What is Cross Matching?
- Cross Match is a laboratory test, performed prior to a blood transfusion to determine whether donor blood is compatible (or incompatible) with recipient blood.
- The Compatibility can be determined by matching the different blood group systems, such as ABO and Rh system, and/or by directly testing for the presence of antibodies against a sample of donor tissues or blood.
- The main purpose of this test is to distinguish the appearance of antibodies in the recipient against the red blood cells of the donor. These antibodies can be found on the surface of red blood cells of the donor after transfusion.
- An incompatible transfusion can lead to severe hemolytic anemia and even death.
- The Cross Match test does not perform in dogs and horses, because in them the naturally occurring antibody against important hemolytic red blood cell antigens are absent. Hence, these animals need sensitization to the red cell antigen, before a hemolytic reaction will occur.
- After completion of blood transfusion to a dog or horse, a crossmatch should be performed prior to any subsequent transfusions to detect antibodies that may have been produced against a different red blood cell antigen.
Purpose of Blood Cross Matching
This test is performed as the final step of pretransfusion compatibility testing. The main purpose of compatibility tests are to detect: irregular antibodies; errors in ABO grouping, and clerical errors in patient identification and result recording. The cross match is used to detect;
The purpose of blood cross matching is to ensure compatibility between a recipient’s blood and a donated blood product, such as red blood cells, platelets, or plasma. The test is typically performed before a blood transfusion or organ transplant to reduce the risk of a reaction between the recipient’s blood and the donated blood product.
There are several different blood cross matching tests that may be performed, depending on the type of blood product being transfused or the specific blood group system being tested. Some common blood cross matching tests include the ABO blood group cross matching test, the Rh blood group cross matching test, the major crossmatch or antibody screening test, and the minor crossmatch or direct antiglobulin test (DAT).
In general, blood cross matching tests are designed to detect the presence of antibodies in the recipient’s blood that may react with the donated blood cells. If the recipient’s blood contains antibodies that are specific to certain blood groups, they may bind to the donated blood cells and cause them to clump together. This indicates that there is an incompatibility between the recipient’s blood and the donated blood, and that the transfusion or transplant should not proceed.
By performing a blood cross matching test before a transfusion or transplant, healthcare providers can ensure that the donated blood product is compatible with the recipient’s blood and reduce the risk of a reaction between the two. This helps to ensure the safety and success of the transfusion or transplant.
Principle of Cross Matching
Cross-matching is based on the serological detection of any clinically significant abnormal/unexpected antibodies in the blood of either the donor or the receiver. There are two varieties of cross-matching:
Major Cross Match: It entails comparing the donor’s red cells with the recipient’s serum to evaluate the presence of any antibodies that may cause hemolysis or agglutination of the donor’s red cells. This is more crucial than minor cross-matching.
Minor Cross Match: It entails analysing donor plasma with recipient red cells to evaluate the presence of any antibodies that may cause hemolysis or agglutination.
| Type | Donor’s | Recipient’s |
|---|---|---|
| Major Cross Match | Red Cells | Serum/Plasma |
| Minor Cross Match | Serum/Plasma | Red Cells |
Types of cross match
Blood cross matching is a laboratory test that is used to determine compatibility between a potential blood donor and a recipient before a blood transfusion is given. There are several types of blood cross matching that are used to ensure the safety of the transfusion:
1. ABO blood group cross matching
This type of cross matching involves matching the ABO blood group of the donor and recipient. The ABO blood group system consists of four blood types: A, B, AB, and O. It is important to match the blood type of the donor and recipient to avoid complications such as hemolysis (the breakdown of red blood cells).
Principle of ABO blood group cross matching
The ABO blood group cross matching principle involves matching the ABO blood group of the donor and recipient to ensure compatibility before a blood transfusion is given. The ABO blood group system consists of four blood types: A, B, AB, and O.
In order for a blood transfusion to be successful, the blood type of the donor and recipient must be compatible. If the blood types of the donor and recipient are incompatible, it can cause a transfusion reaction, which is an adverse reaction that occurs when the donor’s blood and the recipient’s blood are incompatible.
The ABO blood group cross matching principle is based on the presence or absence of certain antigens on the surface of red blood cells. Antigens are proteins that are found on the surface of red blood cells and are used by the body’s immune system to identify foreign substances.
There are two main antigens in the ABO blood group system: A and B. If a person’s red blood cells have the A antigen, they are blood type A. If their red blood cells have the B antigen, they are blood type B. If their red blood cells have both the A and B antigens, they are blood type AB. If their red blood cells have neither the A nor the B antigens, they are blood type O.
In order to ensure compatibility between the donor and recipient, the blood type
2. Rh blood group cross matching
This type of cross matching involves matching the Rh blood group of the donor and recipient. The Rh blood group system consists of two blood types: Rh positive and Rh negative. It is important to match the Rh blood type of the donor and recipient to avoid complications such as hemolysis (the breakdown of red blood cells).
Principle of Rh blood group cross matching
The Rh blood group system is a system of blood typing that is used to classify red blood cells based on the presence or absence of a particular protein called the Rh factor. People who have the Rh factor are known as Rh-positive, while those who do not have the Rh factor are known as Rh-negative.
The Rh blood group cross matching test is a laboratory test that is performed to determine if a person’s blood is compatible with a particular blood product, such as red blood cells, platelets, or plasma. The test is typically performed before a blood transfusion or organ transplant to ensure that the recipient’s body will not reject the donated blood or organ.
To perform the Rh blood group cross matching test, a small sample of the recipient’s blood is mixed with a sample of the donated blood. The samples are then incubated together and observed for any signs of agglutination, or clumping of the red blood cells. If the red blood cells clump together, it indicates that there is an incompatibility between the two blood samples and that the transfusion or transplant should not proceed.
The principle behind the Rh blood group cross matching test is based on the presence or absence of antibodies in the recipient’s blood that may react with the Rh factor on the donated blood cells. If the recipient’s blood contains antibodies that are specific to the Rh factor, they may bind to the donated blood cells and cause them to clump together. This indicates that there is an incompatibility between the recipient’s blood and the donated blood, and that the transfusion or transplant should not proceed.
3. Antibody screening
This type of cross matching involves testing the recipient’s blood for antibodies that may react with the donor’s blood. If the recipient has antibodies that react with the donor’s blood, it could cause a transfusion reaction.
Principle of Antibody screening
The antibody screening test is a laboratory test that is used to determine if a person’s blood contains antibodies that may react with a particular blood product, such as red blood cells, platelets, or plasma. The test is typically performed before a blood transfusion or organ transplant to ensure that the recipient’s body will not reject the donated blood or organ.
The principle behind the antibody screening test is based on the presence of antibodies in the recipient’s blood that may react with the donated blood cells. Antibodies are proteins that are produced by the immune system to help protect the body against foreign substances, such as bacteria and viruses. If the recipient’s blood contains antibodies that are specific to certain blood groups, they may bind to the donated blood cells and cause them to clump together. This indicates that there is an incompatibility between the recipient’s blood and the donated blood, and that the transfusion or transplant should not proceed.
To perform the antibody screening test, a small sample of the recipient’s blood is mixed with a sample of the donated blood. The mixed blood samples are then incubated together and observed for any signs of agglutination, or clumping of the red blood cells. If agglutination occurs, it indicates that there is an incompatibility between the recipient’s blood and the donated blood, and that the transfusion or transplant should not proceed. If no agglutination occurs, the result is reported as compatible and the transfusion or transplant can proceed.
It is important to note that the antibody screening test is just one of several tests that may be performed to ensure compatibility between a recipient’s blood and a donated blood product. Other tests may include cross matching for specific blood group systems, such as the ABO and Rh blood group systems, as well as testing for other antibodies or antigens that may cause a reaction between the recipient’s blood and the donated blood product.
4. Direct antiglobulin test (DAT)
This type of cross matching involves testing the donor’s blood for antibodies that may react with the recipient’s red blood cells. If the donor’s blood contains antibodies that react with the recipient’s red blood cells, it could cause a transfusion reaction.
Principle of Direct antiglobulin test (DAT)
The direct antiglobulin test (DAT), also known as the direct Coombs test, is a laboratory test that is used to detect the presence of antibodies or other proteins on the surface of red blood cells. The test is typically used to diagnose autoimmune hemolytic anemia, a condition in which the body’s immune system mistakenly attacks and destroys its own red blood cells.
The principle behind the DAT is based on the fact that antibodies or other proteins can bind to the surface of red blood cells and cause them to clump together or agglutinate. To perform the DAT, a small sample of the person’s blood is mixed with a solution containing antihuman globulin, a protein that binds to antibodies or other proteins on the surface of red blood cells. If antibodies or other proteins are present on the surface of the red blood cells, they will bind to the antihuman globulin and cause the red blood cells to clump together. This indicates the presence of antibodies or other proteins on the surface of the red blood cells.
The DAT is typically performed in conjunction with other laboratory tests, such as the indirect antiglobulin test (IAT) and the complete blood count (CBC), to diagnose autoimmune hemolytic anemia and to determine the appropriate treatment.
It is important to note that the DAT is just one of several tests that may be used to diagnose autoimmune hemolytic anemia. Other tests may include the IAT, the CBC, and tests to measure the levels of certain enzymes and proteins in the blood.
5. Autocontrol
This cross match test is performed between the recipient serum with recipient red blood cells.
It’s worth noting that blood cross matching is an important step in the process of transfusing blood to ensure the safety of the recipient. It helps to reduce the risk of transfusion reactions and other complications that may occur as a result of the transfusion.
Requirement
- Red Cells from donor’s body and Serum/Plasma from Recipient’s (For Major Cross Match).
- Serum/Plasma from donor’s body and Red Cells from Recipient’s (For Minor Cross Match).
Cross Matching Procedure
There are present various techniques for cross-matching. Among them, Anti-human globulin (AHG) cross match technique is widely used. Some examples of Cross Match techniques are;
| Method of Cross Match | Detects Antibody of Type : |
|---|---|
| Saline Cross Match | IgM |
| Albumin Cross Match | IgG |
| Anti-Human Globulin (AHG) Cross Match | IgG |
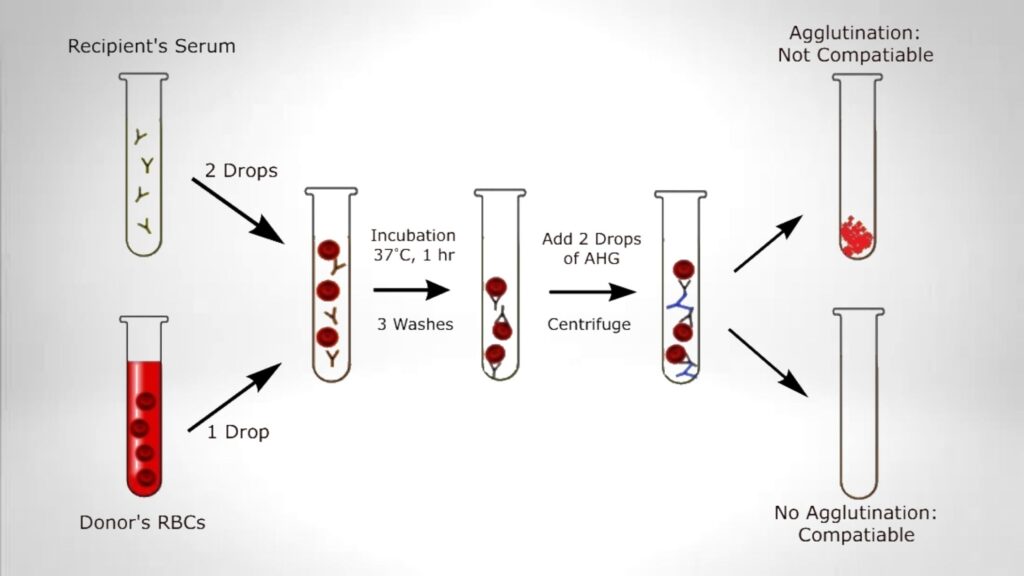
Major Cross Match
- Prepare blood samples from both the donor and the recipient, including the donor’s red cells and the recipient’s serum/plasma.
- Prepare a 3-5% red cell suspension in saline.
- Label a test tube.
- Add two drops of the donor’s serum and one drop of the recipient’s serum.
- Mix and incubate the tubes for 60 minutes at 37 degrees Celsius.
- Remove all of the serum and wash the cells three times in saline.
- Mix with two drops of Anti-human Globulin (AHG). Allow to stand for 5 minutes at room temperature.
- Centrifuge at 1500 rpm for 1 minute.
- Using both macro- and microscopy, search for agglutination.
- If no macroscopic agglutination is noticed, a little amount should be transferred to a glass slide and examined for microscopic agglutination. Rouleaux does not signify incompatibility.
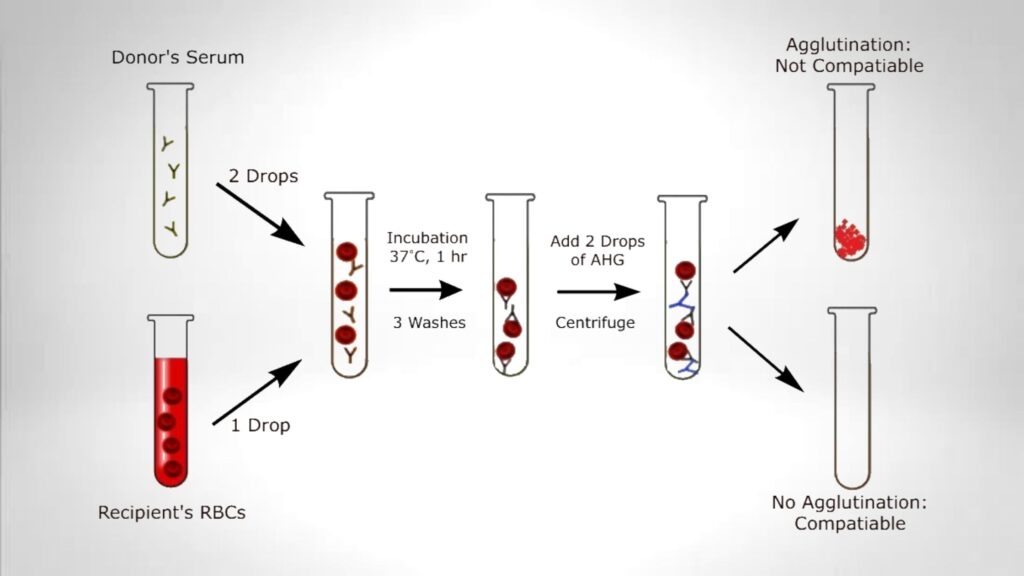
Minor Cross Match
- Prepare blood samples from the donor and recipient: the recipient’s red cells and the donor’s serum/plasma.
- Label a test tube.
- Add two drops of serum from the donor and one drop of cell suspension from the recipient.
- Mix and incubate the tubes for 60 minutes at 37 degrees Celsius.
- Remove all of the serum and wash the cells three times in saline.
- Mix with two drops of Anti-human Globulin (AHG). Allow to stand for 5 minutes at room temperature.
- Centrifuge at 1500 rpm for 1 minute.
- Using both macro- and microscopy, search for agglutination.
- If no macroscopic agglutination is noticed, a little amount should be transferred to a glass slide and examined for microscopic agglutination. Rouleaux does not signify incompatibility.
Result of Cross Matching
Both major and minor cross-matches should reveal no agglutination between compatible donor and receiver blood. Blood that is incompatible in a major cross-match should never be transfused, as the recipient’s huge plasma volume containing antibodies can quickly destroy the donor’s red cells. Minor incompatibility is less significant since the antibodies in the donor’s serum are diluted in the recipient’s plasma, rendering them useless.
Application of Cross Match test
- This test is used during a blood transfusion.
- Cross Match test is used if anyone having a certain medical problem that could cause significant blood loss, such as a cesarean section, a renal biopsy, or a cholecystectomy.
- Used for sickle cell disease or thalassemia.
- Used to check the effects of chemotherapy.
- Used for detection of a bleeding disorder, for example, hemophilia.
- During pregnancy, this test is used to find out if the patient is Rh-negative or positive.
- This test is performed during organ transplant, bone marrow transplant, or tissue transplant.
Why to Get Cross matching?
Cross matching is a laboratory test that is used to determine compatibility between a potential blood donor and a recipient before a blood transfusion is given. There are several reasons why cross matching is important:
- To reduce the risk of transfusion reactions: Cross matching helps to reduce the risk of transfusion reactions, which are adverse reactions that can occur when the donor’s blood and the recipient’s blood are incompatible. Transfusion reactions can range from mild to severe and can include symptoms such as fever, chills, shortness of breath, and hives.
- To ensure the safety of the transfusion: Cross matching helps to ensure the safety of the transfusion by identifying any potential incompatibilities between the donor’s blood and the recipient’s blood. This helps to reduce the risk of complications that may occur as a result of the transfusion.
- To match the blood type of the donor and recipient: Cross matching helps to match the blood type of the donor and recipient to avoid complications such as hemolysis (the breakdown of red blood cells). It is important to match the blood type of the donor and recipient to ensure that the transfusion is successful and does not cause any adverse reactions.
- To match the Rh blood group of the donor and recipient: Cross matching also helps to match the Rh blood group of the donor and recipient. The Rh blood group system consists of two blood types: Rh positive and Rh negative. It is important to match the Rh blood type of the donor and recipient to avoid complications such as hemolysis (the breakdown of red blood cells).
Overall, cross matching is an important step in the process of transfusing blood to ensure the safety of the recipient and to reduce the risk of transfusion reactions and other complications that may occur as a result of the transfusion.
Why do I need this test?
It is not possible for me to determine why you specifically may need a blood cross matching test without more information. Blood cross matching is a laboratory test that is used to determine compatibility between a potential blood donor and a recipient before a blood transfusion is given. There are several reasons why a person may need to have a blood cross matching test, including:
- To prepare for a blood transfusion: If you are going to receive a blood transfusion, your healthcare provider may order a blood cross matching test to ensure that the donor’s blood is compatible with your blood. This helps to reduce the risk of transfusion reactions and other complications that may occur as a result of the transfusion.
- To check for bleeding disorders: If you have a bleeding disorder, your healthcare provider may order a blood cross matching test to determine if you have any antibodies that may react with the donor’s blood. If you have antibodies that react with the donor’s blood, it could cause a transfusion reaction.
- To prepare for surgery: If you are going to have surgery, your healthcare provider may order a blood cross matching test to ensure that you have enough red blood cells and to check for any potential incompatibilities between your blood and the donor’s blood.
- To diagnose a blood disorder: If you are experiencing symptoms that may be related to a blood disorder, your healthcare provider may order a blood cross matching test to help diagnose the condition.
It is important to speak with your healthcare provider to determine why you specifically may need a blood cross matching test. They will be able to provide you with more information about the test and the specific reasons why it is being ordered.
What happens if crossmatch is positive?
If a blood crossmatch test is positive, it indicates that there is an incompatibility between a recipient’s blood and a donated blood product. This means that the transfusion or transplant should not proceed unless additional testing or precautions are taken to ensure the safety and success of the procedure.
A positive crossmatch does not necessarily mean that the transfusion or transplant cannot proceed, but it does indicate that additional testing or precautions may be necessary to ensure the safety and success of the procedure. Some possible options in the event of a positive crossmatch may include:
- Performing additional crossmatching tests to determine the specific cause of the incompatibility
- Using a different blood product that is compatible with the recipient’s blood
- Pretreating the recipient’s blood with medications to remove or neutralize any antibodies that may cause a reaction with the donated blood product
- Using a blood product from a universal donor, such as type O negative red blood cells
It is important to carefully follow the transfusion or transplant guidelines and protocols to ensure the safety and success of the procedure, even in the event of a positive crossmatch.
FAQ
What is the cross matching of blood?
Blood cross matching is a laboratory test that is used to determine if a person’s blood is compatible with a particular blood product, such as red blood cells, platelets, or plasma. The test is typically performed before a blood transfusion or organ transplant to ensure that the recipient’s body will not reject the donated blood or organ.
There are several different blood cross matching tests that may be performed, depending on the type of blood product being transfused or the specific blood group system being tested. Some common blood cross matching tests include the ABO blood group cross matching test, the Rh blood group cross matching test, the major crossmatch or antibody screening test, and the minor crossmatch or direct antiglobulin test (DAT).
To perform a blood cross matching test, a small sample of the recipient’s blood is mixed with a sample of the donated blood. The mixed blood samples are then incubated together and observed for any signs of agglutination, or clumping of the red blood cells. If the red blood cells clump together, it indicates that there is an incompatibility between the two blood samples and that the transfusion or transplant should not proceed. If no agglutination occurs, the result is reported as compatible and the transfusion or transplant can proceed.
The purpose of blood cross matching is to ensure compatibility between a recipient’s blood and a donated blood product and to reduce the risk of a reaction between the two. This helps to ensure the safety and success of the transfusion or transplant.
What are the 3 phases of crossmatching?
There are typically three phases to the blood crossmatching process:
The pretransfusion phase: This phase involves collecting a small sample of the recipient’s blood and testing it to determine the person’s blood type and the presence of any antibodies that may react with the donated blood product.
The compatibility phase: This phase involves mixing a sample of the recipient’s blood with a sample of the donated blood product and observing the mixed blood samples for any signs of agglutination, or clumping of the red blood cells. If the red blood cells clump together, it indicates that there is an incompatibility between the two blood samples and that the transfusion or transplant should not proceed.
The post-transfusion phase: This phase involves monitoring the recipient for any adverse reactions or complications following the transfusion or transplant. This may include monitoring the person’s vital signs, such as heart rate, blood pressure, and temperature, as well as checking for any signs of allergic reactions or hemolytic reactions.
It is important to note that the specific steps and procedures involved in the blood crossmatching process may vary depending on the specific test being performed and the type of blood product being transfused or transplanted. In addition, other tests and procedures may be performed to ensure compatibility between the recipient’s blood and the donated blood product.
Which blood products need crossmatch?
Crossmatching is typically performed before transfusing or transplanting any blood product that contains red blood cells, such as whole blood or packed red blood cells. Crossmatching is also typically performed before transfusing or transplanting platelets or plasma.
The purpose of crossmatching is to ensure compatibility between a recipient’s blood and the donated blood product and to reduce the risk of a reaction between the two. This helps to ensure the safety and success of the transfusion or transplant.
It is important to note that not all blood products require crossmatching. For example, some blood products, such as albumin or immunoglobulin, do not contain red blood cells and do not require crossmatching. In addition, some blood products, such as type O negative red blood cells, are considered “universal donors” and do not require crossmatching with the recipient’s blood. However, it is always important to carefully follow the transfusion or transplant guidelines and protocols to ensure the safety and success of the procedure.
What is a positive crossmatch?
A positive crossmatch refers to a situation in which there is an incompatibility between a recipient’s blood and a donated blood product, as detected by a blood crossmatching test.
Blood crossmatching tests are typically performed before a blood transfusion or organ transplant to ensure compatibility between the recipient’s blood and the donated blood product and to reduce the risk of a reaction between the two. There are several different blood crossmatching tests that may be performed, depending on the type of blood product being transfused or the specific blood group system being tested.
During a blood crossmatching test, a small sample of the recipient’s blood is mixed with a sample of the donated blood. The mixed blood samples are then incubated together and observed for any signs of agglutination, or clumping of the red blood cells. If the red blood cells clump together, it indicates that there is an incompatibility between the two blood samples and that the transfusion or transplant should not proceed. This result is referred to as a positive crossmatch.
A positive crossmatch does not necessarily mean that the transfusion or transplant cannot proceed, but it does indicate that additional testing or precautions may be necessary to ensure the safety and success of the procedure.
Why is albumin used in cross matching?
Albumin is a protein that is found in the blood and is responsible for helping to maintain the proper balance of fluids in the body. It is not typically used in the crossmatching process itself, but it may be used as a part of the testing procedure in some cases.
In some cases, albumin may be added to the recipient’s blood sample during a blood crossmatching test to help maintain the stability of the red blood cells. This is because albumin helps to keep the red blood cells suspended in the blood plasma and prevents them from clumping together or settling to the bottom of the test tube.
It is important to note that albumin is not typically used as a blood product in itself, and is not typically transfused or transplanted. Rather, it is used to help maintain the proper balance of fluids in the body and is typically produced by the liver. In some cases, albumin may be used to treat conditions that cause a deficiency of albumin in the blood, such as liver disease or malnutrition. However, albumin is not typically used in the crossmatching process itself.
When should crossmatch samples be taken?
Crossmatching samples are typically collected before a blood transfusion or organ transplant to ensure compatibility between the recipient’s blood and the donated blood product and to reduce the risk of a reaction between the two.
The specific timing for collecting crossmatching samples may vary depending on the type of blood product being transfused or transplanted and the specific transfusion or transplant guidelines and protocols. In general, crossmatching samples should be collected and tested as soon as possible before the transfusion or transplant to ensure that the results are available in time to make a decision about the procedure.
It is important to follow the transfusion or transplant guidelines and protocols carefully when collecting crossmatching samples to ensure the accuracy and reliability of the results. This may include taking care to properly label the samples and handle them according to recommended guidelines to avoid contamination or degradation.
In addition to crossmatching samples, other tests and procedures may also be performed before a transfusion or transplant to ensure compatibility between the recipient’s blood and the donated blood product and to reduce the risk of a reaction between the two. These may include tests to determine the recipient’s blood type and the presence of any antibodies that may react with the donated blood product, as well as tests to evaluate the recipient’s overall health and readiness for the procedure.
How long does crossmatch last for?
The results of a blood crossmatch test are typically considered valid for a certain period of time, depending on the specific test being performed and the transfusion or transplant guidelines and protocols.
In general, the results of a crossmatch test are considered valid for a period of time ranging from several hours to several days, depending on the specific circumstances. For example, the results of a crossmatch test performed before a blood transfusion may be considered valid for several hours, while the results of a crossmatch test performed before an organ transplant may be considered valid for several days.
It is important to note that the validity of the crossmatch test results may be affected by a number of factors, including the stability of the blood samples, the presence of any changes in the recipient’s blood or health status, and the specific transfusion or transplant guidelines and protocols. In some cases, it may be necessary to perform additional crossmatching tests or to take other precautions to ensure the safety and success of the transfusion or transplant.
It is always important to carefully follow the transfusion or transplant guidelines and protocols and to consult with a healthcare provider to determine the appropriate course of action based on the specific circumstances.
How long does a crossmatch take?
The amount of time it takes to perform a blood crossmatch test can vary depending on the specific test being performed and the transfusion or transplant guidelines and protocols. In general, most crossmatching tests take a few hours to a full day to complete.
The specific steps involved in a crossmatching test can also affect the amount of time it takes to complete the test. For example, some crossmatching tests may require multiple steps and multiple rounds of incubation and observation, while others may be more streamlined and require fewer steps.
It is important to note that the time it takes to perform a crossmatching test may also be affected by other factors, such as the availability of the necessary equipment and supplies, the workload of the laboratory, and the overall complexity of the test. In some cases, it may be necessary to prioritize certain crossmatching tests or to perform additional tests to ensure the accuracy and reliability of the results.
It is always important to carefully follow the transfusion or transplant guidelines and protocols and to consult with a healthcare provider to determine the appropriate course of action based on the specific circumstances.
What does a negative crossmatch test reveal?
A negative crossmatch test result indicates that there is no incompatibility between a recipient’s blood and a donated blood product, as detected by a blood crossmatching test. This means that the transfusion or transplant can proceed as planned, assuming there are no other contraindications or issues that need to be addressed.
Blood crossmatching tests are typically performed before a blood transfusion or organ transplant to ensure compatibility between the recipient’s blood and the donated blood product and to reduce the risk of a reaction between the two. There are several different blood crossmatching tests that may be performed, depending on the type of blood product being transfused or the specific blood group system being tested.
During a blood crossmatching test, a small sample of the recipient’s blood is mixed with a sample of the donated blood. The mixed blood samples are then incubated together and observed for any signs of agglutination, or clumping of the red blood cells. If the red blood cells do not clump together, it indicates that there is no incompatibility between the two blood samples and that the transfusion or transplant can proceed as planned. This result is referred to as a negative crossmatch.
It is important to note that a negative crossmatch does not necessarily mean that the transfusion or transplant can proceed without any additional precautions or considerations. Other tests and procedures may also be performed to ensure the safety and success of the procedure.
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.