What is Reticulocytes?
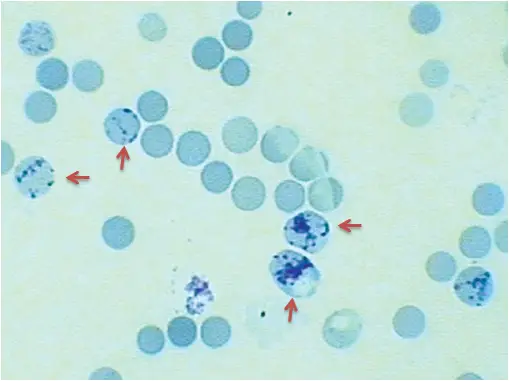
Reticulocytes are immature red blood cells (erythrocytes) that have not yet completed the final stages of maturation. They are usually produced in the bone marrow and have a characteristic reticulated (network-like) appearance when stained with special dyes.
Reticulocytes are important in the evaluation of anemia, as they provide information about the bone marrow’s ability to produce new red blood cells. A higher-than-normal reticulocyte count can indicate that the bone marrow is compensating for a low red blood cell count, such as in cases of iron-deficiency anemia or hemorrhage. A lower-than-normal reticulocyte count, on the other hand, can indicate a problem with the bone marrow’s ability to produce new red blood cells, such as in cases of aplastic anemia or leukemia.
Reticulocytes can also be used to monitor the effectiveness of treatments for anemia, such as iron supplementation or blood transfusions. The reticulocyte count is usually performed as part of a complete blood count (CBC) along with other tests to diagnose and monitor anemia.
Principle
Based on the ability of ribosomal RNA to react with an isotonic solution of a supravital stain such as New methylene blue or brilliant cresyl blue, the reticulocyte count is determined. Supravital stains are those that discolour live tissue. Therefore, in order to detect ribosomal RNA in reticulocytes, they must be fixed.
Blood and the stain are combined and incubated. The RNA in the cell precipitates as a network or reticulum that is dark blue. A blood smear is prepared and analysed using a microscope. Due to the impossibility of a direct count, a relative count is performed against the number of RBcs and expressed as a percentage of RBCs.
Requirements for Reticulocyte Count
- Specimen: EDTA whole blood/capillary blood
- Reagent:
- New Methylene Blue:
New methylene blue = 1.0 gm
Sodium citrate = 0.6 gm
Sodium chloride = 0.7 gm
Distilled water = 100 ml - OR, Brilliant Cresyl Blue:
Brilliant cresyl blue = 1.0 gm
Sodium citrate = 0.6 gm
Sodium chloride = 0.7 gm
Distilled water = 100 ml
- New Methylene Blue:
Procedure of Reticulocyte Count
- Take two to three drops of the dye solution and place them in a test tube.
- Add 2-4 drops of blood sample that has been thoroughly mixed and mix.
- Incubate the tube at 370 degrees Celsius for 10 to 15 minutes.
- After incubation, thoroughly combine and spread a thin layer of coloured blood.
- When the films are dry, examine them without fixing or counterstaining.
- Determine the number of reticulocytes present among 1000 RBCs. The reticulum or network of reticulocytes will be dark blue.
Calculation for Reticulocyte Count
1. Retculocyte Percentage
This is the proportion of reticulocytes per 1,000 red blood cells.
Retculocyte Percentage = No. of Retculocyte per 1000 RBCs/1000 x 100%
2. Absolute Reticulocyte Count
Absolute reticulocyte count (ARC) is the number of reticulocytes present in 1 mL of whole blood.
Absolute Reticulocyte Count = Reticulocyte (%) x RBC Count (1012/L)
3. Corrected Reticulocyte Count
Because whole blood contains less RBCs, the percentage of reticulocytes may be erroneously inflated in specimens with a low hematocrit. Using a correction factor, the average normal hematocrit is determined to be 45%.
Corrected Reticulocyte Count = Reticulocyte (%) x Patient’s Hematocrit / 45
Reference Ranges
| Adults | 0.2-2% |
| Infants | 2-6% |
| Childrens upto 5 years | 0.2-5.0% |
Clinical Significances
Reticulocytosis
Increased reticulocyte count is referred to as reticulocytosis. The like:
- Hemolysis-associated anaemias: Immunologic hemolysis, Primary RBC membrane abnormalities, Sickle cell disorders, Enzyme deficiencies, Contact with poisons
- As a result of bleeding
- After therapy for anaemias
- Increase in physiology during pregnancy and in newborns.
Reticulocytopenia
A condition characterised by a decline of reticulocytes. For example,
- iron deficiency anaemia.
- Aplastic anaemia.
- Radiation treatment
- Anemia pernicious, untreated.
- Cancer of the bone marrow
Importance of Reticulocyte Count
The reticulocyte count is an important laboratory test that provides information about the bone marrow’s ability to produce new red blood cells. It is used to evaluate and monitor anemia, which is a condition characterized by a low red blood cell count. The reticulocyte count is performed as part of a complete blood count (CBC) and can help to diagnose the cause of anemia, monitor the effectiveness of treatment, and track the progression of the disease.
Here are some of the key benefits and importance of a reticulocyte count:
- Evaluates Anemia: The reticulocyte count is used to diagnose anemia and to evaluate the bone marrow’s ability to produce new red blood cells in response to anemia. A higher-than-normal reticulocyte count indicates that the bone marrow is compensating for a low red blood cell count, while a lower-than-normal reticulocyte count can indicate a problem with the bone marrow’s ability to produce new red blood cells.
- Monitors Treatment Effectiveness: The reticulocyte count can be used to monitor the effectiveness of treatments for anemia, such as iron supplementation or blood transfusions. It provides information about how well the treatment is working and can be used to adjust the treatment plan if necessary.
- Identifies Bone Marrow Disorders: A low reticulocyte count can indicate a problem with the bone marrow’s ability to produce new red blood cells, which can be caused by a number of conditions, such as aplastic anemia, leukemia, or other bone marrow disorders. The reticulocyte count can help to identify these disorders and guide further testing and treatment.
- Tracks Disease Progression: The reticulocyte count can be used to track the progression of anemia or bone marrow disorders over time and to monitor response to treatment. This information can help to guide treatment decisions and predict future health outcomes.
In conclusion, the reticulocyte count is an important laboratory test that provides valuable information about the bone marrow’s ability to produce new red blood cells. It is widely used in the evaluation and management of anemia and other hematological disorders.
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.