- Although it takes much longer—days or weeks—for the adaptive, or acquired, immune response to become established, it is more specific to pathogens and has memory.
- After being exposed to an antigen, whether by a vaccination or a pathogen, the body develops an adaptive immune response.
- When an infection cannot be stopped by the body’s innate immune response, the adaptive immune response kicks in.
- In reality, the adaptive immune response would be unable to be activated without input from the innate immune system.
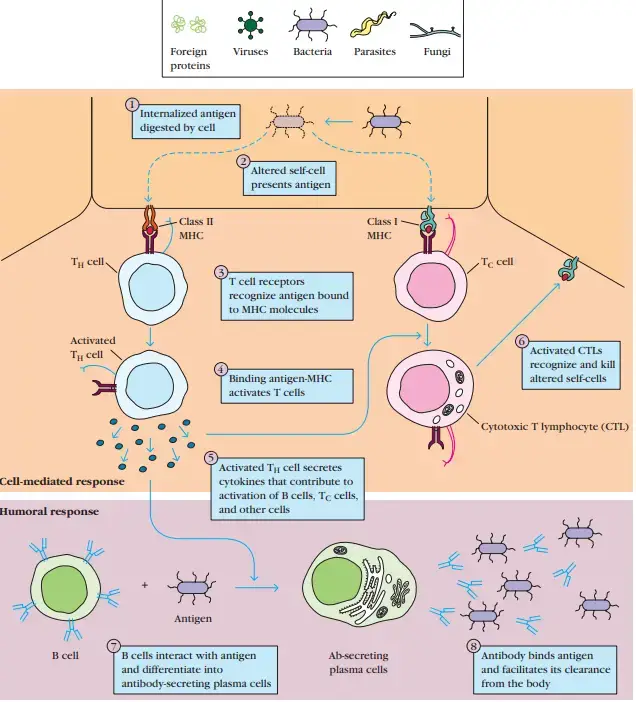
- In the adaptive immune system, T cells execute the cell-mediated immune response, while activated B cells and antibodies direct the humoral immune response.
- Pathogens are countered by a proliferation of T cells and B cells that have been activated and are specific to molecular structures on the invading pathogen.
- Their assault can either directly kill pathogens or stimulate the phagocytosis of pathogens to interrupt an infection.
- Adaptive immunity not only involves a memory to protect the host from reinfection with the same type of pathogen, but also to promote an effective and rapid response upon re-exposure.
Features Adaptive (Acquired) Immunity
- It is the resistance a somebody acquires over their lifetime.
- It occurs in response to exposure to a pathogen and is mediated by antibodies and T lymphocytes (helper T cells and cytotoxic T cells).
- It possesses immunologic memory and an exceptional capacity to distinguish between self and nonself antigens.
- Once acquired immune system cells have detected an antigen, the reaction to it is particular and can be repeated. In most situations, repeated exposure enhances the acquired immune response.
- The immune response to the second exposure occurs more rapidly, is stronger, and is frequently more effective at eliminating the pathogen.
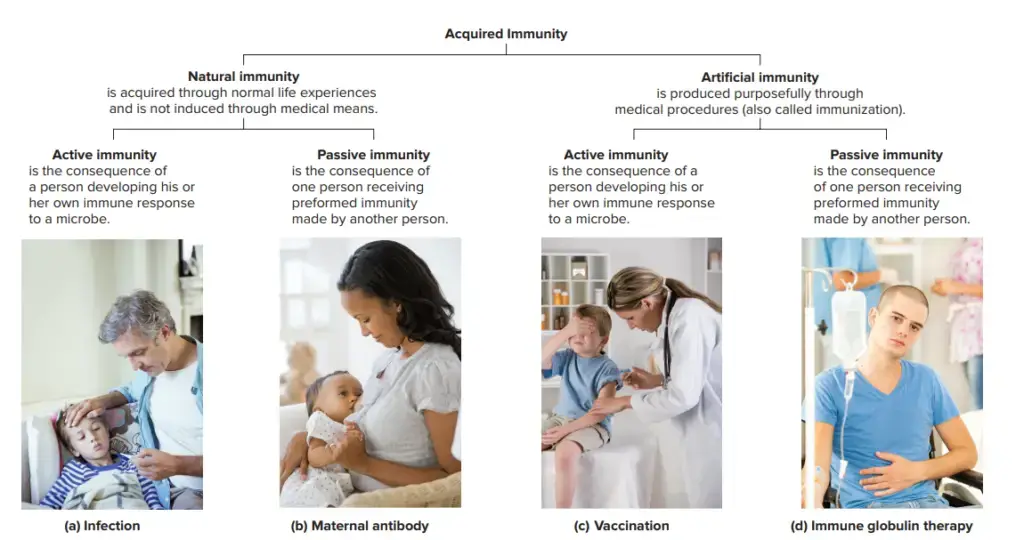
Types of acquired immunity
An acquired immunity against a microorganism may be produced through the host’s response to the bacterium or by the transfer of particular antibodies or lymphocytes. There are two types of immunity: active and passive.
1. Active immunity
- Active immunity is the immunity induced by exposure to a foreign antigen.
- Active immunity is the resistance that an individual develops in response to encounter with external antigens, such as microbes. This contact may take the following forms:
- Infection, clinical or subclinical.
- Immunization using infectious pathogens that are alive or dead, or their antigens
- Exposure to microbe-produced toxins and toxoids.
- Under all of these conditions, the host’s immune system is stimulated to produce an immunological response consisting of antibodies, activated helper T (TH) cells, and cytotoxic T lymphocytes/cells (CTLs).
- After a latent period during which the host’s immunity is primed to operate against the pathogen, active immunity emerges.
- Therefore, its onset is gradual, particularly during this early response. However, once active immunity develops, it is durable; this is the primary benefit of active immunity.
Types of Active immunity
There are two varieties of active immunity: natural active immunity and artificial active immunity
- Natural active immunity: It is transmitted through subclinical or clinical infections. Such inherent immunity is long lasting. For instance, persons with smallpox develop immunity to a second bout of the illness.
- Artificial active immunity: Vaccines induce it in human beings. There is a vast selection of vaccines against numerous microbiological pathogens. These vaccines may be live, dead, or comprised of bacterial components.
Mediators of active immunity
Humoral immunity and cell-mediated immunity mediate active immunity. These two forms of immunity are mediated by various immune system components and kill different types of infections in different ways.
a. Humoral immunity
- It is mediated by antibody molecules in the blood and mucosal secretions.
- B cells are the subgroup of lymphocytes that release antibodies.
- Antibodies identify microbial antigens, combine precisely with the antigens, counteract the infectiousness of microorganisms, and target bacteria for elimination via a variety of effector mechanisms.
- The primary defence mechanism against external microorganisms is humoral immunity.
b. Cell-mediated immunity
- It is mediated by CTLs and activated TH cells. TH cells release cytokines that activate phagocytic cells, allowing them to phagocytose and destroy germs.
- Against a wide range of bacterial and protozoan infections, this sort of cell-mediated immune response is very crucial.
- CTLs serve a crucial function in the destruction of virus-infected and tumour cells. They eliminate changed self-cells.
Differences between cell-mediated and humoral immunity
| Cell-mediated immunity | Humoral immunity |
| Immune response mediated by cells | Immune response mediated by antibodies |
| Both CD4+ and CD8+ T cells are involved | Only TH cells are involved |
| Mediates delayed (type IV) hypersensitivity | Mediates immediate (types I, II, and III) hypersensitivity |
| Protects against fungi, viruses, and facultative intracellular bacterial pathogens | Protects against extracellular bacterial pathogens and viruses infecting respiratory or intestinal tract; and prevents recurrence of viral infections |
| Only T-cell-dependent antigens lead to cell mediated immunity | B cells directly bind soluble antigens resulting in production of antibodies |
| Provides immunological surveillance and immunity against cancer | No major role in immunological surveillance |
| Participates in rejection of homografts and graftversus-host reaction | May be involved in early graft rejection due to preformed antibodies |
Antigen recognition
- Lymphocytes do not recognise the totality of antigens, which are typically extremely vast and intricate.
- Instead, both B and T cells identify specific antigenic determinants, or epitopes, on the antigens.
- Epitopes are the immunologically active sections of a complex antigen, specifically the areas that bind to B-cell or T-cell receptors.
- B cells and T cells have distinct antigen recognition systems. T cells only recognise the antigen when the epitope is “presented” by one of the specialised antigen-presenting cells, whereas B cells recognise the antigen through interaction with the epitope on their own.
- Once the antigen has been identified, these cells diversify through a series of complex procedures.
- This diversity contributes to the immune system’s uniqueness, one of its defining qualities.
Major histocompatibility complex (MHC)
- It is a genetically complicated organism with numerous loci. Class I and class II MHC molecules are the two major types of membrane-bound glycoproteins encoded by MHC loci.
- Antigens are presented by class II molecules to TH cells, while class I molecules do the same for CTLs.
- Foreign protein antigens must be degraded into tiny antigenic peptides that form complexes with class I or class II MHC molecules in order for T cells to identify them.
- Antigen processing and presentation refers to the conversion of proteins into MHC-associated peptide fragments.
2. Passive immunity
- Passive immunity is acquired through the transmission of serum or lymphocytes from an individual who has been specially vaccinated.
- This is an effective technique for conferring resistance quickly, i.e., without waiting for an active immune response to develop.
Types of Passive immunity
Passive immunity may be natural or artificial.
a. Natural passive immunity
- During pregnancy, it is observed when IgG is transferred from mother to foetus.
- This is the foundation for preventing neonatal tetanus in newborns through aggressive immunisation of expectant moms.
- It is accomplished by delivering tetanus toxoid to pregnant women during their third trimester.
- This causes the mother to produce large levels of antibodies against tetanus toxin, which are then transferred to the foetus via the placenta.
- After delivery, the antibodies protect newborns against the risk of tetanus.
- During breastfeeding, IgA is also shown to be transferred from the mother to the infant, demonstrating the presence of passive immunity.
b. Artificial passive immunity
- It is caused by administering premade antibodies, typically in the form of antiserum, produced against an infectious pathogen.
- By administering these antisera, enormous quantities of antibodies are made available in the receiver to counteract the effect of poisons.
- During the incubation stage, the administration of premade antibodies against rabies and hepatitis A and B viruses, etc., prevents virus reproduction and thereby modifies the course of infection.
- The fundamental benefit of passive immunity is the immediate availability of huge amounts of antibodies.
- Two downsides of passive immunity are the limited lifespan of these antibodies and the likelihood of hypersensitivity reaction if antibodies generated in other animal species are administered to persons who are hypersensitive to these animal globulins (e.g., serum sickness).
- Combined passive–active immunity is achieved by administering both preformed antibodies (antiserum) and a vaccination to provide both rapid and long-term protection against a disease, respectively.
- This method is used to prevent some infectious diseases, including tetanus, rabies, and hepatitis B.
Cells of the adaptive immune system
- Unlike the innate immune system, the adaptive immune system is comprised of fewer cell types: B cells and T cells.
- B cells and T cells are lymphocytes that originate in the bone marrow from multipotent hematopoietic stem cells.
- After being produced in the bone marrow, stem cells must mature and become active. Each type of cell develops in a unique manner to reach their mature forms.
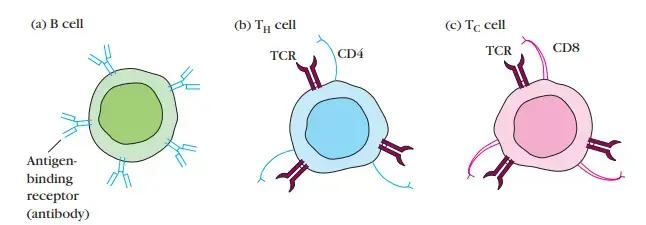
B cells
- After formation and maturation in the bone marrow (hence the name “B cell”), naive B cells enter the lymphatic system to circulate in the body.
- Naive B cells encounter an antigen in the lymphatic system, which initiates the maturation process for the B cell. B cells have one of millions of distinct antigen-specific surface receptors encoded in the organism’s DNA.
- Naive B cells, for instance, express antibodies on their cell surface, which are also known as membrane-bound antibodies.
- When a naive B cell encounters an antigen that is compatible with its membrane-bound antibody, it rapidly divides to become a memory B cell or an effector B cell, also known as a plasma cell. Antibodies can bind directly to antigens.
- The antigen must effectively bind with the membrane-bound antibody of a naive B cell in order to initiate differentiation, or the process of a B cell transforming into one of its new forms.
- Memory B cells express the same antibody bound to the cell membrane as the original naive B cell, or “parent B cell.”
- Plasma B cells produce the identical antibody as their parent B cells, but they are not membrane-bound.
- Plasma B cells can instead produce antibodies. Antibodies function to recognise free pathogens that circulate throughout the body. Plasma cells and memory B cells are produced when a naive B cell divides and differentiates.
- Additionally, B cells express a specialised receptor known as the B cell receptor (BCR). B cell receptors aid in antigen binding, antigen internalisation, and antigen processing. Additionally, B cell receptors play a crucial role in signalling pathways.
- In order to communicate with other immune cells, the B cell can initiate signalling pathways, such as cytokine release, 7 after antigen internalisation and processing. Check out this article about cell-to-cell communication for more information on cell signalling.
T cells
- T progenitor cells travel from the bone marrow to the thymus (thus the name “T cell”) to mature and become T cells.
- During their development in the thymus, T cells begin to express T cell receptors (TCRs) as well as CD4 and CD8 receptors.
- All T cells express either CD4 or CD8 T cell receptors, but not both. Thus, some T cells display CD4, whereas others express CD8.
- T cell receptors can only recognise antigens that are attached to Major Histocompatibility Complex class 1 (MHCI) and class 2 receptor molecules, unlike antibodies, which can bind to antigens directly (MHCII).
- On antigen-presenting cells, such as dendritic cells and macrophages, these MHC molecules are membrane-bound surface receptors. By attaching to either MHCI or MHCII, CD4 and CD8 contribute to T cell recognition and activation.
- T cell receptors must undergo a process known as rearrangement, which results in the almost infinite recombination of a gene that encodes T cell receptors.
- Rearrangement provides for a great deal of binding variety diversity. This diversity could lead to unintentional attacks against self-cells and -molecules, as certain rearrangement configurations can accidentally resemble a person’s self-proteins and -molecules.
- Only foreign antigens bound to self-MHC molecules should be recognised by mature T cells for an optimal immunological response.
- T cells undergo two selection steps to ensure optimal function once they have reached maturity and have been liberated from the thymus:
- Positive selection assures MHC limitation by assessing the capacity of MHCI and MHCII to differentiate between self- and non-self-proteins. To pass the positive selection process, cells must be able to bind exclusively to their own MHC molecules. These cells fail the positive selection process and are destroyed by apoptosis if they bind nonself molecules instead of self-MHC molecules.
- Negative selection is a self-tolerance test. Negative selection evaluates the unique binding capacities of CD4 and CD8. Ideal self tolerance occurs when T cells only bind to self-MHC molecules that present a foreign antigen. If a T cell connects via CD4 or CD8 to a self-MHC molecule that is neither presenting an antigen nor presenting a self-antigen, it will fail negative selection and be killed by apoptosis.
- These two selection processes are in place to safeguard your cells and tissues from your immune reaction. Without these selection processes, autoimmunity would be significantly more prevalent.
- Three types of mature T cells remain after positive and negative selection: Helper T cells (THcells), Cytotoxic T cells (TCells), and T regulatory cells (T reg cells).
- Helper T cells express CD4 and are involved in the activation of TC cells, B cells, and other immune cells.
- Cytotoxic T cells are important for eliminating pathogens and diseased host cells; they express CD8.
- CD4 and CD25 are receptors that are expressed by T regulatory cells. The ability of T regulatory cells to differentiate between self and nonself molecules reduces the risk of autoimmune disorders.
Immunological memory
- Due to the fact that the adaptive immune system can learn and recall specific pathogens, it can provide long-lasting defence and protection against recurring infections.
- When the adaptive immune system is exposed to a new threat, the antigen is memorised in order to prevent recurrence of the disease.
- The concept of immunological memory derives from the body’s capacity to produce antibodies against many infections.
- Immunizations are an excellent illustration of immunological memory. Vaccination against a virus can be administered using either active, but weakened or attenuated virus or inactive virus components.
- Both attenuated entire viruses and virus particles are incapable of causing an infectious disease. Instead, they simulate the presence of an active infection to elicit an immune response, despite the absence of actual dangers. By receiving a vaccination, you expose your body to the antigen necessary to generate antibodies against a particular virus and acquire a memory of the virus without becoming unwell.
- Some immunological memory system malfunctions can result in autoimmune disorders.
- Due to a cross-reactive immune reaction against the infection, the molecular mimicry of a self-antigen by an infectious pathogen, such as bacteria and viruses, may induce autoimmune disease. Streptococcus infection is an example of an organism that exploits molecular mimicry to evade immune protection.
Differences between passive and active immunity
| Passive immunity | Active immunity |
| No active host participation received passively | Produced actively by host’s immune system |
| Antibodies transferred directly | Antibodies induced by infection or by immunogens |
| Passive immunity is due to readymade antibodies | Active immunity often involves both the cell-mediated and humoral immunity |
| Types: Natural—transfer of maternal antibodies through placenta; Artificial—injection of immunoglobulins | Types: Natural—clinical or inapparent infection; Artificial— induced by vaccines |
| Immediate immunity; no lag period | Immunity effective only after lag period |
| Transient; less effective | Durable; effective protection |
| No immunological memory | Immunological memory present |
| Subsequent dose less effective due to immune elimination | Booster effect on subsequent dose |
| No negative phase | Negative phase may occur |
| Applicable even in immunodeficient | Not applicable in immunodeficient |
What is Local Immunity?
- Local immunity is the immunity at a specific spot, typically at the site of invasion and growth of a disease.
- IgA antibodies present in various bodily fluids give local immunity.
- Local plasma cells found on mucosal surfaces or in secretory glands produce these antibodies.
- Natural infection or oral or intranasal administration of attenuated live virus vaccines promotes local immunity in the gut mucosa and nasal mucosa, respectively.
What is Herd Immunity?
- Herd immunity refers to a community’s immunity as a whole. The eradication of an infectious disease is contingent upon the development of a strong herd immunity to the pathogen.
- When herd immunity to a disease is very low, showing the presence of a greater number of susceptible individuals in the population, an epidemic of that disease is likely to arise.
Functions of Adaptive (Acquired) Immunity
When a disease evades the innate immune system and (1) develops a threshold quantity of antigen and (2) generates “stranger” or “danger” signals activating dendritic cells, acquired immunity is activated in vertebrates.
The principal roles of the acquired immune system are:
- Antigen presentation involves the recognition of certain “non-self” antigens in the presence of “self” antigens.
- Generation of reactions that are targeted to destroy pathogens or pathogen-infected cells to the greatest extent possible.
- In the formation of immunological memory, pathogens are “remembered” by memory B cells and memory T cells.
The adaptive immune system requires 4–7 days to mount a substantial response in humans.
References
- Alberts B, Johnson A, Lewis J, et al. Molecular Biology of the Cell. 4th edition. New York: Garland Science; 2002. Chapter 24, The Adaptive Immune System. Available from: https://www.ncbi.nlm.nih.gov/books/NBK21070/
- https://www.khanacademy.org/science/in-in-class-12-biology-india/xc09ed98f7a9e671b:in-in-human-health-and-disease/xc09ed98f7a9e671b:in-in-types-of-immunity-and-the-immune-system/a/adaptive-immunity
- https://opentextbc.ca/biology/chapter/23-2-adaptive-immune-response/
- https://www.zmchdahod.org/pdf/college/acquiredimmunity11102018.pdf
- https://mlinjawi.kau.edu.sa/Files/0001735/files/18855_LECTURE%2005%20Acquired%20immunity%20and%20clonal%20selection.pdf