What is Urethra?
- The urethra is a vital anatomical structure responsible for transporting urine from the urinary bladder to the outside of the body through the urinary meatus. This tube also plays a crucial role in the reproductive system of placental mammals by facilitating the passage of semen during ejaculation.
- In males, the urethra is longer compared to females due to its additional function in the reproductive process. It serves as a conduit for both urine and semen, allowing for the expulsion of these fluids from the body.
- Control over urination is facilitated by two sphincter muscles. The external urethral sphincter, composed of striated muscle fibers, provides voluntary control over the flow of urine. On the other hand, the internal urethral sphincter, made up of involuntary smooth muscle fibers, controls the passage of urine through the urethra. This sphincter receives its nerve supply from the sympathetic division of the autonomic nervous system.
- Both males and females possess an internal urethral sphincter, which helps in the process of micturition, or the act of urination. This involuntary muscle regulates the flow of urine from the bladder into the urethra.
- In summary, the urethra is a vital component of the urinary and reproductive systems in mammals, facilitating the passage of urine and semen while being regulated by both voluntary and involuntary sphincter muscles.
Definition of Urethra
The urethra is a tube that carries urine from the bladder to the outside of the body. In males, it also transports semen during ejaculation.
Structure of Urethra
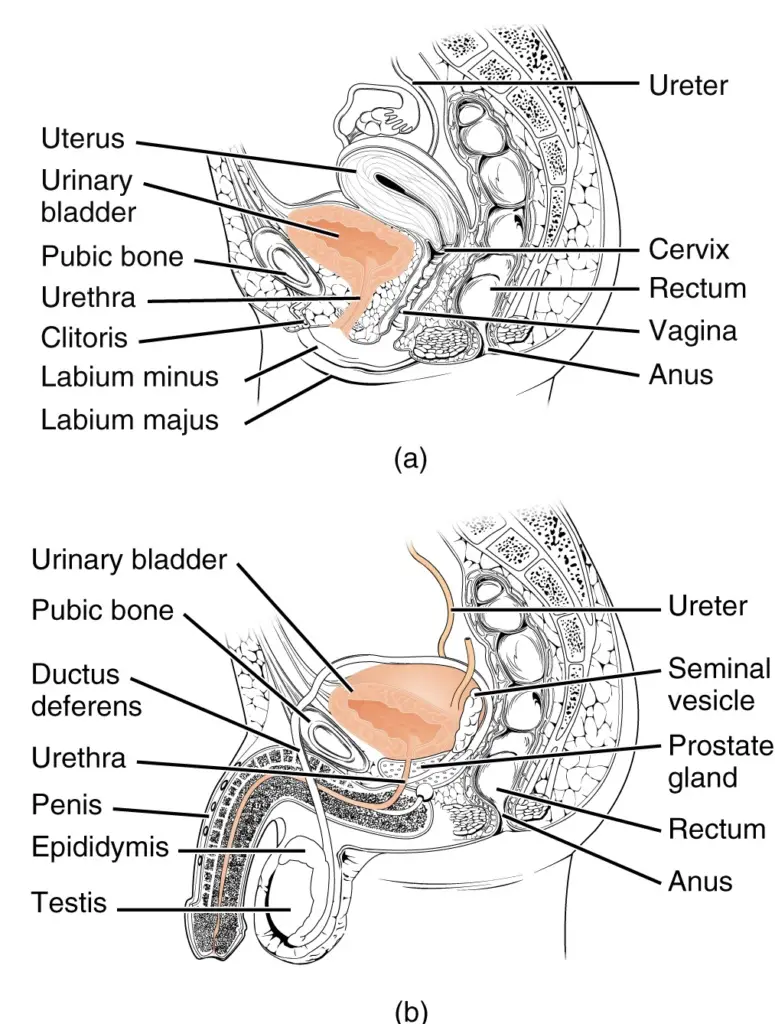
The urethra is a fibrous and muscular tube that serves as the conduit for urine from the urinary bladder to the external environment through the urethral meatus. The structure and length of the urethra differ significantly between males and females due to their anatomical and reproductive functions.
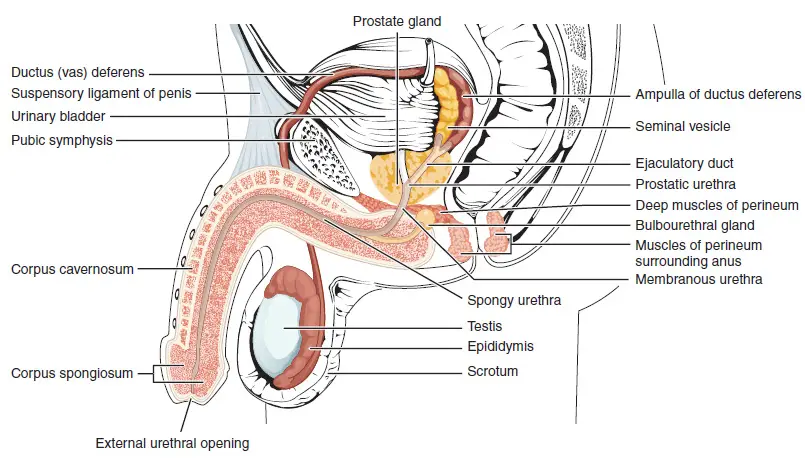
Male Urethra
In males, the urethra is approximately 18 to 20 centimeters (7.1 to 7.9 inches) long and is divided into four distinct regions, each with specific characteristics and functions:
- Pre-prostatic Urethra:
- Description: This segment is the intramural part of the urethra surrounded by the internal urethral sphincter.
- Length: Varies between 0.5 and 1.5 cm, depending on bladder fullness.
- Epithelium: Transitional epithelium.
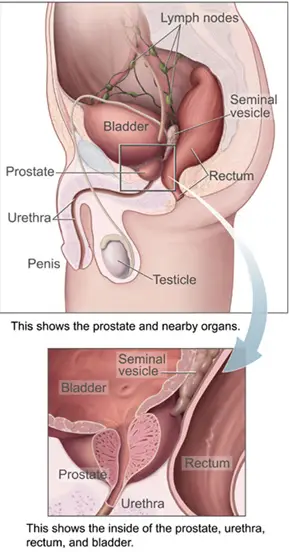
- Prostatic Urethra:
- Description: Passes through the prostate gland. Features several openings collectively known as the verumontanum, including the ejaculatory ducts and prostatic ducts.
- Functions: Transports both urine and ejaculate fluid.
- Epithelium: Transitional epithelium.
- Clinical Note: Common site of obstruction in benign prostatic hyperplasia (BPH).
- Membranous Urethra:
- Description: A short segment (1 to 2 cm) passing through the external urethral sphincter.
- Location: Deep perineal pouch.
- Features: Narrowest part of the male urethra.
- Epithelium: Pseudostratified columnar epithelium.
- Spongy (Penile) Urethra:
- Description: Extends along the length of the penis through the corpus spongiosum.
- Length: About 15 to 25 cm.
- Functions: Contains ducts from the urethral glands (glands of Littré) and the bulbourethral glands (Cowper’s glands).
- Epithelium: Pseudostratified columnar epithelium proximally, transitioning to stratified squamous epithelium distally.
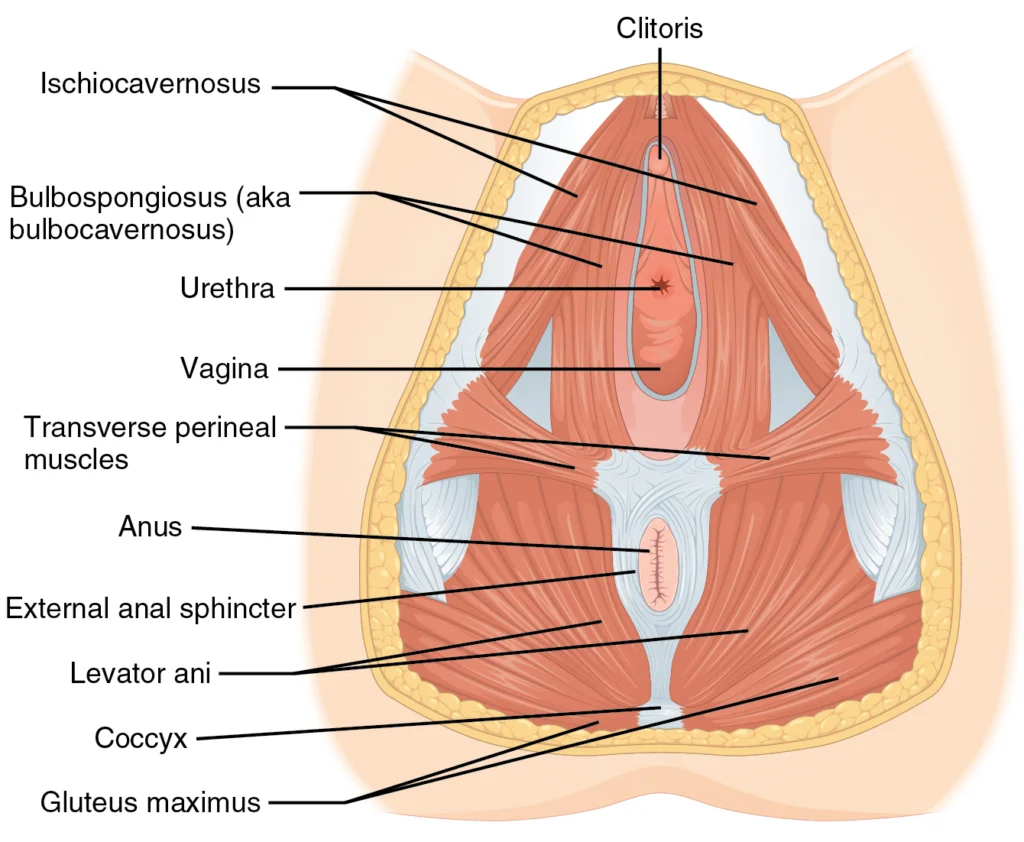
Female Urethra
In females, the urethra is much shorter, averaging around 4 centimeters (1.6 inches) in length. It is positioned between the clitoris and the vagina, extending from the internal to the external urethral orifice.
- Description: The female urethra exits the body between the clitoris and the vagina, directed obliquely downward and forward, and embedded in the anterior vaginal wall.
- Epithelium: The proximal two-thirds are lined with transitional epithelial cells, while the distal third has stratified squamous epithelial cells.
- Surrounding Structures: Encircled by the urethral sphincter situated between the superior and inferior fascia of the urogenital diaphragm.
The anatomical differences between male and female urethras account for variations in function and susceptibility to conditions such as urinary tract infections, which are more common in females due to the shorter urethral length and lack of a complex cleaning mechanism like the spiral stream of urine in males.
Microanatomy of Urethra
The urethra’s microanatomy, or microscopic structure, is essential for its functions in transporting urine and, in males, semen. Understanding the cellular composition and structural layers of the urethra provides insight into how it accomplishes these tasks.
Epithelial Lining
The epithelial lining of the urethra changes along its length, adapting to different functional requirements:
- Transitional Epithelium:
- Location: Near the urinary bladder.
- Description: Comprised of variable layers of cells that can appear flat (squamous) or cuboidal, depending on the pressure exerted by urine.
- Function: Accommodates stretching and contraction as urine flows through the urethra.
- Pseudostratified Columnar Epithelium:
- Location: Found in the middle sections of the urethra.
- Description: Appears stratified (layered) but each cell contacts the basement membrane, giving the illusion of multiple layers.
- Function: Provides a protective and supportive barrier.
- Stratified Columnar Epithelium:
- Location: Also present in the middle sections, transitioning from pseudostratified regions.
- Description: Multiple layers of column-shaped cells.
- Function: Adds durability and protection as the urethra approaches the external environment.
- Stratified Squamous Epithelium:
- Location: Near the external urethral meatus.
- Description: Multiple layers of flat cells similar to the surrounding skin.
- Function: Provides a robust barrier against mechanical stress and potential pathogens.
Glands
The urethra contains several glands that aid in lubrication:
- Urethral Glands (Glands of Littré):
- Location: Scattered throughout the urethral lining.
- Function: Secrete mucus to lubricate the urethra, facilitating the smooth passage of urine.
- Bulbourethral Glands (Cowper’s Glands):
- Location: Found in the male urethra, specifically in the spongy urethra.
- Function: Produce a pre-ejaculate fluid that lubricates the urethra before ejaculation.
Structural Layers
The urethra is composed of three main coats:
- Muscular Layer:
- Description: Continuation of the bladder’s muscular layer.
- Function: Provides peristaltic movements to aid in the expulsion of urine.
- Erectile Layer:
- Description: Contains vascular tissue, especially prominent in the male urethra.
- Function: Engorges with blood during sexual arousal, aiding in the process of ejaculation.
- Mucous Layer:
- Description: The innermost layer lining the lumen of the urethra.
- Function: Contains the epithelial cells and glands that secrete mucus, ensuring lubrication and protection.
Blood Supply, Nerve Supply, and Lymphatics
- Blood Supply:
- The urethra receives blood from branches of the internal pudendal arteries.
- Nerve Supply:
- Somatic Innervation: Provided by the pudendal nerve, which controls the external urethral sphincter, allowing voluntary control over urination.
- Lymphatic Drainage:
- Lymph from the urethra drains into the nearby lymph nodes, assisting in immune responses and fluid balance.
Development of Urethra
The development of the urethra is a complex process that occurs early in embryogenesis. This process involves the transformation of primitive structures into distinct urinary and reproductive organs, influenced by the biological sex of the developing embryo.
Early Development
- Cloaca Formation:
- Definition: The cloaca is a common cavity at the hind end of the developing embryo that serves as the precursor for the urinary, genital, and digestive tracts.
- Time Frame: Between the fourth and seventh weeks of embryonic development.
- Division of the Cloaca:
- Process: The cloaca divides into two distinct regions:
- Urogenital Sinus: Forms the basis of the urinary and reproductive systems.
- Anal Canal: Develops into the rectum and anus.
- Urorectal Septum: A wall of tissue that separates the urogenital sinus from the anal canal.
- Process: The cloaca divides into two distinct regions:
Formation of the Urogenital Sinus
The urogenital sinus further differentiates into three parts:
- Upper Part:
- Development: Becomes the largest section and forms the urinary bladder.
- Middle Part:
- Development: Forms the urethra.
- Lower Part:
- Sex Differentiation:
- Males: Develops into structures such as the prostate gland.
- Females: Forms the lower part of the urethra and paraurethral glands.
- Sex Differentiation:
Tissue Origins
- Epithelium:
- Origin: Derived from the endoderm, the innermost layer of cells in the early embryo.
- Function: Lines the interior surface of the urethra, contributing to its protective and secretory functions.
- Connective Tissue and Smooth Muscle:
- Origin: Derived from the mesoderm, the middle layer of embryonic cells.
- Function: Provides structural support and contractile properties necessary for urethral function.
Sex-Specific Development
After the third month of embryonic development, the urethra begins to form sex-specific structures:
- Male Development:
- Prostate Gland:
- Formation: The urethral epithelium multiplies to form the prostate, a gland that produces seminal fluid.
- Function: Plays a key role in the male reproductive system by contributing to the ejaculate.
- Prostate Gland:
- Female Development:
- Urethra and Paraurethral Glands:
- Formation: The upper part of the urogenital sinus develops into the urethra and paraurethral (Skene’s) glands.
- Function: The paraurethral glands are involved in lubrication and may have a role in the female reproductive system.
- Urethra and Paraurethral Glands:
Urethra Pain
Urethra pain, or urethral discomfort, is a common symptom that can arise from various conditions affecting the urinary system. Due to the extensive innervation of the urinary tract, any inflammation, infection, spasm, stenosis, or blockage can cause significant pain, which may be experienced consistently, in waves, or specifically during urination. The nature and type of pain can often help indicate its underlying cause.
Causes of Urethra Pain
- Urolithiasis (Kidney Stones):
- Definition: Urolithiasis refers to the formation of urinary stones, which are crystallized minerals that can partially or completely block the urethra.
- Mechanism: Low water intake and high salt levels promote the crystallization process, leading to the formation of stones.
- Types of Stones:
- Calcium Oxalate Stones: Formed from calcium and oxalic acid or uric acid.
- Calcium Phosphate Stones: Result from an excess of calcium and phosphoric acid.
- Uric Acid Stones: Form in acidic urine, commonly in diabetics and obese individuals.
- Struvite Stones: Caused by bacterial interactions with magnesium and phosphate.
- Cystine Stones: Occur in individuals with cystinuria, a genetic condition.
- Urinary Tract Infections (UTIs):
- Definition: UTIs are infections caused by bacteria, primarily E. coli, entering the urinary tract.
- Types:
- Upper Urinary Tract Infections: Include nephritis (kidney infection) and pyelonephritis, affecting the kidneys and ureters.
- Lower Urinary Tract Infections: Include urethritis (urethra infection) and cystitis (bladder infection).
- Symptoms:
- Upper UTIs: Fever, flank pain, nausea, vomiting, and possibly bloody or cloudy urine.
- Lower UTIs: Pain during urination (dysuria), frequent urge to urinate (pollakiuria), and cloudy or strong-smelling urine.
- Sexually Transmitted Diseases (STDs):
- Definition: Infections transmitted through sexual contact, affecting the urethra among other organs.
- Pathogens: Include viruses, bacteria, yeasts, and parasites.
- Common STDs:
- Chlamydia and Gonorrhea: Cause burning sensations and discharge from the urethra.
- Herpes Simplex Virus: Leads to painful ulcers and inflammation.
- Syphilis: Early stages can cause sores and urethral discharge.
- Urethral Syndrome:
- Definition: Characterized by symptoms of a lower UTI without detectable bacteria or pus in the urine.
- Causes: Can include undetected pathogens, anatomical abnormalities, trauma, allergies, or comorbidities.
- Symptoms: Burning sensations during urination (dysuria) and frequent urination (pollakiuria).
Diagnosis and Management
- Diagnosis:
- Medical History and Physical Examination: Key to understanding the onset, duration, and nature of pain.
- Urine Tests: To detect the presence of bacteria, blood, or crystals.
- Imaging: Ultrasound or CT scans to visualize stones or structural abnormalities.
- Cystoscopy: Direct visualization of the urethra and bladder using a scope.
- Management:
- Hydration: Increased water intake to help flush out small stones and prevent new ones.
- Antibiotics: For bacterial infections, particularly UTIs.
- Pain Relief: Analgesics or anti-inflammatory medications to manage pain.
- Surgical Intervention: In cases of large stones or structural blockages that cannot be managed conservatively.
Urethra Disorder Treatments
Treating urethra disorders involves a range of approaches depending on the underlying cause. Conditions such as lower urinary tract infections (UTIs), urethral stenosis, and urethral strictures are common issues that necessitate different therapeutic strategies. This section explores various treatments, including medication, surgical interventions, and supportive measures.
1. Antibiotic Therapy for Lower UTIs
- Indication: Lower urinary tract infections (UTIs) caused by bacterial pathogens.
- Mechanism: Antibiotics eradicate the infection by targeting specific bacteria.
- Common Antibiotics: Trimethoprim-sulfamethoxazole, nitrofurantoin, and fosfomycin.
- Administration: Typically oral, though severe cases may require intravenous antibiotics.
2. Treatment for Urethral Stenosis and Stricture
- Definition: Urethral stenosis or stricture refers to the narrowing of the urethral lumen due to swelling, scar tissue, or congenital abnormalities.
a. Urethral Dilation
- Procedure: Involves inserting gradually larger dilators into the urethra to widen the lumen.
- Purpose: To allow easier passage of urine.
- Frequency: May need to be repeated periodically to maintain patency.
b. Urethroplasty
- Definition: A surgical procedure to remove a narrowed section of the urethra or to enlarge it using tissue grafts.
- Tissue Sources: Skin, buccal mucosa (lining of the mouth).
- Outcome: Often provides a permanent solution to urethral stenosis.
c. Urethrotomy
- Procedure: Surgical incision of the urethra to release a stricture.
- Technique: Usually performed endoscopically.
- Indication: For short strictures that do not respond to dilation.
3. Stone Removal from the Urethra
a. Extracorporeal Shock Wave Lithotripsy (ESWL)
- Mechanism: Uses shock waves to break stones into smaller fragments that can pass naturally.
- Procedure: Non-invasive, involves targeting stones with sound waves.
- Duration: Typically lasts 30 to 60 minutes.
- Contraindication: Not suitable for pregnant women due to the use of X-rays.
b. Endoscopic Stone Removal
- Procedure: Involves the use of an endoscope to visually locate and remove stones.
- Tools: Laser fibers or mechanical devices may be used to fragment and extract stones.
4. Urethral Stents
- Definition: Small hollow tubes inserted into the urethra to relieve obstructions.
- Indication: Temporary measure before definitive surgery or for palliative care in patients who cannot undergo surgery.
- Function: Reduces complications from pressure buildup in the upper urinary tract.
- Duration: Can be temporary or long-term, depending on patient needs and overall treatment plan.
Urethra Functions
Urine Excretion
- Primary Function: The main function of the urethra is to transport urine from the urinary bladder to the outside of the body.
- Process: Urine, produced by the kidneys, is stored in the bladder and expelled through the urethra during urination (micturition).
- Control Mechanisms:
- Internal Urethral Sphincter: Composed of smooth muscle, this involuntary sphincter helps retain urine in the bladder until the appropriate time for release.
- External Urethral Sphincter: Made of striated muscle, this voluntary sphincter allows conscious control over urination, enabling individuals to initiate or delay the process.
2. Male Urethra Functions
In addition to urine excretion, the male urethra has specific reproductive functions due to its anatomical structure.
- Semen Transport: During ejaculation, the male urethra also serves as a passage for semen, which contains sperm and seminal fluid.
- Regions:
- Prostatic Urethra: Passes through the prostate gland, receiving seminal fluid from the ejaculatory ducts.
- Membranous Urethra: Passes through the urogenital diaphragm.
- Spongy (Penile) Urethra: Extends along the length of the penis and ends at the external urethral meatus.
3. Female Urethra Functions
The female urethra is shorter and has functions limited to the urinary system.
- Urine Passage: The sole function of the female urethra is to conduct urine from the bladder to the external environment.
- Anatomical Position: The female urethra opens into the vulval vestibule between the clitoris and the vaginal opening.
4. Protective Functions
- Mucus Secretion: Urethral glands, including the glands of Littre and, in males, the bulbourethral glands (Cowper’s glands), secrete mucus. This mucus acts as a lubricant, reducing friction and protecting the urethral lining during urination and, in males, ejaculation.
- Defense Mechanism: The urethral mucosa and its secretions provide a barrier to pathogens, helping to prevent infections from ascending into the urinary tract.
References
- https://biologydictionary.net/urethra/#urethra-pain
- https://teachmeanatomy.info/pelvis/viscera/urethra/
- https://www.news-medical.net/health/What-is-the-Urethra.aspx