What is Vitamin D?
- Vitamin D, often referred to as the “sunshine vitamin,” is a crucial component in our body. It is not merely a vitamin but functions more like a hormone. This fat-soluble secosteroid plays a pivotal role in facilitating the absorption of calcium, magnesium, and phosphate in our intestines, thereby influencing various biological processes.
- The primary source of vitamin D is the synthesis of cholecalciferol in the lower layers of our skin. This synthesis occurs through a photochemical reaction triggered by UVB radiation, either from direct sunlight or UVB lamps. Besides this natural synthesis, vitamin D can also be obtained from specific dietary sources and supplements. Notably, only a handful of foods, such as fatty fish, contain significant amounts of vitamin D. In many countries, including the U.S., certain foods like cow’s milk and breakfast cereals are fortified with vitamin D to ensure adequate intake.
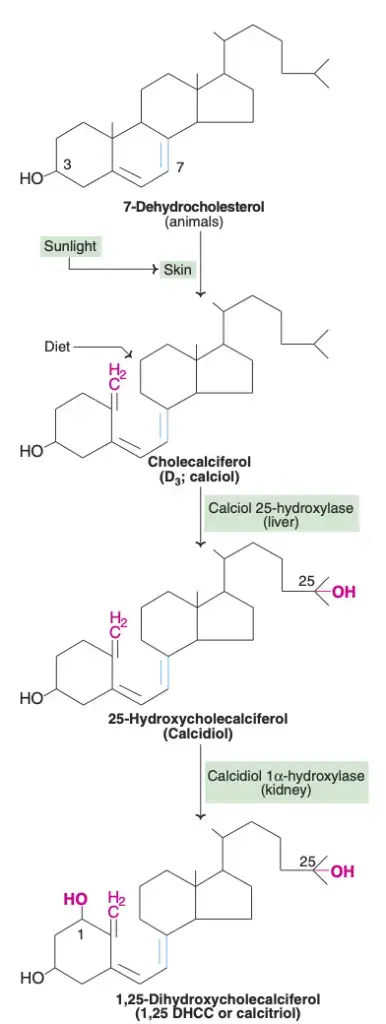
- However, it’s essential to understand that the vitamin D we obtain from the sun, food, or supplements is biologically inactive. It undergoes two crucial hydroxylation processes in the body to become active. The first takes place in the liver, converting vitamin D to 25-hydroxyvitamin D, and the second occurs in the kidneys, producing the active form known as calcitriol. This active form then circulates as a hormone in the bloodstream, regulating calcium and phosphate concentrations. This regulation ensures healthy bone growth and remodeling.
- Therefore, vitamin D is indispensable for maintaining bone health. It prevents conditions like rickets in children and osteomalacia in adults. Besides its skeletal benefits, vitamin D also modulates cell growth, neuromuscular functions, immune functions, and reduces inflammation. It’s noteworthy that many tissues in our body have vitamin D receptors, indicating its widespread influence.
- In dietary supplements and foods, vitamin D exists in two primary forms: D2 (ergocalciferol) and D3 (cholecalciferol). Both forms are effectively absorbed in the small intestine. The presence of dietary fat enhances this absorption, but some absorption still occurs in its absence.
- To assess an individual’s vitamin D status, the serum concentration of 25(OH)D is measured. This concentration reflects both the vitamin D produced in the skin and that obtained from dietary sources. However, determining vitamin D status can be complex due to the variability in the assays used for measurement. Despite this, it’s widely accepted that serum concentrations less than 30 nmol/L indicate vitamin D deficiency.
- In conclusion, vitamin D is vital for our overall health, especially bone health. It ensures the proper absorption of essential minerals and plays various roles in our body’s cellular functions. Therefore, maintaining adequate levels of vitamin D is crucial for optimal health.
Definition of Vitamin D
Vitamin D is a fat-soluble secosteroid that plays a crucial role in calcium absorption in the gut, promoting bone health and regulating various other biological functions. It can be naturally obtained from sunlight exposure, certain foods, and supplements. Once ingested or synthesized in the skin, it undergoes activation in the liver and kidneys to form its active form, calcitriol, which then functions as a hormone in the body.
Properties of Vitamin D
Vitamin D is a fat-soluble vitamin that plays a crucial role in various physiological processes. Here are some of the properties of Vitamin D:
- Nature: Vitamin D is fat-soluble, which means it is stored in the body’s fatty tissues and can be stored for long periods.
- Types: There are two main forms of Vitamin D:
- Vitamin D2 (ergocalciferol): Found in some plants and fungi.
- Vitamin D3 (cholecalciferol): Produced in the skin when exposed to sunlight and found in certain animal-based foods.
- Synthesis: Vitamin D can be synthesized by the body when the skin is exposed to ultraviolet B (UVB) rays from the sun. This is the primary natural source of Vitamin D for many people.
- Role in Calcium Metabolism: Vitamin D is essential for the absorption of calcium from the intestines. It helps maintain adequate serum calcium and phosphate concentrations, ensuring proper mineralization of bones.
- Bone Health: It plays a vital role in bone growth and bone remodeling by osteoblasts and osteoclasts. Without sufficient Vitamin D, bones can become thin, brittle, or misshapen.
- Immune System: Vitamin D also modulates the immune system and has anti-inflammatory properties.
- Deficiency: A deficiency in Vitamin D can lead to rickets in children and osteomalacia in adults, conditions where the bones become soft and weak.
- Sources: Apart from sunlight, Vitamin D can be obtained from foods such as fatty fish (like salmon, mackerel, and sardines), fortified dairy products, beef liver, cheese, and egg yolks.
- Supplementation: For individuals who have limited sun exposure or dietary sources, Vitamin D supplements can be taken to ensure adequate levels.
- Toxicity: While it’s rare, excessive Vitamin D intake can lead to hypercalcemia, a condition where there’s too much calcium in the blood, leading to nausea, vomiting, weakness, and serious complications like kidney damage.
Recommended Intakes of Vitamin D
Vitamin D, a vital nutrient for the human body, has specific intake recommendations set by expert committees of the National Academies of Sciences, Engineering, and Medicine (NASEM). These recommendations, known as Dietary Reference Intakes (DRIs), are designed to cater to the nutritional needs of healthy individuals. The DRIs encompass several values:
- Recommended Dietary Allowance (RDA): This represents the average daily intake level that suffices to meet the nutrient requirements of nearly 97%–98% of healthy individuals. It is a standard used for planning nutritionally adequate diets for individuals.
- Adequate Intake (AI): This level of intake is believed to ensure nutritional adequacy. It is established when there isn’t enough evidence to formulate an RDA.
- Estimated Average Requirement (EAR): This is the average daily intake level estimated to meet the requirements of half the healthy population. It’s primarily used to assess nutrient intakes of groups and can also be applied to individuals.
- Tolerable Upper Intake Level (UL): This is the maximum daily intake that is unlikely to cause adverse health effects.
The RDAs for vitamin D were set by an FNB committee with the primary goal of maintaining bone health and ensuring normal calcium metabolism in healthy people. The values are provided in both micrograms (mcg) and international units (IU), with the conversion being 1 mcg of vitamin D equivalent to 40 IU. It’s worth noting that while sunlight can be a significant source of vitamin D for some, the RDAs were established under the assumption of minimal sun exposure. For infants, the AI was determined based on the amount of vitamin D that maintains specific serum levels and supports bone development.
The table below provides a detailed breakdown of the RDAs for vitamin D:
Recommended Dietary Allowances (RDAs) for Vitamin D
| Age | Male | Female | Pregnancy | Lactation |
|---|---|---|---|---|
| 0-12 months* | 10 mcg (400 IU) | 10 mcg (400 IU) | – | – |
| 1–13 years | 15 mcg (600 IU) | 15 mcg (600 IU) | – | – |
| 14–18 years | 15 mcg (600 IU) | 15 mcg (600 IU) | 15 mcg (600 IU) | 15 mcg (600 IU) |
| 19–50 years | 15 mcg (600 IU) | 15 mcg (600 IU) | 15 mcg (600 IU) | 15 mcg (600 IU) |
| 51–70 years | 15 mcg (600 IU) | 15 mcg (600 IU) | – | – |
| >70 years | 20 mcg (800 IU) | 20 mcg (800 IU) | – | – |
*Note: The value for 0-12 months is an Adequate Intake (AI).
Different countries and professional societies might have varying guidelines for vitamin D intakes due to differences in understanding its biology, the purpose of the guidelines, and the types of studies used to establish recommendations. For instance, the Endocrine Society suggests that adults might need a minimum of 37.5 to 50 mcg (1,500–2,000 IU)/day, and children and adolescents might require at least 25 mcg (1,000 IU)/day. On the other hand, the UK government recommends an intake of 10 mcg (400 IU)/day for those aged 4 years and above.
Therefore, it’s essential to consult specific national or organizational guidelines when determining the appropriate vitamin D intake.
Structure of Vitamin D

Vitamin D, a crucial nutrient, exists in various forms, each with its unique chemical structure. Two primary forms of vitamin D are ergocalciferol (vitamin D2) and cholecalciferol (vitamin D3).
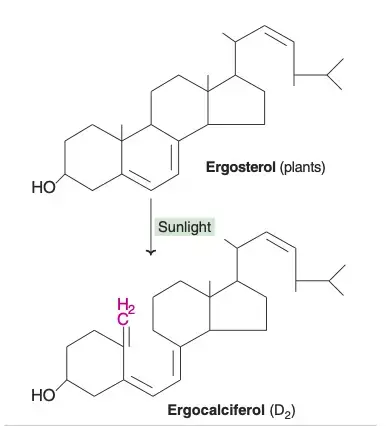
Ergocalciferol (Vitamin D2): This form of vitamin D is derived from ergosterol and is predominantly found in plants. Its structure is similar to cholecalciferol, with two distinct differences: ergocalciferol possesses an additional methyl group and a double bond. Due to its origin and structure, ergocalciferol is often referred to as a provitamin.
Cholecalciferol (Vitamin D3): This variant of vitamin D is present in animals. It is synthesized during the cholesterol biosynthesis process, where 7-dehydrocholesterol acts as an intermediate. When the skin is exposed to sunlight, this intermediate undergoes a transformation, converting 7-dehydrocholesterol into cholecalciferol. Therefore, vitamin D is often termed the “sunshine vitamin.”
The synthesis of vitamin D3 in the skin is directly proportional to sunlight exposure. However, it’s essential to note that the dark skin pigment, melanin, can adversely influence the production of cholecalciferol. This means that individuals with darker skin tones might require more sunlight exposure to produce the same amount of vitamin D3 as those with lighter skin tones.
Besides these two primary forms, there was once a term “vitamin D1,” which is no longer in use. Initially, it referred to a fat-soluble crystalline material. However, subsequent research revealed that it was a mixture, leading to its discontinuation in scientific literature.
In conclusion, both ergocalciferol and cholecalciferol play pivotal roles in providing vitamin D activity in the body. Their unique chemical structures and sources make them essential for various biological functions.
Types of Vitamin D
Vitamin D, a crucial nutrient for various physiological functions, exists in several forms, commonly referred to as vitamers. These vitamers differ in their chemical structure and origin. Here’s a detailed exposition of the various types of vitamin D:
- Vitamin D2 (Ergocalciferol): This form of vitamin D is derived from ergosterol and is known as ergocalciferol. Chemically characterized in 1931, its structure contains a unique double bond between carbons 22 and 23 and a methyl group on carbon 24. It’s noteworthy to mention that ergocalciferol is not produced by the human body but is found in certain plant sources.
- Vitamin D3 (Cholecalciferol): Cholecalciferol, or vitamin D3, is the form synthesized from 7-dehydrocholesterol in the skin upon exposure to ultraviolet radiation. Its chemical structure was defined in 1935, highlighting the importance of sunlight in vitamin D synthesis. Unlike D2, D3 is produced naturally by the human body when the skin is exposed to sunlight.
- Vitamin D1: This is a mixture of molecular compounds, combining ergocalciferol with lumisterol in a 1:1 ratio. However, the term “Vitamin D1” is less commonly used in modern literature.
- Vitamin D4 (22-dihydroergocalciferol): Another variant of vitamin D, D4 is known as 22-dihydroergocalciferol. Its occurrence and significance are less prominent compared to D2 and D3.
- Vitamin D5 (Sitocalciferol): Derived from 7-dehydrositosterol, sitocalciferol is termed as vitamin D5. Like D4, its prominence in literature and practical applications is limited.
From a chemical perspective, all forms of vitamin D are classified as secosteroids. In simple terms, they are steroids with one of the bonds in their rings broken. The primary distinction between D2 and D3 lies in their side chains. Over the years, many analogues of vitamin D have been synthesized for various research and therapeutic purposes.
Therefore, understanding the different types of vitamin D and their respective structures and functions is crucial for both health professionals and the general public. This knowledge aids in making informed decisions regarding supplementation, dietary choices, and sun exposure.
Absorption, transport and storage of Vitamin D
Vitamin D, a fat-soluble vitamin, undergoes a detailed process of absorption, transport, and storage within the human body.
- Absorption: Vitamin D is primarily absorbed in the small intestine. For this absorption to occur efficiently, the presence of bile is crucial. Once absorbed, vitamin D doesn’t directly enter the bloodstream. Instead, it travels through the lymphatic system.
- Transport: After its absorption, vitamin D enters the circulation, where it binds to a specific protein called plasma a2-globulin. This binding ensures the vitamin’s effective distribution to various parts of the body.
- Storage: The liver, along with other tissues, plays a pivotal role in storing vitamin D, albeit in small quantities. This storage ensures a steady supply of the vitamin, even when dietary intake or sunlight exposure is limited.
Metabolism of Calcitriol
Calcitriol, scientifically known as 1,25-dihydroxy cholecalciferol, is the active form of vitamin D. The metabolic pathway of calcitriol involves several steps:
- Initial Conversion in the Liver: Cholecalciferol undergoes conversion in the liver by the enzyme cholecalciferol-25-hydroxylase, resulting in the formation of 25-hydrocholecalciferol, also known as calcidiol.
- Action in the Placenta: Interestingly, the placenta also contains an enzyme named 25-hydroxycholecalciferol-1-hydroxylase, emphasizing the importance of vitamin D metabolism during pregnancy.
- Final Conversion in the Kidney: In the kidneys, based on the body’s requirements, calcidiol can be further converted. When there’s adequate calcitriol, the enzyme 24-hydroxylase transforms calcitriol into 24,25-dihydroxy cholecalciferol. This compound plays a significant role in maintaining calcium and phosphorus homeostasis, ensuring proper bone health and various other physiological functions.
Therefore, the intricate processes of absorption, transport, storage, and metabolism ensure that vitamin D is available to fulfill its numerous roles in the body, from bone health to immune function. The body’s ability to regulate and store vitamin D showcases the importance of this nutrient in maintaining overall health.
Biochemical functions of Vitamin D
Vitamin D, particularly its biologically active form, Calcitriol (1,25-DHCC), plays a pivotal role in regulating the plasma levels of essential minerals like calcium and phosphate. The intricate biochemical actions of Calcitriol ensure that plasma calcium levels remain within the normal range of 9–11 mg/dl. Here’s a detailed exposition of the multifaceted functions of Calcitriol:
- Action on the Intestine: Calcitriol significantly enhances the intestinal absorption of both calcium and phosphate. Within the cells of the intestine, Calcitriol binds to a specific cytosolic receptor, forming a complex. This calcitriol-receptor complex then interacts with the cell’s nucleus and specific DNA sequences, leading to the synthesis of a unique calcium-binding protein. This protein subsequently amplifies the uptake of calcium by the intestine. It’s noteworthy to mention that the mechanism through which Calcitriol operates in the intestine mirrors the action of steroid hormones.
- Action on the Bone: The bone, a major reservoir for calcium and phosphate, is also influenced by Calcitriol. In osteoblasts, which are bone-forming cells, Calcitriol promotes the uptake of calcium, facilitating its deposition as calcium phosphate. This process is vital for bone formation. Furthermore, in conjunction with the parathyroid hormone, Calcitriol aids in mobilizing calcium and phosphate from the bone, elevating their levels in the plasma.
- Action on the Kidney: The kidney, another target organ for Calcitriol, plays a role in conserving calcium and phosphate. Calcitriol minimizes the loss of these minerals through urine by reducing their excretion and promoting their reabsorption in the kidneys.
Besides Calcitriol, another metabolite of vitamin D, known as 24,25-Dihydroxycholecalciferol (24,25-DHCC), is synthesized in the kidney by the enzyme 24-hydroxylase. The precise function of 24,25-DHCC remains somewhat elusive. However, it’s postulated that when Calcitriol levels are adequate, 24-hydroxylase becomes active, leading to the synthesis of 24,25-DHCC, a compound of lesser importance. This synthesis is believed to be crucial in maintaining calcium homeostasis.
Biosynthesis of Vitamin D
Vitamin D, a pivotal nutrient, undergoes a unique biosynthesis process that is intricately linked to ultraviolet (UV) radiation. This synthesis is not just confined to humans but extends to various animals and fungi. Here’s a detailed and sequential explanation of this process:
- Photochemical Synthesis: The synthesis of vitamin D in both animals and fungi is rooted in photochemistry. Specifically, many animals convert 7-dehydrocholesterol to vitamin D3, while many fungi transform ergosterol to vitamin D2. The conversion of 7-dehydrocholesterol to vitamin D3 is a two-step process. First, under the influence of ultraviolet light, 7-dehydrocholesterol undergoes a photolytic reaction resulting in previtamin D3. Then, previtamin D3 spontaneously isomerizes to vitamin D3 through an antarafacial sigmatropic shift. This transformation is notably quicker in the skin compared to an organic solvent. Similarly, ergosterol undergoes photolysis to form previtamin D2, which then isomerizes to vitamin D2.
- Synthesis in the Skin: The skin, specifically its epidermal strata, plays a central role in vitamin D3 production. The precursor, 7-dehydrocholesterol, is abundantly produced and reacts with UVB light, which has wavelengths ranging from 290–315 nm. This UVB light can be sourced from natural sunlight or from UV lamps in tanning beds. It’s worth noting that glass windows block UVB light, rendering them ineffective for this synthesis. The amount of sun exposure required for adequate vitamin D production varies based on skin pigmentation and sunlight intensity. Interestingly, the skin has a protective mechanism where it degrades vitamin D at the same rate as its production, preventing overdose from UV exposure.
- Evolutionary Perspective: From an evolutionary standpoint, vitamin D synthesis is ancient. It began with photosynthesizing phytoplankton in the ocean over 500 million years ago. As land vertebrates evolved, they either consumed vitamin D from their diet or synthesized it through sun exposure. Birds and fur-bearing mammals have a unique mechanism where vitamin D is derived from oily secretions on their fur or feathers, which they ingest during grooming.
- Industrial Synthesis: On an industrial scale, vitamin D3 is produced by exposing 7-dehydrocholesterol to UVB and UVC light, followed by a purification process. This 7-dehydrocholesterol can be sourced from fish organs or wool grease from sheep. Vitamin D2, on the other hand, is synthesized using ergosterol from yeast or mushrooms.

Mechanism of action of Vitamin D
Vitamin D, a vital nutrient, undergoes a series of metabolic activations to execute its biological functions. The process is intricate, sequential, and highly regulated. Here’s a detailed expository explanation of the mechanism of action of Vitamin D:
- Metabolic Activation:
- Liver Hydroxylation: Once Vitamin D enters the bloodstream, it travels to the liver. Here, it undergoes a transformation into the prohormone calcifediol, also known as 25-hydroxycholecalciferol or 25(OH)D. This conversion is facilitated by the enzyme vitamin D 25-hydroxylase, encoded by the CYP2R1 human gene. Once formed, calcifediol is released into the plasma and binds to the vitamin D-binding protein, an α-globulin carrier protein.
- Kidney Hydroxylation: Calcifediol is then transported to the kidneys. In the proximal tubules of the kidneys, calcifediol is hydroxylated at the 1-α position to form calcitriol, the biologically active form of vitamin D. This conversion is catalyzed by the enzyme 25-hydroxyvitamin D3 1-alpha-hydroxylase, encoded by the CYP27B1 human gene. The activity of CYP27B1 is influenced by factors like parathyroid hormone, calcium, and phosphate levels. Once formed, calcitriol circulates, binding to the vitamin D-binding protein, and exerts its effects on various organs, including the intestine, kidneys, and bones. Besides the kidneys, certain cells, such as monocyte-macrophages, also synthesize calcitriol. In these cells, calcitriol acts as a cytokine, bolstering the body’s defenses against microbial invaders by invigorating the innate immune system.
- Inactivation: The activity of both calcifediol and calcitriol can be diminished by hydroxylation at position 24, forming secalciferol and calcitetrol, respectively.
- Difference between Substrates: Vitamin D exists in two forms: Vitamin D2 (ergocalciferol) and Vitamin D3 (cholecalciferol). Both share a similar mechanism of action. However, there are subtle differences. For instance, metabolites from Vitamin D2 bind less effectively to the vitamin D-binding protein compared to those from Vitamin D3. Additionally, while Vitamin D3 can be hydroxylated to calcifediol by sterol 27-hydroxylase (CYP27A1), Vitamin D2 cannot.
- Intracellular Mechanisms: Once inside the target cell, calcitriol binds to the vitamin D receptor in the cytoplasm. This activated receptor then moves to the nucleus and binds to vitamin D response elements (VDRE) on specific genes. This binding stimulates the transcription of these genes, leading to increased production of proteins that mediate the effects of vitamin D. Some cellular responses to calcitriol are rapid, suggesting non-genomic actions of vitamin D. In these pathways, the membrane-bound PDIA3 may serve as an alternate receptor.
Synthesis of 1,25-DHCC
- Vitamins D2 and D3, though essential, are not inherently biologically active. Their metabolic pathways in the body are identical, leading them to be converted into their active forms. The intricate metabolism and biochemical functions of vitamin D can be visualized in specific diagrams, such as Fig.7.8.
- To begin with, cholecalciferol undergoes an initial hydroxylation at the 25th position. This process results in the formation of 25-hydroxycholecalciferol (25-OH D3). This transformation is facilitated by a specific hydroxylase enzyme located in the liver. It’s worth noting that 25-OH D3 stands as the predominant storage and circulatory form of vitamin D.
- Following this, the kidney plays a pivotal role. It houses a distinct enzyme known as 25-hydroxycholecalciferol (calcidiol) 1-hydroxylase. This enzyme is responsible for the hydroxylation of 25-hydroxycholecalciferol at the first position, leading to the synthesis of 1,25-dihydroxycholecalciferol (1,25-DHCC). Given that 1,25-DHCC possesses three hydroxyl groups situated at the 1st, 3rd, and 25th carbon positions, it is often referred to as calcitriol. The hydroxylation processes, both in the liver and kidney, necessitate the presence of cytochrome P450, NADPH, and O2. The detailed synthesis of calcitriol can be further explored in diagrams such as Figs.7.7 and 7.8.
- Furthermore, the synthesis of 1,25-DHCC is not arbitrary. It is meticulously regulated by the plasma concentrations of both calcium and phosphate. These two elements exert control over the hydroxylation reaction at position 1. A decrease in plasma phosphate levels amplifies the activity of 25-hydroxycholecalciferol 1-hydroxylase. On the other hand, a reduction in plasma calcium stimulates the production of parathyroid hormone. This hormone subsequently activates the 1-hydroxylase in the kidney. Therefore, while phosphate has a direct influence, calcium operates indirectly on the kidney’s 1-hydroxylase enzyme.
Regulation of the synthesis of 1,25-DHCC
- The synthesis of 1,25-DHCC, a pivotal compound in the body, is not a random occurrence but is meticulously regulated by specific factors. The concentration of 1,25-DHCC in the body is primarily influenced by the plasma levels of two crucial elements: calcium and phosphate. These elements play a decisive role in controlling the hydroxylation reaction that occurs at position 1.
- Delving deeper into the specifics, when there is a decrease in plasma phosphate levels, there is a corresponding increase in the activity of the enzyme 25-hydroxycholecalciferol 1-hydroxylase. This enzyme is instrumental in the hydroxylation process, emphasizing its functional significance in the synthesis pathway.
- On the other hand, the role of calcium is slightly more intricate. A reduction in plasma calcium levels triggers an increase in the production of the parathyroid hormone. This hormone, in turn, activates the 1-hydroxylase enzyme located in the kidneys. Therefore, while the influence of phosphate on the synthesis process is direct, calcium operates in a more indirect manner, primarily through its impact on the kidney’s 1-hydroxylase enzyme.
- In conclusion, the regulation of the synthesis of 1,25-DHCC is a detailed and sequential process. It underscores the functional roles of various components, such as enzymes and hormones, in ensuring that the body maintains optimal levels of this essential compound. The interplay between calcium and phosphate, and their respective direct and indirect influences, further highlights the complexity and precision of this regulatory mechanism.
Sources of Vitamin D
Vitamin D, often referred to as the “sunshine vitamin,” plays a pivotal role in maintaining bone health and aiding calcium absorption in the body. Therefore, understanding its sources is crucial for overall well-being. This article delves into the various sources of vitamin D, emphasizing their functions and importance.
- Natural Food Sources: Among the best natural sources of vitamin D are fatty fish such as trout, salmon, tuna, and mackerel. The vitamin D content in these fish is primarily in the form of vitamin D3 and its metabolite 25(OH)D3. Besides, fish liver oils stand out as potent sources of this essential nutrient. It’s noteworthy that an animal’s diet can influence the amount of vitamin D in its tissues. Other animal-based sources include beef liver, egg yolks, and cheese, which contain modest amounts of vitamin D. Mushrooms, particularly those exposed to UV light, provide vitamin D2. Some commercial mushrooms undergo UV treatment to enhance their vitamin D2 levels. The Food and Drug Administration (FDA) has even sanctioned UV-treated mushroom powder as a vitamin D2 source in food products.
- Fortified Foods: In the realm of fortified foods, they emerge as the primary contributors to vitamin D intake in American diets. For instance, a significant portion of the U.S. milk supply undergoes voluntary fortification, typically with vitamin D3. Other dairy derivatives, like cheese and ice cream, aren’t usually fortified. However, plant milk alternatives, such as those derived from soy, almond, or oats, often receive fortification akin to cow’s milk. Additionally, certain breakfast cereals, orange juices, yogurts, and margarines have added vitamin D.
- Sun Exposure: Sunlight remains a predominant source of vitamin D for most individuals. When the skin is exposed to UVB radiation, it converts cutaneous 7-dehydrocholesterol to previtamin D3, which subsequently transforms into vitamin D3. However, several factors, including season, time of day, and skin melanin content, can influence UV radiation exposure and, consequently, vitamin D synthesis. It’s essential to strike a balance between obtaining adequate sun exposure for vitamin D production and safeguarding the skin against potential UV damage.
- Dietary Supplements: For those who might not get enough vitamin D from natural sources or sunlight, dietary supplements serve as a viable alternative. These supplements can contain either vitamin D2 or D3. While both forms effectively raise serum 25(OH)D levels, vitamin D3 has shown a greater potency in increasing and maintaining these levels.
Vitamin D is a hormone and not a vitamin—justification
Vitamin D, commonly known as the “sunshine vitamin,” has been redefined in the scientific community as a hormone rather than a mere vitamin. This reclassification is based on its unique characteristics and functions that align more closely with hormones. Here’s a detailed and sequential explanation of why vitamin D is considered a hormone:
- Origin of Vitamin D3 (Cholecalciferol): Vitamin D3, or cholecalciferol, is not derived from dietary sources alone. Instead, it is synthesized in the skin when exposed to the ultraviolet rays of sunlight. This synthesis is akin to how certain hormones are produced in specific body parts.
- Conversion to Active Form: Once synthesized or ingested, vitamin D undergoes a transformation. The kidney plays a pivotal role in converting it into its biologically active form, calcitriol (1,25-DHCC). This process of conversion and activation is a hallmark of hormone functioning.
- Targeted Action: Just like hormones have specific target organs or cells, calcitriol also acts on specific target organs. The primary organs influenced by calcitriol are the intestine, bone, and kidney. In these organs, calcitriol performs specific functions, further emphasizing its role as a hormone.
- Mechanism of Action: Calcitriol’s mode of action mirrors that of steroid hormones. Upon formation, it binds to specific receptors in the cytosol. This complex then interacts with DNA, stimulating the synthesis of calcium-binding protein. This mechanism underscores its hormone-like behavior.
- Influence of Actinomycin D: The action of calcitriol can be inhibited by Actinomycin D. This interaction indicates that calcitriol impacts DNA, leading to RNA transcription. Such a direct influence on genetic material is characteristic of hormones.
- Self-Regulation: One of the defining features of hormones is their ability to self-regulate. Calcitriol exemplifies this by employing a feedback mechanism. In essence, as the levels of calcitriol rise, it suppresses its own synthesis, ensuring that its levels in the body are maintained within a narrow range.
Therefore, based on these characteristics and functions, it is evident that vitamin D operates more like a hormone than a traditional vitamin. Besides its role in calcium metabolism, it has a broader impact on various body functions. Then, considering its synthesis, conversion, targeted action, and self-regulation, it becomes clear that vitamin D’s classification as a hormone is well-justified. The consistent use of technical vocabulary, such as “cholecalciferol,” “calcitriol,” and “Actinomycin D,” further emphasizes the scientific and objective nature of this explanation.
Vitamin D deficiency
Causes of Vitamin D Deficiency:
- Limited Sunlight Exposure: The body produces vitamin D when the skin is exposed to sunlight. People who live in northern latitudes, wear long robes, or stay indoors frequently might not receive adequate sun exposure.
- Dietary Restrictions: Vitamin D is found in certain foods like fatty fish, fortified dairy products, and egg yolks. A strict vegan diet or avoidance of these foods can lead to deficiency.
- Malabsorption: Certain medical conditions, such as Crohn’s disease, cystic fibrosis, and celiac disease, can affect the intestine’s ability to absorb vitamin D from food.
- Kidney and Liver Diseases: These organs play a role in converting vitamin D to its active form. Diseases affecting these organs can lead to lower active vitamin D levels.
- Age: As people age, their kidneys become less efficient at converting vitamin D.
Symptoms of Vitamin D Deficiency:
- Bone Pain: Vitamin D plays a critical role in the absorption of calcium, which is necessary for healthy bone formation and maintenance. A deficiency can lead to bone pain and tenderness, often felt in the lower back, hips, and legs.
- Muscle Weakness: Inadequate vitamin D levels can result in muscle weakness, making everyday activities more challenging. This weakness may manifest as difficulty in climbing stairs, lifting objects, or standing up from a sitting position.
- Bone Deformities (Rickets in Children): Vitamin D deficiency in children can cause rickets. This condition is characterized by soft and weak bones, leading to deformities such as bowed legs, knock-knees, and a pigeon chest. Delayed teething and poor growth may also occur.
- Fractures and Osteoporosis (Osteomalacia in Adults): In adults, vitamin D deficiency can lead to a condition known as osteomalacia. This results in the weakening of bones, making them more susceptible to fractures. Osteoporosis, a condition characterized by reduced bone density and increased fracture risk, can also develop over time.
- Increased Falls: Muscle weakness and impaired balance due to vitamin D deficiency can contribute to an increased risk of falls, particularly among older adults. This can result in fractures and other injuries.
- Fatigue and Weakness: Vitamin D deficiency may lead to overall fatigue and a sense of weakness, which can impact a person’s daily activities and quality of life.
- Depression and Mood Disorders: Emerging research suggests a possible link between vitamin D deficiency and mood disorders like depression. While the exact mechanism is not fully understood, there is evidence that vitamin D may play a role in brain function and mood regulation.
- Impaired Immune Function: Vitamin D is involved in the regulation of the immune system. Deficiency can weaken the immune response, potentially making individuals more susceptible to infections and illnesses.
- Chronic Pain: Some individuals with chronic pain conditions, such as fibromyalgia, report symptom improvement when their vitamin D levels are optimized. While the relationship is not entirely clear, vitamin D deficiency may contribute to chronic pain in some cases.
- Increased Risk of Chronic Diseases: There is ongoing research into the potential links between vitamin D deficiency and various chronic diseases, including cardiovascular diseases, diabetes, and certain cancers. While the exact associations are complex and not fully established, maintaining adequate vitamin D levels is considered important for overall health.
Complications Arising from Vitamin D Deficiency:
- Rickets: A severe deficiency in children can lead to rickets, a condition where bone tissue doesn’t mineralize properly, leading to soft bones and skeletal deformities.
- Osteomalacia: In adults, deficiency can lead to osteomalacia, resulting in weak bones and muscles.
- Increased Risk of Chronic Diseases: Low vitamin D levels have been associated with chronic diseases, including coronary artery disease, asthma in children, and cancer.
Prevention and Treatment:
- Sunlight Exposure: Spending time outdoors, especially during midday, can help boost vitamin D levels.
- Dietary Sources: Consuming foods rich in vitamin D, such as salmon, mackerel, fortified cereals, and dairy products.
- Supplementation: Vitamin D supplements can be beneficial, especially for those at high risk of deficiency.
- Regular Screening: Periodic blood tests can help detect and monitor vitamin D deficiency.
Excessive Vitamin D
While a certain amount of this vitamin is necessary for optimal health, excessive intake can lead to a condition known as vitamin D toxicity or hypervitaminosis D.
Causes of Excessive Vitamin D:
- Supplement Overuse: The most common cause of vitamin D toxicity is the overconsumption of vitamin D supplements. Unlike vitamin D obtained from sun exposure, which the body can regulate, excessive intake from supplements can accumulate in the body.
- Medical Conditions: Some medical conditions, such as sarcoidosis or certain types of cancer, can increase the production of active vitamin D in the body.
- Medications: Some medications can increase vitamin D levels in the body.
Symptoms of Vitamin D Toxicity:
- Elevated Blood Calcium Levels: Excessive vitamin D can lead to increased calcium levels in the blood, known as hypercalcemia. This can result in calcium deposits in soft tissues, leading to potential damage to the heart, blood vessels, and kidneys.
- Digestive Issues: Nausea, vomiting, and loss of appetite can occur.
- Bone Pain and Muscle Weakness: Despite its role in bone health, too much vitamin D can cause bone pain.
- Neurological Symptoms: Confusion, disorientation, and problems with concentration can arise.
- Excessive Thirst and Frequent Urination: These are common symptoms of elevated calcium levels in the blood.
Potential Long-term Complications:
- Kidney Damage: Excessive calcium levels can lead to the formation of kidney stones and potential kidney damage.
- Heart and Blood Vessel Issues: Calcium deposits can lead to complications in the cardiovascular system.
- Bone Loss: Paradoxically, excessive vitamin D can lead to bone loss, making bones more susceptible to fractures.
Prevention and Treatment:
- Monitor Supplement Intake: It’s crucial to adhere to recommended dosages when taking vitamin D supplements. Regular check-ups and blood tests can help monitor vitamin D levels.
- Stay Hydrated: Drinking plenty of water can help reduce symptoms and complications associated with high calcium levels.
- Medical Intervention: In severe cases, medical treatment may be required, which could include medications to reduce calcium levels or intravenous fluids.
Tolerable Upper Intake Levels (ULs) for Vitamin D
| Age | Male & Female | Pregnancy | Lactation |
|---|---|---|---|
| 0-6 months | 25 mcg (1,000 IU) | – | – |
| 7–12 months | 38 mcg (1,500 IU) | – | – |
| 1–3 years | 63 mcg (2,500 IU) | – | – |
| 4–8 years | 75 mcg (3,000 IU) | – | – |
| 9–18 years | 100 mcg (4,000 IU) | 100 mcg (4,000 IU) | 100 mcg (4,000 IU) |
| 19+ years | 100 mcg (4,000 IU) | 100 mcg (4,000 IU) | 100 mcg (4,000 IU) |
What is Hypervitaminosis D?
- Vitamin D, a crucial nutrient for the body, is predominantly stored in the liver. From there, it undergoes a gradual metabolic process. Among the spectrum of vitamins available to us, vitamin D stands out due to its potential toxicity when consumed in excessive amounts, specifically 10 to 100 times the Recommended Dietary Allowance (RDA).
- Therefore, it is imperative to understand the repercussions of such an overdose, commonly referred to as hypervitaminosis D. One of the primary toxic effects of this condition is the demineralization of bone, a process known as resorption. Besides this, there is an enhanced absorption of calcium from the intestine. This, in turn, leads to an elevated level of calcium in the plasma, a condition termed hypercalcemia.
- Then, as a result of prolonged hypercalcemia, there is a risk of calcium deposition in various soft tissues. Notably, organs like the kidneys and arteries are susceptible to this deposition. Furthermore, hypervitaminosis D can pave the way for the formation of renal calculi, which are essentially stones in the kidneys.
- Besides these physiological changes, individuals with high consumption of vitamin D may exhibit certain symptoms. These include a loss of appetite, nausea, an increased sense of thirst, and weight loss, among others.
References
- Bikle DD. Vitamin D: Production, Metabolism and Mechanisms of Action. [Updated 2021 Dec 31]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK278935/
- https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
- https://www.nhs.uk/conditions/vitamins-and-minerals/vitamin-d/
- https://www.onlinebiologynotes.com/vitamin-d-synthesis-regulation-biological-roles-sources-and-deficiency/
- http://materiais.dbio.uevora.pt/BD/Crescimento/Vitamin-D.pdf