. They interact with other immune cells, such as mast cells, to regulate the inflammatory process. Eosinophils release substances that can influence mast cell activity and the release of inflammatory mediators like histamine. This involvement in allergic reactions can lead to symptoms such as itching, swelling, and inflammation.
- Tissue regeneration and wound healing: Eosinophils also play a role in tissue repair and wound healing. They secrete growth factors and cytokines that promote tissue regeneration and stimulate the healing process. By aiding in the resolution of inflammation, eosinophils contribute to the restoration of normal tissue function and structure.
- Diagnostic marker for certain conditions: Abnormally high levels of eosinophils in the blood, a condition called eosinophilia, can be an indicator of various disorders. Allergies, asthma, and certain parasitic infections can trigger an increase in eosinophil count. Additionally, elevated eosinophil levels have been associated with certain malignancies, such as Hodgkin’s lymphoma and certain types of leukemia. Monitoring eosinophil levels can help in the diagnosis and management of these conditions.
Eosinophils, with their unique functions and interactions within the immune system, contribute to host defense, allergic reactions, tissue repair, and act as diagnostic markers for specific disorders. Understanding their functions helps shed light on their role in maintaining immune homeostasis and their involvement in various pathological conditions.
b. Basophils
Basophils are a type of granulocyte or white blood cell that play important roles in the body’s immune response. Here are some key characteristics and functions of basophils:
- Morphology: Basophils have a distinct appearance. Their nucleus is divided into two irregular lobes, and their cytoplasm contains large granules (approximately 0.5 μm in diameter) that can be stained purple with basic dyes. These granules are larger, fewer in number, and more irregularly shaped compared to granules in other granulocytes.
- Low abundance: Basophils make up less than 1% of circulating leukocytes in the blood, which makes them relatively rare. They are often challenging to identify in routine blood smears due to their low frequency.
- Granule contents: The basophilic granules contain various substances that are involved in immune and inflammatory responses. They are rich in histamine, heparin, and other sulfated glycosaminoglycans (GAGs). Basophilic granules also contain mediators of inflammation such as platelet-activating factor, eosinophil chemotactic factor, and the enzyme phospholipase A.
- Immunoglobulin E (IgE) receptors: Basophils have surface receptors for immunoglobulin E (IgE), an antibody involved in allergic reactions. When IgE binds to these receptors, it can trigger the activation of basophils.
- Allergic reactions: Basophils contribute to the immune response during allergic reactions. When exposed to certain antigens and allergens, basophils migrate into connective tissues and release their granular contents, including histamine and other inflammatory mediators. This release of mediators can contribute to the symptoms of allergies, such as itching, swelling, and inflammation.
- Interaction with mast cells: Basophils have similar functions to mast cells, another type of immune cell involved in allergic reactions. They both release histamine and other inflammatory substances and play complementary roles in immune responses.
Although basophils are relatively rare and their exact functions are still being studied, their involvement in allergic reactions and immune responses highlights their importance in the body’s defense mechanisms. Further research is necessary to fully understand the precise role of basophils in health and disease.
Structure of Basophils
The structure of basophils, a type of white blood cell, is characterized by specific features that contribute to their function in the immune system. Here are some key points about the structure of basophils:
- Lobate nucleus: The nucleus of a basophil is lobate, meaning it is divided into multiple irregular lobes. This lobed structure gives basophils a distinct appearance under a microscope.
- Cytoplasmic granules: Basophils have abundant granules in their cytoplasm. These granules are filled with basophilic material, which refers to substances that can be stained with basic dyes. The granules are voluminous and contribute to the characteristic appearance of basophils.
- Storage of inflammatory mediators: The granules present in basophils serve as storage units for various inflammatory mediators. Histamine, heparin, and other substances involved in immune responses are stored within these granules. When basophils are activated, these granules can release the stored mediators to combat invading pathogens or respond to allergic reactions.
- Cytokines and chemokines: Basophils also contain cytokines and chemokines, which are signaling molecules that play a crucial role in immune responses. These molecules can activate and recruit other types of immune cells, amplifying the immune response. By releasing cytokines and chemokines, basophils can help coordinate and regulate the actions of other immune cells during an immune reaction.
The structure of basophils, with their lobate nucleus and voluminous granules, allows them to store and release important substances involved in immune responses. The presence of histamine, heparin, and other inflammatory mediators in their granules enables basophils to participate in the defense against invaders and contribute to immune reactions. Additionally, the cytokines and chemokines present in basophils allow them to communicate with and activate other immune cells, promoting a coordinated immune response.
Functions of Basophils
Basophils, as a type of white blood cell, perform various functions that contribute to the body’s immune response. Here are some key points about the functions of basophils:
- Allergic reactions: Basophils play a critical role in allergic reactions. When an allergen enters the body, basophils release histamine and other inflammatory mediators from their granules. Histamine causes blood vessels to dilate, leading to increased blood flow and permeability. This results in the characteristic symptoms of allergic reactions, such as itching, swelling, and redness.
- Defense against parasites: Basophils are involved in the body’s immune response to parasite infections. They release granules containing toxic substances that can help eliminate parasites. These poisonous substances contribute to the destruction of parasites and aid in the body’s defense mechanism against these invaders.
- Recruitment of immune cells: Basophils have the ability to release cytokines and chemokines, which are signaling molecules that can attract and recruit other immune cells to the site of infection or injury. By releasing these molecules, basophils help amplify and coordinate the immune response, ensuring the involvement of appropriate immune cells to combat the threat.
- Indicators of medical conditions: Abnormally high or low basophil numbers can serve as indicators of certain medical conditions. Elevated basophil levels may be seen in allergies, parasite infections, and some types of leukemia. On the other hand, decreased basophil counts may be observed in certain autoimmune diseases, such as rheumatoid arthritis and systemic lupus erythematosus.
Basophils, through their release of histamine and other inflammatory mediators, contribute to the development of allergic reactions and their associated symptoms. Their involvement in eliminating parasites by releasing toxic substances highlights their role in the immune defense against these invaders. Additionally, the ability of basophils to release cytokines and chemokines aids in recruiting and activating other immune cells, ensuring an effective immune response. Monitoring basophil levels can provide valuable insights into various medical conditions, including allergies, infections, and autoimmune diseases.
c. Neutrophils
Neutrophils are the most abundant type of granulocyte or white blood cell in the human body. They possess small, neutral-staining granules in their cytoplasm. Here are some key points about neutrophils:
- Scavenging and clearance: Neutrophils are rapid and efficient scavenger cells that play a crucial role in clearing damaged areas of the body. They swiftly remove dead cells and debris left behind by invading microorganisms, ensuring the cleanup and restoration of tissues.
- Complex nucleus and lysosomal granules: Neutrophils have a characteristic nucleus that is complex and consists of up to six lobes connected by thin nuclear extensions. Their cytoplasm contains granules that are lysosomes filled with enzymes responsible for breaking down ingested material.
- Short lifespan and rapid multiplication: Neutrophils have a relatively short lifespan in the bloodstream, typically around 6-9 hours. However, once they reach a region of damaged or infected tissue, they rapidly multiply. Mature neutrophils constitute a significant portion, ranging from 50% to 70%, of all circulating leukocytes.
- Chemotaxis and diapedesis: Chemicals called chemotaxins, released by injured cells, act as signals to attract neutrophils in large numbers to the site of infection. Neutrophils possess high mobility and are capable of diapedesis, which allows them to squeeze through the capillary walls to reach the affected area.
- Role in immune response: Neutrophils are the first responders in the immune system’s defense against infection. Through a process called chemotaxis, they actively seek out invading bacteria cells. Once they reach the target, neutrophils employ phagocytosis to engulf and digest the invaders or their waste products, eliminating the threat.
Neutrophils are characterized by their small size, rapid response, and efficient scavenging abilities. Their complex nucleus and lysosomal granules aid in their cellular functions. With a short lifespan in the bloodstream, they quickly multiply upon reaching the site of infection or tissue damage. Chemotaxis guides them to the source of injury, and their high motility enables them to squeeze through capillaries. Neutrophils serve as the frontline defense by actively pursuing and eliminating bacterial cells through phagocytosis. Their pivotal role in immune responses makes them essential components of the body’s defense against infection and tissue repair.
Structure of Neutrophils
The structure of neutrophils is characterized by several key features that contribute to their functionality as white blood cells. Here are some aspects of the structure of neutrophils:
- Nucleus and cytoplasm: Neutrophils possess a distinct nucleus with multiple lobes, typically two to five, connected by thin nuclear extensions. This multilobed nucleus gives neutrophils their distinctive appearance. The cytoplasm of neutrophils contains various cellular components essential for their functions.
- Granules: Neutrophils have numerous small granules dispersed throughout their cytoplasm. These granules stain similarly to neutral proteins, giving neutrophils their name. The granules contain various substances, including antimicrobial components such as enzymes and other molecules involved in the immune response.
- Lysosomes: One important type of granule found in neutrophils is the lysosome. Lysosomes are specialized organelles responsible for intracellular digestion. In neutrophils, lysosomes contain enzymes and other substances that play a vital role in the breakdown and digestion of bacteria, cellular debris, and other foreign particles.
- Antimicrobial ingredients: The granules in neutrophils contain antimicrobial ingredients, including enzymes, peptides, and proteins. These components help neutrophils combat invading microorganisms by breaking down bacterial cell walls, disrupting microbial metabolism, and promoting the destruction of pathogens.
The structure of neutrophils, with their multilobed nucleus and numerous granules, supports their functions as key players in the immune response. The granules, including lysosomes, house antimicrobial ingredients that enable neutrophils to effectively combat infections and digest cellular waste. By utilizing their specialized structure and components, neutrophils contribute to the body’s defense mechanisms against pathogens and participate in the resolution of inflammatory processes.
Functions of Neutrophils
Neutrophils play crucial roles in the immune response and have diverse functions that contribute to the body’s defense mechanisms. Here are some key functions of neutrophils:
- Phagocytosis: Neutrophils are highly effective at engulfing and destroying invading pathogens, particularly bacteria. They recognize and adhere to microorganisms through cell surface receptors, and then proceed to engulf them in a process called phagocytosis. Once inside the neutrophil, the pathogens are exposed to antimicrobial substances and enzymes contained within the cell’s granules, leading to their destruction.
- Tissue repair and inflammation resolution: Neutrophils also contribute to the resolution of inflammation and the mending of damaged tissues. After neutrophils have eliminated pathogens, they release factors that help regulate and reduce inflammation. They promote tissue repair and remodeling by releasing growth factors and other molecules that stimulate cell proliferation and tissue regeneration.
- Production of reactive oxygen species: Neutrophils have the ability to generate reactive oxygen species (ROS) as part of their antimicrobial arsenal. These ROS, such as superoxide radicals and hydrogen peroxide, have potent bactericidal properties and can help neutralize and eliminate pathogens.
- Secretion of cytokines and chemokines: Neutrophils are capable of secreting various cytokines and chemokines, which are signaling molecules that regulate the immune response. These molecules attract and recruit other immune cells to the site of infection or injury, facilitating a coordinated and robust immune response.
- Disease indicators: Abnormal neutrophil numbers can serve as indicators of certain conditions. Increased neutrophil counts, known as neutrophilia, may be observed in bacterial infections, inflammatory disorders, and some forms of leukemia. On the other hand, decreased neutrophil counts, known as neutropenia, can make individuals more susceptible to infections.
- Involvement in inflammatory disorders: Neutrophils are implicated in non-infectious inflammatory disorders, such as rheumatoid arthritis and systemic lupus erythematosus. In these conditions, neutrophils contribute to the inflammatory processes and tissue damage associated with the diseases.
In summary, neutrophils are essential components of the immune response, contributing to the elimination of pathogens, tissue repair, resolution of inflammation, and recruitment of other immune cells. Their functions play vital roles in defending against infections and maintaining tissue homeostasis.
2. Agranulocytes
- Agranulocytes are a group of white blood cells characterized by the absence of specific granules in their cytoplasm. Unlike granulocytes, which have visible granules that can be stained and visualized under a microscope, agranulocytes lack these granules. However, they do contain azurophilic granules, also known as lysosomes, which are involved in various cellular processes.
- The nucleus of agranulocytes is typically spherical or indented, lacking the lobulated appearance seen in granulocytes. This structural difference sets agranulocytes apart from their granulated counterparts.
- Leukocytes, including both granulocytes and agranulocytes, play a vital role in the body’s defense against invading microorganisms. They are essential components of the immune system and contribute to the recognition and elimination of pathogens. Additionally, leukocytes are involved in the repair of injured tissues and the maintenance of overall tissue homeostasis.
- Agranulocytes consist of two main types: lymphocytes and monocytes. Lymphocytes are key players in the adaptive immune response. They are responsible for recognizing specific antigens and orchestrating immune responses against them. Lymphocytes can differentiate into various subtypes, such as B cells, T cells, and natural killer (NK) cells, each with specialized functions in immune defense.
- Monocytes, on the other hand, are involved in both innate and adaptive immune responses. They are responsible for phagocytosis, the process of engulfing and digesting foreign particles, microorganisms, and cellular debris. Monocytes can differentiate into macrophages or dendritic cells, which play crucial roles in antigen presentation and immune regulation.
- Both lymphocytes and monocytes are integral to the body’s defense against antigens and pathogenic microorganisms. They contribute to immune surveillance, immune memory, and the coordination of immune responses to ensure efficient protection against infections and diseases.
- In summary, agranulocytes are a group of white blood cells characterized by the absence of specific granules in their cytoplasm. They include lymphocytes and monocytes, which are essential components of the immune system involved in the recognition and elimination of antigens and pathogens. These cells play critical roles in immune defense, immune regulation, and tissue repair.
a. Lymphocytes
- Lymphocytes are a type of white blood cell characterized by their round shape and large, round nucleus. There are two main classes of lymphocytic cells: B cells and T cells, each with distinct roles in the immune system.
- B cells mature in the bone marrow, while T cells mature in the thymus gland. Lymphocytes are generally the smallest leukocytes and make up approximately one-third of all white blood cells. They exhibit a wider range of sizes compared to most leukocytes. Newly released lymphocytes are similar in diameter to red blood cells, while matured lymphocytes range from 9 to 18 μm in diameter.
- While some lymphocytes circulate in the blood, the majority of these cells are found in tissues, particularly in lymphatic tissues like lymph nodes and the spleen. Lymphocytes are derived from pluripotent stem cells in the red bone marrow and precursor cells in lymphoid tissue.
- Lymphocytes play a crucial role in various immune reactions. When activated, B cells, also known as plasma cells, produce highly specific antibodies that bind to the specific agent (e.g., pathogens, toxins) that triggered the immune response. These antibodies aid in the identification and neutralization of foreign substances.
- T cells, particularly helper T cells, play a different role in the immune response. They secrete chemicals called cytokines that recruit other immune cells and help coordinate their attack against pathogens. Helper T cells play a central role in activating other immune cells, such as cytotoxic T cells and B cells, and enhancing the immune response.
- Lymphocytes are essential for adaptive immunity, the branch of the immune system that provides long-lasting protection against specific pathogens. Through their ability to recognize and respond to specific antigens, lymphocytes contribute to immune surveillance, immune memory, and the regulation of immune responses.
- In summary, lymphocytes are round cells with a single, large nucleus. They are divided into B cells and T cells, each maturing in different locations. Lymphocytes are involved in various immune reactions and are crucial for the body’s defense against pathogens. B cells produce antibodies, while T cells secrete cytokines and coordinate immune responses. These cells play a vital role in adaptive immunity and contribute to immune surveillance and memory.
Structure of Lymphocytes
- Lymphocytes are characterized by their small, round shape and unique cellular structure. These cells have a large, round nucleus and relatively little cytoplasm compared to other types of cells.
- There are three primary types of lymphocytes: B cells, T cells, and natural killer (NK) cells. Each of these lymphocyte types plays a distinct role in the immune system.
- B cells are responsible for the production of antibodies, which are specialized proteins that can recognize and bind to specific antigens, such as pathogens or foreign substances. B cells possess receptor molecules on their surface called B cell receptors (BCRs). These BCRs allow B cells to recognize and respond to specific antigens, initiating an immune response.
- T cells, on the other hand, are involved in cell-mediated immunity. They are responsible for directly attacking infected or abnormal cells, as well as regulating immune responses. T cells express T cell receptors (TCRs) on their surface, which enable them to recognize specific antigens displayed by infected cells or antigen-presenting cells.
- Natural killer (NK) cells are a type of lymphocyte that participates in the innate immune response. NK cells are known for their ability to recognize and kill virus-infected cells and tumor cells without prior sensitization. They play a critical role in the early defense against pathogens and abnormal cells.
- The receptors present on the surface of lymphocytes, including B cell receptors, T cell receptors, and other receptors specific to NK cells, allow these cells to recognize and respond to specific antigens. These receptors are generated through a complex process of genetic recombination, resulting in a diverse repertoire of receptors that can recognize a wide range of antigens.
- The specific structure and surface receptors of lymphocytes enable them to participate in the adaptive immune response, providing a targeted defense against specific pathogens or abnormal cells. Through their ability to recognize and respond to specific antigens, lymphocytes play a fundamental role in the immune system’s ability to distinguish between self and non-self and mount appropriate immune responses.
Functions of Lymphocytes
- Lymphocytes serve vital functions in the immune system, playing a crucial role in defending the body against infections and diseases. Each type of lymphocyte has its specific functions and contributions to immune responses.
- B cells are primarily responsible for the production of antibodies, also known as immunoglobulins. Antibodies are proteins that recognize and bind to specific foreign substances, such as bacteria, viruses, or toxins. This process, known as humoral immunity, helps to neutralize and eliminate pathogens by marking them for destruction or preventing their entry into cells. B cells undergo a process called antibody-mediated or humoral response, generating a diverse repertoire of antibodies that can specifically recognize and target a wide range of antigens.
- T cells have various functions within the immune system. Helper T cells (CD4+ T cells) play a central role in coordinating immune responses. They help activate other immune cells, including B cells and cytotoxic T cells, by releasing chemical signals called cytokines. These cytokines enhance the immune response and direct immune cells to the site of infection or inflammation. Cytotoxic T cells (CD8+ T cells) are responsible for directly killing infected or abnormal cells, such as those infected with viruses or cancer cells. They recognize specific antigens displayed on the surface of infected cells and induce their destruction.
- Natural Killer (NK) cells are part of the innate immune system and have the ability to recognize and kill abnormal cells, including virus-infected cells and cancer cells. NK cells use a combination of receptors to identify cells that lack the expression of self-molecules or exhibit stress-related markers. Once identified, NK cells release cytotoxic molecules to destroy these abnormal cells, a process known as natural cytotoxicity.
- Together, lymphocytes orchestrate a dynamic and coordinated immune response. They recognize and eliminate foreign invaders, coordinate the activities of other immune cells, and regulate immune responses to maintain a balanced and effective defense system. Lymphocytes are essential for the body’s ability to mount specific immune responses against pathogens, prevent reinfection, and provide immune memory for long-term protection.
b. Monocytes
- Monocytes are a type of agranulocyte, which means they lack specific granules in their cytoplasm. They are the largest of all white blood cells and serve as precursors to various cell types in the mononuclear phagocyte system, including macrophages, osteoclasts, and microglia, which are involved in immune responses and tissue maintenance.
- Circulating monocytes typically have diameters ranging from 12 to 15 μm, although macrophages can be even larger. The nucleus of a monocyte is large and often exhibits distinct indentations or a C-shaped appearance. The chromatin within the nucleus is dense. In the cytoplasm, monocytes have basophilic staining properties, and they contain numerous small lysosomal azurophilic granules. Additionally, they possess mitochondria, areas of rough endoplasmic reticulum (ER), and a Golgi apparatus involved in the formation of lysosomes.
- Monocytes play a crucial role in the immune response, particularly in inflammation. They are capable of producing various cytokines and signaling molecules, including interleukin 1 (IL-1). IL-1 functions as a pro-inflammatory cytokine that promotes the activation of B cells and enhances phagocytosis, the process by which cells engulf and eliminate pathogens or cellular debris.
- As monocytes migrate into tissues, they differentiate into macrophages, which are specialized phagocytic cells responsible for engulfing and destroying pathogens, debris, and foreign substances. Macrophages also play a role in tissue repair and remodeling. In addition to their role in inflammation and phagocytosis, monocytes/macrophages are involved in antigen presentation, immune regulation, and the initiation of immune responses.
- Overall, monocytes are important components of the immune system, serving as precursors to diverse cell types and participating in various immune functions. They contribute to the body’s defense against infections, the clearance of cellular debris, and the regulation of immune responses through the production of cytokines and the activities of their differentiated forms, such as macrophages.
Structure of Monocytes
- Monocytes are a type of white blood cell with a distinct structure. They have the ability to differentiate into various immune cells and are characterized by their large, kidney-shaped nucleus.
- The diameter of circulating monocytes typically ranges from 12 to 15 μm, although macrophages derived from monocytes can be larger in size. The nucleus of a monocyte is massive and often exhibits a recessed or C-shaped appearance. It is surrounded by thick chromatin, which gives it a dense and compact structure.
- In terms of cytoplasmic features, monocytes have a basophilic cytoplasm, meaning it stains blue-purple with basic dyes. The cytoplasm contains numerous tiny azurophilic granules, which are believed to be lysosomes. These granules are involved in intracellular digestion and the breakdown of cellular debris.
- Compared to other types of white blood cells, monocytes tend to be larger in size. They have a lower nucleus-to-cytoplasm ratio, indicating that their cytoplasm occupies a larger volume. This feature allows monocytes to carry out their diverse functions effectively.
- Observing the Golgi apparatus, an organelle involved in protein synthesis and modification, is also possible in monocytes. The Golgi apparatus is visible within the cytoplasm and plays a crucial role in the production and processing of proteins.
- Monocytes have a wide array of receptors on their cell surface, allowing them to communicate with and respond to various signals from other immune cells. Among these receptors are Toll-like receptors (TLRs), which play a vital role in recognizing pathogen-associated molecular patterns (PAMPs). When TLRs detect PAMPs, they initiate an immune response to combat potential pathogens.
- In summary, the structure of monocytes is characterized by their large, kidney-shaped nucleus, basophilic cytoplasm with tiny azurophilic granules, and the presence of receptors such as Toll-like receptors. These structural features enable monocytes to differentiate into different immune cells and participate in the immune response by detecting and responding to signals from pathogens.
Functions of Monocytes
Monocytes play crucial roles in the immune system with their diverse functions:
- Phagocytosis: Monocytes possess the ability to engulf and digest foreign particles, including bacteria, viruses, and other microorganisms. Through phagocytosis, monocytes contribute to the defense against infections by eliminating pathogens and preventing their spread.
- Antigen presentation: Monocytes can act as antigen-presenting cells (APCs). They capture foreign antigens, break them down into smaller fragments, and present these fragments on their cell surface. By presenting antigens, monocytes help to activate other immune cells, particularly T cells, initiating a targeted immune response against the specific pathogen.
- Differentiation: Monocytes have the remarkable capacity to differentiate into different types of immune cells based on the signals they receive. One common differentiation pathway is their transformation into macrophages, which are highly specialized cells involved in phagocytosis, tissue repair, and immune regulation. Monocytes can also differentiate into dendritic cells, which are essential for antigen presentation and immune activation.
- Cytokine production: Monocytes are capable of producing various cytokines, which are small signaling molecules that regulate immune responses. These cytokines include interleukins, tumor necrosis factor (TNF), and interferons. By secreting cytokines, monocytes can modulate the activity of other immune cells, promoting inflammation, orchestrating immune reactions, and contributing to the coordination and regulation of the overall immune response.
Through their phagocytic activity, antigen presentation, differentiation into specialized immune cells, and cytokine production, monocytes play vital roles in immune defense, immune regulation, and coordination of immune responses against infections. Their multifunctional nature makes them essential components of the immune system and critical players in maintaining overall immune homeostasis.
Platelets or Thrombocytes
Platelets, also known as thrombocytes, are small, non-nucleated cells derived from the cytoplasm of megakaryocytes in the red bone marrow. They play a crucial role in blood clotting and hemostasis. Here are some key points about platelets:
- Size and Composition: Platelets are very small cells, typically measuring 2-4 μm in diameter. Unlike most cells in the body, platelets lack a nucleus. However, their cytoplasm is densely packed with granules containing various substances involved in blood clotting and wound healing.
- Blood Platelet Count: The normal blood platelet count in humans ranges from 200 × 10^9/L to 350 × 10^9/L (200,000–350,000/mm^3). Adequate platelet count is essential for proper clotting and prevention of excessive bleeding.
- Platelet Production: The exact mechanism of platelet regulation is not fully understood. However, the liver produces a hormone called thrombopoietin, which stimulates the production of platelets from megakaryocytes in the bone marrow. Thrombopoietin plays a vital role in maintaining appropriate platelet levels in the bloodstream.
- Lifespan and Clearance: Platelets have a relatively short lifespan, typically lasting between 8 and 11 days. After this period, if not utilized in clotting, platelets are removed from circulation. Macrophages, primarily located in the spleen, phagocytize and break down aging platelets.
Platelets are integral to the process of blood clotting, which is crucial for preventing excessive bleeding. When blood vessels are damaged, platelets adhere to the site of injury, aggregate together, and form a platelet plug. Additionally, platelets release various substances, such as clotting factors and growth factors, which initiate and promote the clotting cascade.
While platelets are vital for hemostasis, abnormalities in platelet count or function can lead to bleeding disorders or thrombotic conditions. Too few platelets (thrombocytopenia) can result in increased bleeding tendencies, while excessive platelet activity (thrombocythemia) can lead to the formation of unwanted blood clots.
Overall, platelets serve as essential components of the blood coagulation system, playing a critical role in maintaining hemostasis and preventing excessive bleeding.
Structure of Platelets or Thrombocytes
Platelets, also known as thrombocytes, are small, irregularly-shaped cells that play a crucial role in blood clotting. Here are some key points about the structure of platelets:
- Shape: Platelets have a discoid shape, although they are actually more irregularly oblate in structure. Their typical diameter is only 2–4 micrometers, making them significantly smaller than both red and white blood cells.
- Granules: Platelets contain numerous granules within their cytoplasm. These granules store a variety of proteins and chemicals that are essential for blood clotting. When platelets are activated during an injury, the contents of these granules are released to initiate the clotting process.
- Platelet Membrane: The platelet membrane is the outer layer of the cell and is composed of lipids and proteins. It contains specific glycoproteins that enable platelets to adhere to injured blood vessel walls and to other platelets. This adhesion is crucial for the formation of the initial platelet plug during clot formation.
- Cytoplasm: The cytoplasm of platelets contains a network of microtubules and microfilaments. These structures help maintain the shape of the platelet and allow it to transform into a clotting spheroid when necessary. The cytoplasm also contains other organelles, such as mitochondria, which generate energy for the platelet to carry out its functions.
- Mitochondria: Platelets possess a small number of mitochondria. These organelles are responsible for producing energy in the form of adenosine triphosphate (ATP), which fuels the platelet’s activities.
The unique structure of platelets enables them to respond rapidly to injury and initiate the process of blood clotting. Their discoid shape, granules, membrane glycoproteins, and cytoplasmic components all contribute to their ability to form a clot and stop bleeding at the site of vascular damage.
It’s important to note that platelets are not complete cells in the traditional sense, as they lack a nucleus and other cellular organelles. However, their specialized structure allows them to carry out their vital role in maintaining hemostasis and preventing excessive bleeding.
Functions of Platelets or Thrombocytes
Platelets, or thrombocytes, have several important functions in the body. Here are key points regarding the functions of platelets:
- Blood clotting: One of the primary functions of platelets is their role in blood clotting or coagulation. When a blood vessel is damaged, platelets are activated and adhere to the site of injury. They form a temporary plug to prevent further bleeding. Platelets release clotting factors and other substances that promote the formation of a stable blood clot. This process is essential for maintaining hemostasis and preventing excessive blood loss.
- Wound healing: Platelets contribute to the wound healing process. When platelets adhere to the site of injury, they release growth factors that stimulate the proliferation of cells involved in tissue repair. These growth factors promote the formation of new blood vessels (angiogenesis) and support the growth and regeneration of damaged tissues. Platelets play a crucial role in the early stages of wound healing.
- Immune response: Platelets are involved in the body’s immune response. They can interact with white blood cells, such as neutrophils and macrophages, to enhance their immune functions. Platelets can help to recognize and destroy bacteria and other pathogens, aiding in the defense against infections. They also contribute to the activation and regulation of the immune system during an immune response.
- Inflammation: Platelets release various chemicals, including cytokines and chemokines, that can contribute to inflammation. Inflammation is a normal response to injury or infection and plays a role in initiating the healing process. Platelets can amplify and regulate the inflammatory response, recruiting immune cells and promoting the release of additional inflammatory mediators. However, excessive inflammation can lead to chronic inflammation and contribute to certain health conditions.
Overall, platelets play a crucial role in maintaining hemostasis, supporting wound healing, participating in the immune response, and regulating inflammation. Their functions are essential for ensuring proper clot formation, tissue repair, and protection against infections.
Blood Coagulation
- Blood coagulation, also known as clotting, is a vital process that ensures the maintenance of vascular integrity and prevents excessive bleeding. When a blood vessel is damaged, coagulation is triggered to form a blood clot, leading to hemostasis and subsequent repair of the injured vessel.
- The process of coagulation involves a complex series of events that occur almost instantaneously upon injury to the endothelium, the lining of blood vessels. Two key processes are initiated: changes in platelets and the exposure of subendothelial tissue factor to plasma factor VII. These processes ultimately lead to the formation of a cross-linked fibrin clot.
- Primary hemostasis is the initial response to vessel injury, where platelets rapidly adhere to the exposed subendothelial matrix, forming a plug at the site of injury. This plug helps to prevent further blood loss temporarily. At the same time, secondary hemostasis takes place. It involves a cascade of coagulation factors beyond factor VII, which work together to form fibrin strands that strengthen the platelet plug.
- Coagulation disorders can occur when there is an imbalance or dysfunction in the coagulation process. These disorders can manifest as excessive bleeding, easy bruising, or abnormal blood clotting, leading to thrombosis. Hemophilia and von Willebrand disease are examples of inherited coagulation disorders, while liver disease, vitamin K deficiency, and certain medications can cause acquired coagulation disorders.
- Coagulation is a highly conserved biological process found across different species. It involves both cellular components, such as platelets, and proteinaceous components, known as coagulation factors. Although coagulation is present in all mammals, the human coagulation pathway has been extensively studied and is the best understood.
- Understanding the intricacies of blood coagulation has significant clinical implications. It has led to the development of anticoagulant medications to prevent excessive clotting in conditions like deep vein thrombosis, pulmonary embolism, and atrial fibrillation. Conversely, hemostatic agents and clotting factors are used to manage bleeding disorders and promote clot formation in specific medical procedures.
- In summary, blood coagulation is a complex and tightly regulated process that plays a crucial role in maintaining vascular integrity. Through the activation, adhesion, and aggregation of platelets, as well as the deposition and maturation of fibrin, coagulation ensures the formation of a stable blood clot to prevent excessive bleeding. Understanding the mechanisms of coagulation helps in diagnosing and managing various coagulation disorders, ultimately improving patient care and outcomes.
Process of blood coagulation
The process of blood coagulation, also known as hemostasis, involves a series of steps that work together to stop bleeding and form a clot. These steps can be divided into three major phases:
- Primary Hemostasis: The first step in hemostasis is vasoconstriction, which occurs in response to injury to the blood vessel walls. Vasoconstriction helps reduce blood flow to the affected area, slowing down the bleeding. Concurrently, platelets, tiny cell fragments in the blood, play a crucial role in primary hemostasis. They adhere to the injured site and form a platelet plug to temporarily seal the damaged vessel.
- Secondary Hemostasis: Platelets not only contribute to primary hemostasis but also initiate the secondary hemostasis process. Activated platelets release stored granular contents, including serotonin, ADP, and thromboxane. These substances further activate platelets and promote the formation of a fibrin clot. Fibrin is a fibrous protein that forms a mesh-like structure, stabilizing the platelet plug and reinforcing the clot formation.
- Coagulation Cascade: The formation of a stable blood clot requires the activation of multiple clotting factors in a sequence known as the coagulation cascade. These clotting factors interact with one another, leading to a chain reaction that ultimately results in the conversion of soluble plasma protein called fibrinogen into insoluble fibrin proteins. Fibrin strands then intertwine and stick together to form a meshwork, further reinforcing the clot. If red blood cells are also present in the clot, it is known as a red thrombus, while a clot composed mainly of platelets is termed a white thrombus.
The coagulation cascade is a highly regulated process, involving a series of enzymatic reactions and activation steps. The cascade can be initiated through two main pathways: the intrinsic pathway, which is triggered by factors within the blood, and the extrinsic pathway, which is initiated by the release of tissue factor from damaged tissues. These pathways eventually converge and lead to the activation of a common pathway, resulting in the formation of fibrin.
Functions of Blood cells
Blood cells, including red blood cells (RBCs), white blood cells (WBCs), and platelets, perform various functions essential for the proper functioning of the body. Here are the main functions of blood cells:
- Red Blood Cells (RBCs):
- Oxygen transport: RBCs carry oxygen from the lungs to the tissues and organs throughout the body. They contain a protein called hemoglobin, which binds to oxygen in the lungs and releases it in the tissues. RBCs also transport a small amount of carbon dioxide back to the lungs to be exhaled.
- Acid-base balance: RBCs transport bicarbonate ions, which help maintain the body’s acid-base balance and pH levels.
- White Blood Cells (WBCs):
- Immune defense: WBCs play a crucial role in the body’s immune system. They detect and eliminate foreign microbes, viruses, and other pathogens, protecting the body from infections. WBCs produce antibodies that neutralize harmful substances and regulate inflammation.
- Tissue repair: WBCs aid in the elimination of dead cells and debris, contributing to tissue repair and regeneration. They help remove damaged cells and promote the growth of healthy tissue.
- Control of body temperature and fluid balance: WBCs play a role in controlling body temperature and preserving fluid and electrolyte balance.
- Platelets:
- Blood clotting: Platelets are essential for the formation of blood clots. When a blood vessel is damaged, platelets migrate to the site of injury, clump together, and initiate a series of reactions that lead to the formation of a stable clot. This process helps prevent excessive bleeding and promotes wound healing.
- Tissue repair and regeneration: Platelets release growth factors that promote tissue repair, blood vessel formation (angiogenesis), and regeneration of damaged tissues.
All three types of blood cells contribute to the distribution of vital nutrients, hormones, and oxygen throughout the body. They play a crucial role in maintaining overall health, supporting the immune system, ensuring proper clotting, and aiding in the repair and regeneration of tissues.
FAQ
What are blood cells?
Blood cells are the cells that make up blood. They include red blood cells, white blood cells, and platelets.
What is the function of white blood cells?
White blood cells, or leukocytes, are part of the immune system and help the body fight off infections and diseases.
What is the function of red blood cells?
Red blood cells, or erythrocytes, carry oxygen from the lungs to the rest of the body and carry carbon dioxide from the body to the lungs to be exhaled.
Where are blood cells made?
Blood cells are made in the bone marrow, which is the spongy tissue inside bones.
How long do blood cells live?
The lifespan of blood cells varies by type. Red blood cells typically live for about 120 days, white blood cells can live for a few hours to a few days, and platelets live for about 7-10 days.
What happens when someone has a low red blood cell count?
A low red blood cell count, also known as anemia, can cause fatigue, weakness, shortness of breath, and other symptoms.
What happens when someone has a high white blood cell count?
A high white blood cell count, also known as leukocytosis, can be a sign of infection, inflammation, or other medical conditions.
Can blood cells be donated?
Yes, blood cells can be donated through blood donation. Red blood cells, platelets, and plasma can all be donated to help patients in need.
Can blood cells be replaced?
Yes, blood cells can be replaced through a bone marrow transplant. This is a medical procedure in which healthy stem cells are transplanted into a patient to replace damaged or diseased bone marrow.
References
- Blumenreich MS. The White Blood Cell and Differential Count. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 153. Available from: https://www.ncbi.nlm.nih.gov/books/NBK261/
- Barbalato L, Pillarisetty LS. Histology, Red Blood Cell. [Updated 2022 Nov 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539702/
- Dean L. Blood Groups and Red Cell Antigens [Internet]. Bethesda (MD): National Center for Biotechnology Information (US); 2005. Chapter 1, Blood and the cells it contains. Available from: https://www.ncbi.nlm.nih.gov/books/NBK2263/
- http://qu.edu.iq/el/mod/resource/view.php?id=60981
- https://basicmedicalkey.com/blood-3/
- https://mybiblioteka.su/10-80714.html
- https://www.statpearls.com/articlelibrary/viewarticle/28286/
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.