What is Placenta?
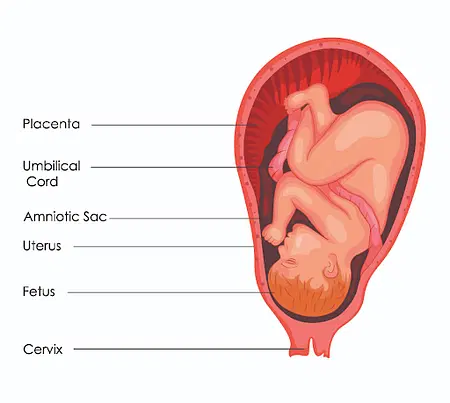
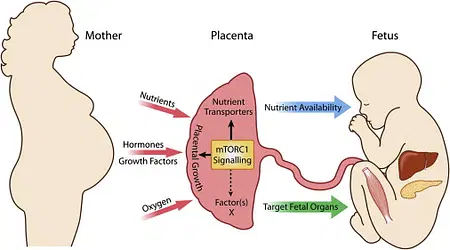
- The placenta is a vital organ that develops in the uterus during pregnancy. It plays a crucial role in supporting the growth and development of the baby. This remarkable structure not only provides oxygen and essential nutrients to the growing fetus but also helps eliminate waste products from the baby’s bloodstream.
- The placenta forms a connection with the uterine wall and gives rise to the baby’s umbilical cord, which serves as a lifeline between the mother and the developing child. In addition to its role in facilitating the exchange of oxygen and nutrients, the placenta also produces various hormones that are important for pregnancy, such as lactogen, estrogen, and progesterone.
- While the placenta is primarily associated with placental mammals, it is also found in marsupials and certain non-mammals at different stages of development. The term “placenta” originates from the Greek word “placentation,” which means “flat cake.” This name is fitting because the human placenta is a round, flat mass that resembles a pancake.
- Broadly speaking, the term “placenta” refers to any region in a viviparous organism where maternal and embryonic tissues closely interact and facilitate the exchange of physiological substances between the parent and the embryo. It acts as a temporary organ throughout pregnancy, assuming the functions of the baby’s lungs, intestines, kidneys, and endocrine glands.
- One of the remarkable features of the placenta is its ability to enable the transfer of substances between the maternal and fetal bloodstreams. This allows the baby to receive the necessary nutrients and oxygen from the mother while eliminating waste products. The placenta acts as a guardian, feeding, and protecting the developing fetus throughout the entirety of pregnancy.
- After childbirth, the placenta is expelled from the mother’s body through the vagina, earning it the name “afterbirth.” It is a transient circulatory organ unique to mammals, and it forms a vital connection between the fetus and the mother’s uterus during pregnancy. This connection is facilitated by the umbilical cord, which links the fetus to the placenta and allows for the transfer of materials.
- In most cases, the placenta is attached to different regions of the uterus, including the top, bottom, side, front, or back. However, in severe situations, a condition called placenta previa may occur, where the placenta becomes attached to the lower part of the uterus. Placenta previa can pose significant risks and complications during pregnancy.
- Overall, the placenta is a fascinating organ that plays a crucial role in supporting the development of a baby during pregnancy. Its temporary nature, ability to facilitate nutrient exchange, and connection to the mother’s uterus make it a vital component of the reproductive process in mammals.
Definition of Placenta
The placenta is a temporary organ that develops during pregnancy and connects the developing baby to the mother’s uterus. It provides oxygen, nutrients, and eliminates waste products from the baby’s blood.
Types of Placenta
There are several types of placenta, characterized by different factors and arrangements. Here are the different types of placenta based on various criteria:
A. Based on the Involvement of Embryonic Tissue
- Yolk-Sac Placenta: The yolk-sac placenta forms when the extraembryonic somatopleure and the midgut extension of the splanchnopleure, enclosing the yolk, come into contact with the uterine wall. This type is observed in animals like Mustelus.
- Chorio-Allantok Placenta: In this type, the extraembryonic somatopleure fuses with the allantoic evagination of the hindgut to establish contact with the uterine tissue. Examples include Eutherian animals and the Chalcides lizard.
B. Based on the Distribution of Villi
- Diffused Placenta: In this type, numerous villi are evenly dispersed throughout the entire chorion. Examples can be found in ungulates and cetaceans.
- Cotyledonary Placenta: Here, the villi cluster together in specific areas, forming small tufts. Ruminants, such as cows and sheep, have this type of placenta.
- Zonary Placenta: The villi in this type are restricted to an annular zone on the chorion. This type is observed in carnivores like Pinnipedia (seals, sea lions).
- Discoidal Placenta: Villi are limited to a discoidal area on the chorion. This type can be seen in primates (including humans), apes, and some insectivores.
C. Based on the Relationship of Villi with the Uterine Wall
- Deciduate Placenta: In this type, the mucous membrane of the uterine wall develops an intimate connection with the villi and is expelled with the embryo at birth.
- Indeciduate or Adeciduate Placenta: The uterine walls, weakly connected to the villi, detach from the uterus during birth.
D. Based on the Degree of Involvement of Fetal and Maternal Tissues
- Epitheliochorial Placenta: The uterine epithelium and the embryo’s chorion remain in simple apposition. This type is observed in animals like horses and pigs.
- Syndesmochorial Placenta: The uterine epithelium disappears, and the chorion makes direct contact with either the glandular epithelium or the endometrium. This type can be seen in sheep.
- Vasochorial or Endotheliochorial Placenta: The endometrium and glandular epithelium vanish, and the chorion directly contacts the uterine capillary endothelium. Dogs and cats have this type of placenta.
- Haemochorial Placenta: In this type, the endometrium, glandular epithelium, and endothelium of the capillaries disappear, and the chorion is bathed in maternal blood. Humans have this type of placenta.
- Haemoendothelial Placenta: Similar to the haemochorial placenta, the glandular epithelium, endometrium, and endothelium of the maternal blood capillaries vanish. The fetal endothelium separates the maternal and fetal circulating bloodstreams. This type is observed in many mice species.
These different types of placenta illustrate the variety of adaptations in placental structure and function across different species.
Structure of Placenta
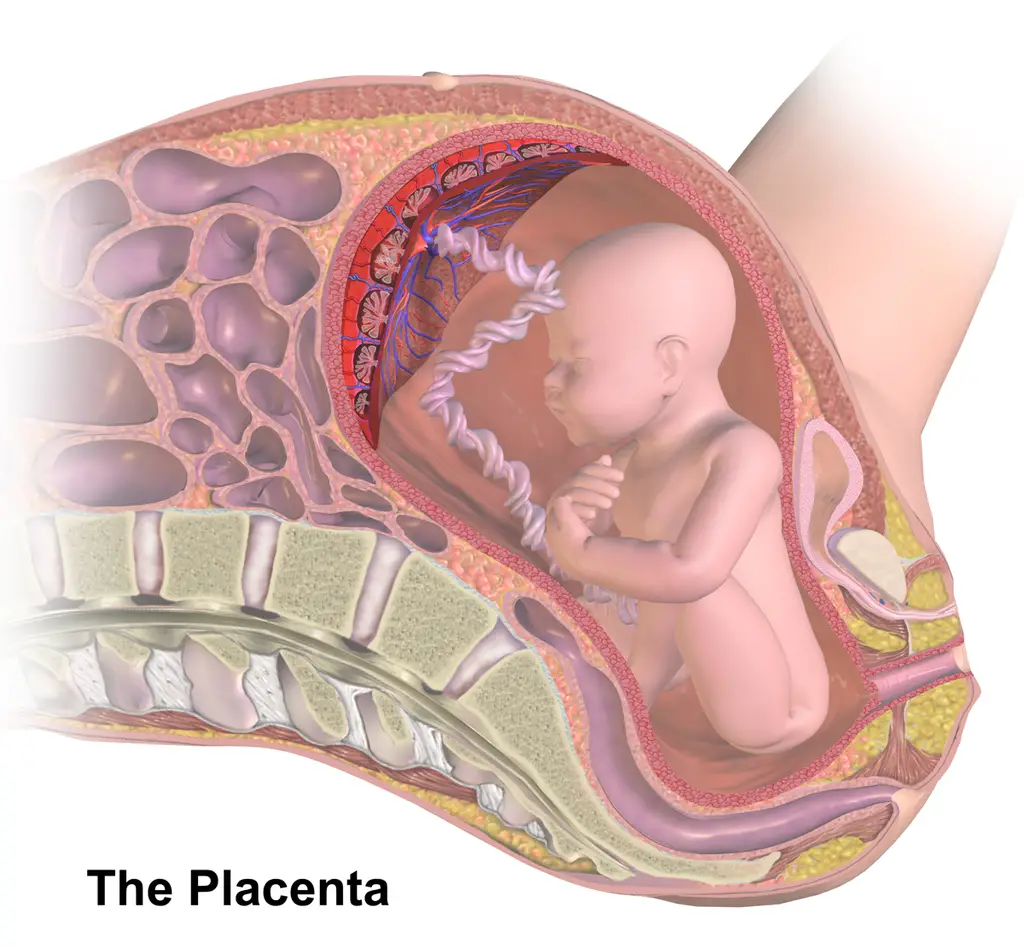
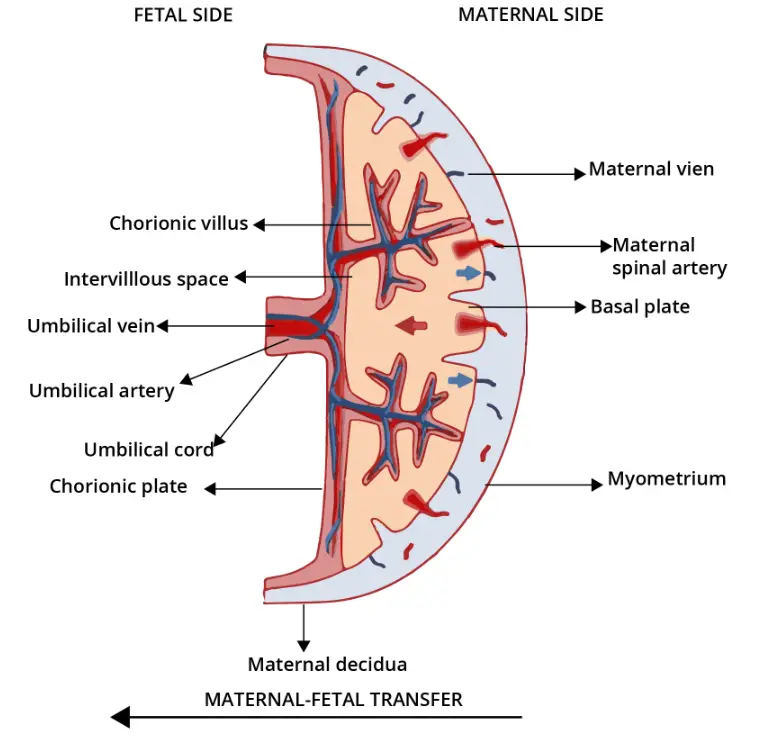
- The placenta is composed of both maternal and embryonic tissues. The embryonic component is called the chorion and is made up of trophoblasts, which form the outer cell layer of the blastocyst. The placenta itself is fetal tissue that is embedded in the uterine wall and receives maternal blood supply through the uterine spiral arteries.
- The placenta has three layers: the innermost layer is called the amnion, which surrounds the fetus; the middle layer is the allantois, derived from the embryonic hindgut, and it contains blood vessels from the umbilicus; the outermost layer is the chorion, which contacts the endometrium and consists of inner cytotrophoblast and outer syncytiotrophoblast cells.
- The placenta forms a firm connection between the fetus and the mother. Chorionic villi, which are finger-like projections, grow from the outer surface of the chorion into the uterine tissue. These villi penetrate the maternal uterine wall and form the placenta. Through the placenta, the developing embryo receives nutrients and oxygen from the mother, while releasing carbon dioxide and nitrogenous waste.
- The placenta allows for close proximity between maternal and fetal blood, enabling the exchange of materials. Nutrients, water, mineral salts, vitamins, hormones, antibodies, and oxygen pass from the maternal blood into the fetal blood, while fetal metabolic wastes like carbon dioxide, urea, and heat pass into the maternal blood. The placenta serves as the nutritive, respiratory, and excretory organ for the fetus.
- It’s important to note that the blood of the mother and fetus do not mix within the placenta or elsewhere. They are separated by a membrane through which substances must diffuse or be actively transported. In humans, the placenta is described as deciduate (with intimate contact between fetal and maternal tissue), discoidal (villi in the form of a disc), and haemochorial (chorionic epithelium in direct contact with maternal blood).
Development of Placenta
The development of the placenta can be understood as follows:
- Implantation: The process of placental development begins with the implantation of the blastocyst, a structure formed from the fertilized egg, into the maternal endometrium (the lining of the uterus). This usually occurs around week 4 of pregnancy.
- Formation of Trophoblast: The outer layer of the blastocyst develops into the trophoblast, which will later become the outer layer of the placenta. The trophoblast is further divided into two layers: the cytotrophoblast, which is the underlying layer, and the syncytiotrophoblast, which is the outer layer.
- Syncytiotrophoblast Formation: The syncytiotrophoblast is a continuous layer of cells with multiple nuclei that covers the surface of the placenta. It forms through the differentiation and fusion of the underlying cytotrophoblast cells. This process continues throughout placental development, and the syncytiotrophoblast plays a crucial role in the placental barrier function.
- Formation of Chorionic Villi: Around 12 weeks of pregnancy, the chorionic villi, finger-like projections that grow from the outer layer of the chorion (part of the trophoblast), begin to interdigitate with the tissue of the mother’s uterus. This interlocking structure helps establish the placenta as a structural and functional unit between the developing embryo (or fetus) and the maternal body.
- Maternal Blood Supply: By the end of the first trimester, around week 14, the development of the maternal blood supply to the placenta is complete. Maternal blood enters the placenta through the uterine spiral arteries and comes into close contact with the fetal blood within the placental villi, allowing for the exchange of nutrients, gases, and waste products.
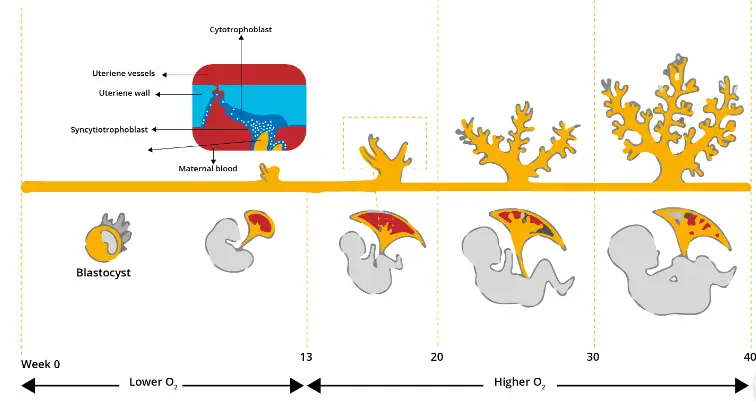
Overall, the development of the placenta involves the transformation of the blastocyst into the trophoblast, the formation of the syncytiotrophoblast layer, and the establishment of the chorionic villi that interlock with the maternal tissue. This process ensures the proper connection and exchange between the developing embryo or fetus and the maternal body, providing essential nutrients and oxygen while facilitating the removal of waste products.
Anatomical Variations
The placenta, although typically forming in a regular manner, can exhibit anatomical variations that may have implications for pregnancy. Here are some common anatomical variations of the placenta:
- Bilobed Placenta: Also known as “placenta duplex,” this condition involves the placenta forming two roughly equal-sized lobes. The umbilical cord may attach to either lobe, pass through both, or be located between them. While this variation does not increase the risk of harm to the fetus, it can result in complications such as first-trimester bleeding, excessive amniotic fluid, placental abruption, or retained placenta.
- Succenturiate Placenta: In this variation, an additional lobe of placenta forms separately from the main body and remains connected to the fetus through the umbilical cord. It is more commonly observed in older mothers or those who have undergone in vitro fertilization. This condition may lead to complications such as retained placenta and placenta previa.
- Circumvallate Placenta: In circumvallate placenta, the membranes of the placenta fold back around its edges, forming a ring-like structure. This can cause the outer membrane (chorion) to create a hematoma and result in various complications such as vaginal bleeding, membrane rupture, preterm delivery, incomplete placental development, and placental abruption. Diagnosis of this condition during pregnancy can be challenging.
- Circummarginate Placenta: This is a less problematic variant of circumvallate placenta where the placental membranes do not curl back.
- Placenta Membranacea: This rare condition is characterized by chorionic villi covering either a portion or the entire fetal membrane, causing the placenta to develop as a thinner structure at the periphery of the chorion. Placenta membranacea can lead to vaginal bleeding in the second or third trimester and may increase the risk of placenta previa or accreta.
- Ring-Shaped Placenta: A variation of placenta membranacea, this condition results in the placenta having a ring-like or horseshoe-like shape. It is a very rare occurrence and can lead to bleeding before or after delivery, as well as restricted fetal growth.
- Placenta Fenestrata: In this condition, the central portion of the placenta is absent. Placenta fenestrata is also rare, and the main concern for healthcare providers is the potential for retained placenta during delivery.
- Battledore Placenta: Also known as “marginal cord insertion,” this condition involves the umbilical cord inserting into the margin of the placenta rather than the center. It occurs in 7% to 9% of single pregnancies and is more common in twin pregnancies. Battledore placenta can lead to preterm labor, fetal complications, and low birth weight.
It’s important for healthcare professionals to be aware of these anatomical variations and closely monitor any associated risks or complications to ensure the well-being of both the mother and the fetus during pregnancy.
Parturition (Birth)
- Parturition, also known as birth, is the process of delivering the baby after the gestation period. In humans, the gestation period is approximately 280 days. Parturition is initiated by a series of involuntary contractions of the uterus known as “labour pains.” These contractions are triggered by signals from the fully developed fetus and the placenta, leading to mild uterine contractions called the fetal ejection reflex.
- Parturition is a complex neuroendocrine process. When it is time for the baby to be born, the pituitary gland secretes adrenocorticotrophic hormone (ACTH), which stimulates the adrenal glands to produce steroids. These steroid hormones stimulate the placenta to produce prostaglandins. Additionally, the hormone oxytocin is secreted from the pituitary gland. The combined action of prostaglandins and oxytocin causes the uterus to undergo powerful muscular contractions that progressively become stronger over a period of 2 to 18 hours.
- During this time, the cervix dilates fully, and the amniotic sac ruptures. The baby is then expelled out of the uterus through the birth canal. Following the birth of the baby, the placenta is also expelled from the uterus. In some cases, labour pains can be induced artificially by administering oxytocin injections or inserting prostaglandins into the vagina.
- If a woman is unable to undergo labour or if there are complications that could endanger the mother or baby, a surgical procedure called a caesarean section can be performed to deliver the baby. This involves making an incision in the abdomen and uterus to safely remove the baby.
- Parturition is a natural process that allows the safe delivery of the baby, and it is crucial for the continuation of the human species. Medical interventions, such as induction or caesarean section, are used when necessary to ensure the well-being of both the mother and the baby.
Lactation
- Lactation refers to the production and release of milk, which occurs after parturition (birth). It is stimulated by the hormone prolactin, which is produced by the anterior pituitary gland. However, high levels of estrogen can inhibit the action of prolactin on the mammary glands.
- After giving birth, the mother initially produces a thick, yellowish fluid called colostrum for about 2-3 days. Colostrum is rich in proteins and contains a high concentration of maternal antibodies. It plays a crucial role in strengthening the baby’s immune system, providing important passive immunity. Additionally, colostrum acts as a natural laxative, aiding in the removal of meconium, which is the waste material accumulated in the baby’s intestine.
- When the newborn baby suckles at the mother’s breast, it stimulates the release of both prolactin and oxytocin from the pituitary gland. Prolactin is responsible for milk production, while oxytocin triggers the release of milk from the mammary glands, a process known as let-down or milk ejection.
- Breastfeeding is highly recommended during the period of infant growth as it provides essential nutrients and antibodies for the baby’s optimal development. It not only fulfills the baby’s nutritional needs but also promotes bonding between the mother and child and offers numerous health benefits for both the baby and the mother.
- Lactation is a natural process that ensures the nourishment and well-being of the infant. It is important for mothers to receive proper support and education on breastfeeding techniques to establish successful breastfeeding and provide their babies with the best start in life.
Placenta Associated Conditions
The placenta can be associated with various medical conditions that can pose risks and complications during pregnancy. Here are some notable placenta-associated conditions:
- Placenta Previa: This condition occurs when the placenta partially or completely covers the lower part of the uterus, including the cervix. It can increase the risk of bleeding during pregnancy and may require a cesarean delivery, especially in cases of complete previa where the cervix is completely covered by the placenta.
- Placenta Accreta: Placenta accreta is characterized by the abnormal attachment of the placenta to the uterine wall, without proper penetration into the uterine muscle. It can lead to difficulties during the third trimester and delivery. Placenta accreta is rare but more likely to occur in women who smoke, have advanced maternal age, or a history of previous uterine surgeries or cesarean deliveries. It can be associated with placenta previa and may result in complications such as hemorrhage and shock during delivery.
- Placenta Increta: Placenta increta is a subtype of placenta accreta in which the placenta penetrates into the myometrium, the muscle layer of the uterus. This can lead to severe hemorrhage during childbirth and typically requires cesarean delivery along with hysterectomy or similar treatments.
- Placenta Percreta: Another type of placenta accreta, placenta percreta occurs when the placenta penetrates through the uterine wall and can even invade surrounding organs such as the bladder or colon. It is associated with a higher risk of complications and may necessitate cesarean delivery and/or hysterectomy.
- Placental Insufficiency: Placental insufficiency refers to the inability of the placenta to adequately provide nourishment and oxygen to the fetus. It can result from various factors such as genetic defects, deficiencies in essential vitamins, chronic infections, high blood pressure, diabetes, anemia, heart disease, and other health conditions. Treatment options for placental insufficiency may include dietary adjustments, medication (such as low-dose aspirin, heparin, or sildenafil citrate), or close monitoring of the pregnancy.
These placenta-associated conditions require careful management and monitoring by healthcare professionals to ensure the well-being of both the mother and the fetus.
Tests
During pregnancy, various tests are conducted to monitor the health and development of the fetus, including specific diagnostic techniques for assessing the placenta. Here are some commonly used tests:
- Ultrasound: Ultrasound is a frequently used diagnostic tool to monitor fetal development and assess the condition of the placenta. It utilizes high-frequency sound waves to create real-time images of the uterus and surrounding structures. Ultrasound can help detect placenta previa and other placental disorders. Additionally, ultrasound findings can be used to determine the maturity of the placenta through a grading system ranging from grade 0 to grade III, which can indicate potential issues like placental insufficiency.
- Chorionic Villus Sampling (CVS): CVS is a genetic testing procedure that involves taking a small sample of the placenta for analysis. It is typically performed between weeks 10 and 13 of pregnancy. The sample is obtained using a specialized catheter guided by ultrasound either through the vagina and cervix or through the abdominal muscles. The collected tissue is then sent to a laboratory for genetic testing, with results available within a week to ten days. CVS helps identify chromosomal abnormalities and genetic disorders in the fetus.
- Magnetic Resonance Imaging (MRI): MRI employs powerful magnetic and radio waves to create detailed images of the fetus and placenta. While not commonly used as a routine test during pregnancy, MRI can be helpful in diagnosing conditions like placenta increta and percreta, where the placenta penetrates the uterine wall. It can also be used in cases of suspected placental insufficiency to assess blood flow and placental function.
These diagnostic tests, including ultrasound, CVS, and MRI, provide valuable information for healthcare providers to monitor the development and well-being of both the fetus and the placenta during pregnancy. The results of these tests aid in making informed decisions regarding appropriate medical care and interventions, if necessary.
Functions of Placenta
The placenta performs several crucial functions during pregnancy:
- Nutrition: The placenta allows for the transfer of nutrients from the mother’s blood to the fetal blood. It facilitates the passage of food materials necessary for the fetus’s growth and development.
- Digestion: Specialized cells in the placenta, called trophoblasts, help digest proteins before they are transported to the fetal blood.
- Respiratory Function: The placenta acts as a respiratory organ for the developing fetus. Since the fetal lungs are not functional, the exchange of oxygen and carbon dioxide takes place through the placenta. Oxygen from the maternal blood diffuses into the fetal blood, while carbon dioxide from the fetal blood diffuses into the maternal blood.
- Excretory Function: Metabolic waste products, such as urea, uric acid, and creatinine, are excreted from the fetal blood to the maternal blood through the placenta. This is necessary because the fetal kidneys are not fully developed and cannot perform the excretory function on their own.
- Storage: The placenta can store glycogen and fat, providing a reserve of energy for the fetus before its liver is fully developed.
- Barrier: The placenta acts as a protective barrier, allowing beneficial substances to pass from the maternal blood to the fetal blood while preventing harmful substances from crossing over. However, certain substances like nicotine, addictive drugs, viruses, and bacteria can cross the placental barrier and pose risks to the developing fetus.
- Protective Function: The placenta acts as a barrier, preventing the transmission of certain bacteria and viruses from the mother to the fetus. It helps protect the developing fetus from potential infections, even if the mother is infected.
- Endocrine Function: The placenta functions as an endocrine gland, secreting various hormones to support pregnancy. These hormones include human chorionic gonadotropin (hCG), estrogen, progesterone, and human chorionic somatomammotropin. hCG is important for maintaining the function of the corpus luteum until the placenta can produce sufficient estrogen and progesterone to support pregnancy. The placenta gradually takes over the production of these hormones during the first trimester.
Overall, the placenta ensures the necessary exchange of nutrients, oxygen, and waste products between the mother and the fetus. It also provides a protective barrier and produces hormones essential for a healthy pregnancy.
Purpose of the Placenta
The purpose of the placenta can be summarized as follows:
- Nutrition: The placenta serves as a conduit for transferring food materials from the mother’s blood to the fetal blood, ensuring that the growing baby receives the necessary nutrients for development.
- Storage: The placenta acts as a temporary storage site for glycogen, fat, and other nutrients. It provides reserves for the fetus before its liver is fully developed and able to perform these functions.
- Endocrine Function: The placenta functions as an endocrine gland, producing and secreting hormones such as estrogen, progesterone, and human chorionic gonadotropin (HCG). These hormones play crucial roles in maintaining pregnancy, supporting fetal growth, and regulating maternal physiological changes during pregnancy.
- Protein Digestion: Trophoblast cells in the placenta help break down proteins before delivering them to the fetal circulation, ensuring that the fetus receives the necessary amino acids for its development.
- Excretion: Nitrogenous waste products, such as urea, are transported from the fetal blood to the maternal blood through the placenta. These waste products are then filtered out by the mother’s kidneys, helping to maintain the fetal environment.
- Respiration: The placenta facilitates the exchange of gases between the mother and the fetus. Oxygen passes from the maternal blood to the fetal blood, providing the fetus with the necessary oxygen for cellular respiration. At the same time, carbon dioxide, a waste product, moves from the fetal blood to the maternal blood for elimination.
- Barrier Function: The placenta acts as a protective barrier, allowing essential substances to pass from the maternal blood to the fetal blood while preventing the transfer of harmful substances. However, certain substances like nicotine from cigarettes, addictive drugs, viruses, and bacteria can cross the placental barrier, highlighting the importance of avoiding harmful substances during pregnancy.
In summary, the placenta plays a vital role in supporting the developing fetus by providing nutrition, hormone production, waste elimination, gas exchange, and acting as a protective barrier. It is a temporary organ that functions to sustain and protect the growing baby throughout pregnancy.
FAQ
What is the placenta?
The placenta is an organ that develops during pregnancy and is attached to the uterine wall. It provides nourishment, oxygen, and waste elimination for the developing fetus.
What is the function of the placenta?
The placenta serves several functions, including supplying nutrients and oxygen to the fetus, removing waste products, producing hormones to support pregnancy, and acting as a barrier against certain infections.
How is the placenta formed?
The placenta is formed from the fertilized egg, with cells from both the mother and the developing embryo contributing to its development. It starts to form shortly after implantation in the uterus.
When does the placenta develop?
The placenta begins to develop soon after conception, and by the end of the first trimester (around 12 weeks), it is fully formed and functioning.
Can problems occur with the placenta?
Yes, there can be various placental abnormalities or conditions that can affect pregnancy outcomes. These include placenta previa, placental abruption, placenta accreta, and placental insufficiency, among others.
What is placenta previa?
Placenta previa is a condition in which the placenta partially or completely covers the cervix, leading to potential complications during childbirth. It may require a cesarean delivery.
What is placental abruption?
Placental abruption occurs when the placenta separates from the uterine wall before delivery. It can cause vaginal bleeding, abdominal pain, and can be a medical emergency requiring immediate attention.
What is placenta accreta?
Placenta accreta is a condition in which the placenta attaches too deeply into the uterine wall, potentially causing difficulties during delivery and an increased risk of bleeding.
How is the health of the placenta assessed?
The health of the placenta is often assessed through ultrasound examinations, which can evaluate its position, thickness, blood flow, and signs of any abnormalities.
What happens to the placenta after delivery?
After childbirth, the placenta is delivered during the third stage of labor. It is typically examined to ensure it is intact and that no fragments remain in the uterus, which could cause complications.