- In healthcare settings, Serratia marcescens is known to colonise and cause pathogenic illnesses.
- Serratia spp. (S. marcescens subsp. marcescens biogroup 1, Serratia liquefaciens, Serratia rubidaea, and Serratia odoriferous biogroups 1 and 2) are motile, slow lactose fermenters that are DNAse- and orthonitrophenyl galactoside (ONPG)– positive.
- In North America, Latin America, and Europe, Serratia spp. are the sixth most often isolated bacterium from paediatric patients.
- Transmission may be person-to-person, but medical devices such as urinary catheters, respirators, IV fluids, and other medical treatments are frequently involved.
- Additionally, Serratia species have been isolated from the respiratory system and wounds. The organism can survive in extremely hostile environmental conditions and is resistant to numerous disinfectants.
- The red pigment (prodigiosin or 2-methyl-3-amyl-6- methoxyprodigiosene) produced by S. marcescens is often the determining factor for identification, despite the fact that pigment-producing strains tend to be less virulent. From human infections, S. liquefaciens, S. odoriferous, and S. rubidaea have also been isolated.
- The presence of an inducible, chromosomal AmpC beta-lactamase confers resistance to ampicillin and first-generation cephalosporins in Serratia spp.
- In addition, some strains have plasmid-encoded resistance to other cephalosporins, penicillins, carbapenems, and aminoglycosides.
Classification of Serratia marcescens
- Serratia marcescens, once considered a harmless saprophyte, is now recognised as a significant opportunistic pathogen with a predisposition for healthcare-associated illness and antibiotic resistance.
- Serratia marcescens belongs to the genus Serratia, which is a member of the Enterobacteriaceae family. Currently, fourteen species of the genus Serratia are identified, eight of which are involved with human illness.
- The most well-known of the eight species implicated in clinical infection are S. marcescens, S. liquefaciens, and S. odorifera.
- S. marcescens is the most prevalent clinical isolate and the most significant human pathogen among all Serratia species.
Habitat of Serratia marcescens
- Serratia marcescens is present in fresh, stagnant, or saline water, as well as in soil, plants, insects, and animals, including humans.
- It has a recognised pathogenicity for non-plant life that is made even more powerful by its multi-antibiotic resistance.
- S. marcescens is capable of surviving in biological and non-biological conditions and has caused innumerable outbreaks worldwide.
- From contaminated water supplies to the transmission of a single bacterium in intensive care units, the capacity of this bacterium to proliferate in less-than-ideal conditions and its resistance to treatment make a Serratia infection potentially lethal.
- From the soil to the crop to the plate, or from the healthcare worker to the wound to the connective tissues of the central nervous system, extremely motile Serratia bacteria are poised to take advantage of every chance and colonise inside living organisms.
- Early in the 19th century, a single-celled organism was identified as the origin of reddened polenta made in an Italian village. However, evidence from the fourth century A.D. recalls the phenomenon of “blood bread.” This red hue in particular food varieties was frequently attributed with either heavenly or demonic involvement.
- A Bohemian priest celebrated mass in Bolsena in 1263. As he bent over the holy wafer, the altar appeared to be stained with blood. Since then, the Mass of Bolsena has been held, unknowingly applauding the strength of a bacterium.
- Around 550 years later, while Italian locals believed this colour shift was due to diabolical activities, scientists determined the perpetrator was less magical and concluded that the bloody polenta was caused by fungi. This putative fungus was given the name Serratia marcescens.
Serratia Marcescens Taxonomy

- The taxonomy of Serratia marcescens remained a mystery until the late 20th century. The initial scientific studies referred to it as a fungus without a stem. Researchers later concluded that it was yeast or mould.
- This resulted in many names for a single bacterial species, which complicated its study and delayed its ultimate nomenclature until the 1960s.
- S. marcescens is currently recognised as a member of the Enterobacteriaceae family and a bacterium that, along with other members of the Serratia genus, frequently produces the red pigment prodigiosin.
- Not all pathogenic strains of Serratia create this red colouring, it should be noted.
- Serratia marcescens is an exceptionally motile gram-negative, facultatively anaerobic, rod-shaped bacteria. As seen below, a S. marcescens gramme stain reveals small, pink-colored specks.
- Rod-shaped bacteria, bacilliform bacteria, or bacilli are terms used to characterise Serratia marcescens’ usual shape.
- This microbe is facultatively anaerobic, meaning it can grow in the presence or lack of oxygen, greatly enhancing its chances of survival in a variety of physiological systems.
- In addition, S. marcescens may thrive in a broad range of temperatures and pH values, from extremely acidic to neutral.
- All of the extracellular enzymes produced by Serratia bacteria, including AmpC type -lactamases, elastase, gelatinase, lecithinase, alkaline protease, and caseinase, improve bacterial resistance to antimicrobial therapy.
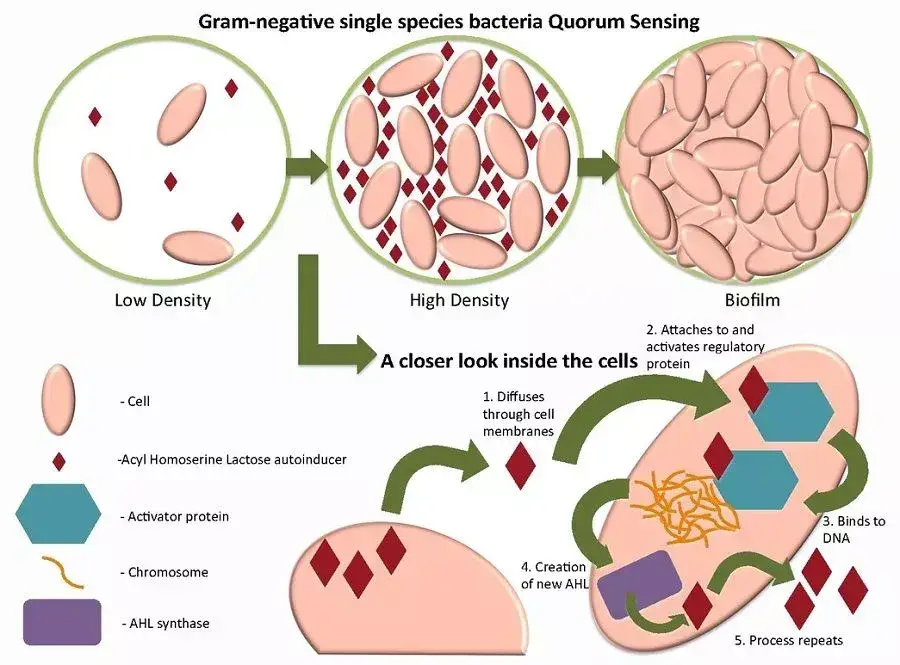
- All S. marcescens drug resistance factor (R-factor) characteristics within a single bacteria can be transmitted to entire populations by means of quorum sensing, a type of cell signalling; it is also known that drug resistance in S. marcescens is significantly more prevalent than in other Enterobacteriaceae. Furthermore, R-factors can be transferred between various strains of these bacteria.
- The dispersal stage of biofilm production transfers numerous motile S. marcescens bacteria to other parts of the body, where they might infect others by coughing, sneezing, or excretion; however, healthcare worker hands are the most usually reported mechanism of transmission.
- When the thickness of a S. marcescens biofilm reaches a specific height, it flakes off regularly.
- This practically automated method permits the rapid formation of many infection sites. In combination with resistance characteristics, this makes a S. marcescens infection in a severely ill hospital patient potentially lethal.
Serratia Marcescens as a Tracer Organism
- Prior to the discovery of its pathogenicity, Serratia marcescens was utilised for many years as a tracer organism.
- S. marcescens’ unique red colouring made it possible to study the mechanics of bacterial infection via the mouth and gastrointestinal tract during the First World War, when controlled medical experiments were frequently conducted on soldiers.
- For instance, medical researchers would apply S. marcescens to the gums prior to dental surgery to determine whether bacteria could reach the bloodstream.
- Most notably, the U.S. military utilised Serratia marcescens to demonstrate the potential effects of biological warfare by releasing huge quantities of the organism into subway systems, government and military institutions, and metropolitan populations.
- This resulted in infection and a small number of deaths attributable to S. marcescens infection. In the late 1960s, press coverage of the subsequent court proceedings reached global audiences.
Serratia Marcescens Symptoms
- Serratia marcescens causes a variety of symptoms in humans, although it is most usually related with nosocomial infections, such as catheter-associated bacteremia and respiratory, urinary, and wound infections. In children, infections are typically restricted to the digestive system.
- Symptoms of S. marcescens depend on the localization and spread of the infection.
- If an infected hand comes into contact with the eye and natural immunity is inadequate to prevent Serratia colonisation, conjunctivitis, keratitis, or tear duct infections may ensue.
- Serratia bacteria can cause endocarditis, bacteremia, meningitis, osteomyelitis, and arthritis once they have entered the bloodstream.
- Treatment for Serratia marcescens is restricted to the medications cefotaxime and gentamicin. If Serratia strains gain resistance to these medications, there are very few remaining treatment choices.
Serratia Marcescens as a Cancer Therapy?
- Prodigiosin extracted from S. marcescens strains has been proven to be harmful to malignant cells but much less so to healthy cells.
- As a result, prodigiosin is currently being researched as a natural cancer treatment.
- Even for healthy cells, cell toxicity has long been an issue in the development of anticancer treatments.
- Microorganism metabolites, such as prodigiosin, the pigment responsible for the red hue of S. marcescens colonies, disrupt some cancer cell signalling pathways, resulting in the early death of cancer cells; however, the precise mechanism of action remains unknown.
- Prodigiosin has demonstrated anticancer activity in tests of breast cancer, prostate cancer, and choriocarcinoma, however all of these research have been conducted in the laboratory.
- This area of inquiry, known as bacteria-mediated cancer therapy or BMCT, is gaining popularity as a research topic in the pharmaceutical sector.
Morphology of Serratia marcescens
- Microscopically, S. marcescens is a bacillus with rounded ends measuring between 0.5 m and 0.8 m in width and 0.9 m and 2.0 m in length. Peritrichous flagella are normally in motion and are present.
- At 24 hours of incubation at 37°C, S. marcescens colonies measure between 1.5 and 2.0 mm in size, are opaque, frequently have a reddish or pink colour due to pigment formation, and have a unique odour (similar to urine) due to the generation of ammonia or trimethylamine. Certain strains produce colonies that are typically white or grey and lack pigmentation.
Virulence Factors of Serratia marcescens
Hemolysin production
- Hemolysin (ShlA), which is cytotoxic to fibroblasts, epithelial cells, and red blood cells, has been identified as S. marcescens’ key virulence factor.
- ShIA facilitates the generation of leukotriene and histamine, which enhances vascular permeability and contributes to granulocyte buildup, edoema formation, and other symptoms associated with bacterial infections.
- The ShlB protein regulates ShlA export (belonging to the Omp85 subfamily).
Lipopolysaccharide
- LPS, which is a component of the outer membrane of gram-negative bacteria, mediates the biological activity of endotoxin.
- LPS O-polysaccharides may boost the pathogenicity of a bacteria by increasing its resistance to serum-mediated lysis. It shields the cell from hazardous chemicals by delaying their penetration and blocking their access to the target spot.
- Since S. marcescens contains more than 24 somatic antigens, its LPS structure is varied.
Extracellular products
- S. marcescens is one of the most effective organisms for the biological breakdown of chitin, as it produces many extracellular enzymes. Biotechnology is interested in chitinolytic enzymes because its substrate, chitin, is a major structural component of bacterial cell walls.
- Thus, chitinolytic enzymes may, in theory, be used as natural antifungal agents by, for instance, expressing their genes in agricultural plants or in bacteria utilised in fermentation processes susceptible to fungal attack.
Serratia marcescens Pathogenesis
S. marcescens, an emerging multidrug-resistant organism, has the potential to manifest in a number of clinical manifestations. As a prominent nosocomial pathogen that mostly affects intensive care unit patients, its worrying growth in antimicrobial resistance has made it a top priority for the development of new antibiotics. This Enterobacterium possesses many virulence characteristics that allow it to colonise and survive on surfaces, including catheters and medical devices, elude the immune system, and rapidly develop antibiotic resistance.
1. Attachment/adherence
- Piliation has been shown to alter microbial adhesion to host epithelial surfaces. S. marcescens possesses pili, attaches to uroepithelial cells, and is responsible for nosocomial UTI.
- It has been suggested that there are two groups of adhesins. Mannose-sensitive (MS) pili agglutinate guinea pig and chicken erythrocytes in the presence of D-mannose, whereas mannose-resistant (MR) pili agglutinate chicken erythrocytes in the presence of D-mannose.
- A S. marcescens strain US46 urinary tract isolation appeared to exhibit both Ml2 and MS pili. According to this study, MS-piliated bacteria trigger PMNLs to generate active oxygen radicals that induce tissue damage in the infected organ.
2. Biofilm formation
- Biofilms are formed when bacteria cluster and attach to a surface. When they are gathered together, quorum sensing enables them to communicate with one another.
- Biofilm production is a multicellular phenomenon that allows bacteria to thrive in harsh settings and be resistant to several antimicrobial agents.
- S. marcescens biofilm development involves five stages: initial adhesion to a surface, exopolysaccharide synthesis, construction of the initial structure of the biofilm, maturation, and cell dispersal. Chronic infections are facilitated by the development of biofilms.
Lab Diagnosis of Serratia marcescens
- Serratia species are Gram-negative, rod-shaped bacteria.
- S. marcescens cultivates effectively on blood agar and MacConkey agar. It is lactose-free fermentation. At room temperature, several bacteria develop a red pigment on nutritional agar, tryptic soy agar, and MacConkey agar.
- Identification: Biochemical tests separate them from other coliforms.
.
| Name of the test | Result |
| Urease test | varies according to bacterial strains. |
| Voges-Proskauer test | Positive |
| ONPG test | Positive |
| Lactose fermentation | varies according to bacterial strains. |
| Mannitol fermentation | Positive |
| Glucose fermentation | Positive |
| Sucrose fermentation | Positive |
| Oxidase test | Negative |
| Citrate test | Positive |
| Motility | Positive |
| Indole test | Negative |
| Lysine decarboxylase | Positive |
| TSI/KIA medium* | Acid or Alkali/Acid, gas (-), H2S (-) * |
Treatment of Serratia marcescens
- S. marcescens possesses inherent resistance to penicillin, first- and second-generation cephalosporins, macrolides, tetracycline, nitrofurantoin, and colistin.
- Fluoroquinolones (gyrA mutations), aminoglycosides (plasmid-mediated aminoglycoside modifying enzymes and 16S methyltransferase enzymes) (Multidrug resistance mechanisms: extended spectrum beta lactamases (ESBLs), ampC beta lactamase, carbapenemases.
Biochemical Characteristics of Serratia marcescens
| Test | Result |
|---|---|
| Gram stain | − |
| Oxidase | − |
| Indole production | − |
| Methyl Red | > 70% − |
| Voges-Proskaeur | + |
| Citrate (Simmons) | + |
| Hydrogen sulfide production | − |
| Urea hydrolysis | > 70% − |
| Phenylalanine deaminase | − |
| Lysine decarboxylase | + |
| Motility | + |
| Gelatin hydrolysis, 22 °C | + |
| Acid from lactose | − |
| Acid from glucose | + |
| Acid from maltose | + |
| Acid from mannitol | + |
| Acid from sucrose | + |
| Nitrate reduction | + (to nitrite) |
| Deoxyribonuclease, 25 °C | + |
| Lipase | + |
| Pigment | some biovars produce red |
| Catalase production (24h) | + |
References
- Hejazi A, Falkiner FR. Serratia marcescens. J Med Microbiol. 1997 Nov;46(11):903-12. doi: 10.1099/00222615-46-11-903. PMID: 9368530.
- Dipankar Paul, Indrani Bhattacharyya, Mandira Chakraborty, Palash Das, Sangita Das Ghosh. “A Red Alert! Nosocomial Infection by Serratia Marcescens”. Journal of Evolution of Medical and Dental Sciences 2014; Vol. 3, Issue 49, October 02; Page: 11766-11770, DOI: 10.14260/jemds/2014/3546
- Pinna A, Usai D, Sechi LA, Carta A, Zanetti S. Detection of virulence factors in Serratia strains isolated from contact lens-associated corneal ulcers. Acta Ophthalmol. 2011 Jun;89(4):382-7. doi: 10.1111/j.1755-3768.2009.01689.x. Epub 2009 Oct 20. PMID: 19845561.
- Su LH, Ou JT, Leu HS, Chiang PC, Chiu YP, Chia JH, Kuo AJ, Chiu CH, Chu C, Wu TL, Sun CF, Riley TV, Chang BJ; Infection Control Group. Extended epidemic of nosocomial urinary tract infections caused by Serratia marcescens. J Clin Microbiol. 2003 Oct;41(10):4726-32. doi: 10.1128/JCM.41.10.4726-4732.2003. PMID: 14532211; PMCID: PMC254321.
- http://www.antimicrobe.org/b26.asp#:~:text=CLINICAL%20MANIFESTATIONS,meningitis%20(72%2C%2074)
- https://microbenotes.com/serratia-marcescens-an-overview/
- https://www.pathologyoutlines.com/topic/microbiologyserratiaspecies.html
- https://www.slideshare.net/doctorrao/serratia-marcescens