What are mast cells?
- Mast cells, also referred to as mastocytes or labrocytes, are a specific type of resident cell found in connective tissue. They possess numerous granules that are abundant in histamine and heparin. These cells are derived from the myeloid stem cell and are integral components of the immune and neuroimmune systems. Their discovery dates back to 1877 when Paul Ehrlich first identified them. While mast cells are commonly associated with their involvement in allergies and anaphylaxis, they also serve a crucial protective role. They are intricately engaged in processes such as wound healing, angiogenesis, immune tolerance, defense against pathogens, and regulation of vascular permeability in brain tumors.
- In terms of appearance and function, mast cells bear a striking resemblance to basophils, another type of white blood cell. Initially, it was believed that mast cells were simply tissue-resident basophils. However, research has demonstrated that these two cell types arise from different hematopoietic lineages, indicating that they are distinct entities. Mast cells of the hematopoietic lineage are widely distributed in vascularized tissues throughout the body.
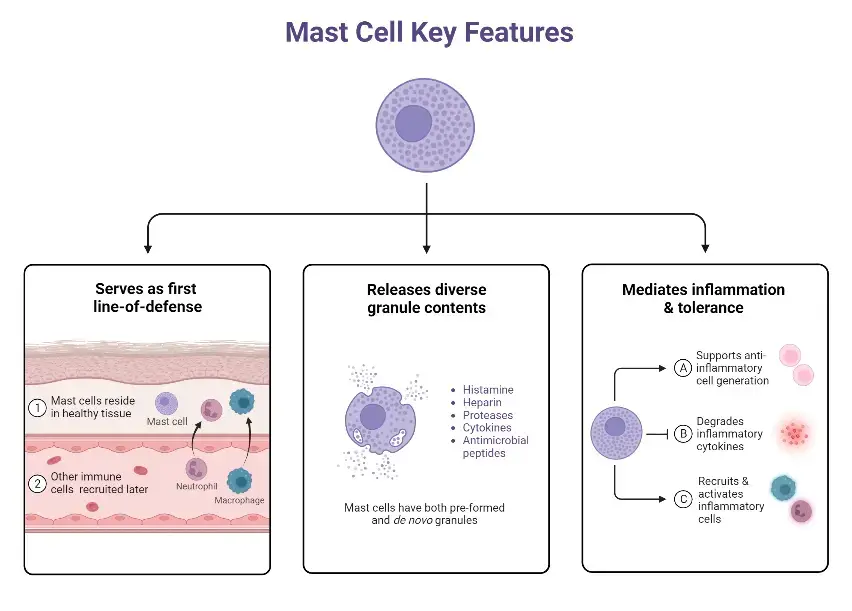
- Unlike many immune cells that circulate in the bloodstream, mast cells do not remain in the blood but instead localize themselves in mucosal and epithelial tissues throughout the body. Due to their strategic positioning, mast cells are among the first cells to encounter environmental antigens, as well as invading pathogens and microorganisms. Consequently, they are considered one of the initial immune cells to interact with external antigens. While mast cells are primarily associated with IgE-dependent responses, they also respond to various innate signals from pathogens, complement compounds, and other host cell types. Furthermore, mast cells express numerous costimulatory molecules with immunoregulatory functions, contributing to the regulation of immune responses within the body.
- Originating from pluripotent progenitor cells that possess CD34+ and CD117+ markers, mast cells are produced in the bone marrow. Initially, they are released into the bloodstream as undifferentiated cells. Upon leaving the blood and migrating to specialized tissues, these cells undergo maturation, a process that is dependent on KIT activation.
- In summary, mast cells play vital roles in the immune system and neuroimmune system. They have distinct features and functions, contributing to various physiological processes such as immune response, wound healing, and defense against pathogens. Their distribution in different tissues and their ability to interact with antigens make them important players in the body’s defense mechanisms.
Definition of mast cells
Mast cells are a type of immune cell found in connective tissue that are involved in allergic reactions, immune responses, inflammation, and wound healing. They contain granules rich in histamine and play a crucial role in the body’s defense against pathogens.
Structure of Mast cell
- Mast cells possess a distinctive structure that sets them apart as unique immune cells. They are mononuclear cells characterized by small secretory granules ranging in size from 0.2 to 0.8 micrometers. In some cases, the granules are dense enough to obscure the visibility of the nucleus. The cells themselves are oval or irregularly shaped, typically with a central nucleus. The nucleus contains densely packed peripheral chromatin.
- The majority of the cytoplasm in mast cells is occupied by cytoplasmic granules, although there are also a few secondary lysosomes present. Additionally, the cells feature small finger-like projections extending from the cell membrane.
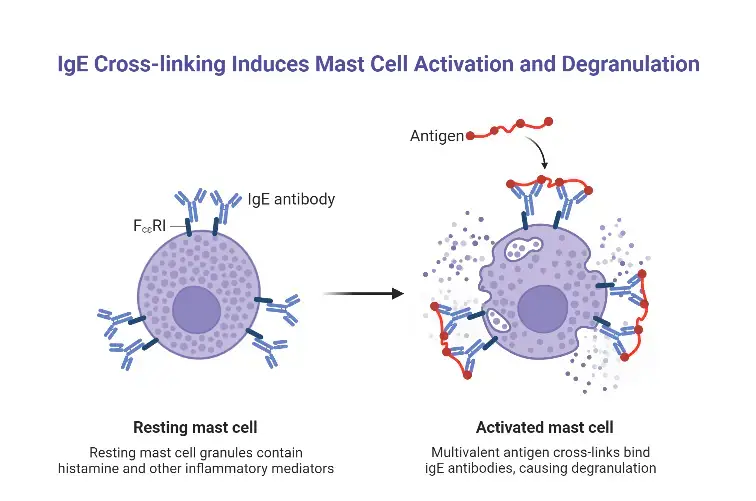
- These granules within mast cells serve as storage sites for various inflammatory mediators, including histamine, heparin, cytokines, and proteases. The plasma membrane of mast cells contains IgE receptors, which bind to the Fc region of circulating IgE antibodies. This binding triggers degranulation of the mast cells, leading to the release of the stored mediators.
- While mast cells share similarities with basophils, they can be differentiated based on their mononuclear morphology and the use of monoclonal antibodies. Basophils have lobated nuclei, whereas mast cells have round nuclei.
- Mast cells exist in three distinct forms based on their structural characteristics. Intact cells are predominantly found in blood vessels and dermal tissues, exhibiting closely packed granules that obscure other organelles. These cells typically have a spindle-shaped appearance. Spreading cells are present in the superficial connective tissue and possess fewer granules compared to intact cells. Degranulated cells, on the other hand, lack metachromatic properties and exhibit clear cytoplasm with a prominent nucleus.
- It is worth noting that mast cells and basophils are similar in granulated nature, containing histamine and heparin. They also share IgE receptor binding and the release of histamine and other inflammatory mediators upon antigen stimulation. Some researchers speculate that mast cells may be tissue-localized basophils. They both arise from a common precursor in the bone marrow expressing the CD34 molecule. Basophils mature in the bone marrow and circulate in a mature form, while mast cells mature in specific tissues after settling there.
- In rodents, mast cells are classified into two subtypes: connective tissue-type mast cells and mucosal mast cells. The activity of mucosal mast cells depends on T-cells.
- Mast cells are widely distributed throughout various tissues, typically surrounding blood vessels, nerves, and lymphatic vessels. They are particularly prominent in regions where the external environment meets the internal milieu, such as the skin, mucosa of the lungs and digestive tract, as well as the mouth, conjunctiva, and nose.
Types of Mast Cells
Mast cells are a type of immune cells that play an important role in the body’s defense against pathogens and in allergic reactions. There are several types of mast cells that differ based on their location and the types of molecules they produce.
The two main types of mast cells are:
1. Connective tissue mast cells
These mast cells are found in connective tissues throughout the body, such as the skin, lungs, and digestive tract. They are responsible for the immediate response to allergens and parasites, and release histamine, prostaglandins, and leukotrienes, which cause inflammation and smooth muscle contraction.
2. Mucosal mast cells
These mast cells are found in the mucous membranes that line the respiratory and digestive tracts, as well as the genitourinary tract. They are involved in immune surveillance and response to pathogens, and release cytokines, chemokines, and proteases.
In addition to these two main types, there are also other subtypes of mast cells that have been identified based on their location, function, and expression of specific proteins. These include perivascular mast cells, skin mast cells, and serosal mast cells, among others.
Morphologies of mast cell – mast cells microscope
Under Light Microscope
Mast cells are irregularly or oval-shaped cells. Often, thick granular cytoplasm obscures the nucleus and other organelles under optical microscopy. The nucleus is central and the cell is mononuclear when it is visible. Mast cells are located in connective tissue throughout the body. Some are randomly distributed throughout the tissue. They tend to congregate close to blood arteries, where cells are more elongated. Concentrates can also be detected at hair follicles, sebaceous glands, and sweat glands in the skin.
By means of light microscopy, three morphologies of mast cells have been identified;
- Near blood arteries and deep into the dermis and subcutaneous tissue, one can find Intact Cells. Granules are densely packed, making it difficult to discern other cellular features. As stated previously, these cells have a spindle-like morphology.
- Spreading Cells are located in the superficial connective tissue, in close proximity to the upper dermis. However, there are fewer granules than in a complete cell type. This makes it possible to distinguish between each granule.
- Degranulated Cells are not metachromatic anymore. They are stained with a faint pink hue and have a blue nucleus.
Under Electron Microscope
Mast cells are again characterised by an abundance of cytoplasmic granules, also known as secondary lysosomes, when viewed by scanning electron microscopy. These granules have a lipid membrane surrounding them. Under optimal conditions, one can observe profound invaginations of the cell membrane. When a cell degranulates, its plasma membrane forms channels, exposing granules located deep within the cell to the external environment.
A large number of tiny, finger-like pseudopods protrude from the cell membrane. Round, tightly packed chromatin encircles the centrally placed nucleus. The type of cell determines the ultrastructure of granules.
- Granules of intact cells have little visible structure.
- The majority of Spreading Cells’ granules are composed of tiny particle materials. Lamellae arranged in circular “scroll-like” patterns are interspersed throughout these granules.
Stain for mast cells
The most commonly used stain for mast cells is toluidine blue. This basic dye stains the metachromatic granules present in mast cells, making them easily visible under a microscope. When toluidine blue is used to stain tissue sections, mast cells appear as dark purple or blue-black granular cells. Other staining methods, such as Giemsa or Wright’s stain, can also be used to visualize mast cells, but toluidine blue is considered the gold standard for mast cell staining. Immunohistochemistry can also be used to identify mast cells by staining for specific mast cell markers, such as tryptase or chymase.
Mechanism of Activation
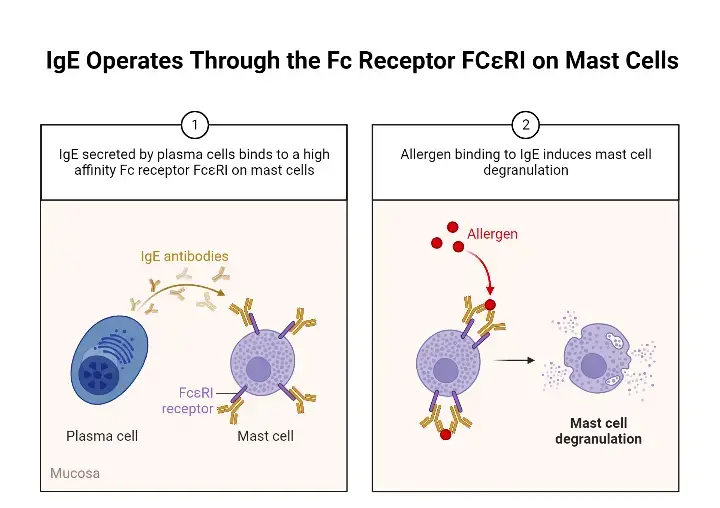
- The primary mode of action of mast cells is IgE-mediated allergic responses mediated by the FcRI receptor.
- Mature B cells generate IgE antibodies in response to CD4+ Th2 cells. IgM and IgD antibodies are made by nave mature B lymphocytes.
- B cells will proliferate once they’ve been triggered by an antigen. If these B cells engage with IL-4 (which is controlled by CD4+ Th2 cells), the antibody type changes from IgM to IgE.
- IgE is predominantly found attached to FcRI receptors on mast cells, and relatively little IgE circulates as a soluble antibody. When an antigen contacts a mast cell, it causes the crosslinking of two or more FcϵRI molecules and the release of granules from the mast cell. Connective tissue beneath the epithelial layers of the epidermis, the respiratory tract, and the gastrointestinal tract all contain IgE.
- Mast cells have Fc receptors for IgA and IgG, receptors for adenosine, C3a, chemokines, cytokines, and pathogen-associated molecular patterns (PAMPs), as well as toll-like receptors (TLRs), which are all involved in mast cell activation and immune response. Cross-linking between antigen, IgE, and FcϵRI is the most frequent physiologic mechanism for mast cell activation.
- FcϵRI is composed of a β-chain that binds to IgE, a α-chain that bridges the membrane, and disulfide-linked homodimer γ chains. FcϵRI interacts with LYN tyrosine kinase, which phosphorylates immunoreceptor tyrosine bases activation motifs (ITAMs) on the B and γ chains of FcϵRI.
- Lyn stimulates Syk tyrosine kinases, which phosphorylate signalling proteins including LAT1 and LAT2 (linkers for activation of T cells). Phosphorylated PLCγ generates inositol-1,4,5-triphosphate (IP3) and diacylglycerol by hydrolyzing phosphatidylinositol-4,5-bisphosphate (DAG). Both IP3 and DAG are second messengers, and IP3 mobilises calcium from the endoplasmic reticulum.
- Calcium release activates and translocates NFκB to the cell nucleus, resulting in production of cytokines including IL-6, TNF-α, and IL-13. Zeb2 is involved in the regulation of degranulation in response to FcϵRI stimulation.
- FcϵRI activation stimulates Fyn (Src kinase). Fyn controls mast cell degranulation, complementing the Lyn signalling pathway. Fyn stimulates PI3K, which subsequently activates Akt and generates PIP3.
- This stimulates the mTOR protein, which is essential for mast cell chemotaxis and cytokine production. There are also IgG receptors known as FcγR. Since the y-chain homodimer is identical in FcRI and FcϵRI, the signal transmitted by FcϵR might crosstalk with FcϵRI.
- Repeated exposure of mast cells to antigen under controlled conditions can desensitise a patient. The slow and continuous degranulation of mast cells is believed to be one of the mechanisms, despite the fact that they are not fully understood.
- Patients who are allergic to particular medications (e.g., penicillin) but require therapy for a life-threatening bacterial infection that can only be cured with this drug undergo desensitisation.
- By exposing mast cells to escalating antigen doses, desensitisation can ensue. This method can be utilised if a patient is allergic to a vital drug and for the prevention of food-related anaphylaxis events.
- By desensitising the receptors, this can reduce the amount of FcϵRI molecules on the surface of mast cells.
Role of Mast cell in Angiogenesis
- Mast cells play a role in promoting angiogenesis. Mast cells produce pro-angiogenic factors including VEGF, bFGF, TGF-beta, TNF-alpha, and IL-8.
- In addition, mast cells release proteases and heparin, which cause pro-angiogenic factors to be released and bind to heparin.
- Histamine, which is produced by mast cells, causes microvasculature permeability and angiogenesis.
- There is additional evidence that mast cells promote tumour angiogenesis.
Role of Mast cell in Homeostasis
- Mast cells help to immune system balance. Due to their placement on the skin and mucosa, they act as the first line of defence against antigens entering the body.
- Mast cells play a crucial role in maintaining the intestinal commensal bacteria’s equilibrium.
- The digestive system is continuously exposed to antigens, including commensal and pathogenic bacteria and dietary antigens.
- The digestive system’s epithelial cells function as a barrier against these antigens. ATP signalling is essential for the development of follicular helper T cells involving mast cells.
- Therefore, mast cells play a role in IgA maturation and overall gut bacterial balance.
Role of Mast cell in Innate and Adaptive Immunity
- Mast cells are crucial to both innate and adaptive immunity. Mast cells identify hazardous antigens by attaching directly to pathogens or interacting with PAMPs on the surface of mast cells.
- TLRs and complement receptors are the most prevalent receptors on mast cells. Once the antigen connects to the mast cell’s receptors, it triggers the release of inflammatory mediators, which aid in the elimination of the pathogen that activated the cell.
- The mechanism through which this occurs is dependent on the PAMP that is detected. Gram-positive bacteria and, to a lesser extent, Gram-negative bacteria and mycobacteria activate TLR2, causing the mast cell to release cytokines such as IL-4.
- TLR4 binds to LPS from Gram-negative bacteria, resulting in the production of proinflammatory cytokines (TNFα, IL-1, and IL-6) without degranulation.
- Alternatively, the Gram-positive bacterial product peptidoglycan induces mast cell degranulation and histamine release by activating TLR2.
- By releasing inflammatory mediators that increase vascular permeability, increase fluid buildup, and draw immune cells such as eosinophils, NK cells, and neutrophils, mast cells contribute in the eradication of germs.
- In addition, mast cells produce directly antimicrobial substances, including cathelidcidins, defensins, and psidins. Mast cells also contribute to antiviral responses by recruiting IFN-α and IFNβ—producing CD8+ T cells.
- When activated by IgE, one of the earliest discovered activities of the mast cell was to establish an anti-parasitic environment. Mast cell release of mediators enhances vascular permeability and smooth muscle contraction, so aiding in the expulsion of parasites from the gastrointestinal tract by producing vomiting or diarrhoea, and from the respiratory tract by coughing.
- Mast cells participate in adaptive immunity as well. Mast cells use MHCI and MHCII to digest and deliver antigens.
- Mast cells stimulate dendritic cells, which serve as antigen-presenting cells as well. When mast cells are activated by TLF-7, they release IL-1 and TNFα, causing dendritic cells to migrate from the skin to lymph nodes and activate cytotoxic T cells.
- In addition, mast cells emit TNFα, which can directly activate cytotoxic T lymphocytes.
Mast Cells Function
- The inflammatory cascade is the classic and best-known function of mast cells. Mast cells serve as a component of the body’s innate immune system.
- When membrane-bound IgE hits a foreign material and two Fc receptors crosslink, the mast cell promptly degranulates and releases a huge quantity of mediators into the surrounding extracellular space.
- Granules are surrounded by a lipid membrane that merges with the plasma membrane. Histamine is the most significant cytokine secreted.
- Histamine promotes chemotaxis of white blood cells, constriction of airway smooth muscle, and enhanced vascular permeability. Tryptase, chymase, and TNF-alpha are other mediators secreted from the granules.
- The mast cell then synthesises and releases pro-inflammatory prostaglandins and leukotrienes derived from lipids. Lastly, an increase in gene transcription increases cytokine production.
- The innate immune system utilises the inflammatory impact of mast cells as its first line of defence.
- MC(T) cells are the primary immune response cell type. When a foreign protein is met, the mast cell’s pro-inflammatory activities result in the recruitment of circulating immune cells.
- Cytokines have direct effects on local tissue, such as an increase in mucus production or an increase in intestinal peristalsis, in order to prevent pathogen invasion.
- Additionally, mast cells contribute to tissue healing and angiogenesis. Upon damage, MC(TC) independently of IgE pathways produce procoagulant cytokines, leukotrienes, and platelet-activating factor.
- Later, heparin, tryptase, and t-PA from the cell modify blood flow in order to improve the delivery of nutrients and immune cells. Inflammatory mediators stimulate fibroblast and endothelial cell differentiation and proliferation.
- Additionally, mast cells contain numerous angiogenic cytokines, such as VEGF and FGF 2. Mast cells have also been linked to the constriction of wounds and regeneration of nerve fibres.
- Mast cells have never been shown to be deficient, indicating that their functions are vital to survival.
How do Mast Cells work against pathogens? (Immunity)
- Mast cells play a significant role in the immune response against pathogens through various mechanisms. One of the key ways in which mast cells contribute to immunity is through IgE-mediated allergic reactions via the Fc receptor.
- When the body encounters a pathogen, mature B cells are activated by CD4+ Th2 cells, leading to the production of IgE antibodies. This process involves class switching from IgM to IgE in the presence of IL-4. The produced IgE antibodies then bind to Fc receptors on mast cells, triggering their activation and subsequent release of granules.
- Upon binding, the Fc receptors activate the LYN tyrosine kinase within the mast cells. LYN phosphorylates the tyrosine in the binding site, leading to the activation of specific motifs. Additionally, LYN activates Syk tyrosine kinase, which phosphorylates signaling proteins like LAT1 and LAT2.
- Phosphorylated PLCγ is then involved in the hydrolysis of phosphatidylinositol-4,5-biphosphate, resulting in the formation of inositol-1,4,5-triphosphate (IP3) and diacylglycerol (DAG). IP3 and DAG act as second messengers, triggering the mobilization of calcium from the endoplasmic reticulum. This release of calcium from the ER leads to the translocation of NFκB to the nucleus of the cell.
- The process is further accompanied by the release of cytokines such as IL-6, TNFα, and IL-13. These cytokines play a regulatory role in the degranulation of mast cells, contributing to the immune response against pathogens.
- Furthermore, mast cell desensitization is an important mechanism employed in response to allergies caused by drugs or food particles. In this process, repeated exposure to the allergen leads to a reduced response from mast cells, resulting in decreased allergic reactions over time.
- Overall, mast cells are actively involved in the immune response against pathogens. Through IgE-mediated reactions and the release of cytokines, they contribute to the regulation of inflammation and play a crucial role in defending the body against various pathogens.
Eosinophils vs Mast cells
Eosinophils and mast cells are two types of immune cells that play different roles in the body’s immune response.
Eosinophils are a type of white blood cell that are involved in the body’s response to parasites, allergic reactions, and certain infections. They are characterized by their ability to release cytotoxic granules, such as major basic protein and eosinophil peroxidase, which can damage parasites and certain host tissues. Eosinophils also produce cytokines and chemokines that can recruit and activate other immune cells.
Mast cells, on the other hand, are a type of immune cell that are primarily involved in the body’s response to allergic reactions and certain infections. They are located throughout the body in tissues such as the skin, lungs, and digestive tract, and are characterized by their ability to release histamine, prostaglandins, and leukotrienes, which can cause inflammation, smooth muscle contraction, and other allergic symptoms. Mast cells also play a role in host defense against certain pathogens and parasites, and can produce cytokines and chemokines that can recruit and activate other immune cells.
While both eosinophils and mast cells can be involved in the body’s response to allergic reactions, they differ in their mechanisms of action and the types of molecules they produce. Eosinophils are primarily involved in the destruction of parasites and certain host tissues, while mast cells are involved in the release of inflammatory molecules that cause allergic symptoms.
Functions of Mast Cells
Mast cells serve a range of important functions within the body, contributing to various physiological processes and immune responses. Here are some key functions of mast cells:
- Angiogenesis: Mast cells play a role in promoting the formation of new blood vessels through the secretion of pro-angiogenic factors like VEGF, bFGF, TGF-beta, and IL-8. They also release proteases and heparin, which induce microvasculature permeability, facilitating angiogenesis.
- Defense against antigens: Mast cells are among the frontline defenders against invading antigens. They help maintain the body’s homeostasis, particularly in the gastrointestinal tract, by recognizing and responding to antigens that enter the body.
- Innate immunity: Mast cells contribute to innate immunity by binding to antigens through specific receptors, leading to the release of inflammatory mediators such as IL-4, TNFα, and IL-6. These mediators initiate and regulate the inflammatory response.
- Viral immunity: Mast cells play a role in providing immunity against viral antigens. They release interferons, specifically IFN-α and IFN-β, which have antiviral properties and help in combating viral infections.
- Adaptive immunity: Mast cells participate in adaptive immunity by processing and presenting antigens via major histocompatibility complex (MHC) molecules, including both MHCI and MHCII. They also activate dendritic cells, which are professional antigen-presenting cells, contributing to the initiation and regulation of adaptive immune responses.
- Mediator release: One of the primary functions of mast cells is the release of newly synthesized mediators required for immune responses. This includes the secretion of histamine, cytokines, chemokines, and other bioactive molecules involved in inflammation and immune regulation.
- Allergic reactions: Mast cells are central players in allergic reactions. When activated by an allergen, they release a cascade of inflammatory mediators, leading to symptoms such as itching, redness, swelling, and bronchoconstriction. Over-activation of mast cells can result in hyper-allergic reactions, which can be severe and life-threatening.
Through their multifaceted functions, mast cells contribute to immune surveillance, tissue homeostasis, angiogenesis, and immune responses against pathogens. Understanding the roles and regulation of mast cells is crucial for unraveling their involvement in various diseases and developing targeted therapeutic approaches.
FAQ
What are mast cells?
Mast cells are a type of immune cell that play an important role in the body’s defense against pathogens and in allergic reactions.
Where are mast cells found in the body?
Mast cells are found throughout the body in tissues such as the skin, lungs, and digestive tract.
What is the function of mast cells?
Mast cells are involved in the body’s immune response to pathogens and parasites, as well as in the development of allergic reactions.
What molecules do mast cells release?
Mast cells release molecules such as histamine, prostaglandins, and leukotrienes, which cause inflammation, smooth muscle contraction, and other allergic symptoms.
What is mast cell activation syndrome?
Mast cell activation syndrome is a condition in which mast cells become overactive and release excessive amounts of inflammatory molecules, leading to a range of symptoms such as hives, abdominal pain, and difficulty breathing.
How is mast cell activation syndrome diagnosed?
Mast cell activation syndrome can be diagnosed through a combination of clinical symptoms, laboratory tests, and tissue biopsies.
What is the treatment for mast cell activation syndrome?
The treatment for mast cell activation syndrome typically involves a combination of medications to reduce inflammation and stabilize mast cells, as well as avoidance of triggers and lifestyle modifications.
How is mastocytosis diagnosed?
Mastocytosis can be diagnosed through a combination of clinical symptoms, laboratory tests, and tissue biopsies.
What is mastocytosis?
Mastocytosis is a rare disorder characterized by the abnormal accumulation of mast cells in various tissues, leading to a range of symptoms such as skin lesions, gastrointestinal disturbances, and bone pain.
What is the treatment for mastocytosis?
The treatment for mastocytosis depends on the type and severity of the disease, and may involve medications to reduce symptoms and complications, as well as lifestyle modifications and avoidance of triggers.
References
- Gilfillan, A.M., Austin, S.J., Metcalfe, D.D. (2011). Mast Cell Biology: Introduction and Overview. In: Gilfillan, A.M., Metcalfe, D.D. (eds) Mast Cell Biology. Advances in Experimental Medicine and Biology, vol 716. Springer, Boston, MA. https://doi.org/10.1007/978-1-4419-9533-9_1
- Krystel-Whittemore, M., Dileepan, K. N., & Wood, J. G. (2016). Mast Cell: A Multi-Functional Master Cell. Frontiers in Immunology, 6. doi:10.3389/fimmu.2015.00620
- Fong M, Crane JS. Histology, Mast Cells. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499904/
- https://microbenotes.com/mast-cells/