Plasmodium parasite is considered the oldest known parasite in the world. In 1880, Charles Louis Alphonse Laveran first described the presence of Plasmodium parasites in the blood of malaria patients.
In the beginning, Charles Louis Alphonse Laveran called it Oscillaria malariae. Later two zoologists Ettore Marchiafava and Angelo Celli term this parasite as a member of a new genus, called Plasmodium, In 1885.
In 1886, Camillo Golgi first noticed that there are different Plasmodium parasites which are responsible for different nakarua diseases.
Later two distinct human malaria species were identified by Giovanni Batista Grassi and Raimondo Filetti. They named it Plasmodium vivax and Plasmodium malariae.
Plasmodium Classification
| Domain: | Eukaryota |
| (unranked): | Diaphoretickes |
| Clade: | TSAR |
| Clade: | SAR |
| Infrakingdom: | Alveolata |
| Phylum: | Apicomplexa |
| Class: | Aconoidasida |
| Order: | Haemospororida |
| Genus: | Plasmodium |
| Family: | Plasmodiidae |
What is Plasmodium vivax? – Plasmodium Definition
Plasmodium is also known as the malaria parasite and is the genus of intracellular parasitic protozoa. They are digenetic parasites because Plasmodium are obligate parasites of insects (such as mosquitoes) and vertebrates.
The term “malaria” originated from two Italian words; “mal” which means bad, and “aria” means air.
The plasmodium parasite does not affect the infected mosquito (nor does it die from malaria). Because they don’t have red blood like others, where the parasites develop and thrive.
Plasmodium Morphology
Plasmodium Falciparum
Plasmodium Falciparum is considered as the most virulent species among the all human malaria parasites. P. Falciparum causes severe malaria (malignant malaria) with the development of irregular paroxysms and high fever and may cause death if not treated.
The diagnostic form or stage determines the morphological characteristics of Plasmodium Falciparum.
1. The Ring Form
- Inside the erythrocytes the ring form of Plasmodium Falciparum is found.
- It is called ring form because it looks like a ring. It contains nucleus, cytoplasm and a central vacuole.
- The diameter of ring form is one fifth of erythrocytes and the ring form is very thin and thus delicate.
- It contains 1 – 2 chromatins.
2. Trophozoites
- The size of Trophozoites ranges between between 1.25 and 1.5um.
- They contain a thin cytoplasm with a signet ring shape.
- Trophozoites are vacuolated and have a single nucleus.
3. Schizonts
- Schizonts are 4.5 to 5 um in diameter.
- They capture 2-3 of a red cell.
- They have 2 or 4 merozoites and a pigment which forms dark color during staining. A mature Schizonts contains about 30 merozoites.
4. Gametocytes
- Gametocytes are crescent shaped (banana-shape) and are considered as the sexual forms of the parasite.
- The advantage of the sexual forms is the parasite contains both male and female forms which have a size about one and a half of a normal red cell.
- They are infectious to mosquitoes.
5. Sporozoites
- They are infectious to humans.
- Sporozoites are 10 to 15 um in length
- They contain a thick pellicle, a mitochondrion, a single nucleus.
- They can move which is possible by the peripheral fibers.
- The pellicle contains double-membrane and also has an additional layer made of subpellicular microtubules.
Plasmodium Vivax
1. Ring form
- It has a signet ring shape.
- Plasmodium Vivax contains a large cytoplasm with a large chromatin.
- After maturation they form an amoeboid shape.
- The size of Ring form is a third the diameter of red cells.
2. Trophozoites
- They appear as a few dots of large chromatin with amoeboid cytoplasm as well as fine pigments (hematin) that are yellowish-brown in color.
3. Gametocytes
- These are round and oval in shape.
- They contain high amounts of brown pigments which are scattered within the infected red cells.
4. Schizonts
- They contain 12 to 24 merozoites and are large enough to fill the entire cell erythrocyte.
- Schizonts also contain a yellowish-brown pigment.
Plasmodium Ovale
1. Ring form
- They appear as one or two large chromatin dots as well as a sturdy/thick cytoplasm.
- The Schuffner’s dots are formed when they are matured.
2. Trophozoites
- The trophozoite’s cytoplasm is sturdy with a few chromatin dots.
- They are irregular in shape and some of them appear to be more compact.
3. Gametocytes
- These are round or oval in shape and large enough to fill the whole erythrocyte cell.
- They also contain brown pigment.
4. Schizonts
- They contain about 6 to 14 merozoites.
- Schizonts has a mass of dark-brown pigment which is covered by large nuclei.
Plasmodium Characteristics
- They are unicellular eukaryotes.
- Plasmodium are obligate parasites of vertebrates and insects.
- They are responsible for human malaria disease.
- They are considered the most researched genera of parasites.
- The Plasmodium parasite is mainly found in tropic and subtropic areas.
- Plasmodium falciparum, Plasmodium ovale, Plasmodium vivax, and Plasmodium malariae are responsible for human malaria.
- They use Anopheline mosquito as a vector.
- The symptoms of malaria disease are sometimes unnoticed or misdiagnosed; clinical signs include fever, chills, weakness, headache, vomiting, diarrhea, anemia, pulmonary and renal dysfunction, neurologic changes.
Plasmodium Genome
- The complete genome sequencing of Plasmodium falciparum showed us that it contains 14 chromosomes and 5,300 genes. These genomes are responsible for dodging the host’s immunities
- Plasmodium falciparum is considered the most common form of Plasmodium which is responsible for human malaria.
- The average gene density is approximately 1 gene/4,338 base pairs.
Plasmodium Host
Plasmodium requires two host cells to complete their life cycle. They complete their asexual cycle within human body and the sexual cycle is within the female anopheline mosquito.
The female Anopheles mosquito is the definitive or primary host of Plasmodium whereas the human body is the intermediate or secondary host.
Except human plasmodium infects other hosts such as Monkeys (P. knowlesi and P. coatneyi),
Chickens (P. juxtanucleare), Pigeon (P. relictum), Snakes (P. wenyoni), Canaries (P. cathemerium).
Plasmodium Species
Plasmodium is the largest member of the order Haemosporidia. There are about 250 species within this genus. All of them are responsible for malaria disease in different vertebrates.
About 29 species cause infection in non-human primates; rodents outside the tropical parts of Africa are rarely affected. Bats, porcupines, and squirrels; carnivores, insectivores, and marsupials are infected by few known species.
Here is the name of few Plasmodium Species;
| Plasmodium accipiteris | Plasmodium achiotense | Plasmodium achromaticum |
| Plasmodium caprae | Plasmodium capistrani | Plasmodium caloti |
| Plasmodium buteonis | Plasmodium bubalis | Plasmodium bucki |
| Plasmodium brygooi | Plasmodium brumpti | Plasmodium brasilianum |
| Plasmodium brodeni | Plasmodium bouillize | Plasmodium booliati |
| Plasmodium blacklocki | Plasmodium biziurae | Plasmodium bioccai |
| Plasmodium bigueti | Plasmodium bertii | Plasmodium beltrani |
| Plasmodium beebei | Plasmodium beaucournui | Plasmodium basilisci |
| Plasmodium bambusicolai | Plasmodium billcollinsi | Plasmodium azurophilum |
| Plasmodium balli | Plasmodium billbrayi | Plasmodium attenuatum |
Plasmodium Cell Structure
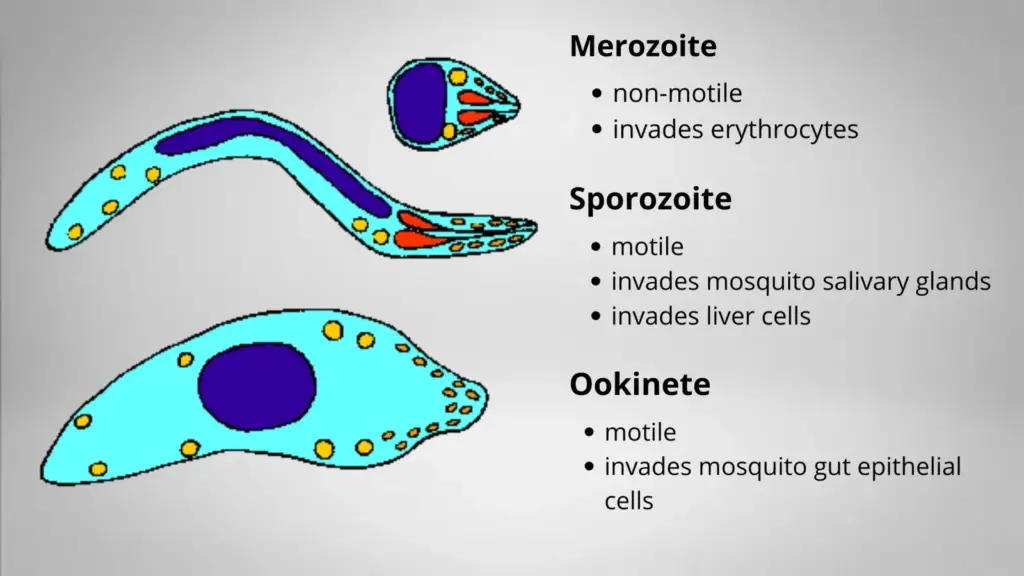
In some ways, all the species of plasmodium differ from each other. They show the same life cycle. Anopheles mosquito injects the sporozoites with the saliva when they bite a human.
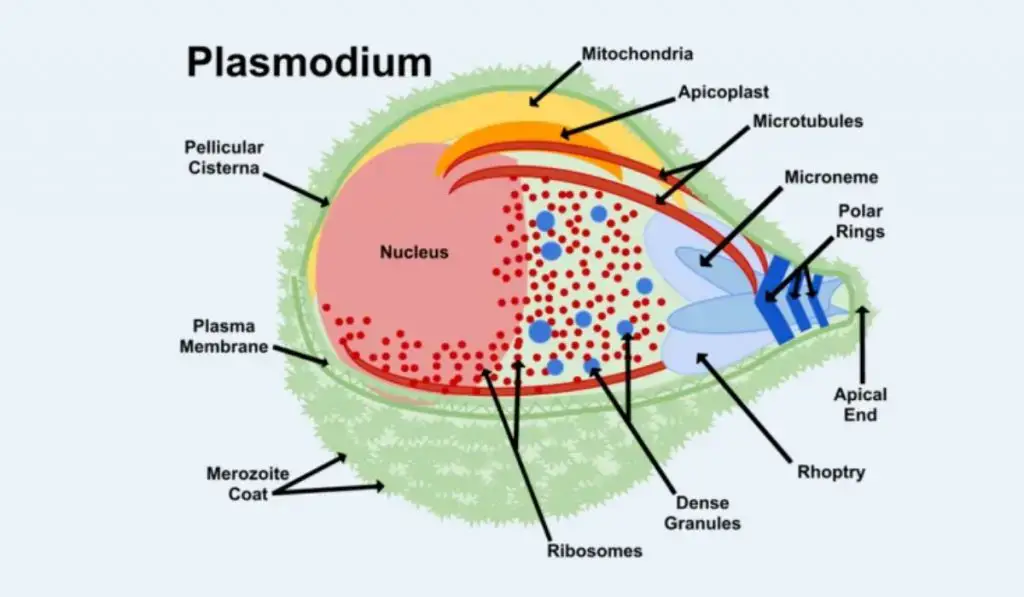
- The size of this sporozoite is about 10 -15 µm in length and 1 µm in diameter.
- The sporozoites contain a thin outer membrane.
- The subpellicular microtubules lie below the inner membrane.
- The membrane contains 3 polar rings and the rhoptries are long, extending half the length of the body.
- The micronemes, convoluted elongate bodies, move forward to the anterior of the sporozoite entering a common duct with the rhoptries.
- The posterior end contains the Mitochondria.
- The sporozoites use the apical organelles to invade the liver cells when they enter the circulatory system.
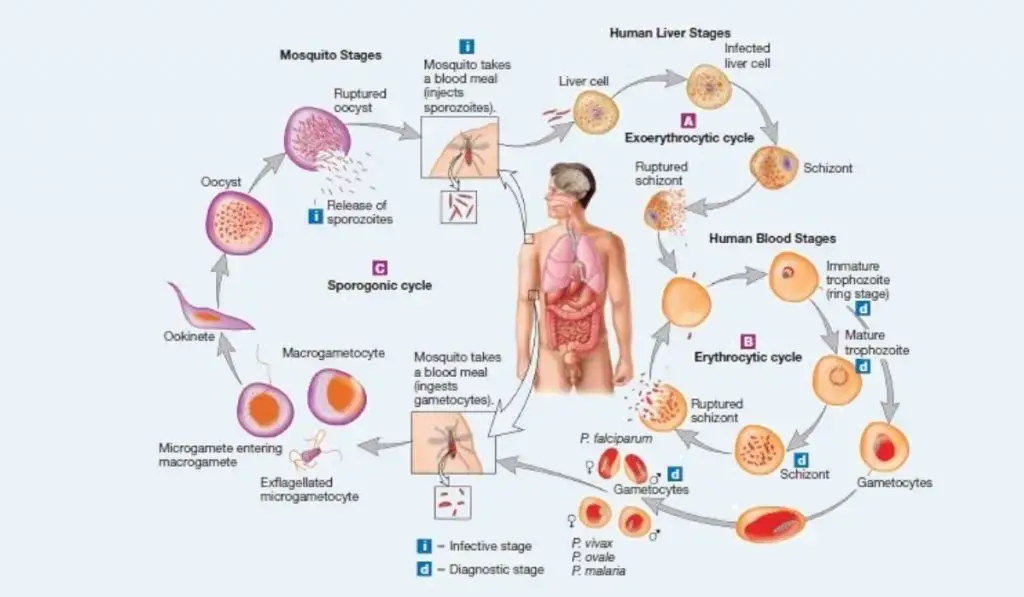
Plasmodium life cycle
Five species of Plasmodium are responsible for human malaria such as: P. falciparum, P. malariae, P. vivax, P. knowlesi, and P. ovale.
The plasmodium parasite is transferred through the female Anopheles mosquito. When an infected female Anopheles mosquito bites a human it injects the parasite inside the bloodstream.
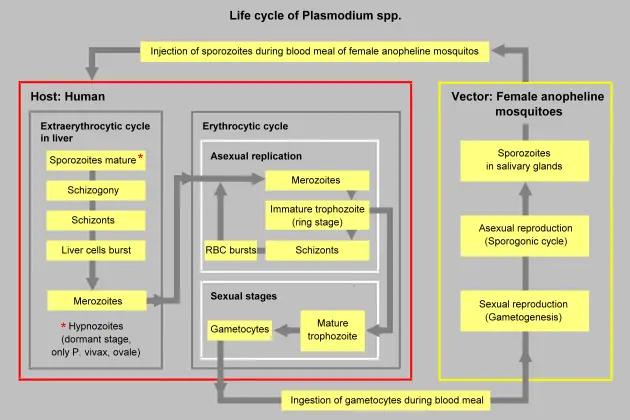
- During male, the mosquito injects the small haploid sporozoites with saliva within the bloodstream.
- Then the sporozoite immediately enters into the hepatic cells of the liver from the bloodstream.
- There they produce merozoites by undergoing multiple asexual fission (schizogony).
- Then the merozoites are attached and penetrate inside the erythrocytes, after being released from the hepatocytes.
- After that, the plasmodial cell started to enlarge as a mononucleate cell known as a trophozoite.
- The nucleus of trophozoite is divided and produces schizont, which contains 6 to 10 nuclei.
- Then mononucleated merozoites are produced with the division of schizont.
- These merozoites are released when the infected erythrocytes are lysed. After that these merozoites infect other erythrocytes.
- This erythrocytic stage is cyclic and repeats approximately every 48 to 72 hours or longer, depending on the species of Plasmodium involved.
- Then the symptoms of malaria disease such as chills, fever, and sweats are developed when the merozoites, toxins, and erythrocyte debris are released into the bloodstream.
- Occasionally, macrogametocytes and microgametocytes are developed with the differentiation of merozoites. They do not rupture the erythrocyte.
- When these are ingested by a mosquito during a blood meal, they develop into female and male gametes, respectively.
- The erythrocytes are lysed and the gametes fuse to develop a diploid zygote known as the ookinete. The formation of ookinete is performed within the mosquito’s gut.
- Then the ookinete gets attached and penetrates the mosquito’s gut wall to form an oocyst.
- After that, the sporozoites are formed when the oocysts undergo meiosis. This process is known as sporogony. Then the sporozoites are Migrate to the salivary glands of the mosquito.
- The cycle will repeat again when the mosquito bites another human host.
Genome of Plasmodium
- The genome of four Plasmodium species have been sequenced such as Plasmodium falciparum, Plasmodium knowlesi, Plasmodium vivax, and Plasmodium yoelli. All of these species contain 14 chromosomes and genomes of about 25 megabases results consistent with earlier estimates.
- The chromosomes whose length is known to vary from 500 kilobases to 3.5 megabases in length. It is considered that this is the pattern everywhere the genus.
- The typical chromosome fraction of Leukcytozoon has not yet been confirmed.
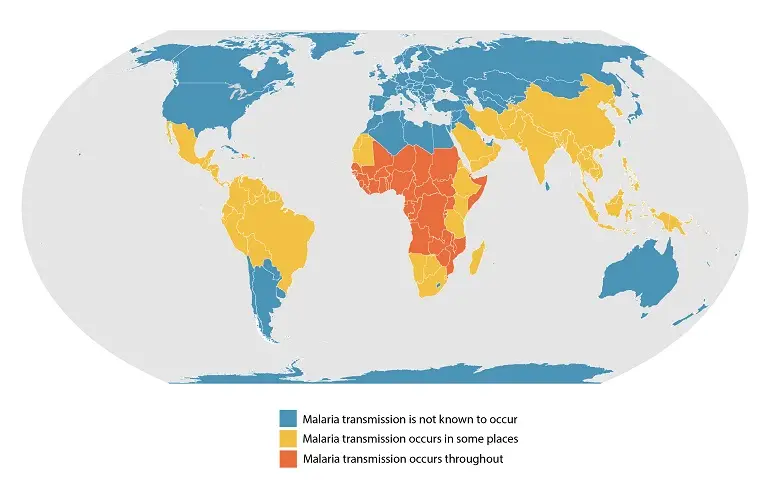
Occurrence Malaria
- There are several environmental factors which influence the occurrence of Malaria worldwide, such as temperature, humidity, and rainfall.
- Malaria is mainly spread in tropical and subtropical areas, where, the vector of malaria or Anopheles mosquitoes can survive and multiply, and most importantly where malaria parasites can complete their growth cycle in the mosquitoes (“extrinsic incubation period”).
- Temperature play an important role in the occurrence of malaria, because Plasmodium falciparum can not complete its growth cycle within Anopheles mosquito at temperatures below 20°C (68°F), and thus cannot be transmitted.
- There are several tropical and subtropical areas where the transmission of malaria does not occur. The transmission will not occur if the following criteria are founds;
- At very high altitudes;
- During colder seasons in some areas;
- In deserts (excluding the oases); and
- In some countries where transmission has been interrupted through successful control/elimination programs.
- Generally, in warmer regions closer to the equator:
- Transmission will be more intense
- Malaria is transmitted year-round
- P. falciparum predominates.
- The highest transmission is found in Africa South of the Sahara.
- At low temperatures, the transmission of malaria will be less intense and more seasonal.
Classification of malaria disease
| Name | Pathogens | Properties |
|---|---|---|
| algid malaria | Plasmodium falciparum | severe malaria affecting the cardiovascular system and causing chills and circulatory shock |
| bilious malaria | Plasmodium falciparum | severe malaria affecting the liver and causing vomiting and jaundice |
| cerebral malaria | Plasmodium falciparum | severe malaria affecting the cerebrum |
| congenital malaria | various plasmodia | plasmodium introduced from the mother via the fetal circulation |
| falciparum malaria, Plasmodium falciparum malaria, pernicious malaria | Plasmodium falciparum | |
| ovale malaria, Plasmodium ovale malaria | Plasmodium ovale | |
| quartan malaria, malariae malaria, Plasmodium malariae malaria | Plasmodium malariae | paroxysms every fourth day (quartan), counting the day of occurrence as the first day |
| quotidian malaria | Plasmodium falciparum, Plasmodium vivax, Plasmodium knowlesi | paroxysms daily (quotidian) |
| tertian malaria | Plasmodium falciparum, Plasmodium ovale, Plasmodium vivax | paroxysms every third day (tertian), counting the day of occurrence as the first |
| transfusion malaria | various plasmodia | plasmodium introduced by blood transfusion, needle sharing, or needlestick injury |
| vivax malaria, Plasmodium vivax malaria | Plasmodium vivax |
| transfusion malaria | various plasmodia | plasmodium introduced by blood transfusion, needle sharing, or needlestick injury |
| tertian malaria | Plasmodium falciparum, Plasmodium ovale, Plasmodium vivax | paroxysms every third day (tertian), counting the day of occurrence as the first |
| quotidian malaria | Plasmodium falciparum, Plasmodium vivax, Plasmodium knowlesi | paroxysms daily (quotidian) |
| quartan malaria, malariae malaria, Plasmodium malariae malaria | Plasmodium malariae | paroxysms every fourth day (quartan), counting the day of occurrence as the first day |
| ovale malaria, Plasmodium ovale malaria | Plasmodium ovale | |
| falciparum malaria, Plasmodium falciparum malaria, pernicious malaria | Plasmodium falciparum | |
| congenital malaria | various plasmodia | plasmodium introduced from the mother via the fetal circulation |
| cerebral malaria | Plasmodium falciparum | severe malaria affecting the cerebrum |
| bilious malaria | Plasmodium falciparum | severe malaria affecting the liver and causing vomiting and jaundice |
| algid malaria | Plasmodium falciparum | severe malaria affecting the cardiovascular system and causing chills and circulatory shock |
Plasmodium Disease/ Malaria Disease
About 40% of the world population lives in endemic areas. The emerging case of malaria per year is about 3-500 million. About 1.5 to 2.7 million peoples are died due to malaria per year. There are two important problems that are re-emerging the disease such as resurgence in some areas, and drug resistance which increasing mortality.
Plasmodium parasite is responsible for the Malaria disease. There are different species of Plasmodium which are responsible for malaria in different hosts such as P. vivax, P. falciparum, P. ovale and P. malariae, P. knowlesi.
Symptoms of Malaria
Symptoms of malaria develop within 10 days to 4 weeks. The common symptoms include shaking chills that can range from moderate to severe,
- high fever
- profuse sweating
- headache
- nausea,
- vomiting,
- abdominal pain,
- diarrhea, anemia,
- muscle pain,
- convulsions,
- coma,
- bloody stools.
A malaria disease will be called “severe” if it meets the following criteria, otherwise, it is considered uncomplicated.
- Decreased consciousness
- Significant weakness such that the person is unable to walk
- Inability to feed
- Two or more convulsions
- Low blood pressure (less than 70 mmHg in adults and 50 mmHg in children)
- Breathing problems
- Circulatory shock
- Kidney failure or haemoglobin in the urine
- Bleeding problems, or hemoglobin less than 50 g/L (5 g/dL)
- Pulmonary oedema
- Blood glucose less than 2.2 mmol/L (40 mg/dL)
- Acidosis or lactate levels of greater than 5 mmol/L
- A parasite level in the blood of greater than 100,000 per microlitre (µL) in low-intensity transmission areas, or 250,000 per µL in high-intensity transmission areas
Different Phases of malaria infection
Pre-erythrocyte schizogony
- This phase of malaria infection occurs when the infective form of the parasite, sporozoites enters the skin by the Anopheles mosquito.
- During this phase, no symptoms appear within the patient and the patient is not infective.
- Those Sporozites are not eliminated by the body’s defense mechanism, these are migrated to the liver and undergo development.
- After a changeable period, the micromerozoites are released. Sporozoites of P. vivax and P. ovale may remain in the liver in the form of hypnozoites
Erythrocytic schizogony
- During this step, the micromerozoites infects the red blood cells.
- Within the red blood cells, the micromerozoites undergo various stages of development until they form merozoites.
- In P.vivax this occurs at about 12 days, in P. falciparum about 9 days.
- The invasion of red blood varies based on the types of species such as; P. falciparum invades all red blood cells. P. vivax and P. ovale preferentially invade young red blood cells and reticulocytes. P. malariae preferentially invades senescent red blood cells.
- Then the merozoites then enter a cycle, where they move through the different stages of development to form more merozoites. As each cycle terminates the red cells are ruptured and the merozoite are released into the circulation.
- After that, the merozoites may attack more red blood cells and the cycle continues again.
- The cycle occurs roughly every 48 hours in P. falciparum infection, every 48-72 hours in P. vivax and P. ovale, and every 72 hours in P. malariae infection.
Gametogony
- Gametogony takes place when a few merozoites developed the sexual form of the parasite termed gametocytes.
- This phase may takes palace after the erythrocytic phase has been occurring for a considerable length of time.
- The patient becomes infective after the formation of gametocytes. Only the developed forms of the gametocytes are observed in the peripheral blood.
Exoerythrocytic schizogony (hypnozoite)
- Exoerythrocytic schizogony stage takes place with P. vivax and P. ovale where the parasites rest in a latent form in the liver.
- P. malariae also possesses a latent form that remains in the blood in these benign forms of malaria decline may consequently occur.
- P. falciparum, does not contain a latent form, and following successful cure, no relapses occur.
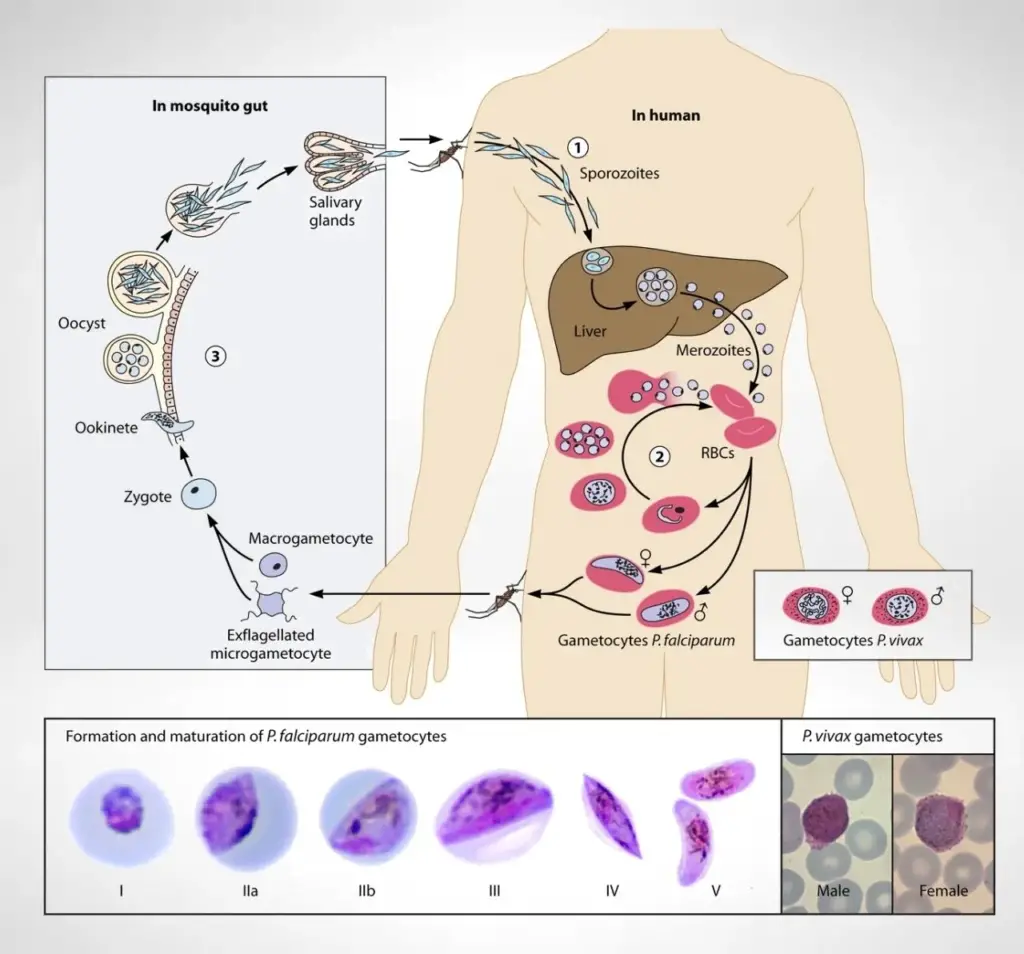
Sporogony
- Passage of malaria relies on the strong development of Plasmodium parasites within mosquitoes, a method is known sa sporogony.
- Sporogony is a complex phenomenon comprising several morphologically distinct life-stages nand starts when mosquitoes ingest blood carrying male and female gametocytes.
- Sporogony has three essential phases based on differences that occur in parasite abundance within the mosquito vector.
- The first phase of Sporogony known as “early sporogony”, a comparatively short period of time where parasite amounts typically decrease inside the mosquito. Early events include gametogenesis and fertilization, zygote transformation into ookinetes, ookinete motility through the bloodmeal and peritrophic matrix, penetration across midgut epithelia, and encystment beneath the midgut basal lamina to form oocysts. These events occur during the time that the engorged mosquito is digesting its bloodmeal (ca. 2 days).
- Early sporogony is followed by a period lasting up to a week or more (= “mid-sporogony”) where parasites are in the oocyst stage. Oocysts grow in size but their numbers remain static. The enlarging oocysts undergo multiple rounds of mitosis to form a syncytium, followed by cellular differentiation to form several thousand daughter cells (= sporozoites).
- The final phase is “late sporogony” which involves the release of the sporozoites into the mosquito haemocoel and their subsequent invasion into the mosquito salivary glands. Sporogony is considered complete after sporozoites successfully infect the mosquito salivary glands (ca. 10 to 16 days after initiation) and mosquitoes are able to transmit the parasite to a vertebrate host by infectious bite.
Diagnosis of Malaria
- The diagnosis of malaria can be done by observing the developing symptoms such as chills, sweats, fever, muscle pain, nausea, and vomiting which may appear within 7 to 30 days after infection.
- The detection of malaria can be done by laboratory tests such as serology tests, PCR, and drug-resistance tests or observing the blood sample of malaria patients under a microscope.
Treatment of Malaria
The treatment procedure for malaria disease depends on several factors such as
- the types of parasite species.
- the concentration of parasites within the bloodstream.
- whether the parasite is drug resistant or not
- the country where the parasite is located.
WHO recommended that the treatment will start within 24 hours after the development of symptoms.
For those patients, who’s malaria parasite is not identified they will be treated as they are infected with P. falciparum until the parasite is identified.
In those countries where chloroquine-resistant strains are not found, chloroquine can be used to treat P. falciparum, chloroquine.
In those countries where chloroquine resistance strain are founded, there three different types of treatment methods can be used such as;
- a combination of atovaquone and proguanil.
- oral quinine plus tetracycline, doxycycline, or clindamycin or
- 3 –mefloquine
Primaquine is an effective drug P. vivax and P. ovale, it prevents the spread of the parasite into the bloodstream. Chloroquine with hydroxychloroquine can be used For P. vivax infections as a second-line alternative.
The new drug Artemisinins is the most effective agents against multi-resistant malaria strains. But they are not widely available and are very expensive.
For severe malaria, the infection can be treated with quinidine or an exchange transfusion.
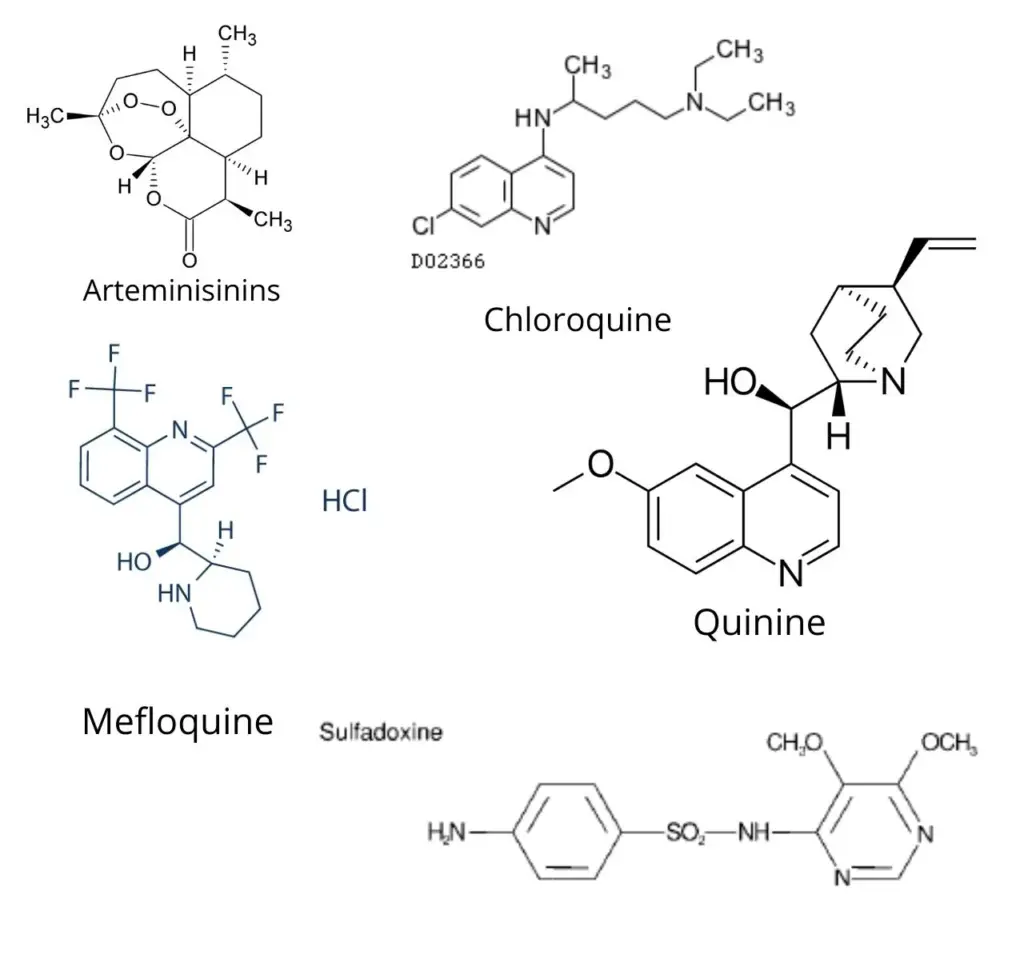
Drugs for Malaria
- Arteminisinins — A family of antimalarial products derived from an ancient Chinese herbal remedy. Two of the most popular varieties are artemether and artesunate, used mainly in southeast Asia in combination with mefloquine.
- Chloroquine — An antimalarial drug that was first used in the 1940s, until the first evidence of quinine resistance appeared in the 1960s. It is now ineffective against falciparum malaria almost everywhere. However, because it is inexpensive, it is still the antimalarial drug most widely used in Africa. Native individuals with partial immunity may have better results with chloroquine than a traveler with no previous exposure.
- Mefloquine — An antimalarial drug that was developed by the United States Army in the early 1980s. Today, malaria resistance to this drug has become a problem in some parts of Asia (especially Thailand and Cambodia).
An antimalarial drug that was developed by the United States Army in the early 1980s. Today, malaria resistance to this drug has become a problem in some parts of Asia (especially Thailand and Cambodia). - Quinine — One of the first treatments for malaria, quinine is a natural product made from the bark of the Cinchona tree. It was popular until being superseded by the development of chloroquine in the 1940s. In the wake of widespread chloroquine resistance, however, it has become popular again. Quinine, or its close relative quinidine, can be given intravenously to treat severe Falciparum malaria.
- Sulfadoxone/pyrimethamine (Fansidar) — An antimalarial drug developed in the 1960s. It is the first drug tried in some parts of the world where chloroquine resistance is widespread. It has been associated with severe allergic reactions due to its sulfa component.
Types of Preventive Measures: Drugs
- Prophylaxis with medications based on knowledge of geographic resistance patterns
- Mefloquine, Doxycycline, Atovaquone-Proguanil
- Self treatment: Fansidar, Quinine
- Combination of both: Chloroquine chemoprophylaxis with standby Rx (Not Recommended!)
- MDR resistance a problem in Thailand, Cambodia and Increasingly E. Africa
Transmission of Malaria Parasite
- Malaria Parasite can be transmitted through the bites of female Anopheles mosquitoes.
- It can be transmitted through blood transfusion, organ transplant, or the shared use of needles or syringes contaminated with blood.
- Malaria can transmit from a mother to her unborn infant.
Prevention of Malaria
- Take prophylactic measures when travelers are going into malaria-endemic countries. Before travel and when traveling in malaria-endemic areas take Chemoprophylaxis.
- Avoid mosquito bites by;
- Apply insect repellent which contains 20-35% percent N,N-Diethyl-meta-toluamide (DEET) to your exposed skin.
- When you are outside at night wear long-sleeved clothing and long pants.
- Use a mosquito net over the bed.
- Spray an insecticide or repellent on clothing.
- Before going to bed Spray pyrethrin or a similar insecticide in your bedroom.
Plasmodium Examples
Plasmodium Falciparum
- Plasmodium Falciparum are unicellular protozoan parasites that cause malaria in humans.
- Plasmodium Falciparum considered as the deadliest species of Plasmodium and are responsible for 50% of all malaria cases..
- They cause falciparum malaria which is the most dangerous form of malaria disease.
- They are classified as Group 2A carcinogen because they also help in development of blood cancer (Burkitt’s lymphoma).
- The parasite Laverania which is found in gorillas, is the origin of Plasmodium Falciparum.
The life cycle, diagnosis, treatment, prevention, transmission of Plasmodium Falciparum is already discussed above.
Plasmodium Vivax
- Plasmodium Vivax is responsible for recurring malaria.
- Plasmodium Vivax is less virulent than Plasmodium falciparum.
- They are mainly found in Asia, Latin America, and in some parts of Africa.
- The P. vivax originated from wild chimpanzees and gorillas throughout central Africa.
- 65% of malaria cases in Asia and South America are caused by the P. vivax.
- The spread of Plasmodium Vivax can be done through vector control.
The life cycle, diagnosis, treatment, prevention, transmission of Plasmodium Vivax is already discussed above.
Plasmodium knowlesi
- They are responsible for malaria disease in humans and other primates.
- Plasmodium knowlesi is mainly found in Southeast Asia and responsible for human malaria in Malaysia.
- They required both mosquitoes and a warm-blooded host to complete their life cycle like others.
- In 1932, Plasmodium knowlesi was first discovered.
The life cycle, diagnosis, treatment, prevention, transmission of Plasmodium knowlesi is already discussed above.
FAQ On Plasmodium
1. Are plasmodium protists?
Yes, Plasmodium is a genus of unicellular eukaryotes that are obligate parasites of vertebrates and insects.
2. Are plasmodium heterotrophic or autotrophic?
As like Amoebae and paramecium, plasmodium is a heterotrophic protist.
3. Are plasmodium bacteria?
No, plasmodium is a protista.
4. Can plasmodium falciparum interbreed?
No, plasmodium falciparum can’t interbreed.
5. Can plasmodium move?
Yes, plasmodium can move through a process known as the gliding motility.
6. Can plasmodium cross the placenta?
Yes, plasmodium can be transmitted across the placenta and could result in congenital malaria
7. How does plasmodium reproduce?
They reproduced by asexual reproduction known as the exoerythrocytic cycle within the hepatocytes.
8. How plasmodium is transmitted by mosquitoes?
When an infected female Anopheles mosquito bites a human it injects the parasite inside the bloodstream.
9. How plasmodium causes malaria?
Follow the life cycle of plasmodium.
10. How plasmodium is transmitted?
Mosquito bites, blood transfusion, organ transplant, or the shared use of needles or syringes contaminated with blood. Malaria can transmit from a mother to her unborn infant.
11. What plasmodium causes malaria?
Five species of Plasmodium are responsible for human malaria such as: P. falciparum, P. malariae, P. vivax, P. knowlesi, and P. ovale.
12. When was plasmodium discovered?
Plasmodium parasite is considered the oldest known parasite in the world. In 1880, Charles Louis Alphonse Laveran first described the presence of Plasmodium parasites in the blood of malaria patients.
13. When was plasmodium falciparum discovered?
plasmodium falciparum originated around 10,000 years ago from the malarial parasite Laverania found in gorillas.
14. When does plasmodium reproduce asexually?
Within the hepatocytes the started their asexual reproduction known as the exoerythrocytic cycle.
15. Where plasmodium is found?
Plasmodium falciparum found in tropical and sub-tropical areas. Plasmodium ovale is mostly found in the west coast region of Africa. Plasmodium malariae has a widespread distribution area but is fairly scattered within this area.
16. Where does plasmodium come from?
Plasmodium falciparu originated from the malarial parasite Laverania found in gorillas, Plasmodium vivax originated from the wild chimpanzees and gorillas throughout central Africa
17. Plasmodium eukaryotic or prokaryotic?
Plasmodium are eukaryotic cells.
18. How is Plasmodium vivax transmitted?
Mosquito bites, blood transfusion, organ transplant, or the shared use of needles or syringes contaminated with blood. Malaria can transmit from a mother to her unborn infant.
19. What are the symptoms of Plasmodium vivax?
The symptoms are shaking chills that can range from moderate to severe, high fever, profuse sweating, headache, nausea, vomiting, abdominal pain, diarrhea, anemia, muscle pain, convulsions, coma, bloody stools.
Reference and Further Reading
- Zollner, G.E., Ponsa, N., Garman, G.W. et al. Population dynamics of sporogony for Plasmodium vivax parasites from western Thailand developing within three species of colonized Anopheles mosquitoes. Malar J 5, 68 (2006). https://doi.org/10.1186/1475-2875-5-68
- https://gpnotebook.com/simplepage.cfm?ID=x20140430174005216972
- World Health Organization (WHO) 2014. Fact sheet. Malaria
- Public Health England. Guidelines for malaria prevention in travelers from the UK 2019
- Rosenthal PJ. Artesunate for the Treatment of Severe Falciparum Malaria. NEJM 2008; 358:1829-1836
- Centers for disease control and prevention. Traveler’s health – Yellow book
- http://askdefine.com/define/schizont
- https://www.gdcbasohli.in/images/20181114976393.Presentation-on-Malarial-parasite-by-Prof.-Shiv-kumar.pdf
- https://www.gdcbasohli.in/images/20181114976393.Presentation-on-Malarial-parasite-by-Prof.-Shiv-kumar.pdf
- https://www.scribd.com/document/328583717/Life-Cycle-Pathogenicity-and-Prophylaxis-of-Plasmodium-vivax-pdf#
- https://www.coursehero.com/file/22689849/Life-Cycle-Pathogenicity-and-Prophylaxis-of-Plasmodium-vivax/
- https://www.vedantu.com/biology/plasmodium-vivax
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.