What is Rickettsia?
Small-sized intracellular bacteria with a 0.3 to 2 µm range make up the genus Rickettsia. Rickettsia’s tiny scale made it first confused as a virus. Having DNA and RNA as their genetic material, these bacteria reproduce via binary fission within the cytoplasm of eukaryotic cells.
Gram-negative rickettsia bacteria abound in the digestive system of many arthropods including ticks, fleas, mites, and chiggers. Among the various illnesses they have caused in people are epidemic typhus, murine typhus, rickettsialpox, and Rocky Mountain spotted fever.
Three genera—Rickettsia, Orientia, and Candidatus Cryptoprodotis—are identified inside the Rickettsiaceae family. While Candidatus Cryptoprodotis mostly found in ticks and does not cause illnesses in people, Rickettsia and Orientia are closely linked to one another.
There are 25 recognised species in the genus Rickettsia, split further into four groups. Nonmotile, gram-negative, very pleomorphic, these bacteria can be cocci (0.1 μm in diameter), bacilli (1–4 μm long), or threads (up to around 10 μm long).
One should not mistake the term “rickettsia” with rickets, a vitamin D deficient illness. Rather, the bacterial genus Rickettsia was named for Howard Taylor Ricketts in honour of his innovative studies on tick-borne spotted fever.
Although “Rickettsia” refers to a specific genus, the informal word “rickettsia” (plural “rickettsias”) is commonly used to refer to any Rickettsiales species. Usually endothelial cells, these bacteria are obligate intracellular pathogens depending on entrance, development, and replication inside the cytoplasm of live eukaryotic host cells. Rickettsia species hence must be produced in tissue or embryo cultures rather than cultivated in synthetic nutrient medium. Following a technique devised by Ernest William Goodpasture and his associates in the 1930s, chicken embryos are frequently employed for this purpose.
Every year new strains or species of Rickettsia are identified and reported on. Many Rickettsia species are non-pathogenic to vertebrates, including humans, and only infect arthropods like aphids or whiteflies. Often in symbiotic connection with their arthropod hosts, these non-pathogenic Rickettsia bacteria Medical literature does, however, occasionally confuse them with pathogenic Rickettsia, hence underscoring the anthropocentric bias in the discipline.
Several types of arthropods, like chiggers, ticks, fleas, and lice, carry pathogenic Rickettsia species that cause diseases in both people and plants. Pathogenic Rickettsia causes typhus, rickettsialpox, boutonneuse fever, African tick-bite fever, Rocky Mountain spotted fever, Flinders Island spotted fever, and Queensland tick typhus. Fortunately, most harmful Rickettsia bacteria are sensitive to tetracycline group drugs.
Features of Rickettsia
- Gram-negative rickettsia bacteria have a different cell wall structure and are so categorized as such.
- Unlike certain bacteria, Rickettsia does not develop spores as a survival tactic.
- Rickettsia bacteria lack flagella or other features meant for movement.
- Rickettsia has pleomorphism, so it may adopt many shapes. It may show as cocci (spherical forms) with a diameter of about 0.1 µm, bacilli (rod-shaped) ranging from 1 to 4 µm in length, or thread-like structures up to 10 µm in length.
- Rickettsia’s genetic material has a circular genome ranging in size from 1 to 2.1 megabytes (Mb).
- Rickettsia bacteria proliferate via a mechanism known as binary fission. They split in two exactly identical daughter cells.
- Above its outer membrane Rickettsia has a microcapsular protein layer. This layer could help the bacterium avoid the immune system and adds to their contact with host cells.
- Rickettsia species are obligatory intracellular bacteria, hence they cannot survive in an artificial nutritional environment; they need a live host cell for growth and multiplication. An artificial nutrition media cannot support and foster their growth.
- Growing in tissue cells or chicken embryo culture, Rickettsia may be cultivated and developed in both directions. Designed in the early 1930s, this technique lets scientists examine and spread these microorganisms for experimental needs. Rickettsia is grown using chicken embryos rather often.
Transmission of Rickettsia
- Humans get Rickettsia bacteria mostly via direct contact with infected arthropod vectors during their feeding cycle. Arthropod vectors may include fleas, lice, mites, or ticks. By feeding on diseased rodents or animals, these vectors contract Rickettsia. Later on, when the infected arthropod vector feeds on a human, the germs might enter the human circulation.
- Rickettsia may also be transmitted inadvertently by someone introducing the bacterium into their body. This can happen if someone scratches their skin and spreads arthropod-borne fluids or feces to a bite wound or skin break. Likewise, inoculating Rickettsia bacteria might arise by crushing the arthropod vector at the bite site.
- Some rickettsial diseases may also be transmitted by inhaling microorganisms or inoculating the conjunctiva. Though less frequent, these channels of transmission may cause illness in some situations.
- It is important to note that certain rickettsial pathogens, including Anaplasma and Ehrlichia species, can be transmitted through organ transplantation or transfusion of infected blood products. Even though they don’t happen very often, these ways of transmission show how vital it is to screen blood banks and organ transplant processes properly.
- In general, Rickettsia transmission is facilitated by direct contact with infected arthropod vectors during their foraging process. Inhalation, itching, crushing the arthropod vector, and conjunctival injection are further ways to spread the germs. To take precautions and lower the chance of getting rickettsial illnesses, people must be aware of these ways that the disease can be spread.
Diagnosis of Rickettsia
Rickettsial illness diagnosis may be difficult and usually depends on laboratory tests, clinical awareness, and epidemiological background. These are some salient features of the diagnosis of Rickettsia infections:
- Clinical Recognition and Epidemiologic Context – Timely presumptive diagnosis is usually based on clinical observation, considering the patient’s exposure to arthropod vectors as well as the specific signs and symptoms connected with rickettsial disorders. The recognition of the clinical characteristics of these illnesses depends much on experienced doctors.
- Serologic Testing– Often used to verify rickettsial infection diagnosis is serologic testing. Using indirect immunofluorescence antibody assays (IFA), testing acute-phase and convalescent-phase serum samples for a notable rise in antibody titers—usually a fourfold or larger increase. Cross-reactivity of antigens should be noted as it results in antibodies reacting in group-targeted serologic tests, therefore suggesting group level exposure.
- PCR Assays and Immunohistochemical Analyses – Molecular diagnostic tools include polymerase chain reaction (PCR) tests and immunohistochemistry analysis may provide important data. Swabs or biopsies from eschars (if present), biopsy specimens of rash lesions, or whole blood samples are only a few of the many sample forms PCR may be used on. For species-specific diagnosis especially, eschar samples are very helpful. Still, the accuracy of these tests may be affected by the time and quality of the specimens.
- Anaplasmosis and Ehrlichiosis Diagnosis – Diagnosing probable anaplasmosis or ehrlichiosis is best done by PCR of a whole blood sample. Examining a buffy coat—a layer of white blood cells split from whole blood—can also provide presumptive evidence of infection by spotting leukocyte distinctive inclusion bodies known as intraleukocytic morulae.
- Notifiable Diseases and Commercial Laboratory Testing – In the United States, notifiable illnesses such ehrlichiosis, anaplasmosis, and spotted fever rickettsiosis are commercial laboratory tested for countrywide. Test for rickettsial illnesses including ehrlichiosis, anaplasmosis, and scrub typhus in commercial labs. Some species-targeted serologic tests, however, may only be found at the Rickettsial Zoonoses Branch of the Centres for Disease Control and Prevention.
Epidemiology of Rickettsia
- In epidemiology of Rickettsia, the study of the distribution, transmission, and patterns of infection of the bacteria of the Rickettsia genus Mostly shaped by the presence of tiny blood-sucking arthropods, Rickettsia is a collection of intracellular bacteria found worldwide in tropical, subtropical, and temperate areas.
- The main reservoir for Rickettsia typhi, the bacterium causing murine typhus, are rats. As a vector, the rat flea passes the bacterium on to mammals. Eating the blood of sick rats helps these fleas to acquire R. typhi. Murine typhus results from the infected flea spreading the germs when it bites a person or another creature later on.
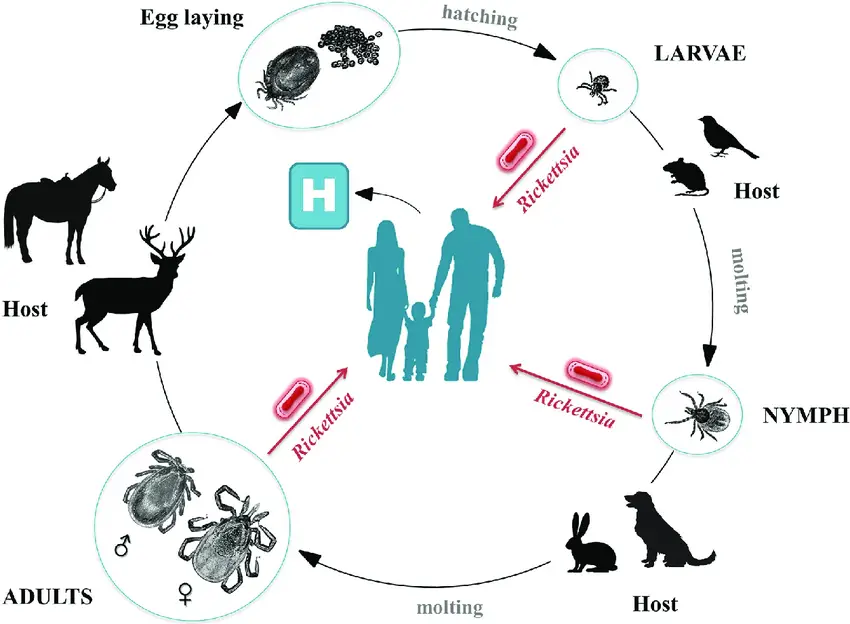
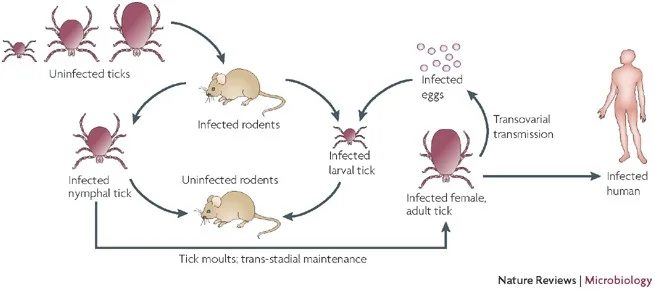
- Another crucial hematophagous arthropod vector linked to rickettsioses transmission are ticks. Through their saliva, they infect people and inject germs into the circulation, hence spreading tropical rickettsioses. Before the bacteria may be spread successfully, the transmission mechanism calls for over six hours of attachment and eating on the surface of the host.
- Two main ways that ticks spread tick-borne rickettsioses and spotted fever groups are transtadial transmission—from one stage of the tick’s life cycle to another—and transovarial transmission—transfer of bacteria from adult female ticks to their eggs. This implies that the infection may be passed from one generation to the next by ticks, therefore enabling the germs to remain in the tick population.
- Apart from direct tick bites, additional ways of transmission for the virus exist. The germs in the body may be introduced by scratching, itching, or rubbing the skin tainted with infected tick excrement. Moreover, rickettsioses might be regarded as newly occurring zoonotic illnesses related to travel abroad. Birds, Northern American flying squirrels, and their ectoparasites may carry ticks, therefore helping these bacteria to move to new areas.
- Another zoonotic cycle may be followed by typhus rickettsiae, the bacterium causing murine typhus. This implies that additional animals and arthropods may participate in the transmission, amplification, or maintenance of the bacteria in addition to the main cycle including rats and fleas.
- Human spotted fever rickettsioses usually strike more in the summer, when more people are outside and more exposure between people and ticks is evident. It is interesting to note that certain age groups are regarded as high-risk populations for particular rickettsial infections. Particularly susceptible to Rocky Mountain spotted fever are children ranging in age from five to nine years old as well as senior individuals between the ages of forty and sixty-four.
- Research using the GeoSentinel database have shown that rickettsioses impact almost 3.1% of passengers. This emphasizes the need of taking these diseases into account when assessing patients with fever problems who have recently visited areas where rickettsial infections are common.
- Global warming is thought to be causing rickettsial diseases to rise as well as the northward spread of tick species. Changing climate circumstances might provide more suitable conditions for ticks to flourish and extend their geographic range, therefore maybe exposing more people to rickettsial diseases.
- Therefore, designing efficient preventative and control plans depends on an awareness of the Rickettsia epidemiology. The dispersion and transmission of rickettsioses depend much on environmental factors, reservoir hosts, and competent vectors as well as other elements. Reducing the effect of these illnesses on human health mostly depends on constant observation, public health education, and suitable vector control strategies.
Pathogenesis of Rickettsioses
- Rickettsioses’ pathogenesis process consists on a sequence of events after the invasion of the host’s body via many channels of infection by the bacteria. The main ways of transmission include bites from infected ticks or mites, swallowing contaminated louse or flea feces via the fecal-oral route, and breathing in the organisms or their excrement in certain workplaces.
- Once inside the host, Rickettsia bacteria assault the layer of cells lining the blood arteries known as the vaseline endothelium. They penetrate the endothelial cells, proliferate in the cytoplasm, then travel the bloodstream to other areas of the body. The bacterium attack and infect smooth muscle cells as well as the vasilevelum. The host mounts an immunological reaction upon this invasion, which increases immune-effector responses.
- Rickettsia’s spread causes vascular cells to become more permeable, which causes fluid to accumulate in the interstitial surrounds. Low blood volume and insufficient tissue perfusion define hypovolemic shock, a disorder caused in part by this fluid buildup. Severe instances may cause potentially death as well as life-threatening consequences.
- Apart from the blood vessels, Rickettsia might compromise other important organs in the body. Particularly vulnerable to infection are the brain, liver, lungs, heart, and adrenal glands; disorders include meningoencephalitis (inflammation of the brain and meninges) and interstitial pneumonitis (inflammation of the lung tissue) follow from this.
- Sometimes illness results by breathing in the germs or their excrement, primarily seen among laboratory personnel with inadequate hygiene habits. This path of infection may cause respiratory problems and difficulties and raises a chance of involvement.
- Reduced fluid perfusion brought on by kidney infection may lead to acute renal failure. The kidneys’ regular operation is hampered by the lower blood flow, which also prevents their efficient waste product filtration from the blood.
- Normal gas exchange may be disrupted by plasma’s vascular leakage into the alveolar spaces of the lungs, therefore producing hypoxemia—low blood oxygen levels. This might aggravate respiratory problems and cause other difficulties.
- Controlling intracellular rickettsiae depends critically on the host’s cellular immunity. An essential method for killing the bacteria within endothelial cells is induced nitric oxide generation by these cells under control of cytokines such gamma interferon and tumour necrosis factor.
- Additionally helping the immune response against rickettsial illnesses are natural killer cells. Their immunological reactions enable the germs from compromised cells to be destroyed.
- Furthermore helping to prevent reinfection is the humoral immune response mediated by antibodies. Made against the outer membrane proteins of Rickettsia, antibodies help the bacterium to be recognized and cleared.
- Rickettsioses’ pathogenesis process is essentially the invasion of vascular endothelium, spread of the germs via the circulation, and consequent infection of several organs. With cellular and humoral immunity helping much to fight the illness, the immune response set off by the host seeks to regulate and eradicate the germs. Knowing the pathogenesis processes helps one to better understand the creation of therapeutic, preventative, and diagnostic plans against rickettsial disorders.
Signs and Symptoms of rickettsial diseases
The particular type of infection will affect the indications and symptoms of rickettsial disorders. Commonalities, meanwhile, include fever, headache, and malaise as well as a broad rash. Following are some particular symptoms and indicators linked to several forms of rickettsial diseases:
- Rocky Mountain Spotted Fever:
- Usually happening two to eight days following a tick bite, either gradual or rapid start
- Fever, headache, uncertainty, muscular pains, and digestive problems
- Starting with tiny red patches on the wrists and ankles, Rash appears around days 2–3 and can occasionally blister.
- Interestingly, about 20% of cases do not produce a rash—a condition sometimes referred to as spotless Rocky Mountain spotted fever.
- Rickettsianpox:
- Irregular fluctuating fever shorter than one week
- Runny nose, sore throat, headache, chills, muscular aches, nausea, vomiting, and stomach pain.
- At the site of the mite bite, a red elevated area forms later to become an eschar—a dry scab.
- Distributed on the face, neck, trunk, and limbs, the rash is easily confused with varicella (chickenpox).
- Boutonneuse Fever:
- Fever; headache; malaise; muscular aches
- Days 3–5 of the sickness show rashes starting from the extremities to the trunk, neck, face, palms, and soles inside 36 hours.
- The rash might last two to three weeks and is patchy and blotchy.
- About half of the cases involve the development of a tache noire, a dry scab sometimes referred to as a black spot.
- Louse-Borne Typhus:
- Start suddenly one to two weeks following a louse bite.
- Fever and persistent headache
- Usually not affecting the face, palms, or soles, rash shows up on days 4–7 of illness from the trunk to the extremities.
- Starting as splotchy, the rash changes to become elevated red dots.
- Usually, recurrence of the illness—known as Brill-Zinsser disease—is milder.
- Murine Typhus:
- Like louse-borne typhus, but often has a milder and shorter course.
- Usually, a flea bite causes an eschar to develop.
- You might have fever, headache, and other vague symptoms.
- Scrub Typhus:
- Commonly occurring is generalised lymph node edema.
- Headache and fever.
- Rash shows up as a dry scab-like sore one to three weeks following a mite attack.
- Usually limited to the trunk, the rash passes through quickly.
Complications from rickettsial diseases
While complications from rickettsial diseases are relatively uncommon when diagnosed and treated promptly, certain complications can arise in some cases. Here are some potential complications associated with rickettsial diseases:
- Bronchopneumonia: In some severe cases, rickettsial infections can lead to the development of bronchopneumonia, which is characterized by inflammation and infection of the bronchial tubes and the lungs.
- Congestive heart failure: Rickettsial infections may cause myocarditis, which is inflammation of the heart muscle. In severe cases, this inflammation can lead to congestive heart failure, a condition where the heart is unable to pump blood efficiently.
- Multi-organ failure: In rare instances of severe rickettsial infections, multi-organ failure can occur. This condition involves the failure of multiple organs, such as the heart, lungs, liver, kidneys, or other vital organs.
- Deafness: Some rickettsial infections, such as certain forms of spotted fever, may rarely result in hearing loss or deafness as a complication.
- Disseminated intravascular coagulopathy (DIC): DIC is a condition characterized by abnormal blood clotting and bleeding. In severe cases of rickettsial infections, DIC can occur as a complication.
- Myocarditis: Inflammation of the heart muscle, known as myocarditis, can lead to various cardiac complications and may be observed in some cases of rickettsial diseases.
- Endocarditis: Endocarditis refers to inflammation of the lining of the heart, typically affecting the heart valves. Although rare, rickettsial infections can lead to endocarditis as a potential complication.
- Glomerulonephritis: Certain rickettsial infections can result in glomerulonephritis, which is inflammation of the kidney’s glomeruli. This can lead to kidney dysfunction and potentially require medical intervention.
Diagnosis of Rickettsioses
A rickettsioses diagnosis calls for several laboratory techniques and testing. The following are some main features of the diagnostic process:
- The first diagnosis of rickettsioses depends much on clinical observation. Important hints for the diagnosis might come from the typical clinical symptoms—flu-like ones and the development of a rash.
- Skin biopsies of skin lesions are taken to find antigens unique to Rickettsia by means of immunohistochemical detection. This approach may assist to verify the presence of the germs in the afflicted tissues.
- Rickettsioses are diagnosed with serological assays most of which are used in confirmation. These assays find in serum samples particular antibodies against Rickettsia. Note that antibodies may not be evident in the first stage of infection; so, repeat tests might be required to catch the immune response.
- Growing Rickettsia bacteria in manmade laboratory environments can be difficult. Usually isolated in viable eukaryotic host cells—embryonated eggs, tissue cultures, antibiotic-free cell cultures, or compatible laboratory animals—they are either HeLa, Hep2, Detriot-6, mouse fibroblasts are common cell lines maintained for Rickettsia. Usually, isolation of the bacteria entails growing in developing 5 to 6 day old chick embryos. From animal specimens, Rickettsia species may be separated using laboratory animals such as mice and Guinea pigs.
- Rocky Mountain spotted fever diagnosis calls for a direct fluorescent antibody (DFA) test. This approach allows quick and targeted detection by means of fluorescently labelled antibodies that especially bind to Rickettsia antigens.
- Early rickettsial disease diagnosis makes growing use of recently created serological assays like the indirect fluorescent antibody (IFA) test and enzyme-linked immunosorbent assay (ELISA). By spotting certain antibodies in patient blood samples, these tests help to identify either current or past illnesses.
- The particular clinical presentation, the stage of illness, and the availability of laboratory resources will all affect the diagnosis tests chosen. Improving diagnostic accuracy might need both recurrent testing and combination testing employing many techniques.
Treatment of Rickettsioses
The therapy for rickettsioses is the use of suitable antibiotics meant to target the fundamental bacterial infection. The following are some crucial factors on rickettsioses’ treatment:
- Presumptive Treatment– Given the possible severity of rickettsial infections and the necessity of quick treatment, a presumption strategy is sometimes chosen. Antibiotics are therefore started without waiting for confirming laboratory testing if there is a strong clinical suspicion of rickettsial infection based on symptoms, epidemiological data, and geographical location.
- Antibiotic Choices– The main antibiotics used in treating rickettsioses include fluoroquinolones, tetracycline, doxycycline, and chloramphenicol. Out of them, doxycycline is the most often advised and successful option. Excellent effectiveness against Rickettsia bacteria makes this antibiotics broad-spectrum antibiotic. Early on following the diagnosis, suspected or confirmed, doxycycline should be taken.
- Alternative Antibiotics– In rare cases, including those of pregnant women or those with particular contraindications to doxycycline, alternative antibiotics might be taken under consideration. One such a substitute antibiotic fit for these situations is chloramphenicol. Nevertheless, chloramphenicol is linked to a greater risk of side effects and is usually regarded as less effective than doxycycline.
- Duration of Treatment– The particular kind of infection, degree of the sickness, and response to treatment determine the length of antibiotic treatment for rickettsioseses. Treatment usually lasts at least 7 to 14 days, although in severe instances or problems it might have to be maintained.
- Supportive Care – Apart from antibiotic therapy, controlling rickettsial infections depends on supportive care. This might cover relaxation, enough water, and handling of certain symptoms or consequences. Severe instances might call for hospitalisation for supportive treatments and strict monitoring.
Prevention and Control of Rickettsioses
Reducing the risk of rickettsioses mostly depends on preventive and controlling measures. These are some crucial steps to give thought:
- Personal Protection– When in places where ticks, lice, mites and fleas are common, people should dress in protective gear like long sleeves, long pants and closed shoes to reduce their chance of infection. Additionally useful in preventing bites from these sources is using insect repellent lotions or sprays on exposed skin. When applying insect repellent, it is advisable to do so per product directions.
- Tick Avoidance– Activities include bushwalking, camping, or spending time in places with plenty of foliage should be taken under careful consideration. These surroundings might have more tick and other vector populations. Steer clear of direct human interaction with plants and bushes as well as grassy and forested regions where ticks are very widespread. Examining the body for attached ticks and quickly removing them will help to greatly lower the likelihood of transmission.
- Vector Control– By means of strategies to manage the population of vectors including ticks, lice, mites, and fleas, one can aid to lower the rickettsial illness transmission. This might call for environmental management, like eradicating tick habitats or applying pesticide treatments in infected regions.
- Public Health Education– Crucially important is increasing knowledge of rickettsioses, their modes of spread, and preventative actions. Teaching people—especially those living in or visiting places where rickettsial diseases are endemic—can assist to encourage personal hygiene habits and lower their risk of exposure.
- Occupational Safety- Those working in areas with a lot of vectors or those in increased danger of exposure, including laboratory personnel handling Rickettsia bacteria, should follow suitable safety procedures. This covers following correct handling and disposal techniques, maintaining appropriate hygienic practices, and wearing personal protective tools.
- Vaccination – Rickettsial infections cannot be prevented with any vaccination at present. Prevention so mostly depends on avoiding direct interaction with the vectors and applying personal preventive actions.
- Surveillance and Early Detection – Active surveillance systems can track disease patterns and aid to pinpoint locations more likely to have rickettsial infections. Early case discovery enables quick treatment and control measure application.
FAQ
What is Rickettsia infection?
Rickettsia infection refers to an infection caused by bacteria belonging to the genus Rickettsia. These bacteria are primarily transmitted to humans through arthropod vectors, such as ticks, fleas, lice, and mites.
How is Rickettsia infection diagnosed?
Diagnosis of Rickettsia infection typically involves a combination of clinical recognition, epidemiological context, and laboratory testing. Serological tests, PCR assays, and immunohistochemical analyses are commonly used to confirm the presence of the bacteria.
What is the treatment for Rickettsia infection?
The primary treatment for Rickettsia infection involves the administration of antibiotics, such as doxycycline, tetracycline, chloramphenicol, or fluoroquinolones. Prompt initiation of antibiotic therapy is important to prevent complications and improve outcomes.
Can Rickettsia infection be prevented?
Yes, Rickettsia infection can be prevented. Measures such as using protective clothing, applying insect repellents, and avoiding direct contact with vectors (ticks, fleas, lice, and mites) can reduce the risk of transmission. Additionally, environmental control measures and public health education play a role in prevention.
Are there vaccines available for Rickettsia infection?
Currently, there are no vaccines available for Rickettsia infection. Prevention mainly relies on avoiding contact with infected vectors and implementing personal protective measures.
What are the common symptoms of Rickettsia infection?
Common symptoms of Rickettsia infection include fever, headache, malaise (general feeling of unwellness), and a widespread rash. The specific symptoms may vary depending on the type of Rickettsia species involved.
How are Rickettsia infections transmitted?
Rickettsia infections are primarily transmitted through the bite of infected arthropod vectors. This can occur during the feeding process when the vectors, such as ticks or fleas, transmit the bacteria to humans. Transmission can also occur when infectious fluids or feces from the vectors contaminate the skin through scratching or crushing of the vector.
Are Rickettsia infections contagious from person to person?
No, Rickettsia infections are not considered contagious from person to person. The primary mode of transmission is through arthropod vectors, and human-to-human transmission is rare.
Can pets transmit Rickettsia infections?
Pets, such as dogs and cats, can become infected with certain Rickettsia species, but their role in transmitting the bacteria to humans is generally minimal. However, it is still important to protect pets from arthropod vectors to prevent their own infections.
Are Rickettsia infections common worldwide?
Rickettsia infections are found globally, but their prevalence varies depending on geographical factors, climate, and the presence of suitable arthropod vectors. Different species of Rickettsia may be more common in specific regions, leading to variations in the incidence of infection.
References
- Snowden J, Ladd M, King KC. Rickettsial Infection. [Updated 2023 Jan 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431127
- https://www.merckmanuals.com/home/infections/rickettsial-and-related-infections/overview-of-rickettsial-infections
- https://wwwnc.cdc.gov/travel/yellowbook/2024/infections-diseases/rickettsial-diseases
- https://reference.medscape.com/article/968385-overview
- https://bestpractice.bmj.com/topics/en-gb/1604
- https://tripprep.com/library/rickettsial-infections/traveler-summary
- https://www.sahealth.sa.gov.au/wps/wcm/connect/public+content/sa+health+internet/conditions/infectious+diseases/rickettsial+infections/rickettsial+infections+-+including+symptoms+treatment+and+prevention