What is Urinary System?
- The urinary system, also known as the urinary tract or renal system, is a vital part of the human body responsible for eliminating waste products, regulating fluid balance, and maintaining the overall chemical stability of the body. It consists of several organs and structures working together to perform these important functions.
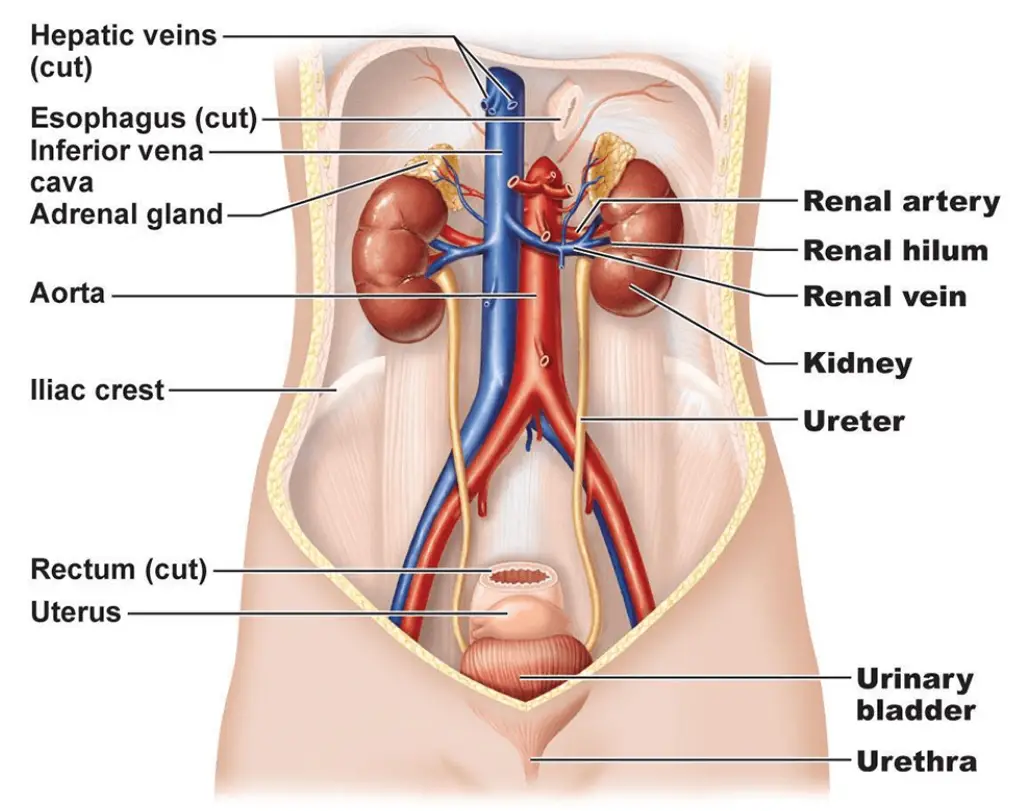
- At the core of the urinary system are the kidneys, two bean-shaped organs located on either side of the spine, just below the ribcage. The kidneys receive a rich blood supply through the renal arteries, allowing them to filter waste products and excess substances from the bloodstream. Each kidney is composed of tiny functional units called nephrons, which are responsible for the filtration process.
- As blood passes through the nephrons, waste products, toxins, excess water, and electrolytes are removed, forming a liquid waste called urine. The urine then travels from the kidneys to the bladder through narrow tubes called ureters. The ureters are muscular tubes that propel urine using peristaltic contractions, ensuring it reaches the bladder.
- The bladder serves as a storage reservoir for urine. It is a muscular organ that expands as urine accumulates and contracts when it’s time to urinate. The bladder’s capacity can vary depending on the individual, but it generally holds around 400-600 milliliters of urine. When the bladder reaches a certain level of fullness, it sends signals to the brain, triggering the sensation of needing to urinate.
- The final component of the urinary system is the urethra, a tube that connects the bladder to the external opening of the body. In males, the urethra is longer and serves a dual function by carrying urine and semen during ejaculation. In females, the urethra is shorter and only transports urine.
- The process of urination, or voiding, involves the contraction of the bladder muscles, which forces urine through the urethra and out of the body. The sphincters, located at the base of the bladder and within the urethra, help control the flow of urine by opening and closing as needed.
- The urinary system plays a crucial role in maintaining homeostasis within the body. By eliminating waste products and regulating fluid balance, it helps control blood volume and blood pressure. The kidneys also contribute to the regulation of electrolyte levels, such as sodium, potassium, and calcium, which are essential for proper cellular function. Additionally, the urinary system helps maintain the body’s acid-base balance, ensuring the pH levels remain within a narrow range for optimal physiological functioning.
- Furthermore, the urinary system is involved in erythropoiesis, the production of red blood cells. The kidneys produce and release a hormone called erythropoietin, which stimulates the bone marrow to produce new red blood cells. This hormone helps maintain an adequate supply of oxygen-carrying cells in the bloodstream.
- In summary, the urinary system is a complex network of organs and structures that work together to remove waste products, regulate fluid balance, maintain electrolyte levels, and contribute to various other physiological processes. Its efficient functioning is essential for the overall health and well-being of an individual.
Definition of Urinary System
The urinary system is a collection of organs, including the kidneys, ureters, bladder, and urethra, that work together to eliminate waste from the body, regulate fluid balance, and maintain the chemical stability of the body.
Anatomy of the Urinary System
Two kidneys, two ureters, a urinary bladder, and a urethra comprise the urinary system. The kidneys alone perform the duties above stated and produce urine, while the other organs of the urinary system serve as temporary storage reservoirs for urine or as transit channels to convey it from one bodily location to another.
1. The Kidneys
The kidneys are remarkable organs responsible for maintaining the purity and balance of our internal fluids. Here are some key features and characteristics of the kidneys:
- Location: The kidneys are located in the superior lumbar region against the dorsal body wall, beneath the parietal peritoneum (a membrane that lines the abdominal cavity). They extend from the T12 to the L3 vertebrae and are protected by the lower part of the rib cage.
- Positioning: The right kidney is positioned slightly lower than the left kidney due to the presence of the liver.
- Size: An adult kidney is approximately 12 cm (5 inches) long, 6 cm (2.5 inches) wide, and 3 cm (1 inch) thick, roughly the size of a large bar of soap.
- Adrenal Gland: Each kidney is topped by an adrenal gland, which is functionally distinct and part of the endocrine system.
- Fibrous Capsule: A transparent fibrous capsule surrounds each kidney, giving it a shiny appearance when fresh.
- Perirenal Fat Capsule: Surrounding each kidney is a mass of fatty tissue called the perirenal fat capsule, which acts as a cushioning layer.
- Renal Fascia: The outermost capsule of the kidney is the renal fascia, which not only encloses the kidney but also helps anchor it and hold it in place against the muscles of the trunk wall.
- Renal Cortex: The outer region of the kidney, light in color, is called the renal cortex.
- Renal Medulla: Deep to the cortex is a darker, reddish-brown area known as the renal medulla.
- Renal Pyramids: The medulla contains several triangular regions with a striped appearance called renal or medullary pyramids. The base of each pyramid faces toward the cortex, while the apex points toward the inner region of the kidney.
- Renal Columns: The renal columns are extensions of cortex-like tissue that separate the renal pyramids.
- Renal Pelvis: Medial to the hilum (the concave part of the kidney where the blood vessels and ureter enter), there is a flat, basin-like cavity called the renal pelvis. It is continuous with the ureter, which carries urine away from the kidney.
- Calyces: Extensions of the renal pelvis, known as calyces, form cup-shaped areas that enclose the tips of the renal pyramids. They collect urine continuously draining from the pyramids into the renal pelvis.
- Arterial Supply: The kidneys receive an arterial supply through the renal artery. As the renal artery approaches the hilum, it divides into segmental arteries, which further branch into interlobar arteries. At the cortex-medulla junction, interlobar arteries give rise to arcuate arteries, which curve over the medullary pyramids. Small cortical radiate arteries branch off the arcuate arteries and supply the cortical tissue.
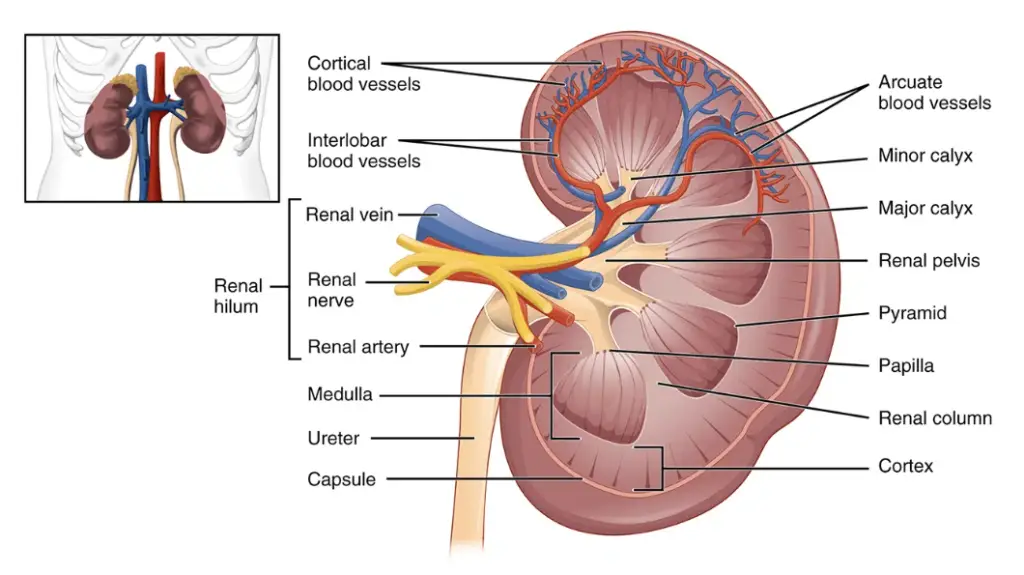
These features and structures contribute to the unique anatomy and function of the kidneys, allowing them to perform their essential role in maintaining fluid balance, filtering waste products, regulating blood pressure, and producing important hormones.
Nephrons
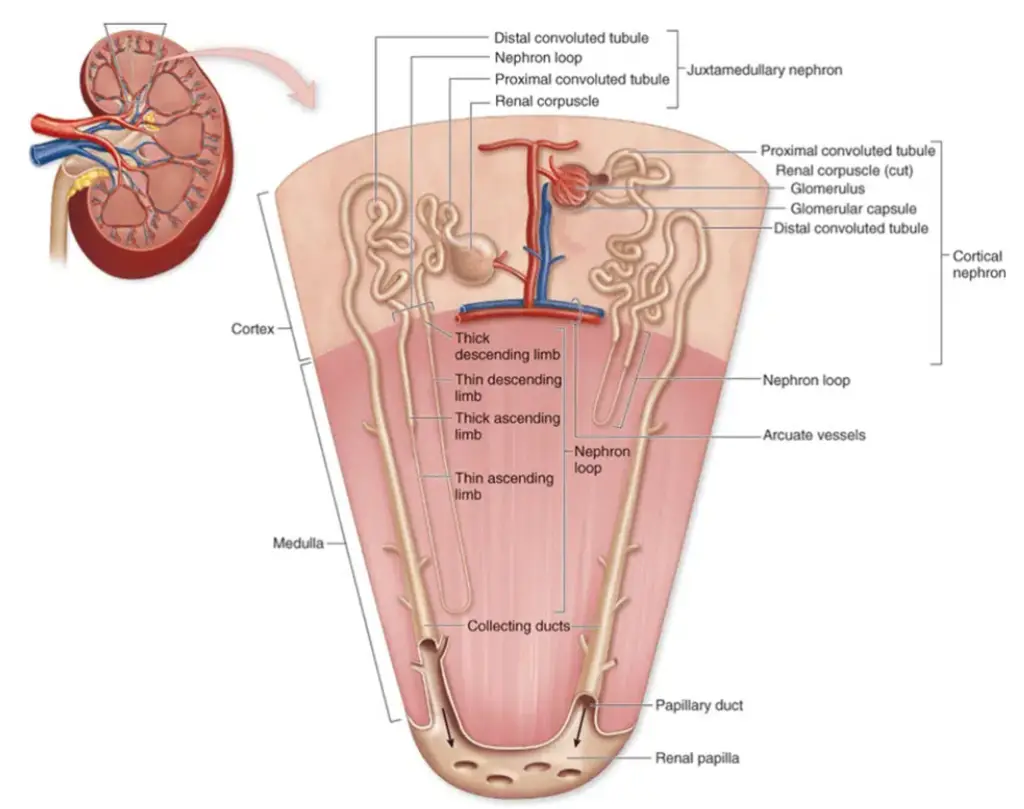
- Nephrons are the remarkable structural and functional units that lie at the heart of the kidneys’ intricate filtration and urine formation processes. In fact, each kidney houses an astonishing number, with over a million nephrons working tirelessly to maintain the body’s fluid balance and eliminate waste products.
- At the core of a nephron lies the glomerulus, a complex network of intertwining capillaries. This crucial component is responsible for the initial filtration of blood. As blood flows through the glomerulus, small molecules such as water, electrolytes, and waste substances are selectively filtered out, while larger molecules like proteins and blood cells are retained within the blood vessels.
- To further process the filtrate, the renal tubule comes into play. This convoluted tube is another essential structure within the nephron. At the beginning of the tubule, the glomerular or Bowman’s capsule embraces and surrounds the glomerulus. Comprised of a closed-end, cup-shaped structure, the Bowman’s capsule ensures that the filtrate is efficiently collected from the glomerulus.
- The inner layer of the Bowman’s capsule is formed by specialized cells known as podocytes. These remarkable cells resemble octopuses, with long, branching processes called foot processes that intricately interweave and attach themselves to the glomerulus. Through their unique structure, podocytes play a crucial role in regulating the filtration process and maintaining the integrity of the blood-urine barrier.
- As the tubule extends beyond the glomerular capsule, it meanders and coils, forming distinct regions with specific functions. The proximal convoluted tubule, situated near the glomerular capsule, is responsible for the reabsorption of vital substances like glucose, amino acids, and electrolytes from the filtrate back into the bloodstream. This reabsorption process ensures that essential molecules are not lost during urine formation.
- Continuing its intricate path, the tubule descends into the medulla, forming the loop of Henle. This hairpin loop consists of a descending limb, followed by an ascending limb. The loop of Henle plays a pivotal role in establishing and maintaining the concentration gradient within the kidney, crucial for the concentration and dilution of urine.
- After the loop of Henle, the tubule takes another twist and becomes the distal convoluted tubule. This final segment of the nephron is responsible for fine-tuning the reabsorption and secretion processes, further adjusting the composition of the filtrate according to the body’s needs.
- Two main types of nephrons exist: cortical nephrons and juxtamedullary nephrons. The majority of nephrons, known as cortical nephrons, are primarily located within the cortex, the outer region of the kidney. In contrast, juxtamedullary nephrons reside close to the cortex-medullary junction, and their unique feature is the presence of long loops of Henle that extend deep into the medulla. This anatomical distinction enables juxtamedullary nephrons to play a crucial role in establishing the concentration gradient needed for water reabsorption.
- To sustain the nephron’s intricate functions, a network of blood vessels supports its activities. The afferent arteriole serves as the “feeder vessel” that supplies blood to the glomerulus, arising from a cortical radiate artery. Once the blood has undergone filtration in the glomerulus, it exits through the efferent arteriole, which leads to the formation of peritubular capillaries. These capillaries surround the renal tubule, allowing for the exchange of substances between the bloodstream and the tubular fluid, ensuring reabsorption and secretion processes occur efficiently.
- Nephrons are true marvels of biological engineering. Their complex and precisely orchestrated structures enable the kidneys to maintain fluid balance, regulate electrolyte concentrations, and eliminate waste products from the body. Understanding the intricacies of nephron function provides insight into the remarkable processes that contribute to our overall health and well-being.
Ureters
- The ureters are an essential part of the urinary system, playing a vital role in the transport of urine from the kidneys to the bladder. These slender tubes, measuring approximately 25 to 30 cm (10 to 12 inches) in length and 6 mm (1/4 inch) in diameter, are responsible for facilitating the passage of urine through the urinary tract.
- Positioned behind the peritoneum, each ureter extends from the renal hilum, the area on the medial side of the kidney where blood vessels, nerves, and the renal pelvis are located. From there, the ureters travel towards the posterior aspect of the bladder, entering it at a slight angle.
- The primary function of the ureters is to transport urine produced by the kidneys to the bladder. This process involves the coordinated contraction of the smooth muscle layers present in the walls of the ureters. These contractions, known as peristalsis, create a wave-like motion that propels urine forward along the length of the ureters.
- To ensure unidirectional flow, the ureters employ a mechanism to prevent urine from flowing back into the kidneys. At the point where the ureters enter the bladder, there are small valve-like folds of bladder mucosa that flap over the ureter openings. These folds act as one-way valves, allowing urine to flow into the bladder but preventing it from moving back up the ureters.
- The ureters’ efficient functioning is crucial for maintaining the balance of bodily fluids and the elimination of waste products. By transporting urine from the kidneys to the bladder, the ureters facilitate the removal of metabolic waste, excess water, and other substances that need to be excreted from the body.
- In conclusion, the ureters serve as passageways that actively transport urine from the kidneys to the bladder. Their slender structure, position, and peristaltic contractions enable the efficient movement of urine through the urinary system. The presence of valve-like folds near the ureter openings ensures unidirectional flow, preventing the backward flow of urine. The proper functioning of the ureters is vital for maintaining a healthy urinary system and overall bodily homeostasis.
Urinary Bladder
- The urinary bladder is an important organ within the urinary system responsible for temporarily storing urine. It is a smooth, collapsible, and muscular sac that exhibits unique features suited to its role.
- Located retroperitoneally in the pelvis just posterior to the symphysis pubis, the urinary bladder occupies a specific position within the body. This location allows for convenient storage of urine without interfering with other bodily functions.
- The primary function of the urinary bladder is to store urine until it can be voluntarily eliminated during urination. To fulfill this role effectively, the bladder possesses specific anatomical and physiological characteristics. The detrusor muscles, found in the bladder wall, play a significant role in facilitating urine storage. These muscles are composed of smooth muscle fibers that contract and relax to regulate bladder volume and control the release of urine.
- Another important feature of the urinary bladder is its lining, composed of a special type of epithelium known as transitional epithelium. This epithelium is designed to accommodate the stretching and distention of the bladder as it fills with urine. It can undergo significant changes in shape and size without compromising its integrity, allowing the bladder to expand and contract as necessary.
- Within the bladder, there is a smooth, triangular region called the trigone. This area is outlined by three openings: two ureteral openings, where the ureters connect to the bladder, and one urethral opening, which connects the bladder to the outside of the body. The trigone is a crucial region prone to infections due to its shape and location. It serves as a potential reservoir for bacteria, leading to persistent urinary tract infections if not properly managed.
- In summary, the urinary bladder is a specialized organ that stores urine temporarily. Its retroperitoneal location, detrusor muscles, and transitional epithelium contribute to its unique ability to accommodate and store urine. The trigone within the bladder serves as a notable region susceptible to infections. Understanding the structure and function of the urinary bladder helps to appreciate its role in maintaining urinary system health and overall bodily homeostasis.
Urethra
- The urethra is a vital component of the urinary system responsible for carrying urine from the bladder to the exterior of the body. It is a thin-walled tube that facilitates the passage of urine through peristaltic contractions.
- At the junction between the bladder and the urethra, there is a thickening of the smooth muscle known as the internal urethral sphincter. This involuntary sphincter plays a crucial role in maintaining urinary continence by keeping the urethra closed when urine is not being passed. It helps prevent urine from leaking out of the bladder unintentionally.
- Additionally, there is a second sphincter called the external urethral sphincter. This sphincter is formed by skeletal muscle as the urethra passes through the pelvic floor and is under voluntary control. It allows for conscious control over the release of urine, enabling us to initiate or inhibit urination voluntarily.
- The female urethra is approximately 3 to 4 cm (1 1/2 inches) in length. Its external opening, or orifice, is located anteriorly to the vaginal opening. The female urethra is relatively short compared to the male urethra, reflecting the difference in anatomical structures between the two sexes.
- In males, the urethra is considerably longer, measuring around 20 cm (8 inches). It consists of three distinct regions: the prostatic urethra, the membranous urethra, and the spongy (penile) urethra. The prostatic urethra passes through the prostate gland, the membranous urethra traverses the muscular pelvic floor, and the spongy urethra extends through the length of the penis. The male urethra opens at the tip of the penis, allowing for the expulsion of urine.
- The urethra serves not only as a conduit for urine but also plays a role in the reproductive system. In males, it serves as the passageway for semen during ejaculation. In females, it functions solely for the elimination of urine.
- In summary, the urethra is a thin-walled tube that transports urine from the bladder to the outside of the body. It contains internal and external sphincters that regulate the flow of urine, and its structure and length vary between males and females. Understanding the anatomy and function of the urethra is essential for comprehending urinary control and the elimination of waste products from the body.
Physiology of the Urinary System
Urine Formation
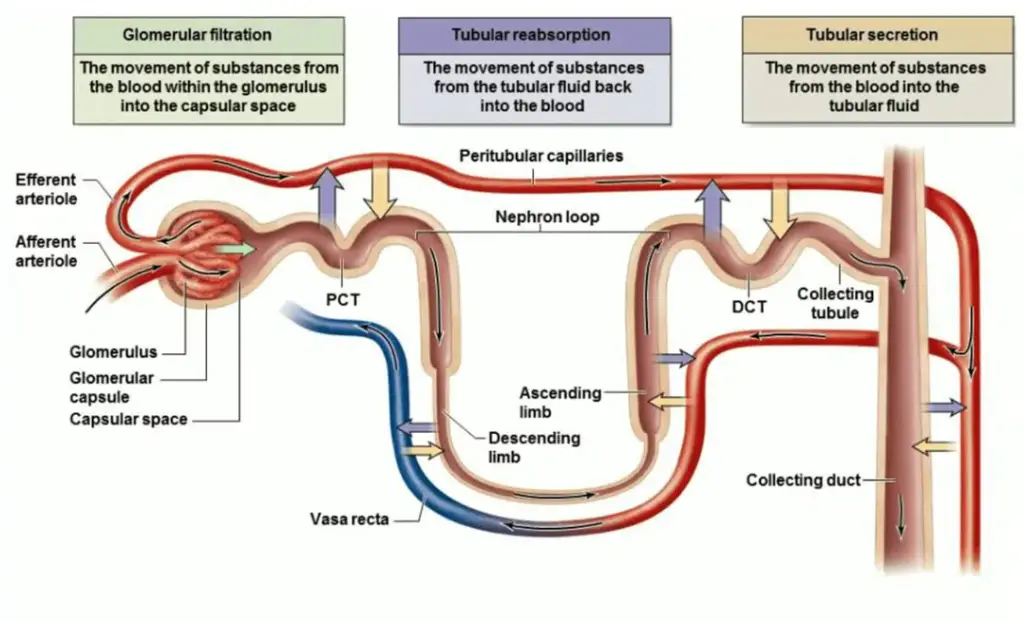
- The formation of urine is a complex process that involves three fundamental processes: glomerular filtration, tubular reabsorption, and tubular secretion. These processes occur within the nephrons, the functional units of the kidneys.
- The first step in urine formation is glomerular filtration. This process takes place in the glomerulus, a network of specialized capillaries located within the renal corpuscle. Blood is filtered under pressure, forcing water and small solutes, excluding proteins, through the capillary walls and pores of the glomerular capsule. This filtered fluid, known as the glomerular filtrate, enters the renal tubule, leaving behind larger molecules such as proteins and blood cells in the bloodstream.
- The second process, tubular reabsorption, occurs as the glomerular filtrate flows through the renal tubule. In this stage, essential substances that the body needs, such as water, glucose, amino acids, and ions, are reabsorbed from the filtrate and transported into the tubule cells. From there, these substances can enter the capillary blood surrounding the tubules and be returned to the systemic circulation. The reabsorption process helps maintain the body’s fluid balance, reabsorbing valuable substances while eliminating waste products.
- The third process, tubular secretion, involves the transfer of certain substances from the peritubular blood into the filtrate. Hydrogen ions, potassium ions, creatinine (a waste product of muscle metabolism), and certain drugs are actively secreted by the tubule cells into the filtrate. Tubular secretion allows the kidneys to regulate the acid-base balance, electrolyte levels, and excretion of certain substances, further refining the composition of urine.
- These three processes work together to form urine. As the glomerular filtrate passes through the renal tubules, it undergoes modifications, with reabsorption and secretion adjusting its composition. The final product, urine, contains waste products, excess water, electrolytes, and other substances that need to be eliminated from the body.
- Urine formation is a dynamic and highly regulated process carried out by the kidneys. It plays a crucial role in maintaining homeostasis by regulating fluid balance, electrolyte concentrations, and the excretion of waste products. Understanding the intricate processes involved in urine formation is essential for comprehending kidney function and the overall regulation of the body’s internal environment.
Characteristics of Urine
Urine exhibits several characteristic features that reflect its composition and the processes involved in its formation. These characteristics provide valuable information about kidney function and overall health. Here are some key characteristics of urine:
- Daily Volume: Despite the kidneys filtering a significant amount of blood plasma, the amount of urine produced in a 24-hour period is relatively small. On average, approximately 1.0 to 1.8 liters of urine are produced per day.
- Components: Urine contains various substances that the body needs to eliminate, including nitrogenous wastes such as urea and uric acid. It also includes unneeded substances like excess water, electrolytes, and other waste products generated by metabolic processes.
- Color: Freshly voided urine is typically clear and varies in color from pale yellow to deep yellow. The color is influenced by the concentration of waste products and the presence of pigments like urobilin, which results from the breakdown of red blood cells.
- Odor: Initially, urine is sterile and possesses a slightly aromatic odor. However, if left standing, bacteria present in the environment can act upon the urine solutes, leading to the development of an ammonia-like odor.
- pH: The pH of urine usually leans toward the slightly acidic side, with a typical value of around 6. However, changes in body metabolism or the consumption of certain foods can cause urine pH to become more acidic or basic.
- Specific Gravity: The specific gravity of urine measures its concentration compared to that of pure water. While water has a specific gravity of 1.0, urine typically falls within a range of 1.001 to 1.035, depending on its concentration of solutes and water content.
- Solutes: Urine contains a variety of solutes that are typically found in the body. These include sodium and potassium ions, urea, uric acid, creatinine, ammonia, bicarbonate ions, and other substances. The presence and concentration of these solutes provide insights into kidney function, electrolyte balance, and metabolic processes.
By analyzing the characteristics of urine, healthcare professionals can gain valuable information about a person’s hydration status, kidney function, and potential underlying health conditions. Changes in urine characteristics may indicate abnormalities or imbalances in the body, making urine analysis an important diagnostic tool.
Micturition
Micturition, also known as voiding, refers to the process of emptying the bladder to eliminate urine from the body. It involves a series of coordinated events that are regulated by the nervous system and muscular contractions. Here are the key aspects of micturition:
- Accumulation: The bladder continues to collect urine until approximately 200 ml of urine have accumulated. During this storage phase, the bladder expands to accommodate the increasing volume of urine.
- Activation: Once the bladder reaches its capacity and stretches, specialized stretch receptors in the bladder wall are activated. These receptors send signals to the central nervous system, indicating that the bladder is full and triggering the micturition process.
- Transmission: The stretch signals from the bladder are transmitted to the sacral region of the spinal cord through the pelvic splanchnic nerves. From there, nerve impulses are sent back to the bladder, causing it to enter into reflex contractions.
- Passage: The reflex contractions of the bladder muscles become stronger, resulting in increased pressure on the stored urine. This pressure forces the urine past the internal urethral sphincter, a thickening of the smooth muscle located at the junction of the bladder and urethra, into the upper part of the urethra.
- External sphincter: Simultaneously, the external urethral sphincter, a skeletal muscle surrounding the urethra, comes into play. This sphincter is under voluntary control, meaning we have the ability to consciously relax or contract it. When we choose to relax the external sphincter, urine is allowed to flow from the bladder through the urethra and out of the body. If we decide to keep the external sphincter contracted, urine elimination is prevented.
The micturition process is a finely coordinated action between the central nervous system, bladder muscles, and external urethral sphincter. It allows for the controlled and voluntary emptying of the bladder. By voluntarily controlling the external sphincter, we can decide when and where to initiate urination, providing a level of conscious control over the process.
Overall, micturition is a vital physiological function that ensures the elimination of waste products from the body. The coordinated interplay between neural signals and muscular contractions enables us to regulate the timing and control of urine elimination according to our needs.
Male Urogenital System
The male urogenital system consists of several organs and structures involved in reproduction and the elimination of waste products. Here are the key components of the male urogenital system:
- Testes: The testes are the primary reproductive organs in males. They are located within the scrotum and are responsible for the production of sperm through a process called spermatogenesis. The testes also produce testosterone, a hormone important for male sexual development and function.
- Epididymis: The epididymis is a coiled tube located on the posterior surface of each testis. It serves as a storage site for sperm and allows them to mature and gain the ability to swim.
- Vas deferens: The vas deferens is a muscular tube that connects the epididymis to the ejaculatory ducts. It carries mature sperm from the epididymis to the urethra during ejaculation.
- Ejaculatory ducts: The ejaculatory ducts are formed by the union of the vas deferens and the ducts from the seminal vesicles. They transport sperm and seminal fluid into the urethra.
- Urethra: The male urethra is a tube that extends from the urinary bladder to the external urethral orifice at the tip of the penis. It serves as a pathway for both urine and semen to exit the body, but not at the same time.
- Penis: The penis is the external male genital organ. It consists of a root and a body, and it plays a crucial role in sexual intercourse and the transfer of semen into the female reproductive tract.
- Prostate gland: The prostate gland is a walnut-sized gland located below the urinary bladder and surrounding the prostatic portion of the urethra. It produces a milky fluid that forms part of semen. This fluid contains various substances, such as enzymes and citrate ions, that nourish and support sperm.
- Accessory glands: The male urogenital system also includes accessory glands that contribute to the production of semen. These glands include the seminal vesicles and the bulbourethral glands. The seminal vesicles produce a fluid rich in fructose, which provides energy for sperm. The bulbourethral glands secrete a lubricating fluid that helps to prepare the urethra for the passage of sperm during ejaculation.
The male urogenital system is essential for reproductive functions and the elimination of waste. Its various components work together to produce, store, and transport sperm, as well as to facilitate the release of semen during sexual intercourse.
Male and Female Excretory System
The excretory system in males and females shares many similarities in terms of the structures involved, including the kidneys, ureters, bladder, and urethra. However, there are some sex differences that arise in the urinary system beyond the bladder neck.
- Kidneys: The kidneys serve as the primary excretory organs in both males and females. They develop from the lateral plate mesoderm and give rise to nephric ridges, which further differentiate into nephrotomes and nephrons. Nephrons are the structural and functional units of the kidneys responsible for filtering blood and producing urine. The basic structure and function of the kidneys are the same in males and females.
- Ureters: The ureters are tubular structures that carry urine from the kidneys to the bladder. They play a crucial role in transporting urine through peristaltic contractions of the smooth muscles in their walls. The structure and function of the ureters are identical in males and females.
- Bladder: The urinary bladder is responsible for temporary storage of urine. It is a muscular organ lined with epithelial cells. In mammals, including males and females, the bladder is typically large and capable of expanding to accommodate urine.
- Urethra: The urethra is a tubular organ that carries urine from the bladder to the outside of the body. In males, the urethra has a more complex structure and a longer length compared to females. It consists of four portions: the prostatic urethra, membranous urethra, bulbar urethra, and pendulous (or penile) urethra. The male urethra measures around 17-20 cm in length. In contrast, the female urethra is shorter, measuring about 2.5-4 cm in length.
The main differences between the male and female urinary systems lie in the structure and length of the urethra. Other than that, the overall anatomy and function of the excretory system, including the kidneys, ureters, and bladder, are similar in both sexes.
Development of Urogenital System
The development of the urogenital system is a complex process that involves the formation of various structures derived from the intermediate mesoderm. Here are the key stages in the development of the urogenital system:
- Urogenital Ridge Formation: The urogenital system originates from the intermediate mesoderm, which gives rise to a pair of urogenital ridges located on either side of the aorta. These ridges serve as the foundation for the development of the urogenital structures.
- Pronephros: The first tubular structure to develop is the pronephros, which is located at the cranial end of the urogenital ridge. However, the pronephros is not fully functional and regresses in most cases, playing a minimal role in kidney development.
- Mesonephros: The mesonephros develops along the midsection of the embryo from the intermediate mesoderm. It consists of mesonephric tubules and the mesonephric duct, also known as the Wolffian duct. Initially, some of the mesonephric tubules perform excretory functions similar to a kidney. However, many of these tubules regress over time. The mesonephric duct, on the other hand, persists and connects to the cloaca, a common cavity at the tail end of the embryo.
- Metanephros: The metanephros is the final and most significant stage of kidney development. It gives rise to the adult kidney in its definitive form. The metanephric blastema, which arises from the condensation of adjacent neurogenic intermediate mesoderm, plays a crucial role in this process. The caudal part of the mesonephric duct extends and forms a bud called the ureteric bud. The ureteric bud penetrates the metanephric blastema, and reciprocal interactions between the two structures lead to the formation of nephrons and the collecting system of the kidney.
Through these developmental processes, the urogenital system transforms from its initial rudimentary forms (pronephros and mesonephros) to the functional adult kidney (metanephros). This intricate series of events ensures the proper formation and function of the urogenital system, which is essential for urine production, waste elimination, and reproductive functions in the human body.
Female Urogenital System
The female urogenital system encompasses the reproductive and urinary organs in females. Here are the key components of the female urogenital system:
- Kidneys: The kidneys, two bean-shaped organs located in the lower back, are responsible for filtering waste products from the blood and producing urine. They play a crucial role in maintaining fluid and electrolyte balance in the body.
- Bladder: The urinary bladder is a muscular sac that stores urine temporarily before it is eliminated from the body. It expands as it fills with urine and contracts during urination to expel the urine through the urethra.
- Ureters: The ureters are two slender tubes that transport urine from the kidneys to the urinary bladder. They use peristaltic contractions of their smooth muscle walls to propel urine towards the bladder.
- Urethra: The urethra is a tube that connects the urinary bladder to the external opening. In females, it is shorter compared to males and serves as a passageway for urine to exit the body.
- Reproductive organs:
- Ovaries: The ovaries are the primary reproductive organs in females. They produce eggs (ova) and secrete hormones, including estrogen and progesterone, which regulate the menstrual cycle and pregnancy.
- Uterus: The uterus, also known as the womb, is a hollow, muscular organ where a fertilized egg implants and develops into a fetus. It undergoes cyclic changes during the menstrual cycle to prepare for pregnancy.
- Fallopian tubes: The fallopian tubes are thin tubes that connect the ovaries to the uterus. They play a crucial role in capturing eggs released from the ovaries and providing a site for fertilization to occur.
- Vagina: The vagina is a muscular canal that connects the uterus to the external genitalia. It serves as the birth canal during childbirth and allows for sexual intercourse. The vagina also provides a passage for menstrual blood to exit the body.
The female urogenital system is essential for reproductive functions, including the production and release of eggs, as well as the elimination of waste products through the urinary system. It undergoes significant changes during the menstrual cycle, pregnancy, and childbirth to support female reproductive health and fertility.
Functions of the Urinary System
The urinary system, composed of the kidneys, ureters, bladder, and urethra, performs several important functions to maintain the body’s overall health and balance. Here are the key functions of the urinary system:
- Filtration: The kidneys filter large amounts of fluid, known as filtrate, from the bloodstream every day. This filtration process removes waste products, excess ions, and toxins from the blood.
- Waste Processing: After filtration, the kidneys process the filtrate, selectively reabsorbing necessary substances, such as water, glucose, and electrolytes, back into the bloodstream. At the same time, waste products and excess ions are concentrated and eliminated in the form of urine.
- Elimination: The kidneys play a major role in eliminating nitrogenous wastes, toxins, and drugs from the body through urine. While other organs, like the lungs and skin, also contribute to excretion, the kidneys bear the primary responsibility for this function.
- Regulation of Blood Volume and Composition: The kidneys maintain the proper balance of water and salts, as well as the appropriate levels of acids and bases in the blood. By adjusting the reabsorption and excretion of these substances, the kidneys help regulate blood volume and maintain a stable internal environment.
- Blood Pressure Regulation: The kidneys produce an enzyme called renin, which plays a crucial role in regulating blood pressure. Renin initiates a series of reactions that ultimately influence blood vessel constriction and fluid balance in the body.
- Red Blood Cell Production: The hormone erythropoietin, produced by the kidneys, stimulates the production of red blood cells in the bone marrow. This hormone ensures an adequate supply of oxygen-carrying cells, supporting overall oxygenation and tissue health.
- Vitamin D Activation: Kidney cells convert inactive vitamin D into its active form. Active vitamin D is essential for the absorption of calcium and phosphate from the digestive system, promoting bone health and mineral balance in the body.
In summary, the urinary system plays a vital role in filtering and processing blood, eliminating waste products, regulating fluid and electrolyte balance, controlling blood pressure, stimulating red blood cell production, and activating vitamin D. These functions are crucial for maintaining overall health and homeostasis within the body.
FAQ
What is the urinary system?
The urinary system, also known as the renal system, is a collection of organs responsible for the production, storage, and elimination of urine from the body. It includes the kidneys, ureters, bladder, and urethra.
What are the kidneys, and what do they do?
The kidneys are two bean-shaped organs located on either side of the spine, just below the ribcage. Their main functions include filtering waste products from the blood, regulating fluid balance, controlling electrolyte levels, and producing hormones important for red blood cell production and blood pressure regulation.
What is the purpose of urine?
Urine serves as a means to eliminate waste products, excess water, electrolytes, and other substances from the body. It helps maintain the body’s fluid balance, remove toxins, and regulate various physiological processes.
How does urine formation occur?
Urine formation involves three main processes: glomerular filtration, tubular reabsorption, and tubular secretion. Glomerular filtration filters the blood, while tubular reabsorption and tubular secretion modify the filtrate to produce urine.
What are the ureters, and what is their role?
The ureters are two slender tubes that connect the kidneys to the bladder. Their primary function is to transport urine from the kidneys to the bladder through peristaltic contractions of their smooth muscle walls.
What is the urinary bladder, and what does it do?
The urinary bladder is a muscular sac that stores urine temporarily. It expands as it fills with urine and contracts during the process of urination to expel urine from the body.
What is the urethra, and what is its function?
The urethra is a tube that connects the urinary bladder to the external opening. Its main role is to carry urine from the bladder to the outside of the body during the process of urination.
How is urine eliminated from the body?
Urine is expelled from the body through the process of micturition or urination. It involves the coordinated contraction of the bladder muscles and relaxation of the urethral sphincters, allowing urine to flow out of the body.
What factors can affect urinary system health?
Various factors can impact urinary system health, including dehydration, infections (such as urinary tract infections), kidney stones, certain medications, urinary incontinence, and underlying medical conditions like kidney disease or diabetes.
How can one maintain a healthy urinary system?
Maintaining a healthy urinary system involves staying hydrated, maintaining good hygiene, avoiding excessive intake of substances that can irritate the urinary tract (like caffeine or alcohol), practicing safe sexual activity, and seeking prompt medical attention for any urinary issues or concerns.
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.