West Nile virus (WNV) is the most prevalent disease transmitted by mosquitoes in the continental United States. It is often transmitted to humans through the bite of an infected mosquito. Cases of West Nile virus arise during the summer and fall mosquito season. There are no vaccinations or drugs to prevent or treat WNV in humans. The majority of those infected with WNV do not experience symptoms. Approximately one in five infected individuals develop fever and other symptoms. Around 1 in 150 infected individuals get a severe, often deadly disease. You can lower your risk of West Nile virus by using insect repellent and wearing long-sleeved shirts and trousers.
West Nile Virus (WNV)
- The West Nile virus (WNV) is an RNA virus with a single strand that causes West Nile illness. It belongs to the family Flaviviridae, which includes the Zika virus, dengue virus, and yellow fever virus.
- The virus is transmitted mostly by mosquitoes, specifically Culex species. The principal hosts of WNV are birds, resulting in a “bird–mosquito–bird” virus transmission cycle. The virus is genetically related to the family of viruses that cause Japanese encephalitis.
- The virus causes disease symptoms in both humans and horses, and infrequently in other species. In Uganda, the disease was identified for the first time in 1937, and by the end of the 20th century, it had spread to many other countries of the world.
- The enclosed, single-stranded RNA virus West Nile virus is a member of the Flaviviridae family. It is an arbovirus that is transmitted to people by mosquito bites.
- It is known to cause an extensive variety of diseases in people. They range from asymptomatic infected patients to those with fever and malaise to those with florid neurological impairments caused by encephalitis.
- Yet, the majority of West Nile virus infections are asymptomatic. Around one-fourth of patients experience fever with signs of a viral illness, whereas approximately one-hundred people acquire neuroinvasive disease.
- In the 1990s, the West Nile virus spread to Europe, Asia, and North America, where it had previously been observed only in Africa. It is now present across the majority of the planet.
- The West Nile virus is transmitted to people through mosquito bites. The mosquito species Culex is the most prevalent vector. The West Nile virus can also infect birds, horses, dogs, and a variety of other species.
- Wild birds may be the most suitable hosts for harbouring and propagating the virus. Due to the low and ephemeral virus levels in the bloodstream, humans are regarded as unintentional dead-end hosts. Other uncommon transmission routes include infected donor blood, organs, breast milk, and transplacental infection.
- Around 1% of persons will develop severe symptoms, and the overall morbidity rate increases with age. Neurological problems are the most prevalent. Sadly, the absence of federal money has prevented many states from maintaining active surveillance of this virus.
Structure of West Nile Virus (WNV)
- WNV, like the vast majority of flaviviruses, is an enclosed virus with icosahedral symmetry. Studies using an electron microscope reveal a 45–50 nm virion surrounded by a reasonably smooth protein shell; this resembles the structure of the dengue fever virus, another Flavivirus.
- Two structural proteins comprise the protein shell: glycoprotein E and tiny membrane protein M. Protein E has multiple roles, including receptor binding, viral attachment, and membrane fusion-mediated cell entrance.
- The outside protein shell is coated by the viral envelope, a lipid membrane obtained from the host.
- Cholesterol and phosphatidylserine have been discovered as components of the flavivirus lipid membrane, but other membrane components have yet to be identified.
- The lipid membrane has multiple functions in viral infection, including acting as signalling molecules and facilitating viral entrance into the cell.
- Particularly, cholesterol is essential for the entry of WNV into a host cell. E and M, two envelope proteins of the virus, are introduced into the membrane.
- The nucleocapsid is composed of 105 amino acid residues of capsid (C) proteins that are attached to the RNA genome. The capsid protein is a structural protein whose primary function is to bundle RNA into growing viruses. It has been discovered that the capsid inhibits apoptosis via the Akt pathway.
Genome structure of West Nile Virus (WNV)
- WNV is a single-stranded, positive-sense RNA virus. Its genome consists of roughly 11,000 nucleotides and is flanked by 5′ and 3′ noncoding stem loop structures.
- The coding section of the genome encodes three structural proteins and seven nonstructural (NS) proteins, which are not incorporated into the viral structure.
- The WNV genome is initially translated into a polyprotein, which is then broken apart by viral and host proteases (i.e. NS1, C, E).
Structural proteins
- The structural proteins C, prM/M, and E are, respectively, capsid, precursor membrane, and envelope proteins.
- The structural proteins are situated at the 5′ end of the genome and are processed by both host and viral proteases into mature proteins.
| Structural Protein | Function |
|---|---|
| C | Capsid protein; encloses the RNA genome and bundles it into immature viral particles. |
| prM/M | Infectious viruses contain M protein, which activates proteins involved in viral entrance into the host cell. prM (precursor membrane) protein is present on immature virions; additional furin cleavage to M protein transforms the virions into infectious particles. |
| E | To enter the host cell, a glycoprotein that forms the viral envelope attaches to receptors on the cell surface. |
Nonstructural proteins
NS1, NS2A, NS2B, NS3, NS4A, NS4B, and NS5 constitute nonstructural proteins. These proteins are mostly involved in viral replication or serve as proteases. Nonstructural proteins are situated close to the 3′ terminus of the genome.
| Nonstructural Protein | Function |
|---|---|
| NS1 | NS1 is a viral replication cofactor, specifically for replication complex control. |
| NS2A | NS2A serves multiple purposes, including viral replication, virion assembly, and induction of host cell death. |
| NS2B | Along with NS3, it forms the NS2B-NS3 protease complex. Transmembrane domains that bind the protease to intracellular membranes are present. |
| NS3 | A serine protease that cleaves polyproteins to create mature proteins; it also functions as a helicase. |
| NS4A | NS4A is a viral replication cofactor that controls the activity of the NS3 helicase. |
| NS4B | Inhibits interferon signaling. |
| NS5 | NS5, the largest and most conserved protein of WNV, functions as a methyltransferase and an RNA polymerase, while lacking proofreading abilities. |
Epidemiology of West Nile Virus
- Uganda reported the first cases of West Nile virus in 1937. In 1999, seven deaths and 62 cases of encephalitis were reported in New York; this marked the first appearance of the virus in the western hemisphere. Nowadays, Africa, Europe, Asia, North America, Australia, and the Middle East are home to West Nile virus.
- First epidemics of the virus manifested as self-limiting and mild illnesses. Midway through the 1990s, the West Nile virus was associated with serious neurologic illness.
- Meningitis and encephalitis (neuroinvasive disease) were found in less than one percent of infected patients in 2013, with a ten percent fatality rate, according to a comprehensive literature analysis. 25% of infected individuals get West Nile fever, whereas the remaining 75% exhibit few or no symptoms.
- This leads to the probable underreporting of West Nile virus infections on a massive scale. Due to the mosquito vector’s life cycle and the amplifying effect of the bird-mosquito-bird cycle, outbreaks tend to occur in late summer and fall. In warmer climates, cases can occur all year long.
- From 1999 to 2015, there were about 444,000 confirmed and probable cases of West Nile virus in the United States, including over 20,000 cases of neuroinvasive illness.
- The number of neuroinvasive cases fluctuates greatly from one year to the next, ranging from 386 to 2,946.
- Serologic surveys and blood donor screening data indicate a neuroinvasive disease rate of approximately 0.5% among infected individuals and an infection rate of 10% in outbreak-affected regions. This information suggests between 3 and 5 million cases of illness.
Transmission of West Nile Virus
West Nile virus is often transmitted to humans by the bite of an infected mosquito.
As mosquitoes feed on infected birds, they become infected. Infected mosquitoes then transmit West Nile virus to humans and other animals through their bites.
In a very tiny number of instances, West Nile virus has been transmitted via:
- Exposition in the laboratory
- Transfusion of blood and organ transplantation
- Mother-to-child throughout pregnancy, birth, and breastfeeding
West Nile virus is not spread:
- Through coughing, sneezing, or direct contact
- By touching living creatures
- From handling contaminated live or dead birds. Avoid using bare hands when handling deceased animals. If you are disposing of a deceased bird, throw the carcass in a rubbish bin using gloves or two plastic bags.
- By consuming infected animals, such as birds. Always adhere to the guidelines for thoroughly cooking meat.
Replication of West Nile Virus
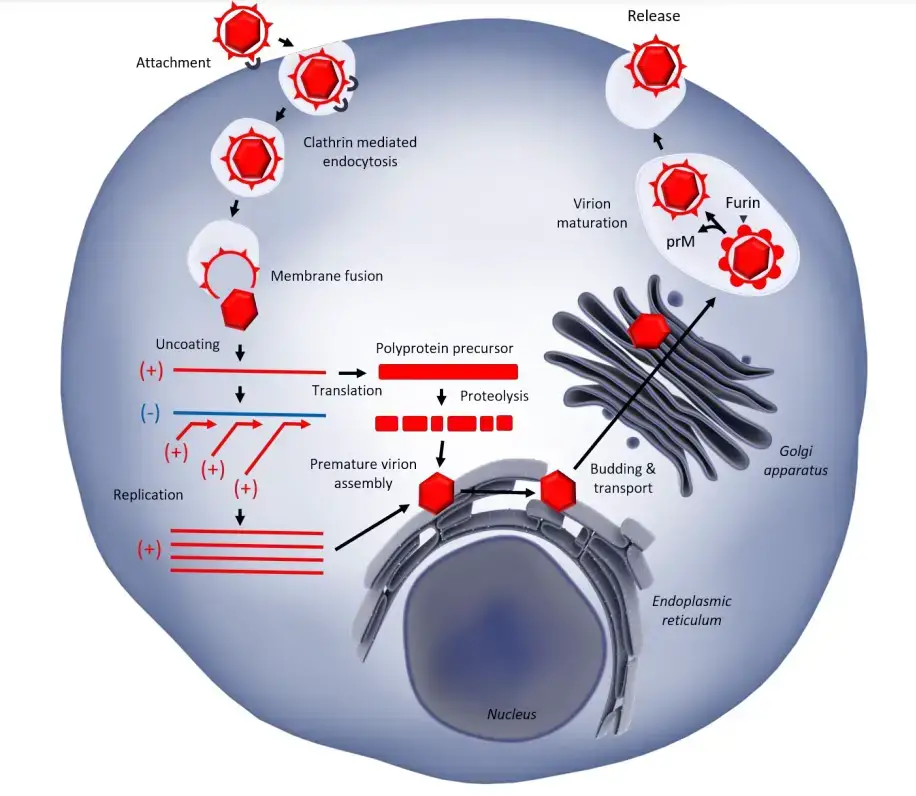
- In human cells, the WNV replication cycle begins with viral envelope glycoproteins engaging cellular receptors, such as the Dendritic Cell-Specific Intracellular adhesion molecule-3-Grabbing Non-integrin (DC-SIGN(R)), which is highly expressed by dendritic cells (DCs) and likely integrins.
- Viral entry is next mediated by clathrin-dependent endocytosis and acidification, which results in membrane fusion and the release of genetic material into the cytoplasm, where viral RNA is translated into a polyprotein.
- Seven non-structural proteins (NS1A, NS1B, NS2A, NS2B, NS3, NS4A, NS4B, and NS5) form the replication complex in which genomic RNA is synthesised. The newly synthesised genomes are then integrated at endoplasmic reticulum (ER) membranes with structural proteins (capsid C, envelope E, and pre-mature membrane prM) to produce pre-mature virions.
- After assembly, prM is cleaved by host cell furin in the transGolgi network to produce mature virions, which are then discharged by exocytosis. While this description covers the replicative cycle under optimal conditions for the virus, immune responses can target distinct phases to inhibit viral reproduction.
- E protein binds viral particles to cellular receptors in the plasma membrane. Following virus attachment, endocytosis mediated by clathrin and acidification of endosomal vesicles allow virus entrance.
- Endosomal acidification causes viral fusion with the endosomal membrane and the release of the (+) ssRNA genome into the cytoplasm following virion decoating.
- The viral genome is subsequently translated into a single polyprotein, which is then cleaved by viral proteases NS2B/NS3 and cellular proteases [30]. All NS proteins are located in the replication organelles of the ER.
- The viral RNA-dependent RNA polymerase NS5, along with other NS proteins, synthesises a (-)ssRNA intermediate that acts as a template for genomic (+)ssRNA production in these compartments.
- On the ER, the structural proteins C, E, and prM assemble with genomic RNA to create immature virion particles. Immature viral particles traverse the secretory route, resulting in furin-mediated cleavage of prM into mature membrane protein M and glycosylation of viral envelope protein. Eventually, mature virions are discharged at the plasma membrane through exocytosis.
Pathogenesis of West Nile Virus
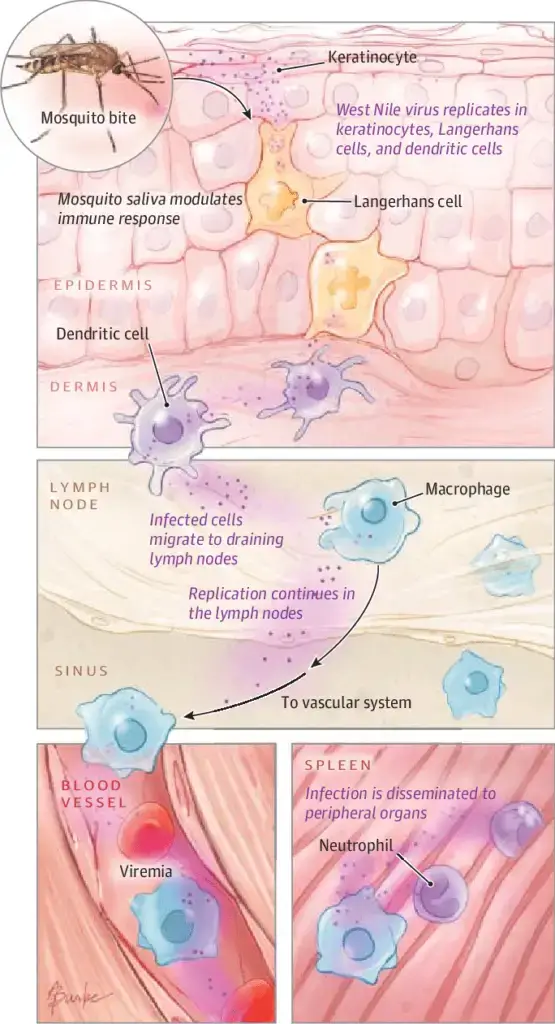
- The majority of our understanding of WNV transmission and pathology is derived from studies in rodent models. WNV infects keratinocytes and Langerhans cells after an infected mosquito bite, which move to lymph nodes and result in primary viremia.
- The virus then travels to peripheral visceral organs such as the kidney and spleen, where it undergoes a second replication stage in epithelial cells and macrophages, respectively.
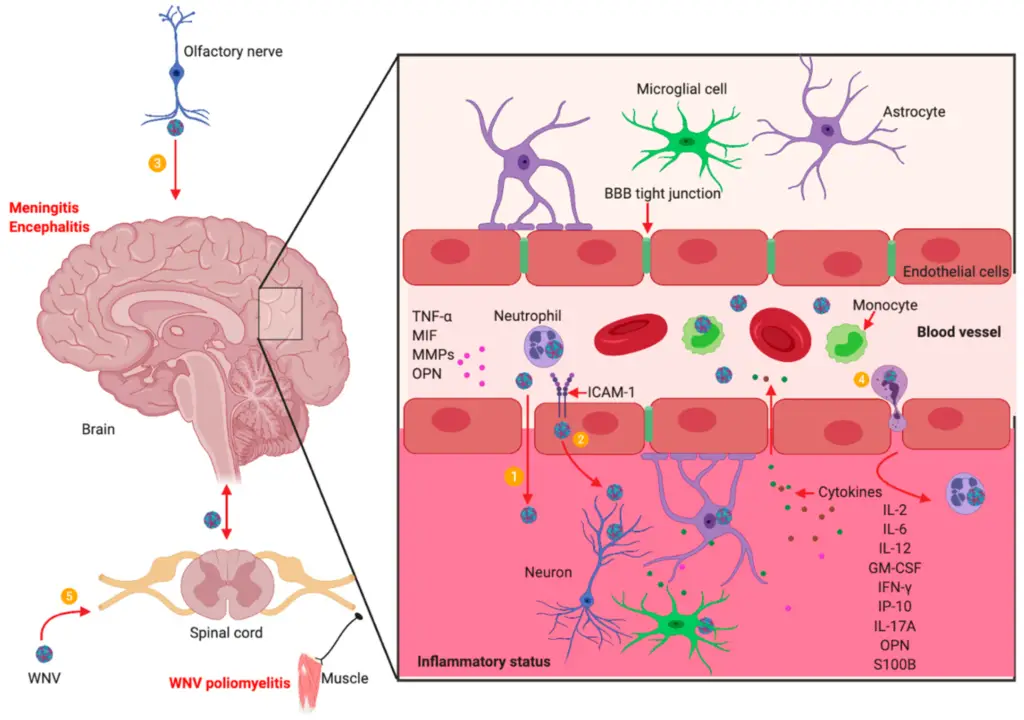
- Depending on the degree of viremia, which reaches its peak on day 3 post-infection (p.i.) in mice, the virus may penetrate the blood-brain barrier (BBB) and enter the central nervous system (CNS), resulting in meningo-encephalitis.
- Several mechanisms have been hypothesised for WNV entrance into the CNS, including TNF-a-mediated changes in endothelial cell permeability and infection of olfactory neurons and dissemination to the olfactory bulb.
- Additional methods include direct axonal retrograde transport from infected peripheral neurons and virus transport by infected immune cells trafficking to the Brain. WNV infects neurons in several regions of the Brain, causing architectural loss, degeneration, and cell death.
- In a later stage, mononuclear cells infiltrate the diseased regions, although it is unclear if they contribute to pathogenesis by killing infected cells and producing cytokines or if they aid stop infection.
- Infected and damaged brain stem, hippocampi, and spinal cord are observed in both human and rodent illness victims. It was discovered that the persistence of WNV in mice is tissue-dependent. Infectious virus could survive for up to four months post-infection, particularly in mice who did not develop symptoms during acute infection and in the skin and spinal cord.
- Similar persistence may also occur in people following a minor febrile illness or subclinical infection; 3% of WNV-positive blood donors had detectable WNV RNA in their blood between 40 and 104 days after the initial donation.
- Less is known about WNV’s pathogenesis in wild birds. Using histology and RT-PCR, the virus has been found in the brain, liver, lungs, heart, spleen, and kidneys of numerous avian species, including ravens, blue jays, goshawks, and magpies.
- Several avian species were shown to be viremic six days after inoculation, with sufficient viremic titers to transmit the virus to mosquitoes through their bites. Infectious WNV was found in the tissues of wild birds for up to six weeks.
- Nonetheless, it is essential to clarify that immune response, virulence, and viral persistence are largely species- and strain-dependent, implicating various genetic determinants of virulence. Immune response, virulence, and viral persistence vary widely among avian species in different geographic regions.
Clinical Manifestations of West Nile Virus
- In around 80% of infected individuals, West Nile virus infection is either asymptomatic (no symptoms) or can lead to West Nile fever or severe West Nile disease.
- Around 20% of infected individuals will get West Nile fever. Symptoms include fever, headache, fatigue, body aches, nausea, vomiting, and occasionally a rash (on the trunk of the body) and swollen lymph nodes.
- Symptoms of severe disease (also known as neuroinvasive disease) include headache, high fever, neck stiffness, stupor, disorientation, coma, tremors, convulsions, muscle weakness, and paralysis.
- An estimated 1 in 150 people infected with West Nile virus will develop a more severe type of illness. When infected with WNV, those over the age of 50 and immunocompromised individuals (such as transplant recipients) are at the greatest risk of becoming extremely unwell.
- Typically, the incubation period lasts from 3 to 14 days.
Diagnosis of West Nile Virus
Laboratory diagnosis depends on the isolation of virus, the detection of viral antigens or RNA in blood or tissues, or the detection of virus-specific IgM antibody, which must be confirmed by the detection of IgG antibody in the same or a subsequent sample.
Antibody
- Cross-reactivity between Flavivirus antigens is a challenge for serological diagnosis and epidemiological studies.
- Sera need to be tested against different related viruses and confirmed by assays such as hemagglutination inhibition, immunofluorescence or plaque reduction neutralization test (PRNT), considered the gold standard.
- A 4-fold increase in PRNT titers between 2 sequential serum samples collected 2-3 weeks apart confirms an acute WNV infection.
- WNV neutralizing titers 4-fold higher than titers to other related-flavivirus is taken as a probe of the specificity of the infection.
- Serological testing was initially based on IgM antibody capture assays (MAC-ELISA) and indirect IgG ELISAs, followed by retesting of positive samples by PRNT.
- ELISAs using monoclonal antibody blocking assays were later developed.
- IgM in the cerebrospinal fluid is indicative of CNS infection, but data should be taken with caution since IgM may persist for an extended period.
- Various assays have been used for detecting anti-WNV antibodies in human and animal samples, including ELISAs using inactivated whole virus as antigen, and those using recombinant viral proteins, mainly the envelope E protein or parts of it.
- These recombinant antigens have been expressed in bacteria, mammalian cells, insect cells, and larvae.
- Microsphere particles in conjunction with fluorescent labeled antibodies and lateral-flow assays have also been recently assayed.
- ELISAs based on inactivated whole virus as antigen require biosafety level 3 (BSL-3) containment facilities to grow the virus, posing risks for laboratory personnel.
Antigen
- Virus isolation in susceptible cell culture is the best method for detecting viruses, but it’s difficult because viremia is typically short-lived and at low levels.
- The need for biosafety level 3 (BSL-3) facilities also makes it challenging.
- As a result, alternative methods have been developed.
- One method is to detect viral antigens using antigen-capture ELISAs, dipstick assays, or immunohistochemical methods.
Nucleic acid
- Different methods have been used to detect WNV RNA for surveillance and diagnosis.
- These methods include reverse transcription polymerase chain reaction (RT-PCR) assays, quantitative real-time RT-PCR, and nucleic acid sequence-based amplification.
- All of these methods have been widely used to test mosquito pools, as well as blood and cerebrospinal fluid (CSF) samples from animals and humans.
- However, samples from humans are usually collected after the onset of clinical signs, when the virus is less likely to be present in them.
Treatment of West Nile Virus
- There is no vaccination or particular treatment for West Nile virus infection. Antibiotics do not treat viruses.
- Relaxation, water, and nonprescription painkillers may alleviate certain symptoms.
- In extreme situations, hospitalisation is frequently required for patients to obtain supportive care, such as intravenous fluids, pain medication, and nursing care.
Prevention and Control of West Nile Virus
West Nile Virus (WNV) is primarily transmitted to humans through the bite of infected mosquitoes, and prevention and control measures mainly focus on reducing mosquito populations and avoiding mosquito bites. Here are some common methods used for the prevention and control of West Nile Virus:
- Mosquito control: This includes measures such as eliminating standing water where mosquitoes breed, using larvicides to kill mosquito larvae, and using insecticides to kill adult mosquitoes.
- Personal protection: To avoid mosquito bites, people are advised to wear long-sleeved shirts and pants, use insect repellents containing DEET or other EPA-approved active ingredients, and avoid outdoor activities during peak mosquito hours.
- Public education: Raising public awareness about the risk of WNV and how to prevent mosquito bites is crucial for controlling the spread of the virus. This can be done through community outreach, public service announcements, and educational campaigns.
- Surveillance: Monitoring mosquito populations, testing mosquito pools for the presence of WNV, and tracking human cases of the virus are important for early detection and response to outbreaks.
- Vaccination: There is currently no vaccine available for humans, but there are vaccines for horses, which can be a reservoir for the virus.
- Blood safety: Screening of blood donations for WNV is important to prevent transmission through blood transfusions.
It’s important to note that prevention and control of WNV requires a coordinated effort between public health authorities, healthcare providers, and the public. By taking appropriate measures to reduce mosquito populations and avoid mosquito bites, we can help prevent the spread of West Nile Virus.
FAQ
What is West Nile Virus (WNV)?
WNV is a virus that is primarily spread to humans through the bite of infected mosquitoes.
What are the symptoms of West Nile Virus?
Most people who are infected with WNV will not experience any symptoms. However, some people may develop fever, headache, body aches, joint pains, vomiting, diarrhea, or rash. In rare cases, severe illness such as encephalitis or meningitis can occur.
How is West Nile Virus diagnosed?
Diagnosis of WNV is typically made through laboratory tests, such as testing for antibodies or viral RNA in the blood or cerebrospinal fluid.
Can West Nile Virus be treated?
There is no specific treatment for WNV, and most people recover on their own. Severe cases may require hospitalization and supportive care, such as intravenous fluids and respiratory support.
Who is at risk of getting West Nile Virus?
Anyone can get WNV, but people who spend time outdoors, especially during peak mosquito hours, are at higher risk. Older adults and people with weakened immune systems may be more susceptible to severe illness.
Can West Nile Virus be spread from person to person?
No, WNV is not typically spread from person to person. It is primarily spread through the bite of infected mosquitoes.
How can I protect myself from West Nile Virus?
You can protect yourself by wearing long-sleeved shirts and pants, using insect repellent, and avoiding outdoor activities during peak mosquito hours. You can also help reduce mosquito populations by eliminating standing water around your home.
Is there a vaccine for West Nile Virus?
Currently, there is no vaccine available for humans. However, there are vaccines for horses.
Can I still donate blood if I have had West Nile Virus?
People who have had WNV should wait at least 28 days before donating blood, according to the American Red Cross.
How common is West Nile Virus?
WNV occurs primarily in the summer and early fall in temperate regions, and its prevalence can vary from year to year. Since its introduction to the United States in 1999, there have been thousands of human cases reported each year.
References
- Clark MB, Schaefer TJ. West Nile Virus. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544246/
- Khan SA, Dutta P, Khan AM, Chowdhury P, Borah J, Doloi P, Mahanta J. West Nile virus infection, Assam, India. Emerg Infect Dis. 2011 May;17(5):947-8. doi: 10.3201/eid1705.100479. PMID: 21529426; PMCID: PMC3321754.
- Petersen, Lyle & Brault, Aaron & Nasci, Roger. (2013). West Nile Virus: Review of the Literature. JAMA : the journal of the American Medical Association. 310. 308-15. 10.1001/jama.2013.8042.
- Bai F, Thompson EA, Vig PJS, Leis AA. Current Understanding of West Nile Virus Clinical Manifestations, Immune Responses, Neuroinvasion, and Immunotherapeutic Implications. Pathogens. 2019; 8(4):193. https://doi.org/10.3390/pathogens8040193
- Valiakos, G., V., L., Touloudi, A., Papatsiros, V., Spyrou, V., Petrovska, L., & Billinis, C. (2013). West Nile Virus: Basic Principles, Replication Mechanism, Immune Response and Important Genetic Determinants of Virulence. InTech. doi: 10.5772/55198
- Martín-Acebes, Miguel & Saiz, Juan-Carlos. (2012). West Nile virus: A re-emerging pathogen revisited. World journal of virology. 1. 51-70. 10.5501/wjv.v1.i2.51.
- Martin, Marie-France & Nisole, Sébastien. (2020). West Nile Virus Restriction in Mosquito and Human Cells: A Virus under Confinement. Vaccines. 8. 256. 10.3390/vaccines8020256.
- https://www.vdci.net/vector-borne-diseases/west-nile-virus-education-and-mosquito-management-to-protect-public-health/
- https://www.health.ny.gov/diseases/west_nile_virus/fact_sheet.htm
- https://www.michigan.gov/emergingdiseases/home/west-nile
- https://dph.illinois.gov/topics-services/diseases-and-conditions/west-nile-virus.html
- https://doh.sd.gov/diseases/infectious/wnv/
- https://doh.sd.gov/diseases/infectious/wnv/
- https://www.nhs.uk/conditions/west-nile-virus/
- https://www.cdc.gov/westnile/index.html
- https://www.who.int/news-room/fact-sheets/detail/west-nile-virus
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/west-nile-virus
- https://www.cdc.gov/westnile/symptoms/index.html
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.