- The family Papovaviridae include papovaviruses, a group of viruses with tiny, enclosed, icosahedral capsids containing double-stranded, circular DNA.
- The term papova is derived from the initial two letters of the virus names (pa, papillomaviruses; po, polyomaviruses; and va, vacuolating agents).
- There are two genera within the family: Papillomavirus and Polyomavirus.
- Currently, the genus Papillomavirus has been divided into a new family called Papovaviridae, while the genus Polyomavirus has been separated into a new family called Polyomaviridae.
- The papovaviruses encode growth-promoting proteins.
- They both cause lytic infections and malignancies (benign or malignant).
- Depending on the infected host cells, these viruses are capable of generating lytic, chronic, latent, or transformative infections.
Human Papillomaviruses
- The Papillomaviridae family originated as a subfamily of the Papovaviridae family.
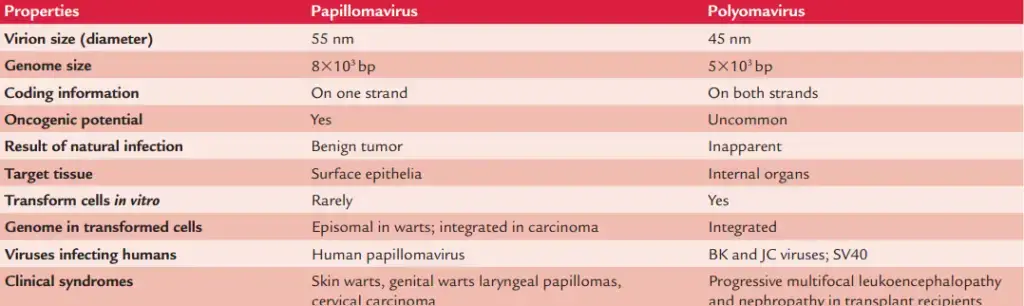
- The papillomaviruses are slightly larger in diameter (55 nm) and contain a larger genome than polyomaviruses (45 nm) (8 kbp versus 5 kbp).
- Papilloma viruses are DNA viruses that infect the squamous epithelia and mucous membranes of vertebrates, including humans.
- In their host species, all papillomaviruses generate hyperplastic epithelial lesions.
- There are currently about seventy recognised varieties of human papillomaviruses (HPVs).
- The HPVs have a high degree of tissue and cell specificity, infecting only the epithelia on the surface of the skin and mucous membranes.
- There is a link between the type of virus and the resulting lesion.
- Human papillomaviruses (HPVs) are the causal agents of papillomas, which are benign skin lesions composed of squamous cells.
- These are also linked to carcinogenic illnesses in humans, including cervical cancer.
Classification
On the basis of DNA homology, tissue tropism, and relationship with oncogenesis, the HPVs have been categorised into 16 groups (A–P), encompassing at least 70 kinds, containing a total of at least 100 types.
Human infections caused by papovaviruses
Papillomavirus
- Skin warts.
- Tumors of the head and neck that are benign.
- Anogenital verrucae.
- Cancerous circumstances (oral premalignant lesions and oral squamous cell carcinoma, intraepithelial cervical neoplasia and cancer) Respiratory papillomatosis recurrence
Polyomavirus
- BK virus: Renal diseases (hemorrhagic cystitis and urethral stenosis).
- JC virus: Progressive multifocal leukoencephalopathy caused by the JC virus.
Morphology of Human papillomaviruses
Human papillomaviruses have the following characteristics:
- They are DNA viruses with a double strand and no envelope.
- The viruses are slightly larger than polyomaviruses and range in diameter from 50 to 55 nm.
- They possess an icosahedral capsid with 72 capsomeres.
- The genome of a virus consists of around 3000 base pairs of supercoiled, double-stranded DNA (bp). Seven to eight early genes (E1–E8) and two late genes (L1 and L2) are encoded by the DNA. All of these genes exist on a single strand, denoted by the symbol. E6 and E7 are early genes associated with carcinogenesis, whereas E1 and E2 are involved in DNA replication.
Viral replication of Human papillomaviruses
- Papillomaviruses exhibit tropism towards skin and mucous membrane epithelial cells.
- During their reproduction in epithelial cells, viruses are dependent on specific components present in successively differentiated epithelial cell states.
- Virus early genes are responsible for cell growth and promote viral genome replication during cell division.
- The virus-induced cell proliferation promotes a thickening of the stratum spinosum’s basal and prickle cell layers.
- The late genes code for the expression of structural proteins, which are found in the differentiated upper skin layers. This results in the tissues being expelled together with the upper layer’s dead cells.
Antigenic and genomic properties
- The HPVs exhibit a vast diversity.
- On the basis of genomic homology, more than 100 different HPVs have been identified.
- Certain kinds of HPV have a special preference for invading particular tissues.
- Approximately thirty varieties of HPVs infect the genital tract, with HPV-6 and HPV-11 being responsible for genital warts.
- HPV types 1–6 typically produce warts on the skin.
Pathogenesis and Immunity
- Human papillomaviruses exhibit an exceptional degree of host specificity.
- They have a strong preference for the skin and mucous membranes.
- HPV infection is transmitted through intimate contact and is begun by skin or mucous membrane diseases.
- Tissue tropism and disease presentation depend on the disease-causing HPV type.
Pathogenesis of human papilloma virus infections
- After infection, the virus replicates in the squamous epithelium of the skin, causing warts, and in the mucous membrane, causing oral, vaginal, and conjunctival papillomas.
- The warts are caused by the proliferation and thickening of the basal and prickly layers of the stratum spinosum and stratum granulosum due to a virus.
- The presence of koilocytes is characteristic of skin infections caused by HPV.
- These koilocytes are larger keratocytes with well-defined halos encircling tiny nuclei.
- The HPV infection always results in a localised infection, and warts typically heal on their own, presumably due to an immune response.
- Human papillomavirus has also been linked to the development of premalignant and malignant diseases of the mouth in humans.
- In addition to HPV-16, HPV-18, HPV-33, and HPV-35 have been associated with oral verruciform proliferation, oral premalignant lesions, and oral squamous cell carcinoma.
- Certain kinds of HPV are linked to dysplasia and may transform into carcinogenic strains in the presence of cofactors.
- It is known that human papillomavirus types 16 and 18 produce cervical papillomas and dysplasia. In over 85 percent of instances of cervical cancer, integrated HPV DNA, as opposed to plasmid-like DNA, was detected.
- These two viruses’ E6 and E7 proteins have been identified as oncogenes. It has been discovered that these oncogenes interfere with the normal function of regulatory proteins such p53, p16, and TRb, hence promoting the growth of tumour cells.
Host immunity
- The precise mechanism responsible for papilloma resolution is unknown.
- However, cell-mediated immunity seems to have a significant role in the resolution of the condition.
- Conditions that decrease cell-mediated immunity, such as HIV infection and immunosuppressive medication, exacerbate HPV infection, resulting in a more severe presentation of the disease.
Clinical Syndromes
Human papilloma virus infection causes: (a) cutaneous warts, (b) benign head and neck tumors, (c) genital warts, and (d) cancerous conditions in humans.
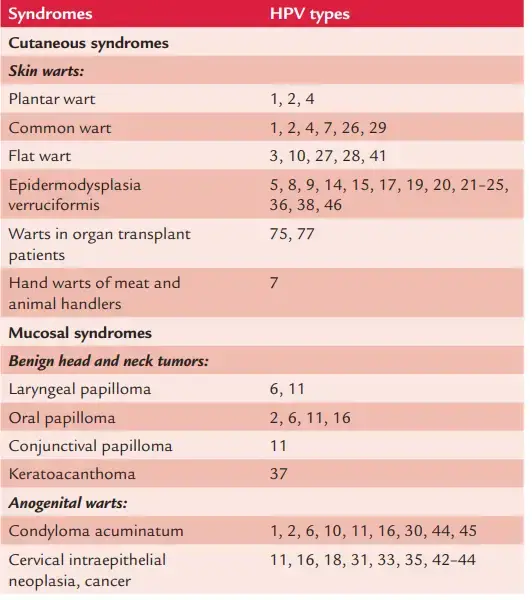
Cutaneous warts
- Common causes of cutaneous warts are HPV-2, HPV-4, and HPV-7.
- Depending on the type of HPV and the place of infection, warts typically appear on the hands and feet after an incubation period of 3–4 months.
- They may have a flat, plantar, or dome-like appearance.
- Plantar and flat warts are particularly prevalent in children and adolescents.
- A wart is typically a benign and self-limiting ailment that resolves with time.
Benign tumors of head and neck
- Oral papilloma, laryngeal papilloma, and conjunctival papilloma are examples.
- Papillomas of the mouth are often solitary but can be numerous.
- They are sessile, verrucous, whitish, and have elevated margins.
- Typically, these lesions manifest on the lips, hard palate, or gingiva.
- Heck disease or focal epithelial hyperplasia is often caused by HPV-13 and HPV-32.
- This disorder is characterised by the presence of numerous, smooth, sessile nodules on the mucosal surface of the lower lip or the buccal mucosa.
- People in North America have been described as having this condition.
- Laryngeal papillomas in children are fatal disorders caused by HPV-6 and HPV-11.
- This is the most frequent benign laryngeal epithelial tumour.
Genital warts
- Condyloma acuminatum or genital warts are caused by HPV-6 and HPV-11.
- The condition is characterised by solitary or multiple cerebriform and pink lesions, which arise more frequently on nonkeratinized mucosa than on keratinized mucosa.
- During sexual activity involving orogenital contact, these genital sores can also spread to the oral cavity.
Cancerous conditions
- Certain forms of the human papillomavirus (HPV), most frequently HPV-16 and less frequently HPV-18, HPV-33, and HPV-35, have been linked to oral premalignancy and cancer.
- These diseases are related with the development of oral verruciform proliferations.
- Oral premalignant lesions and oral squamous cell carcinoma caused by HPV-16 and HPV-18 are the most prevalent risk factors for intraepithelial cervical neoplasia and cancer.
- In 1–4 years, the disease advances from mild to moderate neoplasia to severe dysplasia or cancer in situ.
Epidemiology of HPV
Geographical distribution of HPV
HPV infections are found worldwide.
Reservoir, source, and transmission of infection
- Human papillomaviruses have been discovered in the mouths of approximately 6–10% of children and adolescents and 5–80% of healthy adults.
- Virus-containing vaginal secretions and skin sheddings contain HPVs. Humans are the principal source of infection.
- The shedding of viruses asymptomatically through body secretions increases the spread of infection to other human hosts.
- The illnesses are typically transmitted through skin-to-skin and vaginal contact. They are communicated:
- typically by sexual contact (HPV-16, HPV-18).
- through direct contact through skin and mucosal abrasions.
- via transit through an infected birth canal, as with laryngeal papilloma (types 6 and 11).
Laboratory Diagnosis of HPV
Morphological Identification
- When typical clinical lesions are present, HPV infection is easily diagnosable. Subclinical infection must be confirmed in the laboratory using cytological and histological detection methods.
- Using an immunoperoxidase test and antiserum, HPV capsid antigen in tissue slices or cell smears can be identified immunocytochemically (commercially available). It identifies all kinds of genital HPV.
- Molecular techniques: Amplification of HPV DNA by polymerase chain reaction (PCR) utilising consensus primers to identify a broad variety of HPV strains has also been utilised extensively.
Serology
- Such tests are more useful for demonstrating past exposure than current infection and are suitable for epidemiological research.
Treatment of HPV
- Over the course of months to years, warts are regressed.
- Cryotherapy, electrocautery, or chemical reagents may be utilised to eradicate the warts.
Prevention and Control of HPV
- There are no specific preventative strategies against HPV infection.
- The transmission of warts may be prevented by avoiding direct contact with infected warts.
- Safe sexual behaviour will aid in preventing the sexual spread of HPV.
Polyomaviruses
The Polyomaviridae family is an extinct subfamily of the Papovaviridae family (which no longer exists). These are small (45 nm in diameter) viruses that contain a circular genome of double-stranded DNA encased in a capsid with icosahedral symmetry. Histones are utilised to compact viral DNA within virus particles. The name is derived from the Greek words (poly) and (oma) (tumour). The viruses are species-specific, and while the production of tumours in experimental animals is widely established, to date there is no evidence linking any virus to a naturally occurring cancer in humans. Among the recognised members of this group are:
- Mouse polyomavirus
- SV 40 of monkeys
- JC virus (JCV)
- BK virus
Both JC virus (JCV) and BK virus (BKV) were called after the initials of the individuals from whom they were initially identified.
1. Mouse Polyomavirus
- It naturally produces mild infections in mice.
- When injected into infant rodents, however, it causes several sorts of cancerous tumours.
2. Simian Vacuolating Virus (SV 40)
- The simian vacuolating virus (SV 40) was isolated from uninoculated kidney tissue cultures of rhesus and cynomolgus monkeys.
- The role of SV 40 in the genesis of human malignancies is now being investigated.
- SV40 causes cancer in newborn hamsters.
- Due to its carcinogenic potential, live viral vaccines should only be produced in tissue cultures from monkey kidneys that have been screened and determined to be free of SV 40 infection.
3. JC Virus (JCV)
- 1971 saw the isolation of the JC virus from the brain of a Hodgkin’s disease and progressive multifocal leukoencephalopathy patient (PML).
- It was named after the initials of the individual from whom it was isolated for the first time.
- Progressive multi focal leukoencephalopathy (PML) is caused by JC virus since the lesions are limited to the white matter in immunocompromised individuals.
- In recent years, PML has been observed primarily in AIDS patients.
- Following intracerebral inoculation in neonatal hamsters, it produces malignant gliomas that are carcinogenic. Human brain cancers have been connected with JC virus.
4. BK Polyomaviruses
- From immunocompromised patients, the human polyomaviruses BK and JC have been isolated.
- It was called using the initials of the individual from whom it was initially isolated.
- BK virus was isolated from the kidney transplant recipient’s urine.
- Cystitis, nephropathy, and severe renal allograft failure are brought on by the BK virus.
- It is considered to be the cause of polyomavirus-associated nephropathy in renal transplant recipients, which leads to graft failure in up to 50% of infected patients.
Laboratory Diagnosis of Polyomaviruses
- Electron Microscopy: Human polyomaviruses can be discovered by electron microscopy in the brain tissue of a patient with PML (JC virus) and in the urine of a patient with a kidney transplant (BK virus).
- Virus Isolation: JC polyomavirus can be isolated from the urine or the brain, while BK polyomavirus can be isolated from the urine. JC polyomavirus BK virus is isolated using both human foetal glial cell culture and human diploid fibroblasts. Inhibition of hemagglutination is utilised to discriminate between these two viruses.
- Viral Antigen Detection: Brain biopsies and autopsies can be directly stained with immunofluorescence or immunoperoxidase to detect JCV antigen.
- Viral Nucleic Acid Detection: Nucleic acid hybridization and polymerase reaction can detect viral nucleic acid (PCR).
- Cytopathology: The cytology of urine in human polyomavirus infection is highly distinctive. Exfoliated urinary epithelial cells include bacophilic nuclei with a single inclusion that are larger and strongly pigmented.
Key Point
- Papovaviruses (from pa, papilloma, po, polyoma, va, vacuolating agent) are viruses with double-stranded DNA and two genera, Papillomavirus and Polyomavirus.
- Papillomaviruses are DNA viruses that infect the squamous epithelia and mucous membranes of vertebrates, including humans.
- Currently, over seventy varieties of human papillomaviruses (HPVs) have been identified.
- Papillomaviruses are the cause of various types of human warts, including cutaneous warts, genital warts, pulmonary papillomatosis, oral papillomas, and malignancy.
- Polyomaviruses include. mouse polyomavirus, simian virus 40 (SV 40) of monkeys, JC virus (JCV) and BK polyomavirus.
Differences between human papillomaviruses and human polyomaviruses
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.