Viral Pathogenesis Definition
- Pathogenesis refers to the process by which infection by viruses causes illness. Thus, it is a description of the mechanism by which initial infection triggers the development of disease.
- The pathogenic mechanism is the implantation of the virus on the body’s location (the entry point) and then replication at that location, and then spreading through multiple locations (target organs) where infection or transmission of virus to the environment takes place.
- There are many aspects that influence the pathogenesis. A few of them are the virulence characteristics of the virus that is infecting.
- In order to spread disease it is necessary for the virus to overpower the inhibitory effects within the host, such as physical barriers, distance as well as host defences.
- The pathogenesis of viral infections is influenced by a variety of factors: (1) transmission of the virus, its entry and spread in the host (2) the tropism of the virus, (3) viral virulence, diseases mechanisms, (4) host factors and defense mechanisms for the host.
Mechanisms of Viral pathogenesis/pollution
- Infections caused by viruses must be established in the host cell in order to grow. To cause infections it is necessary for the virus to take over host factors and then be able to evade host immune responses to ensure efficient replication.
- The process of replication for viruses often requires intricate interactions between the host and virus which can cause negative impacts on the host which gives the virus pathogenicity.
Steps of Viral pathogenesis
There are many stages of Viral pathogenesis and infections, for instance;
- Primary transmission
- Entry to host
- Local replication and spread
- Dissemination and secondary replication
- Shedding and secondary transmission
Primary transmission
Three prerequisites must be met in order to ensure the successful infection of the host.
- First, there needs to be a sufficient amount of virus to trigger infection.
- The cells at the site of infection have to be accessible in the sense the sense that cell membranes have host-encoded receptors that viruses could exploit to gain entry into cells.
- The host defense system against viruses must not be effective or ineffective.
Entry to host
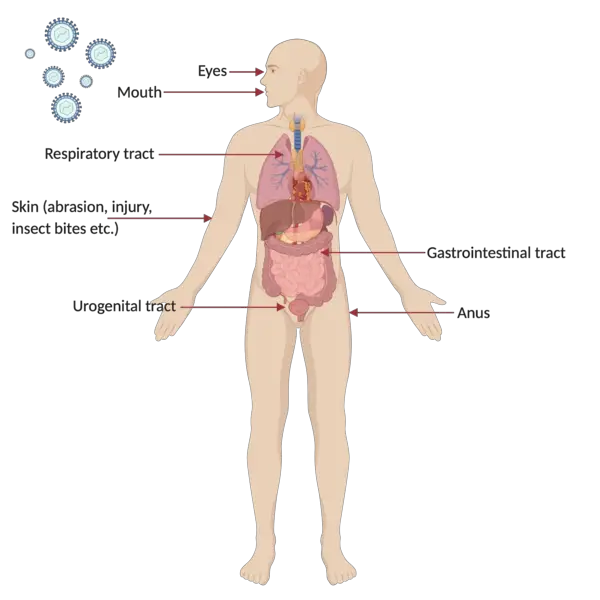
- Human-caused diseases caused by viruses usually get into the nose, mouth and genital tracts, or through damaged skin and genital tract, which is why cells of digestive, respiratory, skin and genital tissues are usually the main site of infection.
- Certain viruses can be capable of transmitting to the mammalian embryo through germ cells infected during the fertilization process or later in pregnancy through the placenta and an infection during birth.
Local replication and spread
- After its initial entry into the human host cell, virus takes over the host cell’s machinery and causes it to allow the process of viral amplification.
- The virus here must modify the host’s innate immune response in order to block the body from eliminating it while also facilitating its replication.
- The virus that is replicated from the initial infected cells then spreads to infect nearby cells, and possibly spreading to different types of cells such as leukocytes. This causes an infection that is localized where the virus is spread and then infects the surrounding cells at the point of entry. In other cases, the virus may get released in extracellular fluids.
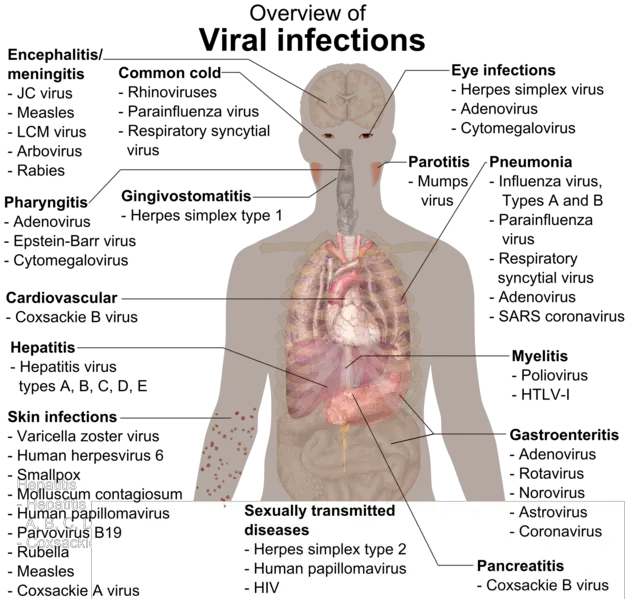
- Localised infections can include commonly-assisted cold (rhinovirus) and flu (parainfluenza) and gastrointestinal diseases (rotavirus) and skin conditions (papillomavirus).
Dissemination and secondary replication
- In some cases the virus may cause systemic illness through an infection that spreads all over the body.
- The most common method of transmission is via the lymphatic or blood system and includes the viruses that cause Chickenpox (varicella Zoster virus) as well as the smallpox (variola), HIV (human immunodeficiency virus).
- Certain viruses may be transmitted through the nervous system.
- In addition, poliovirus may be transmitted through the oral-fecal route, in which it first grows in the place of entry, which is the small intestine, and then spreads to lymph nodes in the region. The virus then disperses through bloodstreams into various organs of our body (e.g. the spleen, liver) and is followed by another cycle of replication and spread to the nervous system central, causing damage to motor neurons.
Shedding and secondary transmission
- In the end, the virus can spread to areas in which shedding into the surrounding environment is possible.
- The alimentary, respiratory and urogenital tracts as well as the blood are among the most frequently shed sites through bodily fluids aerosols, skin and excrement.
- The virus will later be passed on to another person and start the infection cycle over and over.
Factors affecting Viral pathogenesis
There are many factors that influence the Viral pathogenesis, such as:
- Virus tropism
- Virus factors
- Host factors
Virus tropism
- The term “virus tropism” refers to the preference of the virus’s host of replication in distinct kinds of cells in an organ.
- The majority of the time it can be determined through the capability of viral surface proteins to bind or fuse to the surface receptors of targeted cells to initiate an infection. This is why the binding specificity of viral surface proteins is the determinant of the tropism and destruction of specific cells, which is a key factor in the pathogenesis of viruses.
- But, co-receptors can be needed to facilitate the interaction of cell receptors in host cells with viral proteins to create the virus.
- For example, HIV-1 requires target cells to express co-receptors CCR5 or CXCR4 in addition to the CD4 receptor for the purpose of facilitating attachment of the virus. It is interesting to note that HIV-1 may undergo a tropism shift that allows the glycoprotein gp120 initially utilizes CCR5 (mainly for macrophages) as the primary co-receptor to enter cells of the host. In the following, HIV-1 is able to attach with CXCR4 (mainly in T cells) as the infection advances, as a result, it changes the viral pathogenicity to new stage.
- In addition to cellular receptors viral susceptibility can also be controlled by other intracellular factors for instance, the transcription factors that are specific to tissues. For instance, consider the JC polyomavirus where its activity is limited to glial cells as its enhancer only functions within glial cells. JC virus gene expression is dependent on host transcription factors which are expressed only within the glial cell.
- The capacity of organs and tissues to the virus can also affect the activity of tropism.
- Accessibility is influenced through physical obstacles, like those in enteroviruses. They reproduce in the intestine as they can resist digestion enzymes, bile along with acidic environment.
Virus factors
- The viral genetics that encode viral factors can determine the degree of pathogenesis triggered by viral infections. This is known as the degree of virulence. This can be used to evaluate the severity of pathology among the two viruses.
- In other words, the different virus strains that have different factors can result in various degrees of virulence which can then be utilized to study variations in the pathogenesis of virus variants that have different virulence.
- The factors that cause viruses are greatly dependent on viral genetics that is the virulence the determinant for structural proteins or non-structural proteins as well as non-coding sequences.
- In order for a virus to spread and cause disease to the body, it must to encode specific virus genes within its genome, which allow it to beat the preventive physical barriers and to modulate the immune system’s ability to block replication of the virus.
- When it comes to poliovirus the majority of vaccine strains within the oral vaccine for polio have attenuating point mutations within the 5 Untranslated Region (5 5′ UTR).
- However, the virus that causes polio doesn’t contain these five UTR point mutations and therefore exhibits greater pathogenicity for the virus in hosts.
- The viruses that are encoded in the genome are often responsible for controlling ways in which viruses spread, their routes of entry as well as transmission, shedding and entry.
- In polioviruses the attenuating mutations in the point are thought to trigger a replication and translation defect, which reduces the virus’s ability to cross-linking with host cells and reproduce within the nervous system.
- The virus has also created various immunomodulation strategies to thwart the immune response of the host. They typically encode decoy receptors, which target chemokines and cytokines in the immune response of the host or analogues to host cytokines. In this way viruses that can alter the immune response of host cells to the onset of infection to evade immune attack have a higher pathogenicity.
Host factors
- The pathogenesis of viruses is depended on the host. Certain viral infections have demonstrated various manifestations that range from asymptomatic to asymptomatic, or even critical illness, because on the host’s factors.
- Particularly, genetic factors such as age, immunocompetence and genetics are crucial in determining whether the virus is able to be controlled through the body of the patient.
- Mice with functional Mx genes produce an Mx1 protein that is able to effectively block the replication of influenza. Thus, mice with the non-functional Mx allele are unable to synthesize the Mx protein, and are more vulnerable to the infection.
- Additionally, individuals who are immunocompromised because of existing diseases may be suffering from a weak immune system that can make them more susceptible to being damaged by the virus.
- In addition, several viruses exhibit varying pathogenicity based upon the age and gender of their patient. Mumps, polio and Epstein-Barr virus are more serious diseases in adults, while others , like rotavirus, cause more serious infections in infants. This suggests that the immune system of the host and defense mechanisms could change in the aging process.
How do viral infections cause disease?
A viral infection doesn’t always lead to disease. A viral infection is simply replication of the virus within the host. However, diseases are the damage caused by the viral multiplicitation. Someone who has an infection with a virus but doesn’t display any symptoms of disease is referred to as a carrier.
Damage caused by the virus
- Once they are inside host cells viruses are able to destroy cells by different methods.
- The virus can cause direct cytopathic impacts that alter cell functions. It could be due to the release of enzymes that degrade metabolic precursors, or by releasing proteins that block the synthesis of essential host factors DNA, proteins, or the RNA.
- In particular, the herpes simplex virus’s viral proteins virus are able to be degrading host DNA, and also inhibit the replication of host cell DNA and transcription of mRNA.
- Poliovirus is able to inactivate proteins in host mRNA translation , but without impacting poliovirus’s mRNA transcription.
- In some instances, virus fusion protein expression at the surface of host cells may trigger host cells to fusion into multinucleated cells. Examples include measles viruses, HIV and respiratory syncytial viruses.
- It is important to note that viral infections can differ based on “lifestyle strategy”.
- Persistent infections are when cells are able to continue to exist in spite of a viral infection. They may be further classified into latent (only the genome of the virus exists, but there is no replication taking place) as well as persistent (basal level of viral replication that do not trigger any immune reaction).
- In acute illnesses, lytic viruses shed at high levels for rapid infiltration into an additional tissue or host, whereas persistent viruses shed at lower levels to prolong the duration in transmission (months up to years).
- Lytic viruses have the capability of killing host cells through infecting and/or interfering with special roles of cells in the host. One example is the induction of necrosis within host cells that are infected by the virus.
- In addition, the signs of viral infection, for instance HIV binding HIV on the co-receptors CCR5 or CXCR4 may cause the death of cells via the host signalling pathways by immune cells.
- But, many viruses contain proteins that regulate Apoptosis, depending on whether the condition is persistent or acute. Apoptosis-inducing factors, such as by interplay with caspases, can trigger the shedding of viral particles for viral lytic viruses, which facilitates transmission, while the inhibition of apoptosis can delay the development of virus in cells or allow the virus to be hidden within the system of immunity during persistent, chronic diseases.
- But, the an induction of apoptosis within major immune cells, or antigen-presenting cell can also function as an immunosuppressive mechanism in chronic infections such as HIV. The most common cause of immune suppression for HIV patients is the loss of CD4+ T-helper cells.
- It is interesting to note that adenovirus contains an E1A protein that induces an apoptosis process by starting the cell cycle. It also has an E1B protein that blocks the apoptotic pathway by inhibiting of the caspase interaction.
- Persistent virus can alter host cells to cancerous cells. The viruses such as Human papillomavirus (HPV) and the humans T lymphotropic virus (HTLV) among others, are able to cause tumor growth within infected hosts in two ways: either by disrupting the expression of genes that suppress tumours (HPV) or increasing the expression of proto-oncogenes (HTLV).
Damage caused by host immune system
- Sometimes instead the death of cells or cell dysfunction caused by viruses the host immune response may be able to control disease and inflammation.
- In the stimulation process, your adaptive and innate immune system to combat viral infections kills the infected cells. This could cause severe and serious pathological effects for the patient.
- The injury that is caused by immune systems are referred to as the virus-induced immunopathology.
- Particularly, the immunopathology is caused by an excessive release of interferons, antibodies and pro-inflammatory cytokines. It is also caused by the activation of the immune system or the overactivity of T cells that are cytotoxic.
- The release of interferons as well as other cytokines can cause cell damage, fever , and flu-like symptoms.
- In extreme cases of specific viral infections, such as the 2005 avian H5N1 flu an abnormal activation of the host’s immune response may trigger the release of cytokines in a manner called a cytokine storm.
- In certain instances an infection with a virus can trigger an autoimmune reaction, which is triggered by a variety of mechanisms, including molecular mimicry and the bystander mechanism.
- Molecular mimicry is the term used to describe the overlap in structural similarities between a viral antigen as well as self-antigen.
- The bystander mechanism is believed to be responsible for the development of a general and overreactive antiviral response to self-antigens involved in the process.
- The host because of autoimmunity was evident during this case of West Nile virus.
Incubation Period
- When there are many viral illnesses, there are no signs or symptoms of disease are observed during the phase of spread. This is why the incubation time (the period between exposure to the virus and the onset of disease) runs from the moment of implantation to the time of spreading, which ends with the time that virus replication within the targeted organs triggers illness.
- Sometimes mild malaise and fever occur in viremia. However, they are typically temporary and do not have any diagnostic value.
- The duration of incubation is typically be very brief (1 or 3 days) when the virus only travels a short distance to the desired organ (i.e. in cases where the cause of disease is caused by virus replication at the point that allows entry).
- However, incubation time for generalized infections tend to be longer due to the sequential manner that the virus travels throughout the body before getting to the organs of target.
- Other factors can affect the duration of incubation. Togaviruses that cause generalized infections could have an unexpectedly short incubation time due to an injecting (insect bite) of a rapidly growing virus.
- The mechanisms that govern the lengthy incubation time (months or several years) for persistent infection are not fully discovered. The cells that are infected for a long time usually not lysed or lysis may be delayed. Additionally, the disease could be the result of a late immune response to viral antigen (e.g. arenaviruses found in rodents) or from unidentified mechanisms of slow viral infections, during which there has been no immune response identified (as in the scrapie-kuru family) or from a mutation of the host’s genetic material, resulting in cell transformation as well as cancer.
References
- Baron S, Fons M, Albrecht T. Viral Pathogenesis. In: Baron S, editor. Medical Microbiology. 4th edition. Galveston (TX): University of Texas Medical Branch at Galveston; 1996. Chapter 45. Available from: https://www.ncbi.nlm.nih.gov/books/NBK8149/
- Heise M. T. (2014). Viral Pathogenesis. Reference Module in Biomedical Sciences, B978-0-12-801238-3.00079-9. https://doi.org/10.1016/B978-0-12-801238-3.00079-9
- https://virology-online.com/general/Pathogenesis.htm
- https://en.wikipedia.org/wiki/Viral_pathogenesis
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.