What is Coomb’s Test?
- Coomb’s test, also known as the antiglobulin test, is a direct agglutination reaction that was discovered by Coombs, Mourant, and Race in 1945. Initially developed for detecting incomplete anti-Rh antibodies, this test plays a crucial role in diagnosing certain blood disorders and identifying immune-mediated reactions.
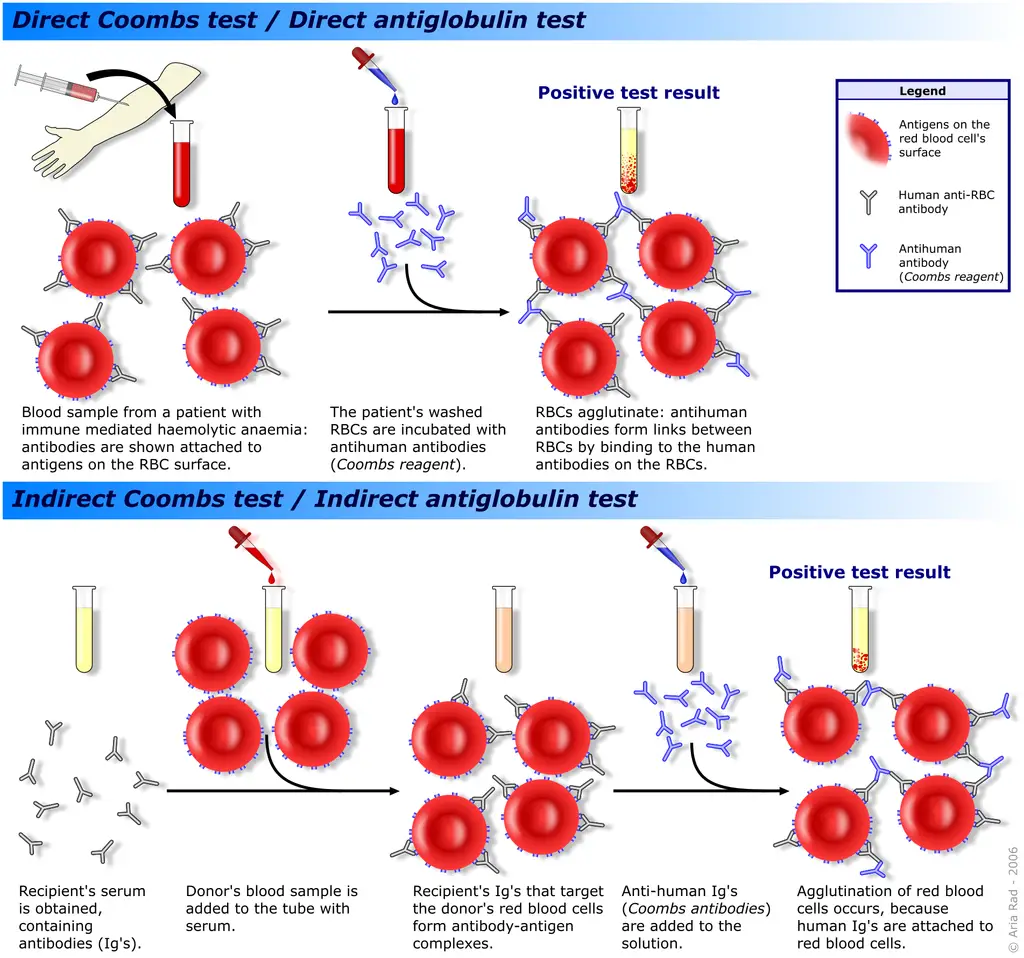
- During the Coomb’s test, incomplete antibodies are unable to agglutinate erythrocytes. These incomplete antibodies coat the surface of red blood cells (erythrocytes) without causing any agglutination. However, when these coated erythrocytes are treated with Coombs’ serum or antiglobulin, the cells undergo agglutination.
- Coombs’ serum, also referred to as Coombs’ reagent, is a specialized serum derived from a rabbit or another animal that has been previously immunized with purified human globulin. This process allows the animal to develop antibodies specifically directed against IgG and complement, such as rabbit antiserum against human globulin. Coombs’ serum is used in both direct and indirect Coombs’ tests and is commonly known as antihuman globulin.
- In the direct Coomb’s test, the patient’s red blood cells are first washed to remove any unbound antibodies. Then, Coombs’ serum is added to the red blood cells. If there are any antibodies coating the patient’s red blood cells, the antiglobulin in the Coombs’ serum will bind to these antibodies, leading to agglutination. This reaction indicates the presence of immune-mediated reactions or certain blood disorders, such as autoimmune hemolytic anemia or hemolytic disease of the newborn.
- The indirect Coomb’s test, on the other hand, is used to detect the presence of antibodies in a patient’s plasma or serum that may react with red blood cells. In this test, the patient’s plasma or serum is mixed with known red blood cells, followed by the addition of Coombs’ serum. If antibodies are present in the patient’s plasma or serum that can bind to the red blood cells, the antiglobulin in the Coombs’ serum will cause agglutination.
- In summary, Coombs’ test, or the antiglobulin test, is a valuable tool in diagnosing immune-mediated reactions and certain blood disorders. By utilizing Coombs’ serum or antiglobulin, this test can identify the presence of antibodies that coat red blood cells, providing crucial information for medical professionals in managing and treating these conditions.
Objectives of Coomb’s Test
The objectives of Coomb’s test are to detect red blood cells that are sensitized with IgG alloantibodies, IgG autoantibodies, or complement components. This helps in determining blood group compatibility for transfusions, diagnosing autoimmune hemolytic anemia, and identifying immune-mediated reactions and conditions such as paroxysmal nocturnal hemoglobinuria. Overall, the test aims to provide important information for the diagnosis and management of blood disorders and immune-related issues.
Principle of Coomb’s Test
The principle of Coomb’s test, also known as the antiglobulin test, revolves around the attachment of complement proteins or incomplete antibodies (IgG) to the surface of red blood cells. These cells, referred to as sensitized red cells, may acquire this sensitization either in vivo (within the body) or in vitro (in the laboratory setting).
In the absence of Coombs’ reagent (antiglobulin serum), the sensitized red cells do not agglutinate. This is because the IgG molecules attached to the red cells are unable to bridge the gap between the sensitized cells. The negative charge present on the surface of these cells keeps them separated, preventing agglutination from occurring.
However, the addition of Coombs’ reagent, or antiglobulin serum, completes the reaction. When this serum is added to the sensitized cells, the Fab portion of the anti-human globulin molecule (anti-IgG) within the reagent reacts with the Fc portions of two adjacent IgG molecules attached to red cells. This bridging of the gap between sensitized red cells leads to agglutination, causing the cells to clump together.
Therefore, a positive Coomb’s test occurs when human IgG antibodies have already attached to the patient’s red blood cells in vivo or when the patient’s serum contains incomplete antibodies that can attach to red blood cells in vitro. The addition of anti-human IgG in the form of Coombs’ reagent induces agglutination of the sensitized cells, confirming the presence of these antibodies or complement proteins.
By utilizing this principle, Coomb’s test serves as a valuable diagnostic tool in identifying immune-mediated reactions, such as autoimmune hemolytic anemia or other conditions involving sensitized red blood cells. It provides a clear indication of whether the patient’s red blood cells have been sensitized and helps healthcare professionals in determining appropriate treatment strategies.
Types of Coomb’s Test
There are two types of Coombs tests: the direct Coomb’s test (direct antiglobulin test) and the indirect Coomb’s test (indirect antiglobulin test).
- Direct Coomb’s Test (Direct Antiglobulin Test): The direct Coomb’s test is the more commonly performed test and aims to detect antibodies that are already attached to the surface of red blood cells (RBCs). In this test, the sensitization of RBCs with incomplete antibodies occurs within the patient’s body (in vivo). To identify the presence of cell-bound antibodies, antiserum against human immunoglobulin is used, which causes agglutination of the patient’s red cells if the antibodies are present.
- Indirect Coomb’s Test (Indirect Antiglobulin Test): The indirect Coomb’s test, on the other hand, is designed to detect unattached antibodies that are circulating freely in the bloodstream. In this test, the sensitization of RBCs with incomplete antibodies takes place outside the body in a laboratory setting (in vitro). The patient’s serum is mixed with normal red cells, and then antiserum to human immunoglobulin is added. If antibodies are present in the patient’s serum, agglutination occurs.
These two types of Coombs tests serve distinct purposes in diagnosing immune-related reactions and blood disorders. The direct Coomb’s test detects antibodies already bound to the surface of RBCs, indicating conditions such as autoimmune hemolytic anemia. The indirect Coomb’s test, on the other hand, detects unattached antibodies in the patient’s serum, which can be useful in determining blood compatibility for transfusions and identifying antibodies in cases like hemolytic disease of the newborn.
Requirements for Coomb’s Test
To perform a Coomb’s test, several requirements are necessary to ensure accurate and reliable results. The essential requirements for conducting a Coomb’s test include:
- Test Tubes: Test tubes are needed to hold the samples and reagents during the test. They provide a controlled environment for the reaction to occur.
- Centrifuge: A centrifuge is required to separate the red blood cells from the serum or plasma. It helps in obtaining clear samples for testing.
- Anti-Human Globulin (AHG) Reagent: The AHG reagent, also known as Coombs’ reagent or antiglobulin serum, is a crucial component of the test. It contains antibodies that can bind to antibodies or complement components attached to red blood cells. It facilitates agglutination, indicating the presence of sensitized red blood cells.
- Pre-sensitized Red Cells (Coombs’ Control Cells): These are red blood cells that have been pre-treated with known antibodies or complement components. Coombs’ control cells serve as a reference or control to ensure that the test is working properly. They help validate the reagents and the overall procedure.
- Saline: Saline solution, typically a physiological saline (0.9% sodium chloride), is used as a diluent or medium to create the appropriate environment for the test. It is used to wash the red blood cells, remove unbound antibodies or reagents, and prepare the samples for testing.
These requirements are necessary for conducting a Coomb’s test accurately and efficiently. Test tubes provide a controlled environment, the centrifuge helps in sample separation, and the AHG reagent enables the detection of sensitized red blood cells. Coombs’ control cells serve as a reference, and saline is used as a diluent and wash solution. By ensuring the availability of these requirements, healthcare professionals can perform Coomb’s tests effectively and obtain reliable results for the diagnosis and management of immune-related reactions and blood disorders.
Procedure of Coomb’s Test
The indirect antiglobulin test (IAT) is a two-stage procedure that employs antihuman globulin serum to detect sensitization of red blood cells in vitro. In contrast, red cell sensitization in vivo is detected by a single-step technique, the direct antiglobulin test (DAT).
Direct Coomb’s Test
The Direct Coomb’s test is a diagnostic procedure used to detect the presence of antibodies on the surface of red blood cells. This test plays a crucial role in identifying and diagnosing conditions such as autoimmune hemolytic anemia and transfusion reactions. Here is a step-by-step description of the Direct Coomb’s test procedure:
- Initially, red blood cells suspected of being sensitized are thoroughly washed in a large volume of saline solution. This washing process is performed around 3 to 4 times to remove any unbound antibodies or other substances that could interfere with the test results.
- Once the washing steps are complete, two drops of anti-human globulin serum are added to the washed red blood cell sample. This serum contains antibodies that specifically bind to human immunoglobulins present on the surface of sensitized red blood cells.
- The sample is then mixed vigorously to ensure proper distribution of the anti-human globulin serum throughout the red blood cell suspension. Afterward, the mixture is centrifuged at a speed of 1500 revolutions per minute (rpm) for approximately one minute. This centrifugation step helps to separate the sensitized red blood cells from the supernatant.
- Following centrifugation, the test tube containing the sample is examined against a lighted background. By tapping the bottom of the tube gently, any agglutination or clumping of red blood cells can be observed. Agglutination indicates the presence of antibodies on the surface of the red blood cells and is considered a positive reaction.
- If no agglutination is observed initially, the test tube is left at room temperature for 10 minutes. This additional incubation time allows for the detection of weaker reacting antibodies, which may require more time to produce visible agglutination. After the incubation period, the tube is re-centrifuged and examined for agglutination again.
- In case no agglutination is observed even after the incubation and re-centrifugation, an additional step is performed. A drop of presensitized red blood cells, prepared as a 5% suspension in saline, is added to the test tube. These presensitized cells already contain known antibodies on their surface.
- If the anti-human globulin (AHG) present in the test serum is reactive, it will bind to the antibodies on the presensitized red blood cells, resulting in agglutination. This agglutination of the presensitized cells confirms the reactivity of the anti-human globulin (AHG) used in the test and validates the result.
By following these procedural steps, the Direct Coomb’s test allows for the detection and identification of antibodies bound to red blood cells. The results obtained from this test aid healthcare professionals in diagnosing and managing various conditions related to immune-mediated destruction of red blood cells.
Indirect Coomb’s Test
The Indirect Coomb’s test is a laboratory procedure used to detect the presence of antibodies in a patient’s serum that can react with red blood cells. This test is valuable in identifying conditions such as hemolytic disease of the newborn and determining compatibility for blood transfusions. Here is a step-by-step description of the Indirect Coomb’s test procedure:
- Initially, a 4% saline suspension of the test cells is prepared. This suspension contains red blood cells that will be used to detect the presence of antibodies in the patient’s serum.
- Two drops of the prepared cell suspension are added to a small test tube. The test cells serve as a substrate for the antibodies present in the patient’s serum.
- Next, two drops of antiserum, which contains known antibodies against specific red blood cell antigens, are added to the cell suspension in the test tube. The antiserum will react with any corresponding antibodies present in the patient’s serum.
- The test tube is then incubated in a water bath at a temperature of 37°C for a period of 30 minutes. This controlled environment promotes antibody-antigen reactions to occur between the patient’s serum antibodies and the red blood cell antigens.
- After the incubation period, the test tube is removed from the water bath and washed 3 to 4 times with a large volume of saline solution. Each washing step helps remove any unbound antibodies or other substances that could interfere with the test results. The contents of the test tube are completely decanted after the final washing.
- Immediately following the washing steps, two drops of anti-human globulin (AHG) are added to the test tube containing the washed cell suspension and patient’s serum. The AHG contains antibodies that can recognize and bind to antibodies present on the red blood cells.
- The test tube is then centrifuged at a speed of 1500 revolutions per minute (rpm) for approximately one minute. Centrifugation aids in separating the sensitized red blood cells, if present, from the supernatant.
- After centrifugation, the test tube is examined for the presence of hemagglutination, which indicates the presence of antibody-antigen reactions. Hemagglutination refers to the clumping or agglutination of red blood cells due to antibody binding.
- In the event of negative hemagglutination, where no clumping is observed, pre-sensitized reagent cells are added to the test to evaluate the reactivity of the anti-human globulin (AHG). The addition of Coombs’ control cells, which are known to cause agglutination, should result in visible clumping or agglutination if the AHG is reactive.
By following these procedural steps, the Indirect Coomb’s test enables the detection and identification of antibodies in a patient’s serum that can potentially cause adverse reactions when interacting with red blood cells. The results obtained from this test aid healthcare professionals in determining appropriate blood transfusion compatibility and managing conditions related to immune-mediated hemolysis.
Result Interpretation of Coomb’s Test
The interpretation of Coomb’s test results involves analyzing the presence or absence of clumping or agglutination of red blood cells. Here is how the results of both the Direct and Indirect Coomb’s tests can be interpreted:
- Positive Result: If clumping or agglutination of red blood cells is observed during the test, it indicates a positive result. In the Direct Coomb’s test, the agglutination suggests the presence of antibodies on the patient’s red blood cells, indicating a condition of hemolysis. This means that the patient’s immune system may be actively targeting and destroying their own red blood cells. In the case of the Indirect Coomb’s test, the agglutination of red blood cells suggests the presence of antibodies circulating in the bloodstream. These antibodies can recognize and react with foreign red blood cells, potentially leading to immune reactions, particularly during blood transfusions.
- Negative Result: If no clumping or agglutination of red blood cells is observed during the Coomb’s test, it indicates a negative result. In both the Direct and Indirect Coomb’s tests, a negative result suggests the absence of antibodies that can cause agglutination. This indicates that there are no detectable antibodies on the patient’s red blood cells (in the case of the Direct Coomb’s test) or no circulating antibodies in the bloodstream (in the case of the Indirect Coomb’s test) that could lead to immune reactions or hemolysis.
Interpreting the results of the Coomb’s test is crucial in diagnosing and managing conditions related to immune-mediated destruction of red blood cells and determining compatibility for blood transfusions. Healthcare professionals analyze these results to guide appropriate treatment decisions and ensure patient safety during transfusion procedures.
Applications of Coomb’s Test
The Coomb’s test has various applications in diagnosing and managing different medical conditions. Here are some key applications of the Coomb’s test:
- Determining the type of anemia: Coomb’s test is used as one of the blood tests to help identify the specific type of anemia in patients who are anemic. By detecting the presence of antibodies on red blood cells, the test aids in diagnosing immune-mediated hemolytic anemias.
- Blood transfusion compatibility: The indirect Coomb’s test is administered to assess whether a patient may have a potential adverse reaction to a blood transfusion. Blood banks utilize this test to determine the compatibility between the recipient’s serum and the donor’s red blood cells. It helps identify the presence of antibodies in the patient’s serum that could react with the donor’s blood cells, leading to transfusion reactions.
- Detection of anti-Rh antibodies: Coomb’s tests, particularly the indirect Coomb’s test, are employed to detect the presence of anti-Rh antibodies. These antibodies are of particular importance in Rh incompatibility during pregnancy and can cause hemolytic disease of the newborn.
- Detection of incomplete antibodies in diseases: The Coomb’s test is used to identify incomplete antibodies associated with certain diseases, such as brucellosis and other infectious conditions. It aids in the diagnosis of these diseases by detecting the presence of antibodies on the surface of red blood cells.
- Prenatal testing: The indirect Coomb’s test is utilized in prenatal testing for pregnant women. It helps determine if the mother has developed antibodies against fetal red blood cells, which can lead to hemolytic disease of the newborn. This test is crucial for managing pregnancies at risk and ensuring appropriate interventions to prevent complications.
- Neonatal testing: The Coomb’s test is performed on the blood sample of newborns, especially in cases where the newborn presents with jaundice. It helps identify the presence of maternal antibodies that may be causing hemolysis and jaundice in the newborn.
- Detection of specific medical conditions: The Coomb’s test aids in the diagnosis and detection of various conditions, including hemolytic anemia, chronic lymphocytic leukemia, erythroblastosis fetalis, infectious mononucleosis, mycoplasmal infection, syphilis, systemic lupus erythematosus, and other autoimmune disorders.
These diverse applications of the Coomb’s test contribute to the accurate diagnosis, management, and prevention of conditions associated with immune-mediated destruction of red blood cells and compatibility in blood transfusions. Healthcare professionals rely on the results of the Coomb’s test to guide appropriate treatment strategies and ensure patient well-being.
Limitations of Coomb’s Test
The Coomb’s test, despite its clinical significance, has certain limitations that should be considered. Here are the limitations of the Coomb’s test:
- Non-specific results: In some cases, particularly among older adults, a Coomb’s test may yield abnormal results even in the absence of any underlying disease or risk factors. These false-positive results can be misleading and may not necessarily indicate the presence of a medical condition or immune-mediated hemolysis.
- Limited diagnostic value: The Coomb’s test, although a valuable tool, has limited diagnostic utility when used in isolation. It provides information about the presence of antibodies on red blood cells or in the serum but does not provide definitive evidence of a specific medical condition. Additional tests and clinical evaluation are often necessary to establish a definitive diagnosis.
- Inability to distinguish between different types of antibodies: The Coomb’s test does not differentiate between various types or subclasses of antibodies. It identifies the presence of antibodies but does not provide information about their specificity or potential clinical implications. Further testing and evaluation are required to determine the specific antibodies involved and their significance.
- False-negative results: In certain situations, the Coomb’s test may yield false-negative results, failing to detect the presence of antibodies that are present in low levels or in certain immune-mediated conditions. False-negative results can occur due to variations in antibody concentration, individual immune response, or technical limitations of the test.
- Limited in assessing antibody strength: The Coomb’s test may not accurately reflect the strength or potency of the antibodies present. It provides qualitative information about the presence or absence of antibodies but does not quantify the antibody levels or their functional activity. Quantitative assessment of antibody titers may be required for a more comprehensive evaluation.
- Lack of specificity for certain diseases: While the Coomb’s test is useful in detecting antibodies associated with certain conditions, it may lack specificity in identifying antibodies related to other diseases. Some medical conditions may have overlapping antibody profiles or may not exhibit detectable antibodies using the Coomb’s test alone, necessitating additional diagnostic approaches.
Despite these limitations, the Coomb’s test remains a valuable diagnostic tool in assessing immune-mediated hemolysis, blood transfusion compatibility, and certain medical conditions. It should be interpreted in conjunction with clinical evaluation, other laboratory tests, and medical history to obtain a comprehensive assessment and accurate diagnosis.
FAQ
What is Coomb’s test?
Coomb’s test is a laboratory test used to detect antibodies that may be present on red blood cells or circulating in the blood. It helps diagnose conditions related to immune-mediated destruction of red blood cells and assess blood transfusion compatibility.
What are the two types of Coomb’s tests?
The two types of Coomb’s tests are the Direct Coomb’s test and the Indirect Coomb’s test.
What is the difference between Direct and Indirect Coomb’s tests?
The Direct Coomb’s test detects antibodies that are already attached to red blood cells, while the Indirect Coomb’s test detects antibodies present in the blood serum.
When is the Direct Coomb’s test used?
The Direct Coomb’s test is used to diagnose immune-mediated hemolytic anemias, determine the cause of jaundice in newborns, and investigate transfusion reactions.
When is the Indirect Coomb’s test used?
The Indirect Coomb’s test is used to identify antibodies in the blood serum that could potentially cause reactions during blood transfusions or in conditions like Rh incompatibility during pregnancy.
How is the Coomb’s test performed?
In the Direct Coomb’s test, red blood cells are washed and then mixed with anti-human globulin serum. In the Indirect Coomb’s test, the patient’s serum is mixed with known red blood cells. After incubation and washing, anti-human globulin serum is added, and agglutination is observed.
What does a positive Coomb’s test result indicate?
A positive result in the Coomb’s test means that there is agglutination or clumping of red blood cells, indicating the presence of antibodies that can cause immune reactions or hemolysis.
What does a negative Coomb’s test result indicate?
A negative Coomb’s test result means that there is no agglutination or clumping of red blood cells, indicating the absence of antibodies that can cause immune reactions or hemolysis.
What are the limitations of the Coomb’s test?
Limitations of the Coomb’s test include non-specific results, limited diagnostic value without additional tests, inability to differentiate between different types of antibodies, and the possibility of false-negative or false-positive results.
Is the Coomb’s test the only test used to diagnose conditions related to immune-mediated destruction of red blood cells?
No, the Coomb’s test is just one of the tests used in the diagnostic process. It is often used in conjunction with other laboratory tests, clinical evaluation, and medical history to establish a comprehensive diagnosis.
References
- Theis SR, Hashmi MF. Coombs Test. [Updated 2022 Sep 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK547707/
- Parija S.C. (2012). Textbook of Microbiology & Immunology.(2 ed.). India: Elsevier India.
- Coombs, R. R.; Mourant, A. E.; Race, R. R. (1945). “A new test for the detection of weak and incomplete Rh agglutinins”. British journal of experimental pathology. 26: 255–66.
- Sastry A.S. & Bhat S.K. (2016). Essentials of Medical Microbiology. New Delhi : Jaypee Brothers Medical Publishers.
- Lydyard, P.M., Whelan,A.,& Fanger,M.W. (2005).Immunology (2 ed.).London: BIOS Scientific Publishers.
- http://www.shareyouressays.com/knowledge/useful-notes-on-coombs-test/115418