- The heart, a vital organ in the human body, plays a crucial role in maintaining life. It beats relentlessly, contracting approximately 108,000 times in a day, more than 39 million times in a year, and nearly 3 billion times during the span of a 75-year lifespan. With each contraction, the heart pumps around 70 mL of blood from its major pumping chambers, amounting to 5.25 liters of fluid per minute and an astonishing 14,000 liters per day. Over the course of a year, this adds up to 10,000,000 liters or 2.6 million gallons of blood flowing through a vast network of approximately 60,000 miles of blood vessels.
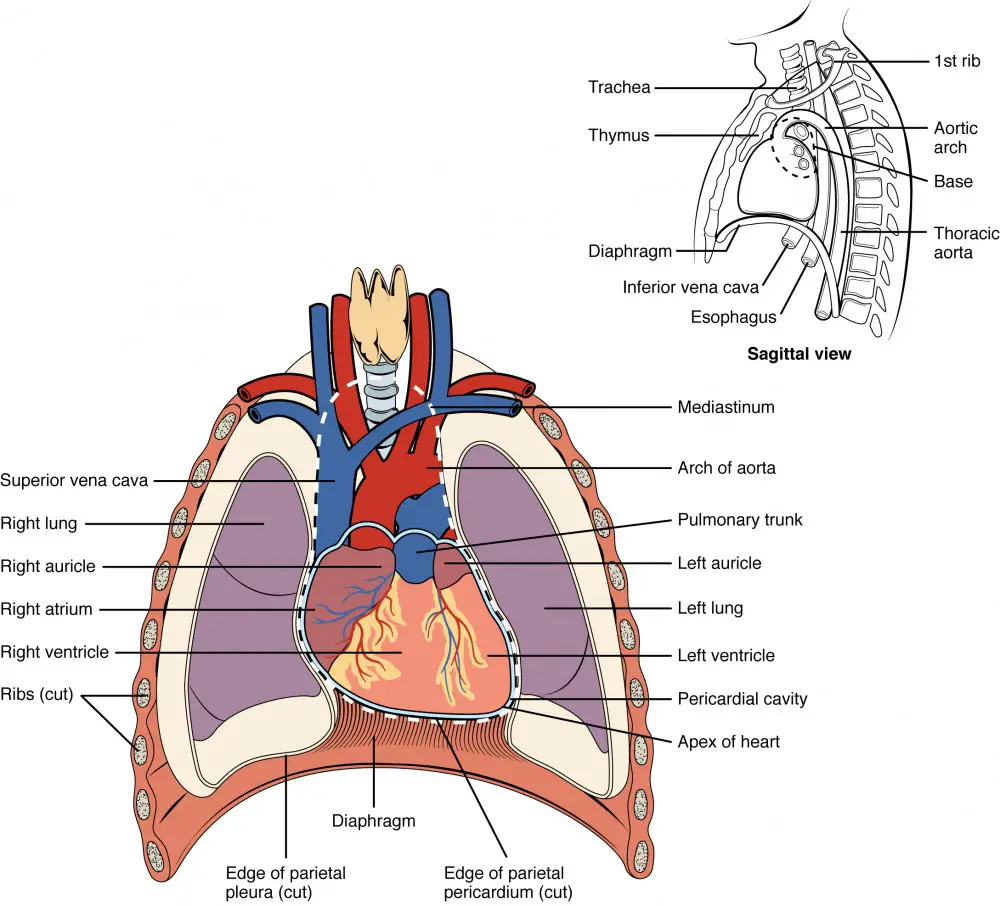
- The heart is often described as being the size of a clenched fist and is located anteriorly, just behind the sternum. Positioned in the mediastinum of the thorax, between the two lungs and resting on the diaphragm, the heart occupies a significant portion of the left side of the body. The mediastinum, the region in the thoracic cavity between the pleural cavities, houses not only the heart but also the thymus, trachea, and esophagus.
- Functionally, the heart is a remarkable hollow muscular organ responsible for generating pressure and circulating blood throughout the body. Its continuous contractions are driven by cardiac action potentials, which initiate and coordinate the pumping action. Serving as the primary organ of the cardiovascular system, the heart propels blood, collecting it from various parts of the body and recirculating it to ensure efficient oxygenation and nutrient delivery.
- The study of the heart and its related conditions is known as cardiology, derived from the Greek word “kardia,” meaning heart. A cardiologist is a medical expert specializing in diagnosing and treating heart-related ailments.
- Composed of smooth muscle, the heart consists of four chambers that contract in a precise sequence, enabling efficient blood circulation from the body to the lungs and back again. The heart’s intricate workings involve specialized pacemaker cells that generate electrical impulses at regular intervals, initiating the rhythmic contractions of the heart muscle.
- While the heart’s functioning may appear complex, an animation can help visualize the interplay between the chambers, valves, and blood vessels that facilitate blood flow throughout the body.
- The heart’s significance cannot be overstated. A malfunctioning heart can have severe consequences, with all other organs, including the brain, succumbing to oxygen deprivation within mere minutes. Heart disease has emerged as the leading cause of death worldwide, often resulting from factors such as age and lifestyle. As individuals age, cholesterol can accumulate in the arteries, particularly in those who consume diets high in saturated fat and cholesterol. However, heart disease can also arise from infections caused by viruses or bacteria that affect the heart or its protective tissues, albeit rarely.
- While scientists have made progress in developing artificial pumps that replicate the heart’s pumping action, these devices face challenges such as rejection by the body and degradation over time.
- The four-chambered heart found in mammals and birds is remarkably efficient compared to the hearts of other animals, which may possess one, two, or three chambers. The high demand for oxygen in warm-blooded animals, particularly humans with their substantial brains, necessitates highly efficient circulation to meet the metabolic needs of their cells.
- In essence, the heart symbolizes the remarkable intersection of structure and function in the human body. Its relentless pumping action sustains life by ensuring the continuous delivery of oxygen and nutrients to every cell, highlighting its crucial role in maintaining our existence.
Definition of Human Heart
The human heart is a vital organ that continuously pumps blood throughout the body, providing oxygen and nutrients to cells and removing waste products. It is a hollow muscular organ located in the chest, primarily on the left side, and consists of four chambers that contract in a coordinated manner to facilitate efficient blood circulation. The heart’s rhythmic contractions are driven by electrical impulses, and its proper functioning is essential for maintaining life.
Location of Heart
- The human heart is situated within the thoracic cavity, specifically in the mediastinum, which is the central space between the lungs. This location provides protection and support for the heart. The heart is separated from other structures in the mediastinum by a tough membrane known as the pericardium or pericardial sac. It occupies its own space called the pericardial cavity.
- When considering the position of the heart within the thoracic cavity, the dorsal surface of the heart lies near the vertebrae, while the anterior surface is situated deep to the sternum and costal cartilages. The superior surface of the heart, referred to as the base, is where the great veins (superior and inferior venae cavae) and great arteries (aorta and pulmonary trunk) are attached. The base of the heart can be found at the level of the third costal cartilage.
- The inferior tip of the heart, known as the apex, is located to the left of the sternum. More specifically, it lies between the junction of the fourth and fifth ribs near their articulation with the costal cartilages. This positioning of the apex is important to consider when using a stethoscope to listen for heart sounds or when examining images taken from a midsagittal perspective.
- Additionally, it’s worth noting that the right side of the heart is deflected anteriorly (forward), while the left side is deflected posteriorly (backward). These deviations in orientation are significant in understanding the anatomical structure and function of the heart.
- The slight deviation of the apex to the left is reflected in a depression in the medial surface of the inferior lobe of the left lung, which is known as the cardiac notch.
- In summary, the heart is located within the mediastinum of the thoracic cavity. It is separated from other structures by the pericardium and resides in the pericardial cavity. The heart’s base is situated at the level of the third costal cartilage, while the apex can be found to the left of the sternum between the junction of the fourth and fifth ribs. The positioning of the heart is important for clinical examinations and imaging studies, and it exhibits slight deflections in orientation between the right and left sides.
Morphology of Heart (Shape and Size of the Heart)
- The heart, with its remarkable shape and size, is a vital organ responsible for pumping blood throughout the body. In terms of its morphology, the heart exhibits a distinct shape that can be compared to a pinecone. Its superior surface is relatively broad, gradually tapering down to a pointed apex. This unique structure allows for efficient functioning and optimal distribution of blood throughout the circulatory system.
- When it comes to the size of the heart, it is often described in relation to the dimensions of a person’s fist. On average, a typical heart measures about 12 cm (5 in) in length, 8 cm (3.5 in) in width, and 6 cm (2.5 in) in thickness. However, it is important to note that individual variations can occur.
- In addition to the dimensions, the weight of the heart also varies between individuals and genders. In general, the female heart weighs approximately 250–300 grams (9 to 11 ounces), while the male heart weighs around 300–350 grams (11 to 12 ounces). It’s worth mentioning that the size and weight of the heart can be influenced by various factors, such as overall body size, fitness level, and specific medical conditions.
- Interestingly, the hearts of well-trained athletes, particularly those involved in aerobic sports, can exhibit significant differences in size compared to the average individual. Regular exercise stimulates the cardiac muscle, prompting a response similar to skeletal muscle. This response, known as hypertrophy, involves the addition of protein myofilaments, which results in the enlargement of individual cardiac muscle cells. Consequently, the hearts of athletes can become larger and more efficient, enabling them to pump blood more effectively, even at lower heart rates.
- However, it is important to note that heart enlargement can also be associated with certain pathological conditions. One such condition is hypertrophic cardiomyopathy, where the heart muscle becomes abnormally enlarged without any obvious cause. This condition often goes undiagnosed and can lead to sudden death, particularly among seemingly healthy young individuals.
- In summary, the morphology of the heart encompasses its unique shape and size. Its pinecone-like structure, broad at the top and tapering to the apex, facilitates its essential function of pumping blood. The average heart size is roughly the size of a fist, but this can vary between individuals, genders, and even athletes. While exercise-induced hypertrophy can result in a larger, more efficient heart, certain pathological conditions can also cause abnormal enlargement, emphasizing the importance of regular medical check-ups and prompt diagnosis of any cardiac abnormalities.
Pericardium
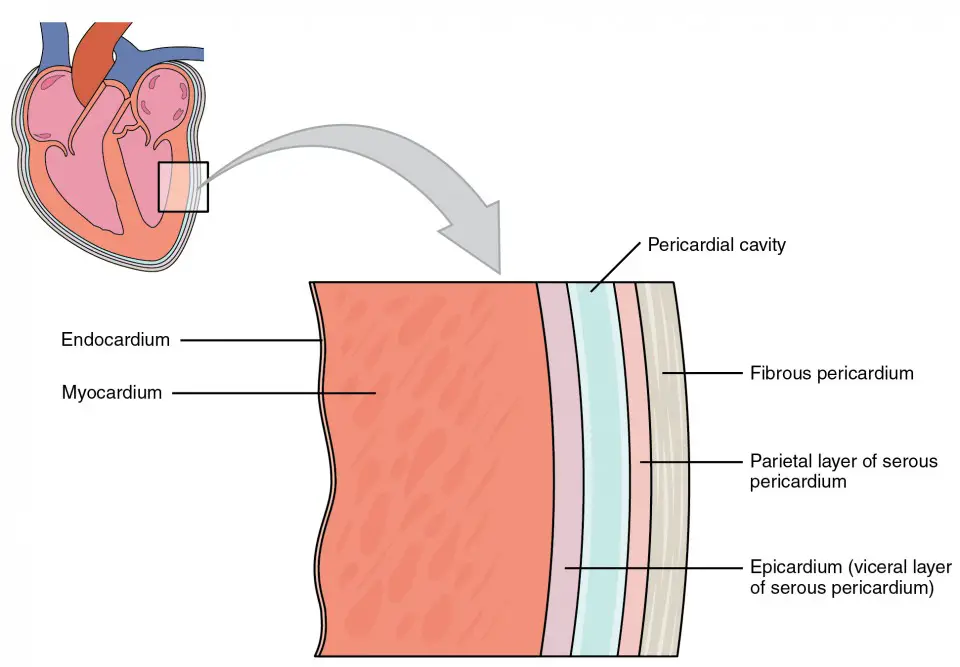
- The pericardium is a vital structure that surrounds and protects the heart. It consists of two layers: the fibrous pericardium and the serous pericardium.
- The fibrous pericardium is the outer layer of the pericardium and is composed of strong connective tissues. It forms a closed space within the mid-mediastinum, creating the pericardial space. Posteriorly, it fuses with the central tendon layer of the diaphragm, while anteriorly, it blends with the outer layer of the great vessels. Ventral to the heart, it is fused with the posterior end of the sternum, effectively sealing and enclosing the heart within a protective sac. The fibrous pericardium provides mechanical protection to the heart, helping to prevent excessive movement and ensuring the heart maintains its position within the thoracic cavity.
- The serous pericardium, the internal layer of the pericardium, is a double-layered membrane consisting of mesothelium, a single layer of epithelium. This layer secretes the pericardial fluid. The outer layer of the serous pericardium, which lines the fibrous pericardium, is called the parietal serous pericardium. Between the parietal and visceral serous pericardium, there exists a small cavity called the pericardial cavity. This cavity is filled with the pericardial fluid, which serves crucial functions in heart function and protection.
- The pericardial fluid acts as a lubricant, reducing friction between the layers of the pericardium during the contraction and relaxation of the cardiac muscles. This allows the heart to beat smoothly without unnecessary resistance or wear. Moreover, the fluid provides a cushioning effect, protecting the heart from mechanical shocks or trauma that may occur due to sudden movements or external forces.
- The visceral serous pericardium, also known as the epicardium, forms the inner layer of the serous pericardium. It continues seamlessly with the outer surface of the heart wall, covering the myocardium. The epicardium provides a smooth surface for the heart’s movements within the pericardial cavity.
- In summary, the pericardium is a double-layered membrane that encloses and safeguards the heart. The fibrous pericardium, the outer layer, offers mechanical protection and structural support. The serous pericardium, consisting of the parietal and visceral layers, secretes the pericardial fluid, which lubricates the heart and shields it from friction and mechanical shocks. The pericardium, with its layered structure and functions, plays a crucial role in maintaining the health and integrity of the heart.
Functions of Pericardium
The pericardium serves several important functions that contribute to the overall protection and proper functioning of the heart.
- First and foremost, the pericardium acts as a robust physical barrier, shielding the heart from mechanical shock, friction, and potential infection. Its tough and fibrous nature provides a protective layer around the heart, reducing the risk of external trauma that could damage this vital organ. Additionally, the pericardium helps prevent the heart from coming into direct contact with other structures in the thoracic cavity, minimizing the risk of friction and abrasion during the heart’s contractions and movements.
- The pericardium also plays a crucial role in anchoring and securing the heart within the mediastinum, the central compartment of the chest. By firmly attaching to the diaphragm posteriorly and merging with the great vessels anteriorly, the pericardium helps maintain the heart in its proper anatomical position. This stability is essential for the heart to function optimally and ensures that its intricate network of blood vessels and conduction pathways remain properly aligned.
- One of the significant functions of the pericardium is the secretion of pericardial fluid. The serous pericardium, specifically the parietal layer, produces this fluid, which fills the pericardial cavity. The pericardial fluid acts as a lubricant, reducing friction between the layers of the pericardium and allowing the heart to beat and contract smoothly. This lubrication is vital during the contraction and relaxation process of the heart muscles, ensuring that the heart’s movements are not impeded by excessive friction.
- Furthermore, the pericardium acts as a limiting membrane, preventing the heart from over-expanding and over-filling. By serving as a tough and relatively inflexible structure, the pericardium restricts the expansion of the heart chambers beyond their optimal capacity. This limitation helps maintain the heart’s efficiency in pumping blood and prevents the chambers from becoming excessively distended.
In summary, the functions of the pericardium encompass protection, stability, lubrication, and limitation. It safeguards the heart from mechanical shock, friction, and infection, while also anchoring it securely within the mediastinum. The secretion of pericardial fluid ensures smooth movements of the heart during its contraction and relaxation phases. Additionally, the pericardium acts as a limiting membrane, preventing over-expansion and over-filling of the heart chambers. Altogether, these functions contribute to the overall well-being and optimal functioning of the heart.
Chambers and Circulation through the Heart
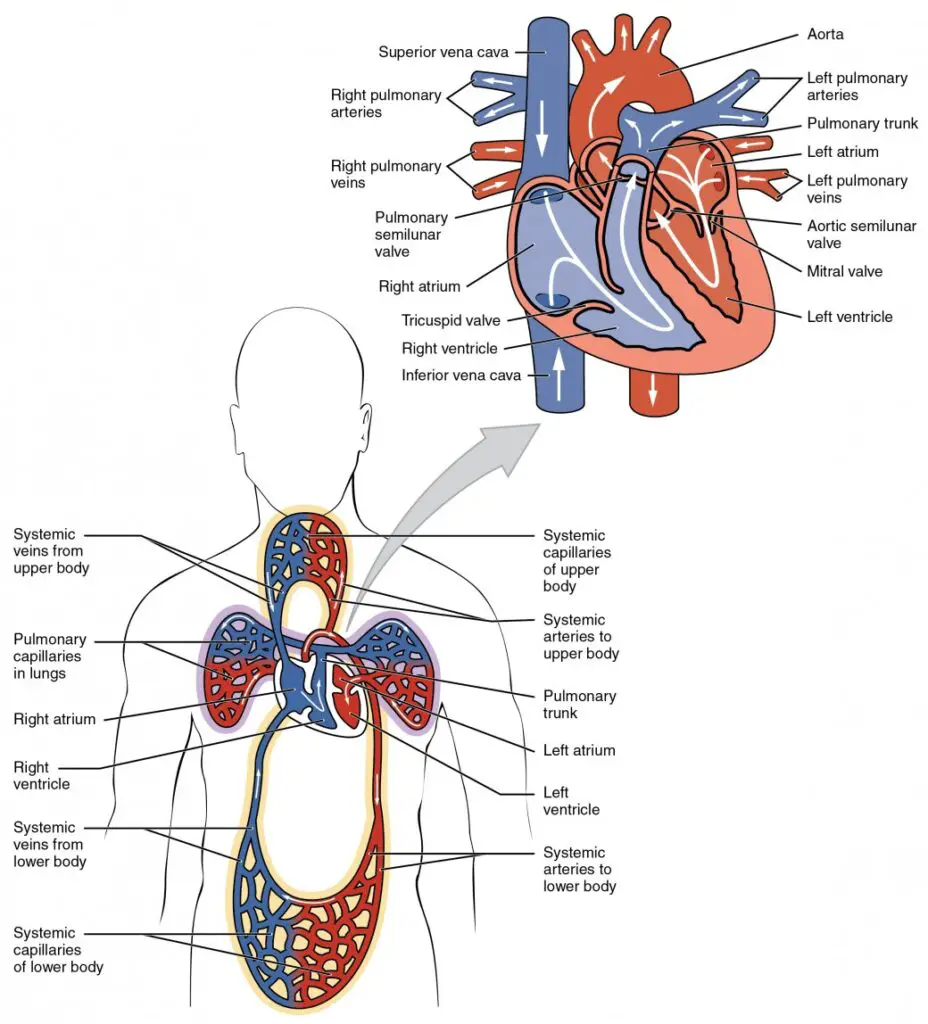
- The human heart is comprised of four chambers: two atria and two ventricles. The atria, consisting of the right atrium and left atrium, serve as receiving chambers that contract to push blood into the lower chambers, the right ventricle and left ventricle, respectively. The ventricles function as the primary pumping chambers of the heart, propelling blood to either the lungs or the rest of the body.
- The circulation through the heart involves two interconnected circuits: the pulmonary circuit and the systemic circuit. The pulmonary circuit transports blood to and from the lungs, where it picks up oxygen and eliminates carbon dioxide during exhalation. On the other hand, the systemic circuit distributes oxygenated blood to virtually all the body’s tissues and returns relatively deoxygenated blood and carbon dioxide back to the heart to be sent back to the pulmonary circulation.
- The journey of blood through the pulmonary circuit begins with the right ventricle pumping deoxygenated blood into the pulmonary trunk, which then bifurcates into the left and right pulmonary arteries. These arteries further branch out until they reach the pulmonary capillaries, where gas exchange occurs. Carbon dioxide exits the blood, and oxygen enters it. It’s important to note that the pulmonary trunk arteries and their branches are the only arteries in the post-natal body that carry relatively deoxygenated blood. Highly oxygenated blood from the pulmonary capillaries travels through a network of vessels that merge to form the pulmonary veins, which are the only post-natal veins in the body that carry highly oxygenated blood. The pulmonary veins transport the oxygenated blood into the left atrium. From there, the blood is pumped into the left ventricle, which subsequently propels oxygenated blood into the aorta, initiating the systemic circuit. The aorta and its branches distribute the oxygenated blood to various parts of the body, ultimately reaching the systemic capillaries, where exchange with the tissue fluid and cells occurs. In this process, oxygen and nutrients exit the systemic capillaries to be used by the cells in their metabolic processes, while carbon dioxide and waste products enter the bloodstream.
- As the blood exits the systemic capillaries, it has a lower concentration of oxygen than when it initially entered. The capillaries gradually merge to form venules, which then combine to form larger veins that eventually flow into the two major systemic veins: the superior vena cava and the inferior vena cava. These veins return the blood to the right atrium, completing the circulation cycle. This continuous process of blood circulation persists as long as the individual remains alive.
- Understanding the flow of blood through the pulmonary and systemic circuits is essential for all healthcare professionals, as it provides crucial insights into the functioning of the cardiovascular system and its role in maintaining overall health.
External Structure of Heart – Membranes, Surface Features, and Layers
The membrane that surrounds the heart, the prominent surface features of the heart, and the layers that comprise the wall of the heart are the first structures of the heart that will be examined in detail. In terms of function, each of these components performs a distinct role.
Membranes
- Membranes play a crucial role in various aspects of the body’s anatomy and physiology. One important membrane is the pericardium, also known as the pericardial sac, which directly surrounds the heart and defines the pericardial cavity. It not only encompasses the heart but also extends to the “roots” of the major vessels closest to the heart.
- The pericardium consists of two distinct sublayers: the fibrous pericardium and the serous pericardium. The fibrous pericardium is the outer layer made of tough and dense connective tissue. It serves to protect the heart and maintain its position within the thoracic cavity. On the other hand, the serous pericardium is a more delicate layer composed of two sublayers.
- The parietal pericardium, fused to the fibrous pericardium, forms the outer layer of the serous pericardium. The inner layer, known as the visceral pericardium or epicardium, is fused to the heart and is actually part of the heart wall. The visceral pericardium is a macroscopic layer rather than a microscopic one, consisting of a simple squamous epithelium called a mesothelium. It is reinforced with loose, irregular, or areolar connective tissue that attaches to the pericardium.
- The mesothelium of the visceral pericardium plays a vital role by secreting a lubricating serous fluid. This fluid fills the pericardial cavity, which lies between the visceral pericardium (epicardium) and the parietal pericardium. The serous fluid acts as a lubricant, reducing friction as the heart contracts and allowing smooth movement within the pericardial cavity.
- Overall, the membranes of the pericardium, including the fibrous pericardium and the serous pericardium with its visceral and parietal layers, provide essential protection for the heart, maintain its position, and facilitate its movement within the thoracic cavity. The lubricating serous fluid produced by the mesothelium ensures minimal friction during the contraction and relaxation of the heart, contributing to its efficient functioning.
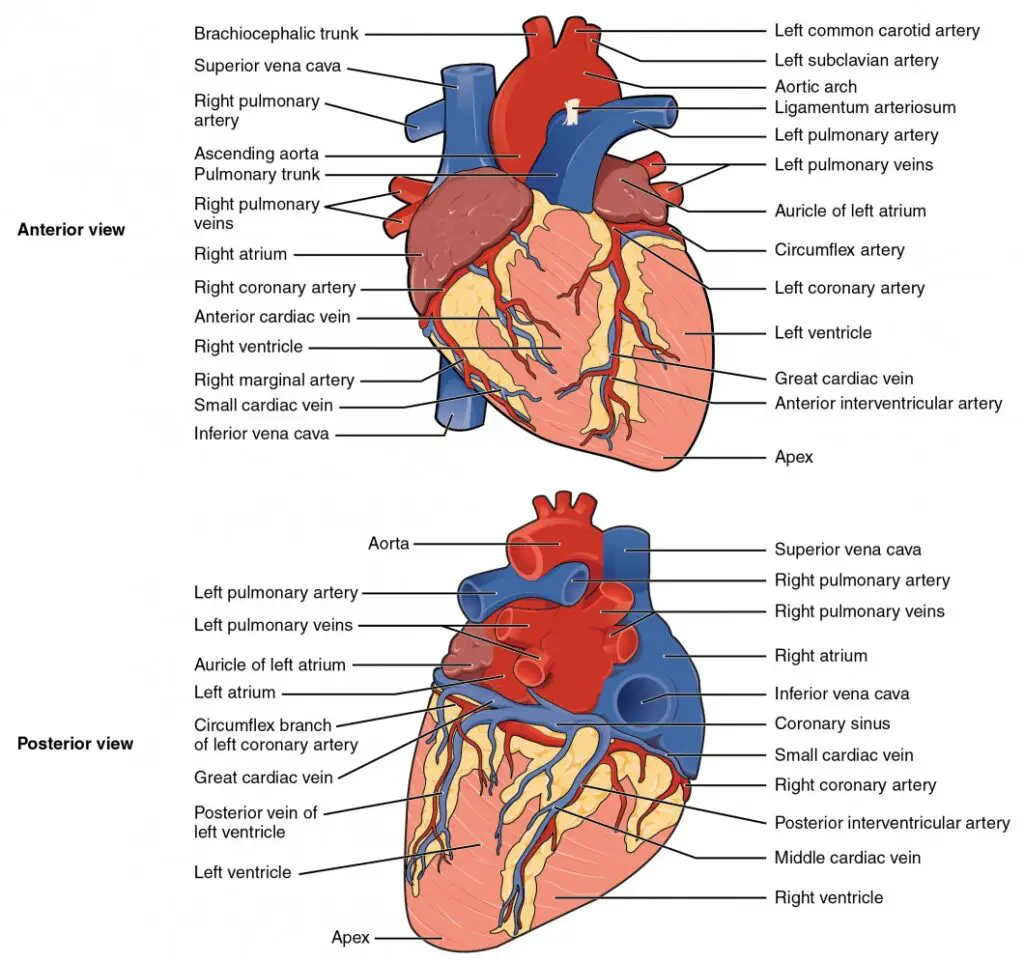
Surface Features of the Heart
- The surface features of the heart, visible within the pericardium, provide important anatomical landmarks. These features include the four chambers of the heart and various distinctive structures.
- One notable feature on the superior surface of the heart is the presence of auricles, which are superficial leaf-like extensions of the atria. These auricles, resembling the shape of human ears, can be found on each side of the heart. They are also referred to as atrial appendages and serve as relatively thin-walled structures that can fill with blood and empty into the atria or upper chambers of the heart.
- In addition to the auricles, there are distinct fat-filled grooves on the superior surface of the heart known as sulci (singular: sulcus). These sulci serve as important landmarks and house major coronary blood vessels. One significant sulcus is the deep coronary sulcus, which is located between the atria and ventricles. This sulcus plays a crucial role in housing and protecting the major coronary blood vessels.
- Between the left and right ventricles, there are two additional sulci that are not as deep as the coronary sulcus. The first is the anterior interventricular sulcus, which is visible on the anterior (front) surface of the heart. The second is the posterior interventricular sulcus, which can be seen on the posterior (back) surface of the heart. These sulci also contain important blood vessels and contribute to the overall surface features of the heart.
- The surface features of the heart, including the auricles and sulci, provide visual clues that aid in identifying and understanding the anatomical structure of the heart. They help in distinguishing different regions of the heart and serve as points of reference for the major coronary blood vessels that supply the cardiac muscle with oxygen and nutrients.
Layers
The wall of the heart is composed of three distinct layers, each with its own unique characteristics and functions. These layers, from outermost to innermost, are the epicardium, the myocardium, and the endocardium.
- The outermost layer of the heart wall is the epicardium, which is also referred to as the visceral pericardium since it is continuous with the inner layer of the pericardium. The epicardium is a thin layer that covers the surface of the heart and provides protection. It consists of connective tissue and is supported by a layer of adipose tissue.
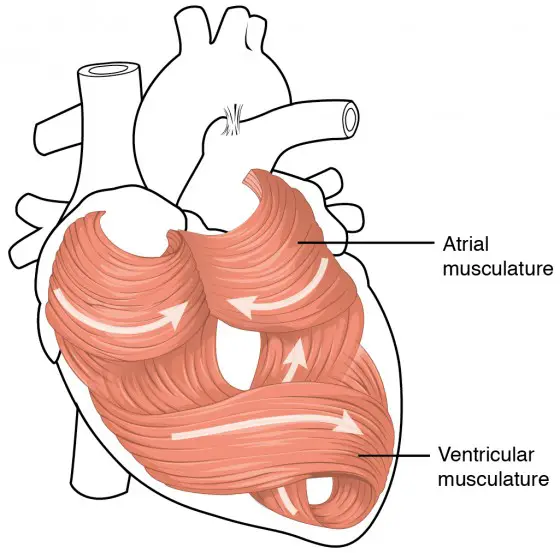
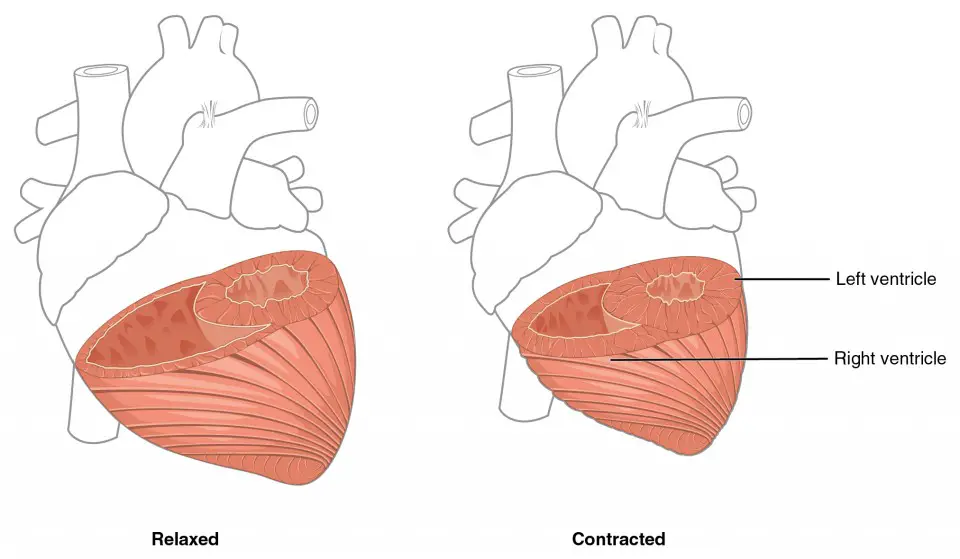
- Beneath the epicardium lies the myocardium, the middle and thickest layer of the heart wall. The myocardium is predominantly composed of cardiac muscle cells. It is responsible for the contraction of the heart, enabling it to pump blood effectively. The myocardium is reinforced by collagenous fibers, blood vessels, and nerve fibers that regulate the heart’s activity. The arrangement of muscle cells within the myocardium forms an intricate swirling pattern, contributing to the heart’s pumping efficiency. This pattern allows the muscle cells to contract in a coordinated manner, facilitating the expulsion of blood from the chambers. The left ventricle, which pumps blood into the systemic circuit, has a thicker and more developed myocardium compared to the right ventricle, which pumps blood into the pulmonary circuit. This difference in muscle thickness reflects the varying pressure requirements of the two ventricles.
- The innermost layer of the heart wall is the endocardium. It is a thin layer of tissue that lines the chambers of the heart and covers the heart valves. The endocardium is composed of simple squamous epithelium called endothelium, which is continuous with the endothelial lining of blood vessels. This layer provides a smooth surface that promotes the smooth flow of blood through the heart chambers. Recent research suggests that the endothelium of the endocardium and coronary capillaries may play active roles in regulating cardiac muscle contraction and growth patterns. The endothelium secretes substances known as endothelins, which influence factors such as ionic concentrations and contractility in the surrounding tissue fluids. Endothelins also have vasoconstrictor effects, contributing to the regulation of blood vessel diameter.
The three layers of the heart wall—the epicardium, myocardium, and endocardium—work together to ensure the efficient pumping of blood and provide necessary protection and structural support.
Internal Structure of the Heart
Due to the pairings of chambers that pump blood into the circulatory system, the heart’s contraction cycle follows a dual pattern of circulation (pulmonary and systemic circuits). To gain a more precise understanding of cardiac function, it is necessary to investigate the internal anatomical structures in greater depth.
Septa of the Heart
- The septa of the heart play a crucial role in dividing and structurally supporting the heart’s chambers. Derived from the Latin word for “something that encloses,” septa refer to walls or partitions that separate different areas within the heart.
- One of the septa in the heart is the interatrial septum, located between the two atria. In adults, the interatrial septum features a depression known as the fossa ovalis. Interestingly, this depression is a remnant of the foramen ovale, an opening present in the fetal heart. During fetal development, the foramen ovale allowed blood to bypass the pulmonary circuit by directly passing from the right atrium to the left atrium. However, shortly after birth, the foramen ovale is closed by a tissue flap called the septum primum, establishing the typical circulation pattern of the heart.
- Another important septum is the interventricular septum, situated between the two ventricles. Unlike the interatrial septum, the interventricular septum remains intact after its formation during fetal development. It is considerably thicker than the interatrial septum due to the greater pressure generated by the ventricles during contraction.
- The septum that separates the atria and ventricles is known as the atrioventricular septum. It contains four openings that allow blood to flow from the atria into the ventricles, as well as from the ventricles into the pulmonary trunk and aorta. Each of these openings is equipped with a valve, ensuring the one-way flow of blood. The valves between the atria and ventricles are called atrioventricular valves, while the valves at the openings leading to the pulmonary trunk and aorta are known as semilunar valves.
- To maintain the structural integrity of the atrioventricular septum, it is reinforced with dense connective tissue called the cardiac skeleton or the skeleton of the heart. The cardiac skeleton comprises four rings that encircle the openings between the atria and ventricles, as well as the openings to the pulmonary trunk and aorta. These rings also serve as attachment points for the heart valves. Additionally, the cardiac skeleton plays a crucial role in the heart’s electrical conduction system by providing boundaries and pathways for the transmission of electrical impulses.
- In summary, the septa of the heart, including the interatrial septum, interventricular septum, and atrioventricular septum, are essential for dividing the heart into chambers and maintaining the proper flow of blood. These structures, along with the cardiac skeleton, contribute to the intricate functioning of the heart, ensuring its efficient pumping action and circulation throughout the body.
Right Atrium
- The right atrium is an essential component of the heart responsible for receiving blood that returns from the systemic circulation. It acts as a receiving chamber for the major systemic veins, namely the superior and inferior vena cavae, as well as the coronary sinus.
- The superior vena cava collects blood from areas above the diaphragm, including the head, neck, upper limbs, and thoracic region. It enters the superior and posterior portions of the right atrium, ensuring the delivery of deoxygenated blood to the heart. On the other hand, the inferior vena cava gathers blood from regions below the diaphragm, such as the lower limbs and abdominopelvic area. It enters the posterior section of the right atrium, below the opening of the superior vena cava. Adjacent to the inferior vena cava’s opening on the posterior surface of the atrium lies the entrance of the coronary sinus. This thin-walled vessel drains the majority of the coronary veins, which carry deoxygenated blood from the heart’s myocardium back into the right atrium.
- The internal surface of the right atrium displays distinct features. While most of the surface is smooth, there is a noticeable depression called the fossa ovalis in the medial region. On the anterior surface, prominent muscular ridges known as pectinate muscles are present. These muscles also extend into the right auricle. It is worth noting that the left atrium lacks pectinate muscles, except for those found in its auricle.
- The atria continuously receive venous blood to ensure a constant flow, even while the ventricles are contracting. Although most ventricular filling occurs when the atria are relaxed, they also exhibit a contractile phase where they actively pump blood into the ventricles just before ventricular contraction. The opening between the atrium and ventricle is guarded by the tricuspid valve, which prevents the backflow of blood and ensures unidirectional flow through the heart.
- The right atrium’s role in receiving deoxygenated blood from the systemic circulation is vital for the heart’s overall function. It serves as an intermediary between the major veins and the ventricles, ensuring a steady flow of blood and facilitating the subsequent pumping of oxygen-depleted blood to the lungs for oxygenation.
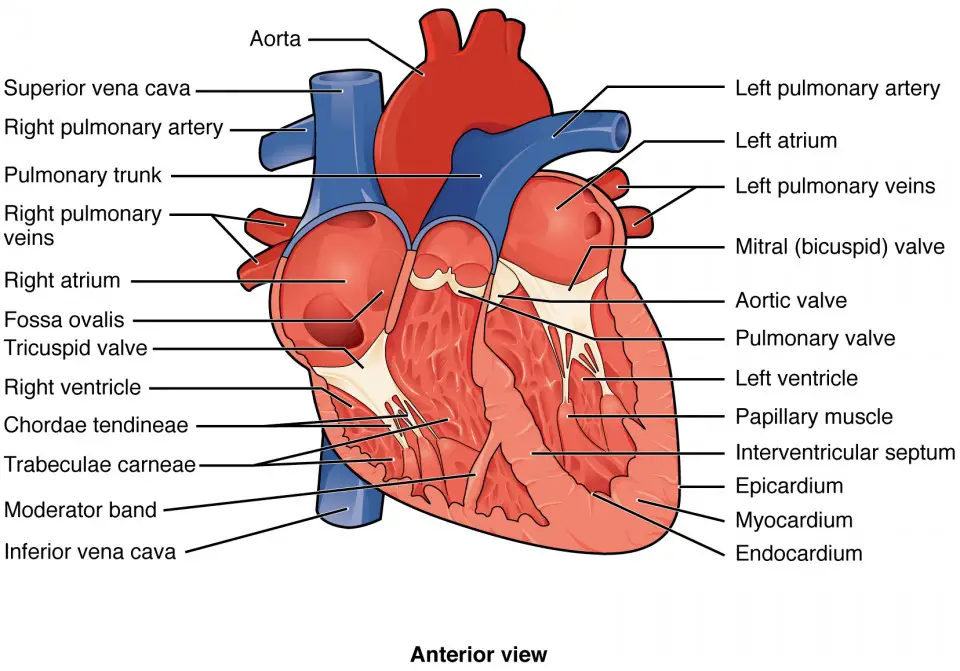
Right Ventricle
- The right ventricle is an important chamber of the heart that receives blood from the right atrium through the tricuspid valve. The tricuspid valve consists of flaps attached to strong strands of connective tissue called chordae tendineae, also known as “heart strings.” Each flap is connected to several chordae tendineae, which are primarily composed of collagenous fibers along with elastic fibers and endothelium. These tendinous cords extend from the flaps to papillary muscles located on the inferior surface of the ventricle. The right ventricle contains three papillary muscles: the anterior, posterior, and septal muscles, corresponding to the three sections of the tricuspid valve.
- During ventricular contraction, the myocardium of the right ventricle generates increased pressure within the chamber. Blood naturally flows from areas of higher pressure to lower pressure, in this case, toward the pulmonary trunk and the atrium. To prevent any backflow of blood, the papillary muscles contract and exert tension on the chordae tendineae. This tension ensures that the flaps of the tricuspid valve remain closed and prevent the blood from being forced back into the atrium. This mechanism is crucial in preventing regurgitation of blood during ventricular contraction. The image of the papillary muscles and chordae tendineae attached to the tricuspid valve provides a visual representation of this structure.
- The walls of the right ventricle are lined with ridges of cardiac muscle called trabeculae carneae, which are covered by the endocardium. These muscular ridges contribute to the efficient contraction of the ventricle. Additionally, there is a specialized band of cardiac muscle covered by the endocardium known as the moderator band. It arises from the inferior part of the interventricular septum and crosses the interior space of the right ventricle to connect with the inferior papillary muscle. The moderator band plays a crucial role in cardiac conduction and helps reinforce the thin walls of the right ventricle.
- During contraction, the right ventricle ejects blood into the pulmonary trunk, which further divides into the left and right pulmonary arteries. These arteries carry oxygen-depleted blood to the lungs for oxygenation. As the superior surface of the right ventricle approaches the pulmonary trunk, it begins to taper. At the base of the pulmonary trunk, there is the pulmonary semilunar valve, which prevents backflow of blood from the pulmonary trunk into the right ventricle.
- The right ventricle’s primary function is to pump deoxygenated blood to the lungs for oxygenation. Its structures, including the tricuspid valve, chordae tendineae, papillary muscles, trabeculae carneae, moderator band, and pulmonary semilunar valve, work in harmony to ensure efficient blood flow and prevent backflow during the cardiac cycle.
Left Atrium
- The left atrium is a crucial component of the heart responsible for receiving oxygenated blood from the pulmonary circulation. Following the exchange of gases in the pulmonary capillaries, blood returns to the left atrium through the four pulmonary veins. These pulmonary veins deliver blood that is rich in oxygen to the left atrium.
- Unlike the right atrium, the left atrium does not contain pectinate muscles on its internal surface. However, it does have an auricle that includes pectinate ridges. The blood flows continuously from the pulmonary veins back into the left atrium, which serves as the receiving chamber. From here, the blood moves through an opening into the left ventricle. The left atrium acts as a passive conduit for the majority of the blood flow into the heart, occurring when both the atria and ventricles are relaxed. However, towards the end of the ventricular relaxation period, the left atrium contracts, actively pumping blood into the left ventricle. This atrial contraction contributes to approximately 20 percent of ventricular filling.
- The opening between the left atrium and left ventricle is guarded by the mitral valve, also known as the bicuspid valve. The mitral valve consists of two flaps, or cusps, which prevent the backflow of blood from the ventricle into the atrium during ventricular contraction. It ensures the unidirectional flow of blood through the heart.
- The left atrium plays a crucial role in the circulation of oxygenated blood. It receives blood from the pulmonary veins and actively contributes to the filling of the left ventricle. The mitral valve ensures that blood moves forward into the left ventricle while preventing any backflow. The coordinated functioning of the left atrium and its associated structures ensures the efficient delivery of oxygen-rich blood to the systemic circulation, supporting the overall functioning of the cardiovascular system.
Left Ventricle
- The left ventricle, a crucial component of the heart, plays a vital role in the systemic circulation. It is worth noting that although both sides of the heart pump the same volume of blood, the left ventricle possesses a significantly thicker muscular layer compared to the right ventricle. This increased thickness is necessary to generate the force required to propel oxygenated blood throughout the entire systemic circuit.
- Similar to the right ventricle, the left ventricle contains trabeculae carneae, which are ridges of cardiac muscle covered by the endocardium. However, unlike the right ventricle, there is no moderator band present in the left ventricle. The moderator band is a specialized structure found only in the right ventricle that plays a role in cardiac conduction.
- The left ventricle is connected to the mitral valve, also known as the bicuspid valve, through chordae tendineae. These tendinous cords attach the valve’s flaps to papillary muscles within the ventricle. Unlike the right ventricle, which has three papillary muscles, the left ventricle has two papillary muscles: the anterior and posterior papillary muscles. These papillary muscles are instrumental in maintaining the proper functioning of the mitral valve, ensuring that it closes tightly and prevents the backflow of blood into the left atrium during ventricular contraction.
- The primary function of the left ventricle is to pump oxygenated blood into the systemic circuit. When the left ventricle contracts, it ejects blood into the aorta through the aortic semilunar valve, which guards the opening between the ventricle and the aorta. The aortic semilunar valve prevents the backflow of blood from the aorta into the left ventricle, ensuring the unidirectional flow of blood and efficient distribution of oxygenated blood to the body’s tissues and organs.
- The left ventricle’s powerful contraction and the expulsion of blood into the systemic circuit are vital for sustaining the body’s oxygen supply. Its robust muscular layer, along with the mitral valve and aortic semilunar valve, works in harmony to ensure the effective propulsion of blood and maintain the integrity of the systemic circulation.
Heart Valve Structure and Function
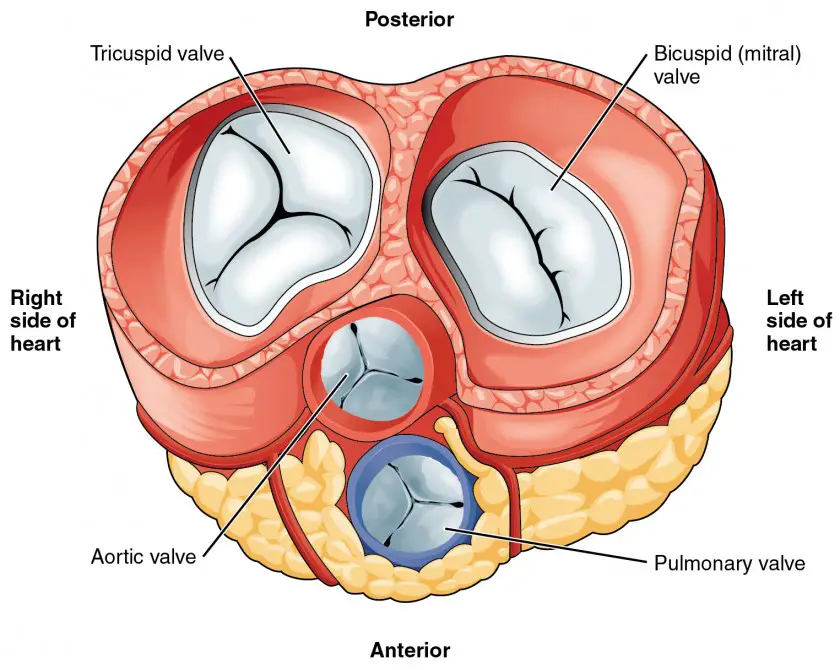
- Heart valves play a crucial role in maintaining the unidirectional flow of blood through the heart. There are four main valves: the tricuspid valve, pulmonary valve, mitral valve, and aortic valve. Each valve has a unique structure and function that ensures efficient circulation.
- The right atrioventricular valve, also known as the tricuspid valve, is located between the right atrium and the right ventricle. It consists of three flaps, or leaflets, made of endocardium and reinforced with connective tissue. These flaps are connected to the papillary muscles by chordae tendineae, which control the opening and closing of the valve. The tricuspid valve prevents backflow of blood from the right ventricle to the right atrium during ventricular contraction.
- The pulmonary valve, also called the pulmonary semilunar valve or pulmonic valve, is positioned at the base of the pulmonary trunk, emerging from the right ventricle. It comprises three small flaps of endothelium reinforced with connective tissue. When the ventricle relaxes, the pressure difference causes blood to flow back into the ventricle from the pulmonary trunk. This flow of blood fills the pocket-like flaps of the pulmonary valve, causing the valve to close and creating an audible sound. Unlike the atrioventricular valves, the pulmonary valve does not have papillary muscles or chordae tendineae associated with it.
- On the left side of the heart, the left atrioventricular valve, known as the mitral valve or bicuspid valve, is located between the left atrium and the left ventricle. It consists of two cusps, the anterior medial cusp and the posterior medial cusp. The cusps are attached to papillary muscles by chordae tendineae, which are projections from the ventricular wall. The mitral valve prevents backflow of blood from the left ventricle to the left atrium during ventricular contraction.
- At the base of the aorta, the aortic valve, also called the aortic semilunar valve, prevents backflow from the aorta into the left ventricle. It is composed of three flaps. When the ventricle relaxes and blood tries to flow back into the ventricle from the aorta, the cusps of the valve fill with blood, causing the valve to close and producing an audible sound.
- The atrioventricular valves (tricuspid and mitral) are closed while the semilunar valves (pulmonary and aortic) are open when the ventricles contract to eject blood into the pulmonary trunk and aorta. This prevents blood from being forced back into the atria. When the ventricles begin to contract, the pressure rises, and blood flows toward the atria. The cusps of the atrioventricular valves close, held in place by the tension created by the contraction of the papillary muscles and the chordae tendineae.
- In contrast, the aortic and pulmonary semilunar valves lack chordae tendineae and papillary muscles. They consist of pocket-like folds of endocardium reinforced with additional connective tissue. When the ventricles relax and the pressure changes, blood presses against these cusps, sealing the openings and preventing backflow.
- Overall, the structure and coordinated function of the heart valves ensure efficient blood flow through the heart, preventing regurgitation and maintaining circulation throughout the systemic and pulmonary circuits.
Disorders of the Heart Valves
- Disorders of the heart valves, known as valvular heart disease, can range from benign to life-threatening and may be congenital, acquired through disease processes, or caused by trauma. When heart valves become incompetent and fail to function properly, they can disrupt the normal flow of blood through the heart.
- Valvular disorders often result from carditis, which is inflammation of the heart. Rheumatic fever, an autoimmune response triggered by Streptococcus pyogenes infection, is a common cause of this inflammation. While any of the heart valves can be affected, mitral regurgitation is the most common valvular disorder, while the pulmonary semilunar valve is least frequently involved.
- When a valve malfunctions, blood flow to a specific region can be disrupted, leading to inadequate blood flow, or insufficiency, in that area. The type of insufficiency is named after the valve involved, such as aortic insufficiency, mitral insufficiency, tricuspid insufficiency, or pulmonary insufficiency.
- A prolapsed valve occurs when one of the cusps of the valve is forced backward, often due to damage or breakage of the chordae tendineae. This failure of the valve to close properly results in regurgitation, where blood flows backward from its normal path. A heart murmur, detected using a stethoscope, is often present as a result of the disrupted blood flow.
- Stenosis is another valvular disorder characterized by the rigidity and calcification of the heart valves over time. This loss of flexibility interferes with normal valve function, causing the heart to work harder to pump blood through the narrowed valve. Aortic stenosis, in particular, is more prevalent in older individuals. In some cases, chordae tendineae tears or the papillary muscle may be affected due to a myocardial infarction (heart attack), requiring immediate surgical intervention.
- Auscultation, the act of listening to a patient’s heart sounds, is a valuable diagnostic tool for detecting valve and septal disorders. It is a safe, proven, and inexpensive method. Abnormal heart sounds can indicate the presence of a valvular disorder. In cases where a valvular disorder is suspected, an echocardiogram, also known as an “echo,” may be performed. Echocardiograms use sound waves to create images of the heart and can help diagnose valve disorders as well as various other heart conditions.
- Overall, disorders of the heart valves can range from mild to severe, and the treatment approach depends on the specific condition. Medications, surgical interventions, or close monitoring may be employed to manage valvular heart diseases, with the goal of restoring proper valve function and maintaining optimal blood flow through the heart.
Coronary Circulation
The coronary circulation is the specialized system of blood vessels that supplies the heart muscle, specifically the cardiomyocytes, with oxygen, nutrients, and removes metabolic waste products. This unique circulation is essential to meet the high demand for oxygen and energy required by the constantly active cardiac muscle.
Unlike other organs, coronary circulation is not continuous but rather cyclical. It reaches its peak during diastole, the relaxation phase of the cardiac cycle when the heart muscle is at rest and filling with blood. During this phase, the coronary arteries dilate and blood flow to the myocardium increases, ensuring an adequate supply of oxygen and nutrients to meet the metabolic demands of the cardiomyocytes. This is crucial for the heart to recover and prepare for the subsequent contraction.
Conversely, during systole, the contraction phase of the cardiac cycle, coronary circulation slows down significantly. The contraction of the myocardium compresses the coronary blood vessels, impeding blood flow temporarily. This reduction in blood flow during systole is known as coronary flow reduction. However, even though coronary circulation is reduced during systole, the cardiac muscle has adapted to ensure sufficient oxygen supply through stored oxygen and metabolic processes that allow for continued ATP production.
The coronary circulation consists of two main coronary arteries: the right coronary artery (RCA) and the left coronary artery (LCA). The RCA supplies blood primarily to the right side of the heart, including the right atrium and ventricle, while the LCA branches into two main arteries: the left anterior descending artery (LAD) and the left circumflex artery (LCX). The LAD supplies blood to the anterior walls of both ventricles, while the LCX provides blood to the left atrium and the lateral wall of the left ventricle.
The coronary arteries branch into smaller arterioles, which further divide into an extensive network of capillaries that permeate the myocardium. These capillaries allow for the exchange of oxygen, nutrients, and waste products between the blood and the cardiomyocytes. The deoxygenated blood from the myocardium is then collected by cardiac veins, with the major coronary vein being the coronary sinus. The coronary sinus drains into the right atrium, completing the coronary circulation cycle.
Disruptions in coronary circulation, such as blockages or reduced blood flow due to atherosclerosis or blood clots, can lead to coronary artery disease, angina, or even myocardial infarction (heart attack). These conditions highlight the critical importance of maintaining a healthy coronary circulation to ensure the proper functioning of the heart and overall cardiovascular health.
Coronary Arteries
- The coronary arteries play a vital role in supplying oxygenated blood to the myocardium and various components of the heart. Originating from the first portion of the aorta after it arises from the left ventricle, the coronary arteries consist of the left and right coronary arteries.
- The left coronary artery arises from the left posterior aortic sinus, while the right coronary artery originates from the anterior aortic sinus. These arteries run along the surface of the heart and follow the sulci, giving them the name epicardial coronary arteries. The left coronary artery is responsible for distributing blood to the left side of the heart, including the left atrium, left ventricle, and the interventricular septum.
- The circumflex artery is a branch of the left coronary artery that follows the coronary sulcus to the left and eventually fuses with small branches of the right coronary artery. The second major branch of the left coronary artery is the anterior interventricular artery, also known as the left anterior descending artery (LAD). The LAD follows the anterior interventricular sulcus around the pulmonary trunk and gives rise to smaller branches that form anastomoses with the branches of the posterior interventricular artery. These anastomoses provide alternate pathways for blood flow in case of partial blockage in one branch.
- The right coronary artery travels along the coronary sulcus and supplies blood to the right atrium, portions of both ventricles, and the heart conduction system. It typically gives rise to one or more marginal arteries below the right atrium, which supply blood to the superficial portions of the right ventricle. On the posterior surface of the heart, the right coronary artery branches into the posterior interventricular artery, also known as the posterior descending artery. This artery runs along the posterior part of the interventricular sulcus toward the apex of the heart, providing blood supply to the interventricular septum and portions of both ventricles.
- The coronary circulation is essential for maintaining the health and function of the heart muscle. Blockages or restrictions in the coronary arteries can lead to inadequate blood supply, resulting in conditions such as myocardial infarction (heart attack) and other cardiac disorders. Understanding the anatomy and distribution of the coronary arteries helps in diagnosing and treating cardiovascular conditions effectively.
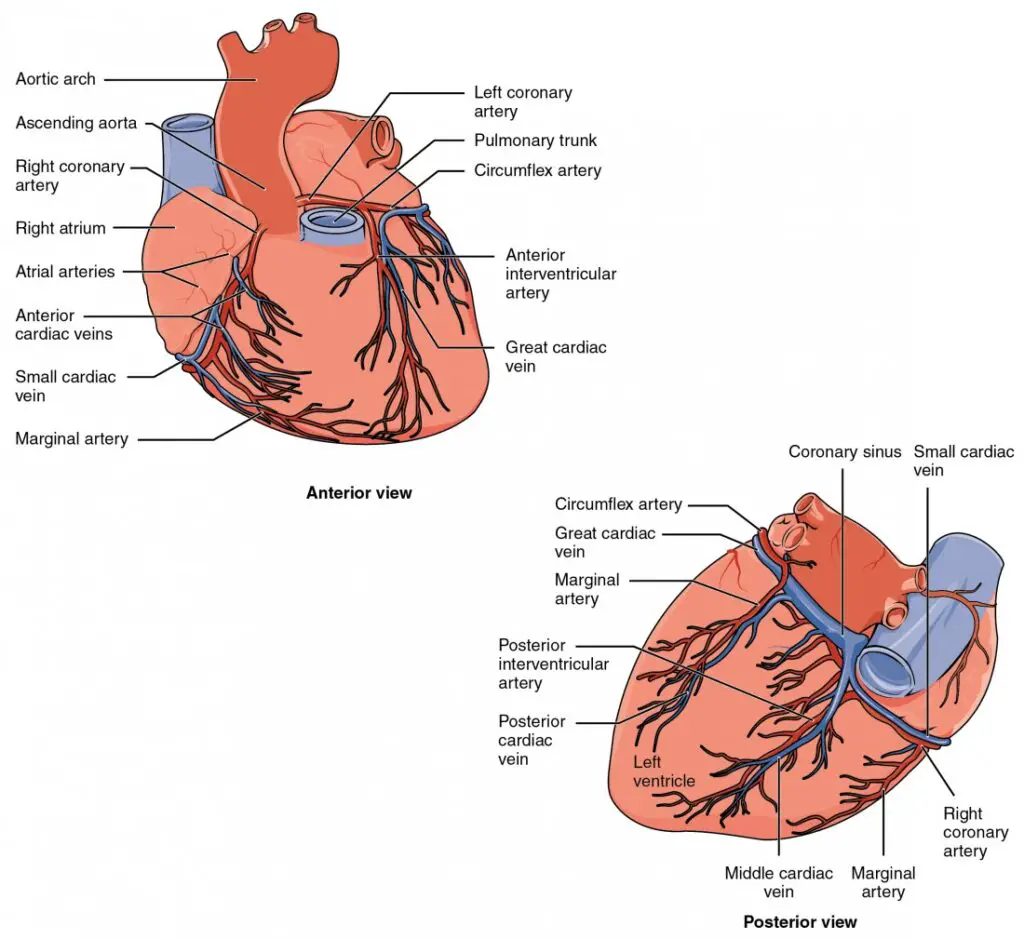
Coronary Veins
- Coronary veins generally run parallel to the major coronary arteries.
- The great cardiac vein follows the interventricular sulcus initially and then flows along the coronary sulcus into the coronary sinus on the posterior surface of the heart.
- The great cardiac vein drains the areas supplied by the anterior interventricular artery and receives several major branches:
- Posterior cardiac vein: Runs parallel to and drains the areas supplied by the marginal artery branch of the circumflex artery.
- Middle cardiac vein: Parallels and drains the areas supplied by the posterior interventricular artery.
- Small cardiac vein: Parallels the right coronary artery and drains the blood from the posterior surfaces of the right atrium and ventricle.
- The coronary sinus is a large vein located in the atrioventricular sulcus on the posterior surface of the heart and directly empties into the right atrium.
- The anterior cardiac veins parallel the small cardiac arteries and drain the anterior surface of the right ventricle.
- Unlike other cardiac veins, the anterior cardiac veins bypass the coronary sinus and drain directly into the right atrium.
Physiology of Heart
1. Blood Flow and Cardiac Cycle
- The cardiac cycle is the regular contraction and relaxation of the heart chambers for blood circulation.
- A cardiac cycle is completed in about 0.8 seconds in humans.
- The cardiac cycle consists of two major stages: systole and diastole.
- Systole is the stage where the heart chambers contract to expel blood.
- There are two systole stages: atrial systole and ventricular systole.
- Atrial systole is the contraction of the atrial wall to pump blood from the atria to the ventricles.
- Ventricular systole is the contraction of the ventricular walls to pump blood into the arteries, expelling it from the heart.
- Diastole is the stage where the heart chambers relax, allowing blood to flow in.
- There are two diastole stages: atrial diastole and ventricular diastole.
- Atrial diastole is when the pressure inside the atria decreases, allowing blood from major veins to flow in and collect inside the atria.
- Ventricular diastole is the stage where blood from the atria enters the ventricles.
- Blood flow cycle:
- Deoxygenated blood is collected by veins and poured into the right atrium via the superior and inferior vena cava during atrial diastole.
- From the right atrium, deoxygenated blood is passed to the right ventricle during ventricular diastole (or atrial systole).
- The blood is then pumped to the lungs for purification via the pulmonary arteries during ventricular systole.
- In the alveoli of the lungs, gaseous exchange occurs, oxygenating the blood.
- The oxygenated blood is taken back to the left atrium via pulmonary veins during atrial diastole.
- From the left atrium, the oxygenated blood is passed to the left ventricle and distributed throughout the body via systemic arteries during ventricular diastole and ventricular systole, respectively.
2. Cardiac Conduction Pathway and Transmission Process
- The cardiac impulse is conducted in a fixed channel called the conduction pathway.
- The SA node generates the action potential and builds up the impulse.
- The impulse is transmitted over the intermodal tract and Bachmann’s bundle in the atrial walls.
- Transmission speed in the intermodal tract and Bachmann’s bundle is 0.07 meters per second.
- The impulse is then collected by the AV node.
- The AV node delays the impulse for about 0.09 seconds.
- The impulse is relayed to the AV bundle, which connects the AV node to the Bundle of His.
- The AV bundle carries the action potential up to the Bundle of His at a speed of 0.05 meters per second.
- The Bundle of His and its branches have higher electrical conductivity.
- Transmission speed in the Bundle of His and its branches is 2 meters per second.
- The Purkinje fibers receive the impulse from the Bundle of His.
- The Purkinje fibers conduct the impulse throughout the ventricular wall, resulting in ventricular contraction.
- The Purkinje fibers have the highest conduction speed of 4 meters per second.
- The interventricular septum transmits the impulse at a speed of 0.16 meters per second.
- The lateral ventricular wall transmits the impulse at a speed of 0.2 meters per second.
- The lowermost ventricular wall transmits the impulse at a speed of 0.18 meters per second.
Function of Heart
- Pumping of Blood: The heart contracts and relaxes to pump blood throughout the body and circulate it back for re-circulation.
- Generation and Transmission of Cardiac Impulses: The heart’s conduction system generates and transmits electrical impulses to regulate the heartbeat.
- Maintenance of Blood Pressure: Atrial systole and diastole contribute to maintaining blood pressure within the human body.
- Oxygenation of Blood: The heart receives deoxygenated blood and pumps it to the lungs for purification and re-oxygenation.
- Delivery of Oxygen and Nutrients: The heart ensures the delivery of oxygen and nutrients to all tissues and organs through the circulatory system.
- Removal of Waste Products: The heart helps in removing waste products, such as carbon dioxide, from the body by pumping deoxygenated blood to the lungs for exhalation.
- Regulation of Body Temperature: The heart plays a role in regulating body temperature by distributing heat throughout the body.
- Hormone Transport: The heart assists in transporting hormones and other signaling molecules to various parts of the body for proper physiological regulation.
- Immune Function: The heart contributes to immune function by transporting immune cells and antibodies throughout the body to fight infections and maintain overall health.
- Maintenance of Homeostasis: The heart helps maintain homeostasis by coordinating with other organs and systems to regulate blood volume, electrolyte balance, and acid-base balance.
Diseases Associated with the Heart
- Pericardial Effusion: Accumulation of excessive fluid in the pericardial space.
- Pericarditis: Swelling and inflammation of the pericardium, often caused by infections.
- Endocarditis: Inflammation of the endocardium, usually resulting from a bacterial infection.
- Stenosis: Narrowing of blood vessels, which restricts blood flow.
- Coronary Artery Disease (Ischemic Heart Disease): Build-up of cholesterol plaques in the coronary arteries, leading to reduced blood flow to the heart.
- Angina Pectoris: Chest pain caused by inadequate blood supply to the heart muscles.
- Myocardial Infarction (Heart Attack): Damage to the cardiac muscle due to a complete blockage of blood supply.
- Cardiomyopathy: Weakening of the cardiac muscle or a decline in its ability to pump blood effectively.
- Cardiac Arrest: Sudden loss of heart function, often resulting in the cessation of blood circulation.
- Heart Valve Disease: Dysfunction or decline in the function of one or more heart valves.
- Arrhythmia: Irregular heartbeat, characterized by abnormal electrical activity in the heart.
- Heart Murmur: Abnormal sound produced during a heartbeat, often indicating a valve problem.
- Mitral Valve Prolapse: Condition where the mitral valve of the heart is slightly pushed backward during contraction.
Conducting System of Heart Beat
- The heart’s conducting system plays a crucial role in regulating the heartbeat and ensuring coordinated contractions of the cardiac muscle. The heart possesses the property of autorhythmicity, meaning it generates its own electrical impulses and beats independently of nervous and hormonal control. However, it is also supplied with autonomic nerve fibers from the sympathetic and parasympathetic divisions of the nervous system, as well as regulated by circulating hormones like adrenaline and thyroxine.
- The initiation of the electrical impulse for the heartbeat begins with the sinoatrial (SA) node, which is a small mass of specialized cells located in the wall of the right atrium near the opening of the superior vena cava. The SA node is electrically unstable and acts as the natural pacemaker of the heart. It generates the electrical impulse and controls the rhythm of the heartbeat. Due to their electrical instability, the cells of the SA node regularly discharge, depolarizing approximately 60-80 times per minute.
- The depolarization initiated by the SA node is then transmitted to the adjacent muscle cells of the right atrium through the conduction of ions via gap junctions of intercalated discs. This causes the neighboring atrial cells to depolarize, creating a wave of electric impulse that spreads throughout the right and left atrium. As a result, the atrial muscles contract, forcing blood down into the ventricles.
- The electrical impulse generated by the SA node continues its path and reaches the atrioventricular (AV) node, which is a small mass of neuromuscular tissue situated in the wall of the atrial septum near the atrioventricular valve (tricuspid valve). The primary function of the AV node is to transmit the electrical signal from the atria to the ventricles. However, there is a deliberate delay of approximately 0.1 second for the signal to pass through the AV node. This delay allows the atria to finish their contraction before the ventricles begin to contract, ensuring proper coordination of the heartbeat.
- The AV node also has a secondary pacemaker function and can take over the role of impulse generation or transmission if there is a problem with the SA node. Once the electrical impulse passes through the AV node, it is conducted to a group of specialized conducting fibers called the Bundle of His (AV bundle). The Bundle of His originates from the AV node and moves downward toward the ventricles. Upon reaching the interventricular septum, the bundle divides into right and left branches.
- Within the ventricular myocardium, the Bundle of His further divides into fine fibers known as Purkinje fibers. These fibers extensively spread throughout the ventricles, transmitting the electrical impulse. The coordinated transmission of the impulse through the AV node, AV bundle, and Purkinje fibers ensures simultaneous contraction of the ventricles, leading to effective ejection of blood from the heart.
- In summary, the conducting system of the heart, starting from the SA node, coordinates the electrical impulses that regulate the heartbeat. The SA node initiates the impulse, which is then transmitted to the atrial muscles, causing them to contract. The impulse continues to the AV node, which delays its transmission to allow the atria to finish contracting before the ventricles contract. From the AV node, the impulse is conducted through the Bundle of His and Purkinje fibers, resulting in coordinated ventricular contractions. This complex system ensures efficient pumping of blood throughout the body.
Mechanism of Impulse Conduction in Heart
- The mechanism of impulse conduction in the heart relies on the generation and propagation of specialized action potentials known as cardiac action potentials. These action potentials can be divided into five distinct phases: resting potential, depolarization, early repolarization, plateau, and repolarization.
- During the resting potential phase, the cardiac muscle cells are in a polarized state, meaning there is a difference in electrical charge between the inside and outside of the cell. This difference is maintained by the activity of ion channels, particularly potassium and sodium channels. At this stage, the inside of the cell is negatively charged compared to the outside.
- The depolarization phase occurs when the cardiac muscle cells receive an electrical stimulus. This stimulus causes a rapid influx of sodium ions into the cell through sodium channels, leading to a reversal of the electrical charge. The inside of the cell becomes positively charged, creating an action potential.
- Following depolarization, the early repolarization phase begins. In this phase, the sodium channels close, and there is a brief period of decreased sodium ion permeability. At the same time, potassium ion channels begin to open, allowing potassium ions to exit the cell. This movement of potassium ions contributes to the repolarization of the cell, restoring the negative charge inside the cell.
- The plateau phase is a characteristic feature of cardiac action potentials and is responsible for the prolonged duration of the cardiac muscle contraction. During this phase, calcium ions enter the cell through calcium channels. The influx of calcium ions counteracts the repolarization process initiated by potassium ions exiting the cell. This prolonged plateau phase helps to sustain the contraction of the cardiac muscle, allowing for efficient ejection of blood from the heart.
- Finally, during the repolarization phase, the calcium channels close, and potassium channels remain open. This results in a further efflux of potassium ions from the cell, which restores the negative charge inside the cell and brings the membrane potential back to its resting state. The repolarization phase prepares the cardiac muscle cells for the next action potential and subsequent contraction.
- The coordinated occurrence of these phases in cardiac action potentials ensures the proper electrical conduction and contraction of the heart. The depolarization and repolarization processes enable the propagation of the electrical impulse from the sinoatrial (SA) node to the atrioventricular (AV) node and through the conducting system of the heart, leading to the coordinated contraction of the atria and ventricles.
- In summary, the mechanism of impulse conduction in the heart relies on the generation and propagation of cardiac action potentials. These action potentials undergo distinct phases of resting potential, depolarization, early repolarization, plateau, and repolarization. These phases are vital for the coordinated contraction of the cardiac muscle and the efficient pumping of blood throughout the body.
Resting potential
- During the resting potential phase in cardiac muscle fibers, the membrane potential is typically around -90mV, indicating a negative charge inside the cell compared to the outside. Under normal conditions, these cells remain stable and maintain this resting potential.
- When electrical impulses originating from the sinoatrial (SA) node are transmitted, they depolarize the cardiac muscle fibers, triggering an action potential. The SA node, known as the natural pacemaker of the heart, generates depolarizations regularly without any external influences. These depolarizations are then transmitted to the atrial cells, leading to their activation.
- Similar to skeletal muscle fibers, cardiac muscle fibers, also known as cardiac myocytes, exhibit a negative membrane potential at rest (-90mV). However, there is a key difference in the mechanism of contraction between cardiac and skeletal muscles.
- In cardiac myocytes, the release of calcium ions (Ca++) from the sarcoplasmic reticulum, a specialized structure within the cell, is induced by the influx of calcium ions into the cell through voltage-gated calcium channels. This phenomenon is referred to as calcium-induced calcium release.
- When there is an increase in the concentration of calcium ions in the myoplasm, which is the cytoplasm of the muscle cell, it triggers muscle contraction. The calcium ions bind to specific proteins within the cardiac myocytes, initiating a cascade of events that leads to the sliding of actin and myosin filaments and the contraction of the muscle fiber.
- Therefore, in cardiac myocytes, the increase in myoplasmic free calcium ion concentration serves as a key signal for muscle contraction. This calcium-induced calcium release mechanism ensures the coordinated and synchronized contraction of the cardiac muscle, allowing for effective pumping of blood from the heart.
- In summary, during the resting potential phase of cardiac muscle fibers, the membrane potential is negative, and the cells remain stable. However, when electrical impulses from the SA node depolarize the cardiac muscle fibers, it triggers an action potential and subsequently leads to the release of calcium ions from the sarcoplasmic reticulum. The increase in myoplasmic free calcium ions is essential for muscle contraction in cardiac myocytes, ensuring proper cardiac function.
Depolarization
- During the depolarization phase, there is a significant increase in the inward movement of sodium ions (Na+) through fast voltage-gated sodium channels in the cardiac muscle cells.
- Normally, during the resting state, the cardiac muscle fiber has a negative membrane potential of around -90mV. However, with the influx of Na+ ions, the membrane potential reverses and becomes more positive. This depolarization process leads to a change in the membrane potential from -90mV to approximately +30mV.
- Concurrently, as the Na+ ions rush into the cell, the permeability of the membrane to potassium ions (K+) decreases, and the potassium channels close. Consequently, very few K+ ions leave the cell during this phase.
- The combined effect of the increase in Na+ ion concentration inside the cell and the decrease in K+ ion concentration outside the cell contributes to the depolarization process. This depolarization is an essential step in the generation of an action potential, as it allows the membrane potential to reach the threshold required for the propagation of the electrical signal.
- The depolarization phase is crucial for the transmission of the electrical impulse throughout the cardiac muscle, enabling coordinated contraction and the proper functioning of the heart. It is followed by subsequent phases, including early repolarization, plateau, and repolarization, which together form the cardiac action potential and regulate the rhythmic contractions of the heart.
- In summary, during the depolarization phase, there is a significant influx of Na+ ions through fast voltage-gated sodium channels in the cardiac muscle cells. This influx of Na+ ions leads to the reversal of the membrane potential from -90mV to +30mV, initiating the depolarization process. At the same time, the permeability of the membrane to K+ ions decreases, resulting in very few K+ ions leaving the cell. The depolarization phase is a critical step in generating the action potential necessary for the propagation of electrical impulses and the coordinated contraction of the cardiac muscle.
Early repolarization
- Early repolarization is a crucial phase in the cardiac cycle characterized by specific electrocardiographic changes. During this phase, the cardiac muscle undergoes repolarization, preparing for the next cycle of electrical activation.
- The repolarization process in early repolarization involves the inactivation of sodium channels as a result of the influx of calcium ions (Ca++) through slow voltage-gated calcium channels. These calcium channels play a significant role in modulating the electrical activity of the cardiac cells. As calcium ions enter the cells, they trigger the release of even more calcium ions from the sarcoplasmic reticulum, a specialized cellular structure responsible for storing and releasing calcium.
- The increase in intracellular calcium ion concentration initiates muscle contraction, leading to the mechanical pumping action of the heart. Additionally, the rise in calcium ions during early repolarization also affects the potassium channels. As a result, the potassium channels open, allowing potassium ions (K+) to move out of the cell.
- The efflux of potassium ions during early repolarization plays a crucial role in restoring the electrical potential across the cardiac cell membrane. This movement of positive potassium ions out of the cell helps to counterbalance the positive charge caused by the influx of calcium ions, leading to repolarization of the cardiac cells. Repolarization is essential for the heart to regain its resting state and prepare for the next depolarization phase.
- It is worth noting that early repolarization is a complex process involving intricate interactions between various ion channels and intracellular calcium dynamics. Disturbances in these mechanisms can lead to abnormalities in repolarization, potentially impacting the electrical stability of the heart and contributing to certain cardiac arrhythmias.
- Overall, early repolarization is a critical phase in the cardiac cycle where inactivation of sodium channels occurs due to the influx of calcium ions. The subsequent release of calcium ions triggers muscle contraction, while the opening of potassium channels allows potassium ions to exit the cell, facilitating repolarization. Understanding the intricacies of early repolarization is essential in comprehending the normal electrical activity of the heart and the potential disruptions that can arise in certain cardiac conditions.
Plateau
- The plateau phase is a critical stage in the cardiac action potential characterized by the maintenance of a depolarized state at around +30mV. This sustained depolarization is achieved through a delicate balance between the inward movement of calcium ions (Ca++) and the outward movement of potassium ions (K+).
- During the plateau phase, the influx of calcium ions through voltage-gated calcium channels is counterbalanced by the efflux of potassium ions through potassium channels. This balance between the two ions helps to maintain the action potential at a plateau level, preventing immediate repolarization of the cardiac cells.
- In addition to the movement of calcium and potassium ions, minor contributions to the plateau phase are made by the Na-Ca exchanger current and the Na+/K+ pump current. The Na-Ca exchanger is responsible for transporting calcium ions out of the cell in exchange for sodium ions, while the Na+/K+ pump actively transports sodium ions out of the cell and potassium ions into the cell. Although these currents play a relatively minor role during the plateau phase, they contribute to the overall maintenance of the depolarized state.
- The balanced movement of ions, primarily calcium and potassium, during the plateau phase causes a delay in repolarization, leading to what is known as the refractory period. The refractory period refers to the time period in which the cardiac cells are unresponsive to further electrical stimuli. In the case of the plateau phase, the refractory period is approximately 0.25 seconds, which is significantly longer than that of skeletal muscle.
- The extended refractory period in the heart serves a crucial purpose. It allows sufficient time for the heart to refill with blood, ensuring adequate ventricular filling before the next contraction. Furthermore, the prolonged refractory period helps to prevent extra beats or premature contractions, maintaining the regular rhythm of the heart and preventing arrhythmias.
- In summary, the plateau phase of the cardiac action potential is characterized by the maintenance of depolarization through a balance between the inward movement of calcium ions and the outward movement of potassium ions. The minor contributions from the Na-Ca exchanger current and Na+/K+ pump current also aid in sustaining the depolarized state. This delay in repolarization during the plateau phase creates a refractory period, which is significantly longer in the heart compared to skeletal muscle. The extended refractory period allows for efficient ventricular filling and helps maintain the regular rhythm of the heart.
Repolarization
- Repolarization is a crucial phase in the cardiac action potential where the cell membrane returns to its resting state after depolarization. During this phase, several important processes occur to restore the normal electrical potential across the cardiac cell membrane.
- Firstly, the potassium channels reopen, allowing potassium ions (K+) to move out of the cell. This outward movement of potassium ions contributes to the repolarization process. Simultaneously, the calcium channels slowly close, blocking the inward movement of calcium ions (Ca++).
- The efflux of potassium ions during repolarization leads to an increase in negative charge inside the cell. This increased negativity helps to return the membrane potential to its normal resting value of approximately -90mV. However, the distribution of ions is altered as a result of the repolarization process. There is an increased concentration of potassium ions outside the cell and a higher concentration of sodium ions (Na+) inside the cell.
- To restore the ionic balance and maintain the resting membrane potential, active transport mechanisms come into play. The sodium-potassium pump, also known as the Na+/K+ pump, actively transports sodium ions out of the cell while pumping potassium ions into the cell. This active transport process requires energy in the form of adenosine triphosphate (ATP).
- By continuously pumping out sodium ions and bringing in potassium ions, the Na+/K+ pump helps to maintain the resting membrane potential of -90mV during the resting phase. This active transport mechanism is crucial for establishing the proper distribution of ions across the cell membrane.
- In summary, repolarization is the phase in the cardiac action potential where the cell membrane returns to its resting state. During this phase, the potassium channels reopen, allowing potassium ions to move out of the cell. This outward movement of potassium ions contributes to the restoration of the negative charge inside the cell. Simultaneously, the closure of calcium channels prevents the inward movement of calcium ions. The distribution of ions is then adjusted through the activity of the Na+/K+ pump, which actively transports sodium ions out of the cell and potassium ions into the cell. This active transport mechanism helps to maintain the resting membrane potential of -90mV and the proper balance of ions across the cell membrane during the resting phase.
FAQ
What is the human heart and what is its primary function?
The human heart is a vital organ responsible for pumping blood throughout the body. Its primary function is to deliver oxygen and nutrients to tissues and organs while removing waste products.
How big is the human heart?
On average, the human heart is about the size of a closed fist. However, its size can vary depending on factors such as age, sex, and overall health.
How many chambers does the human heart have?
The human heart consists of four chambers: two atria (left and right) and two ventricles (left and right). The atria receive blood, while the ventricles pump blood out of the heart.
What are the major blood vessels connected to the heart?
The major blood vessels connected to the heart include the superior and inferior vena cava (which bring deoxygenated blood from the body to the heart), the pulmonary arteries (which carry deoxygenated blood to the lungs), and the pulmonary veins (which return oxygenated blood from the lungs to the heart).
How does the heart maintain its own blood supply?
The heart has its own network of blood vessels called coronary arteries. These arteries supply oxygenated blood to the heart muscle itself, ensuring its proper function.
What is the cardiac cycle?
The cardiac cycle refers to the sequence of events that occur during one complete heartbeat. It involves the contraction (systole) and relaxation (diastole) of the heart chambers, allowing for the efficient pumping of blood.
What causes heart murmurs?
Heart murmurs are abnormal sounds heard during the heartbeat. They can be caused by various factors, including valve problems (such as leaky or narrow valves), congenital heart defects, or certain medical conditions.
How does exercise affect the heart?
Regular exercise has several beneficial effects on the heart. It strengthens the heart muscle, improves its efficiency, and promotes the development of collateral blood vessels, enhancing blood flow to the heart.
What are some common heart diseases?
Common heart diseases include coronary artery disease (caused by the buildup of plaque in the arteries), heart failure (when the heart can’t pump enough blood to meet the body’s needs), arrhythmias (abnormal heart rhythms), and heart valve disorders.
Can lifestyle choices affect heart health?
Yes, lifestyle choices have a significant impact on heart health. Factors such as smoking, poor diet, lack of physical activity, excessive alcohol consumption, and stress can increase the risk of heart disease. Adopting a healthy lifestyle, including a balanced diet, regular exercise, and stress management, can help maintain a healthy heart.
References
- https://pharmeasy.in/conditions/heart-diseases/structure-and-function-of-heart-india/
- https://courses.lumenlearning.com/suny-ap2/chapter/heart-anatomy/
- https://www.vedantu.com/biology/heart
- https://thebiologynotes.com/heart-anatomy-functions/#
- https://www.brainkart.com/article/The-Heart–Structure-and-Function_21076/
- https://anatomyzone.com/thorax/heart/heart-structure-and-function-basics/
- https://www.geeksforgeeks.org/structure-and-functions-of-heart/
- https://practicalbiology.org/cells-to-systems/structure-of-a-heart/looking-at-a-heart
- https://www.onlinebiologynotes.com/human-heart-gross-structure-and-anatomy/
- https://biologydictionary.net/heart/
- https://www.biologydiscussion.com/human-heart/human-heart-anatomy-of-human-heart-with-diagram-biology/81674
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.