Hanta Virus
- Rare and fatal, hantavirus infection is characterized by pulmonary edema, hypoxia, and hypotension. It typically results from exposure to mouse excrement or urine one to three weeks prior to the onset of symptoms and can be fatal within days.
- It is most prevalent in the southwest of the United States and in South America. Hantavirus may be accompanied by flu-like symptoms and associated with hemorrhagic fever and renal syndrome (HFRS).
- This activity describes the clinical manifestations, evaluation, and management of hantavirus infection and emphasizes the role of the interprofessional team in managing patients with this condition.
- Known as hantavirus, hantavirus pulmonary syndrome (HPS) is a pulmonary syndrome characterized by pulmonary edema, hypoxia, and hypotension. It may be accompanied by flu-like symptoms or the hemorrhagic fever and renal syndrome (HFRS).
- This is commonly caused by exposure to mouse excrement or urine within one to three weeks of the onset of symptoms. Southwest United States and South America have the highest incidence of hantavirus. HFRS is more prevalent in Asia and Europe.
- The virus is transmitted through the inhalation of desiccated rodent feces and may also be transmitted through rodent bites.
- Hantavirus is a viral zoonosis prevalent in the southwestern United States, South America, Europe, and Asia. It has been linked to hemorrhagic fevers, ARDS, and renal failure. Hantavirus is an RNA virus belonging to the Bunyaviridae family.
- Hantaviruses were first identified in the early 1950s in Korean War combatants and named Hantaan after the Hantaan River, where the majority of cases occurred. The most prevalent strain of virus in North America is the Sin Nombre virus, which is transmitted primarily by the deer mouse (Peromyscus maniculatus) in the southwestern United States.
- In 1993, a concentration of cases of hantavirus led to the discovery of this particular virus. At least 10 distinct serotypes of hantavirus were identified in the United States by 1977.
- Each serotype is associated with a distinct rodent vector, geographic distribution, and clinical presentation. Most hantavirus serotypes have a preference for the kidneys.
- Hantavirus, like other viruses in the family Bunyaviridae, has a lipid envelope surrounding three RNA segments, but it persistently infects rodents rather than the more common arthropod vectors.
- Hantaviruses can be found wherever Muridae rodents are present. Sin Nombre virus infects Sigmodontinae, the largest group of rodents and mice in the western hemisphere.
Structure of Hanta Virus
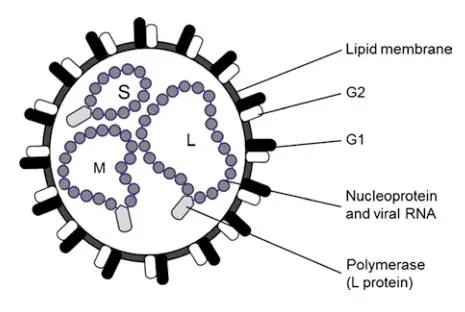
- Hantavirus virions are spherical and range in diameter from 80 to 120 nm. 5–10 nm protruding surface glycoproteins are encased in a bilayer lipid envelope 5–7 nm thick.
- In contrast to other members of the Bunyaviridae, Hantavirus virions have a surface structure resembling a square grid.
- The virion’s interior is composed of three ribonucleocapsids and the L (polymerase) protein, giving it a filamentous or coiled bead-like appearance.
- The lengths of the small (S), medium (M), and large (L) segments are approximately 1,500–2,000 base pairs, 3,600 base pairs, and 6,000–6,500 base pairs, respectively.
- The S RNA encodes the nucleocapsid protein, the L RNA encodes the L protein (an RNA-dependent RNA polymerase), and the M RNA encodes a polyprotein that is cleaved during translation to generate the envelope glycoproteins G1 and G2.
- In addition, a putative non-structural ORF has been identified in the S segment of certain hantavirus species, specifically Arvicoline, Sigmodontini, and Neotomini-borne hantavirus species.
- This protein’s reading frame coincides with the reading frame of the nucleocapsid protein. The 3 and 5 extremities of all three RNA segments contain the same complementary nucleotides, and this sequence is conserved among all viruses within the genus Hantavirus.
- This is also true for other members of the Bunyaviridae, despite the fact that the terminal sequences vary between genera.
Genome Structure of Hanta Virus
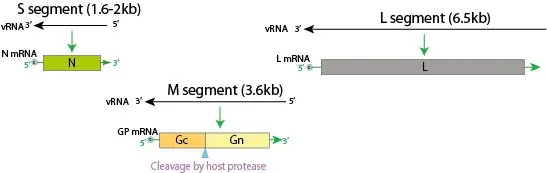
- Hantavirus’s negative-sense, single-stranded RNA genome is trisegmented into small, medium, and large (S, M, and L) segments.
- L segment is between 6.8 and 12 kb, M segment between 3.2 and 4.9 kb and S segment between 1 and 3 kb.
- The respective segments code for three structural proteins: nucleocapsid (N) protein, two glycoproteins Gn and Gc, and an RNA-dependent RNA-polymerase.
- On their S segment, some hantaviruses also encode an NSs protein.
- The genome segments, which are encapsulated by the N protein to form ribonucleoproteins, are surrounded by a lipid envelope that is decorated with Gn and Gc spikes.
Epidemiology of Hanta Virus
- Hantaviruses are a group of viruses that can cause various diseases in humans, ranging from mild flu-like symptoms to severe respiratory and kidney diseases. The transmission of hantaviruses to humans usually occurs through contact with infected rodents, their urine, droppings, or saliva.
- The epidemiology of hantaviruses varies depending on the virus type and geographic location. Hantaviruses are found worldwide and are known to cause disease in humans in Asia, Europe, Africa, and the Americas.
- In North and South America, the hantavirus that causes Hantavirus Pulmonary Syndrome (HPS) is primarily carried by deer mice, while in Europe and Asia, the virus is carried by other rodent species. In Africa, hantaviruses have been identified in rodents but have not yet been linked to human disease.
- HPS was first recognized in the southwestern United States in 1993, and since then, more than 700 cases have been reported in the country. The majority of cases occur in rural areas, and individuals who work or spend time in rodent-infested areas are at higher risk.
- The incidence of hantavirus infection is generally low, and outbreaks are rare. However, in some areas, such as the Four Corners region of the United States, where Colorado, Utah, New Mexico, and Arizona meet, there have been multiple HPS outbreaks.
- Prevention measures include avoiding contact with rodents and their excreta, sealing rodent entry points, and proper cleaning of rodent-infested areas. In addition, people who work in high-risk occupations, such as pest control, should take precautions to minimize their risk of exposure.
- Overall, while hantavirus infections are relatively rare, they can be severe and potentially fatal. It is important to be aware of the risk factors and to take appropriate precautions to prevent infection.
Transmission of Hanta Virus
- Hantaviruses are transmitted to humans through contact with infected rodents or their excreta, such as urine, droppings, and saliva. People can become infected with hantaviruses by inhaling aerosolized virus particles from contaminated materials or by direct contact with contaminated materials.
- In the Americas, the primary carrier of hantavirus is the deer mouse, which sheds the virus in its urine, feces, and saliva. People can become infected with the virus by breathing in the virus-contaminated air or by touching their mouth, nose, or eyes after coming into contact with contaminated surfaces or materials.
- In Europe and Asia, different rodent species can carry hantaviruses, such as the bank vole and the striped field mouse, among others. People in these regions can also become infected through contact with infected rodents or their excreta.
- While rare, human-to-human transmission of hantavirus has been reported in certain circumstances, such as in healthcare settings where there is close contact with infected patients.
- It is important to note that not all rodents carry hantaviruses, and even in areas where infected rodents are present, the risk of transmission can be reduced by taking appropriate precautions, such as wearing protective clothing and masks, properly cleaning and disinfecting rodent-infested areas, and sealing up holes and cracks in buildings to prevent rodent entry.
Replication cycle of hantaviruses
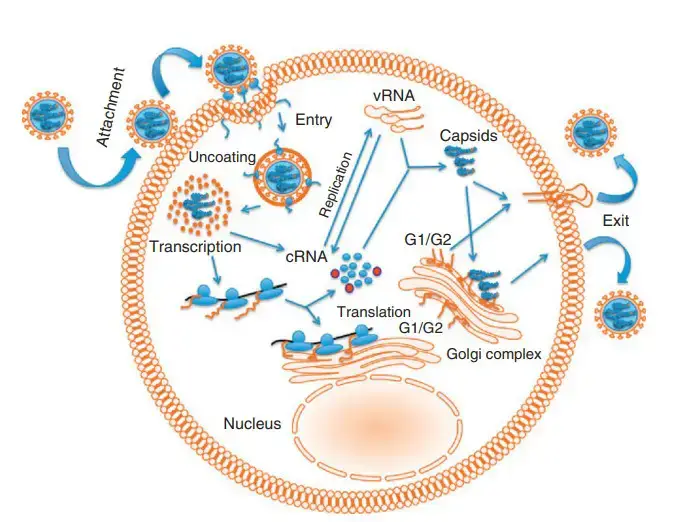
- Multiple cell lineages, including endothelial, epithelial, macrophages, dendritic, and lymphocytes, are infected by hantaviruses. Attachment of virus particles to host cell surface receptors initiates the replication cycle.
- Multiple studies indicate that attachment is mediated by the interaction of viral Gn protein with integrin receptors on the surface of host cells. Receptors for apathogenic and pathogenic hantaviruses are thought to be b1 and b3 integrins, respectively.
- Nonetheless, it has been reported that hantaviruses can infect cells devoid of integrin receptors, indicating that integrins may not be the only receptors that hantaviruses use to attach to host cells.
- After attachment, clatherin-coated crevices mediate cell entry, and virions are ultimately delivered to lysosomes. Virions are decoated and three viral capsids are released into the cytoplasm within the endolysosomal compartment.
- The viral RdRp initiates transcription and produces three mRNAs, one for each viral RNA segment S, M, and L. S and L segment-derived mRNAs are translated on unbound ribosomes, whereas M segment-derived mRNAs are translated on the endoplasmic reticulum (ER).
- At a highly conserved amino acid motif, WAASA, the glycoprotein precursor is intrinsically cleaved to generate two glycoproteins, Gn and Gc, respectively.
- After glycosylation in the endoplasmic reticulum (ER), both Gn and Gc are transported to the Golgi complex, establishing the groundwork for the maturation of virions.
- After initial cycles of transcription, viral RdRp switches to replication mode and generates three viral genomic RNAs that are encapsulated by the viral N protein to form three nucleocapsids. Mature viral nucleocapsids are transported to destinations on the Golgi membrane that are adorned with the Gn and Gc proteins.
- However, the molecular mechanisms that regulate the specific recognition and encapsidation of viral genome by N, transport of capsids to Golgi, and budding of nascent virions into and out of the Golgi complex remain unknown.
- Mechanisms of viral RdRp incorporation into virus particles are intriguing and require more study. The assembly and maturation of New World hantaviruses take place on the plasma membrane.
- The observation that neither SNV nor black Creek Canal virus (BCCV) particles were detected in infected cells provides evidence in favor of this pathway for assembly and maturation.
- Localization of N protein from both old and new world hantaviruses on the Golgi apparatus increases the likelihood of their maturation on the Golgi.
Pathogenesis of Hanta Virus
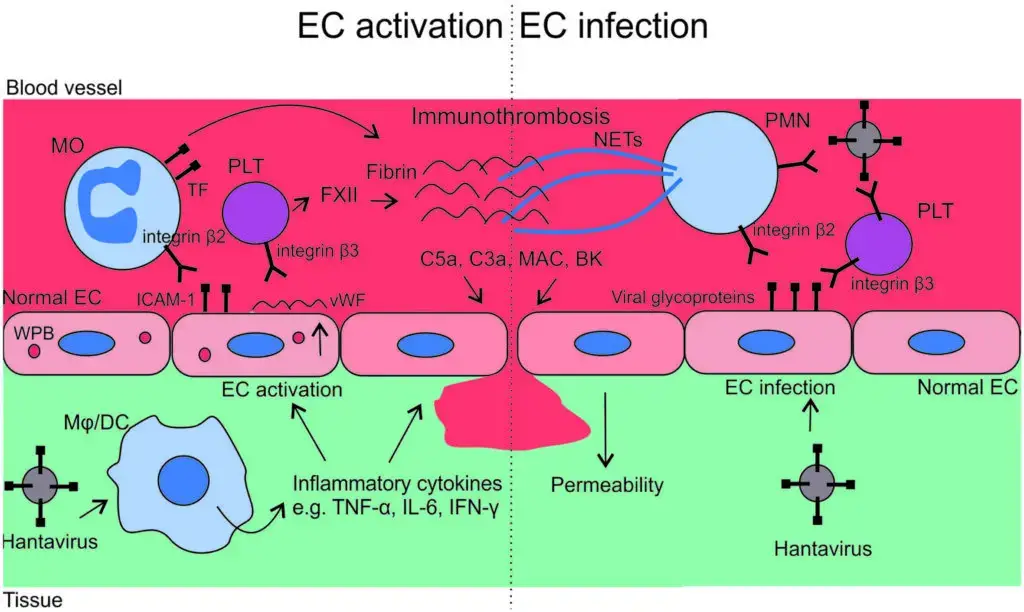
The recognition of hantaviruses by macrophages (M) or dendritic cells (DCs) induces proinflammatory cytokines, which alter the phenotype of endothelial cells (ECs) from anti- to pro-adhesive. Pro-adhesive ECs bind monocytes (MOs) via ICAM-1 – integrin β2 interaction, whereas they bind platelets (PLTs) via vWF via αIIbβ3 integrin interaction. In order to prevent the dissemination of the virus, activated MOs and PLTs promote coagulation via tissue factor (TF) and contact activation pathway (factor XII), respectively. Concurrently, hantavirus-infected ECs express viral glycoproteins on their surface, which bind β2 and β3 integrins of polymorphonuclear neutrophils (PMNs) and platelet-like T cells (PLTs). The binding induces the release of neutrophil extracellular traps (NETs) from PMNs and the activation of PLTs to a greater extent. These virus-induced events exacerbate inflammation and may result in excessive immunothrombosis formation. Complement and contact pathway activations, both of which are linked to immunothrombosis, contribute to vascular leakage via anaphylatoxins C5a and C3, membrane attack complex (MAC), and bradykinin (BK).
Clinical Manifestations of Hanta Virus
- Hantavirus infection can cause a range of clinical manifestations, which can vary depending on the specific virus strain and the individual’s immune response. The symptoms can range from mild to severe, and in some cases, the infection can be fatal.
- The initial symptoms of hantavirus infection can include fever, fatigue, muscle aches, and headaches. These symptoms are often accompanied by abdominal pain, nausea, vomiting, and diarrhea. As the disease progresses, patients may develop coughing and shortness of breath, which can be severe and may require hospitalization.
- In some cases, hantavirus infection can progress to a severe form of the disease known as hantavirus pulmonary syndrome (HPS). HPS is characterized by acute respiratory distress, which can lead to respiratory failure and death in up to 50% of cases. Other symptoms of HPS can include coughing up blood, low blood pressure, and kidney failure.
- It’s important to note that not everyone who is infected with hantavirus will develop symptoms, and some people may have only mild symptoms. However, if you have been exposed to rodents or their droppings and develop any of these symptoms, it’s important to seek medical attention immediately. Early treatment can improve outcomes and reduce the risk of complications.
Hanta Virus Pulmonary Syndrome (HPS)
- Hantavirus Pulmonary Syndrome (HPS) is a severe form of hantavirus infection that can cause respiratory failure and is potentially fatal. HPS is caused by specific strains of hantavirus that are carried by rodents, particularly deer mice in North and South America.
- HPS typically begins with flu-like symptoms, including fever, headache, muscle aches, and fatigue, which can last for a few days. As the disease progresses, patients may experience coughing and shortness of breath, which can become severe and may require hospitalization.
- HPS can be challenging to diagnose, as its symptoms can be similar to those of other respiratory illnesses. However, a combination of laboratory tests and imaging studies, such as chest X-rays or CT scans, can help confirm the diagnosis.
- Treatment for HPS is primarily supportive, and there is currently no specific antiviral medication available. Patients with severe cases may require hospitalization, oxygen therapy, or mechanical ventilation to help them breathe. Early treatment is crucial for improving outcomes and reducing the risk of complications.
- Preventing HPS involves avoiding contact with rodents and their droppings, particularly in areas where hantavirus is known to be present. It’s essential to keep homes and workplaces clean and free of rodent infestations, and to take precautions when cleaning up rodent droppings or nests.
Hemorrhagic Fever with Renal Syndrome (HFRS)
- Hemorrhagic Fever with Renal Syndrome (HFRS) is a viral disease caused by specific strains of hantavirus that are carried by rodents, particularly rats in Asia and Europe. HFRS is characterized by fever, severe headache, muscle aches, abdominal pain, and renal impairment.
- The disease typically progresses through five stages. The first stage is the febrile phase, which lasts for a few days and is characterized by high fever, headache, and muscle aches. In the second stage, patients may develop symptoms such as abdominal pain, nausea, and vomiting, and their blood pressure may drop.
- In the third stage, patients may experience renal impairment, which can include proteinuria, hematuria, and decreased urine output. The fourth stage is the oliguric phase, during which patients may develop severe renal failure and require dialysis. In the fifth and final stage, patients enter the convalescent phase, during which they begin to recover from the illness.
- HFRS can be challenging to diagnose, as its symptoms can be similar to those of other viral diseases. However, a combination of laboratory tests and imaging studies, such as ultrasound or CT scans, can help confirm the diagnosis.
- Treatment for HFRS is primarily supportive, and there is currently no specific antiviral medication available. Patients with severe cases may require hospitalization, supportive care, and in some cases, dialysis. Early treatment is crucial for improving outcomes and reducing the risk of complications.
- Preventing HFRS involves avoiding contact with rodents and their droppings, particularly in areas where hantavirus is known to be present. It’s essential to keep homes and workplaces clean and free of rodent infestations, and to take precautions when cleaning up rodent droppings or nests. Vaccines are available in some countries for individuals who are at high risk of exposure.
Laboratory Diagnosis of Hanta Virus
The laboratory diagnosis of hantavirus infection typically involves a combination of serological tests, molecular tests, and antigen detection assays.
- Serological tests detect the presence of antibodies produced by the immune system in response to hantavirus infection. The most commonly used serological test is the enzyme-linked immunosorbent assay (ELISA), which detects immunoglobulin (Ig) G and IgM antibodies in the patient’s blood. A positive result for IgM antibodies is indicative of acute infection, while a positive result for IgG antibodies indicates previous exposure.
- Molecular tests, such as polymerase chain reaction (PCR), can detect the presence of hantavirus genetic material in patient samples, such as blood, urine, or tissue. PCR is highly sensitive and specific and can detect hantavirus infection early in the course of the disease.
- Antigen detection assays, such as immunofluorescence assays (IFA) and immunohistochemistry (IHC), can detect hantavirus antigens in patient samples, such as tissue or fluid samples. These tests can be used to confirm the presence of hantavirus infection in patients with suspected cases.
- It’s important to note that laboratory testing for hantavirus infection should be performed in specialized laboratories with appropriate biosafety protocols, as the virus can be highly infectious and can cause laboratory-acquired infections. Clinical suspicion, in combination with appropriate laboratory testing, is critical for the accurate diagnosis of hantavirus infection.
Treatment of Hanta Virus
- The treatment of hantavirus infection is primarily supportive, as there is currently no specific antiviral medication available for the disease.
- Patients with mild to moderate cases of hantavirus infection may be managed with supportive care, such as rest, fluids, and pain relievers. However, patients with severe cases of hantavirus infection, such as those with Hantavirus Pulmonary Syndrome (HPS) or Hemorrhagic Fever with Renal Syndrome (HFRS), may require hospitalization and more intensive supportive care.
- In severe cases of HPS, patients may require oxygen therapy, mechanical ventilation, or extracorporeal membrane oxygenation (ECMO) to help them breathe. In severe cases of HFRS, patients may require dialysis for renal failure.
- Early treatment is critical for improving outcomes and reducing the risk of complications. Therefore, it’s important to seek medical attention immediately if you have been exposed to rodents and develop symptoms of hantavirus infection, such as fever, headache, muscle aches, and respiratory or renal symptoms.
- Prevention is also essential in managing hantavirus infection. Avoiding contact with rodents and their droppings, particularly in areas where hantavirus is known to be present, is crucial. Keeping homes and workplaces clean and free of rodent infestations and taking precautions when cleaning up rodent droppings or nests can also help prevent hantavirus infection.
Prevention and Control of Hanta Virus
Prevention and control of hantavirus infection involves taking measures to reduce the risk of exposure to the virus and to prevent the transmission of the virus from person to person. Some key measures include:
- Rodent control: Hantaviruses are carried by rodents, particularly rats and mice. Therefore, it’s essential to control rodent populations by keeping homes and workplaces clean and free of rodent infestations. This can be achieved by sealing entry points, storing food in rodent-proof containers, and disposing of trash properly.
- Personal protective measures: When in areas where rodents may be present, it’s important to take personal protective measures, such as wearing gloves and a mask, to avoid direct contact with rodents and their droppings.
- Environmental sanitation: Areas contaminated with rodent droppings should be thoroughly cleaned and disinfected. This includes using a solution of bleach and water to clean surfaces and properly disposing of any contaminated materials.
- Vaccination: Vaccines are available in some countries for individuals who are at high risk of exposure to hantavirus, such as laboratory workers and field researchers.
- Public education: Raising awareness about hantavirus infection and its prevention through public education campaigns can help reduce the risk of transmission.
It’s important to note that hantavirus infection can also be transmitted from person to person in rare cases, such as through organ transplantation or close contact with infected individuals. Therefore, appropriate infection control measures, such as isolation of infected individuals, should be taken in healthcare settings to prevent the spread of the virus.
FAQ
What is hantavirus?
Hantavirus is a family of viruses that are primarily carried by rodents and can cause severe illness in humans.
How is hantavirus transmitted to humans?
Hantavirus is primarily transmitted to humans through contact with the urine, feces, or saliva of infected rodents, particularly rats and mice.
What are the symptoms of hantavirus infection?
Symptoms of hantavirus infection can include fever, headache, muscle aches, and respiratory or renal symptoms, depending on the type of hantavirus.
How is hantavirus infection diagnosed?
Hantavirus infection is diagnosed through a combination of laboratory tests, including serological tests, molecular tests, and antigen detection assays.
Is there a treatment for hantavirus infection?
There is currently no specific antiviral medication available for hantavirus infection, and treatment is primarily supportive.
How can hantavirus infection be prevented?
Prevention measures for hantavirus infection include controlling rodent populations, taking personal protective measures in areas where rodents may be present, maintaining environmental sanitation, and raising awareness through public education campaigns.
Who is at risk for hantavirus infection?
People who come into contact with rodents or their droppings, particularly in areas where hantavirus is known to be present, are at risk for hantavirus infection.
Is hantavirus infection contagious from person to person?
Hantavirus infection is typically not contagious from person to person, but rare cases of transmission through organ transplantation or close contact with infected individuals have been reported.
Can hantavirus infection be fatal?
Yes, hantavirus infection can be fatal, particularly in severe cases such as Hantavirus Pulmonary Syndrome (HPS) or Hemorrhagic Fever with Renal Syndrome (HFRS).
Where is hantavirus found?
Hantavirus is found worldwide, but different strains are more prevalent in different regions. In the United States, hantavirus is primarily found in the western and southwestern regions.
References
- Moore RA, Griffen D. Hantavirus Syndrome. [Updated 2022 May 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513243/
- Hepojoki, J., Vaheri, A., & Strandin, T. (2014). The fundamental role of endothelial cells in hantavirus pathogenesis. Frontiers in Microbiology, 5. doi:10.3389/fmicb.2014.00727
- Muyangwa M, Martynova EV, Khaiboullina SF, Morzunov SP, Rizvanov AA. Hantaviral Proteins: Structure, Functions, and Role in Hantavirus Infection. Front Microbiol. 2015 Nov 27;6:1326. doi: 10.3389/fmicb.2015.01326. PMID: 26640463; PMCID: PMC4661284.
- Hepojoki J, Strandin T, Lankinen H, Vaheri A. Hantavirus structure–molecular interactions behind the scene. J Gen Virol. 2012 Aug;93(Pt 8):1631-1644. doi: 10.1099/vir.0.042218-0. Epub 2012 May 23. PMID: 22622328.
- Blasdell, Kim & Henttonen, Heikki & Buchy, Philippe. (2012). Hantavirus Genetic Diversity. 10.1007/978-94-007-2114-2_9.
- Hussein, Islam & Haseeb, Abdul & Haque, Absarul & Mir, Mohammad. (2011). Recent Advances in Hantavirus Molecular Biology and Disease. Advances in applied microbiology. 74. 35-75. 10.1016/B978-0-12-387022-3.00006-9.
- https://www3.paho.org/hq/index.php?option=com_content&view=article&id=14911:hantavirus&Itemid=0&lang=en#gsc.tab=0
- https://www.ecdc.europa.eu/en/hantavirus-infection/facts
- https://www.cdc.gov/hantavirus/index.html
- https://www.cdc.gov/hantavirus/hps/index.html
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.