What is Menstrual Cycle?
- The menstrual cycle is a complex physiological process that plays a vital role in female reproductive health, characterized by a series of hormonal and structural changes in the reproductive system. This cycle typically begins at puberty, marked by a stage known as menarche, and continues until menopause, generally occurring between the ages of 10 to 15 and 50, respectively. The average duration of the menstrual cycle is approximately 28 days, although it can vary between individuals, ranging from 20 to 45 days. These variations may influence fertility and overall reproductive health.
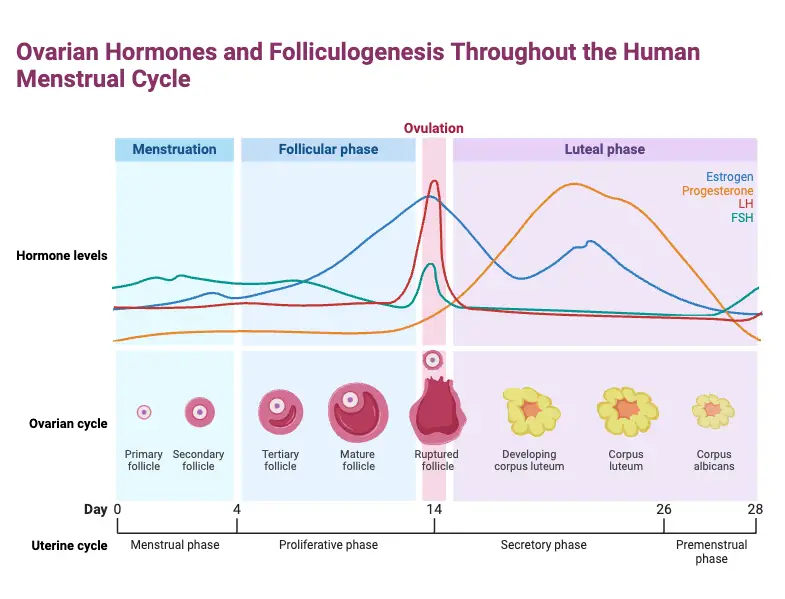
- Central to the menstrual cycle are two critical events that occur within the female reproductive organs: the release of a single ovum (egg) from the ovaries and the preparation of the uterine lining for potential implantation of a fertilized ovum. This cyclical interplay is driven by fluctuations in hormone levels, particularly estrogen and progesterone, which are crucial for the maintenance of the reproductive system’s functionality.
- The female reproductive system consists of several key structures, including the ovaries, which store and release ova; the uterus, where implantation of a fertilized egg occurs; and the fallopian tubes, which connect the ovaries to the uterus. The number of ova is predetermined before birth, and hormone stimulation during puberty initiates the monthly release of an ovum, continuing until menopause.
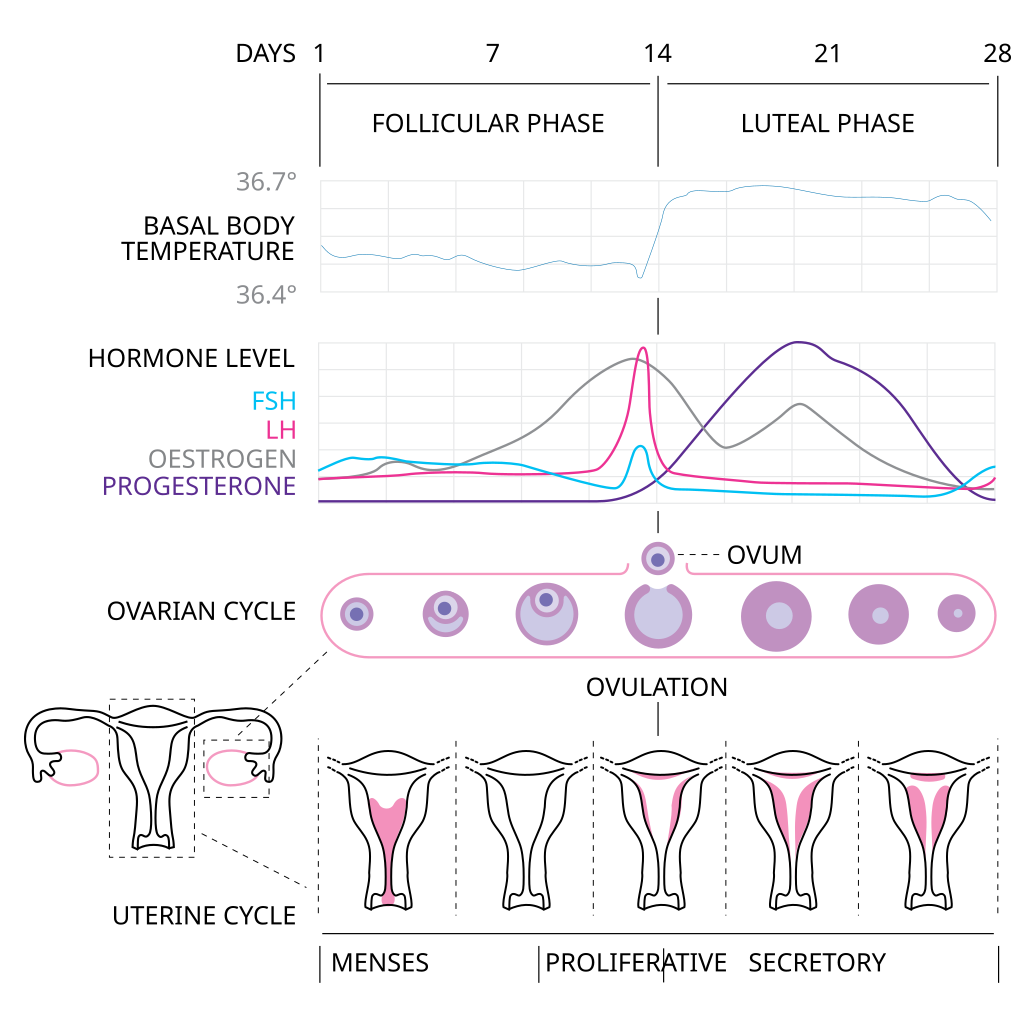
- The menstrual cycle can be divided into two main components: the ovarian cycle and the uterine cycle. The ovarian cycle includes three phases: the follicular phase, where follicles in the ovaries mature; ovulation, the release of the ovum; and the luteal phase, characterized by the production of progesterone to maintain the uterine lining. Concurrently, the uterine cycle consists of the menstrual phase, where the uterine lining sheds if fertilization does not occur; the proliferative phase, where the endometrium thickens in response to estrogen; and the secretory phase, where the endometrium prepares for potential implantation.
- Menstruation, often referred to colloquially as a period, marks the shedding of the uterine lining, resulting in bleeding that typically lasts about five days. This phase begins on the first day of the cycle and is a clear indicator that fertilization has not taken place. Hormonal changes lead to the breakdown of the thickened endometrium, followed by its expulsion from the body.
- In addition to the physiological changes, many women may experience premenstrual syndrome (PMS), which can include a range of symptoms such as breast tenderness, fatigue, and mood swings. A more severe form of this condition, known as premenstrual dysphoric disorder (PMDD), affects approximately 3–8% of women and can significantly impair daily functioning. Furthermore, some women experience dysmenorrhea, or menstrual pain, which can radiate from the abdomen to the back and thighs during the initial days of menstruation.
Definition of Menstrual Cycle
The menstrual cycle is a monthly series of physiological changes in the female reproductive system, characterized by the maturation and release of an ovum from the ovaries and the preparation of the uterine lining for potential implantation of a fertilized egg. If fertilization does not occur, the uterine lining is shed, resulting in menstruation. The cycle typically lasts about 28 days but can range from 20 to 45 days.
Hormones Involved in the Menstrual Cycle
The menstrual cycle is governed by a series of hormones that regulate its various phases, including follicular development, ovulation, and the preparation of the uterine lining for potential implantation.
- Follicle-Stimulating Hormone (FSH)
- Source: Secreted by the anterior pituitary gland.
- Function: FSH is pivotal in stimulating the growth of ovarian follicles. It promotes the maturation of oocytes (egg cells) and facilitates the production of estrogen by the granulosa cells within the developing follicles.
- Luteinizing Hormone (LH)
- Source: Also produced by the anterior pituitary.
- Function: LH is crucial for triggering ovulation. A significant surge in LH levels is what causes the release of a mature egg from its follicle. Following ovulation, LH encourages the formation of the corpus luteum, which is responsible for secreting progesterone.
- Estrogen
- Source: Primarily produced by the developing follicles in the ovaries.
- Function: Estrogen plays a central role in thickening the uterine lining (the endometrium), preparing it for possible implantation of a fertilized egg. Furthermore, it is involved in regulating FSH and LH through feedback mechanisms. Notably, high levels of estrogen can inhibit FSH release while promoting the release of LH just before ovulation.
- Progesterone
- Source: Secreted by the corpus luteum after ovulation.
- Function: Progesterone is essential for maintaining the uterine lining and preparing it for potential implantation of a fertilized egg. If fertilization does not occur, progesterone levels decline, resulting in the shedding of the endometrial lining and the onset of menstruation.
How Do Estrogen and Progesterone Levels Change Throughout the Menstrual Cycle
Estrogen and progesterone are two critical hormones that exhibit significant fluctuations throughout the menstrual cycle. Their changing levels are instrumental in regulating various reproductive functions, including the preparation of the uterine lining for potential implantation. The following outlines the hormonal changes during the different phases of the menstrual cycle:
- Menstrual Phase (Days 1-5)
- Estrogen and Progesterone Levels: Both hormones are at their lowest.
- Effects: The decline in estrogen and progesterone triggers the shedding of the uterine lining, leading to menstrual bleeding.
- Follicular Phase (Days 1-14)
- Early Follicular Phase:
- Estrogen: Begins to rise slightly as the follicles begin to develop but remains low initially.
- Progesterone: Continues to stay low.
- Mid-Follicular Phase (Around Day 7):
- Estrogen: Levels increase significantly due to the maturation of the dominant follicle, which produces more estradiol. This rise in estrogen contributes to the thickening of the endometrium in preparation for a potential pregnancy.
- Progesterone: Remains low during this phase.
- Early Follicular Phase:
- Ovulation (Around Day 14)
- Estrogen: Reaches its peak just before ovulation, driven by high levels produced by the mature follicle. This peak in estrogen stimulates a surge in Luteinizing Hormone (LH), which is crucial for triggering ovulation.
- Progesterone: Remains low until after ovulation occurs.
- Luteal Phase (Days 15-28)
- Post-Ovulation:
- Estrogen: After ovulation, estrogen levels decrease slightly but then rise again due to production by the corpus luteum.
- Progesterone: Levels rise significantly due to secretion from the corpus luteum, which prepares the endometrium for potential implantation of a fertilized egg. This phase typically lasts about 14 days.
- Post-Ovulation:
Summary of Hormonal Fluctuations
| Phase | Estrogen Levels | Progesterone Levels |
|---|---|---|
| Menstrual | Lowest | Lowest |
| Early Follicular | Low | Low |
| Mid-Follicular | Rising | Low |
| Ovulation | Peak | Low |
| Luteal | Rising then moderate | High |
Phases of the Menstrual Cycle
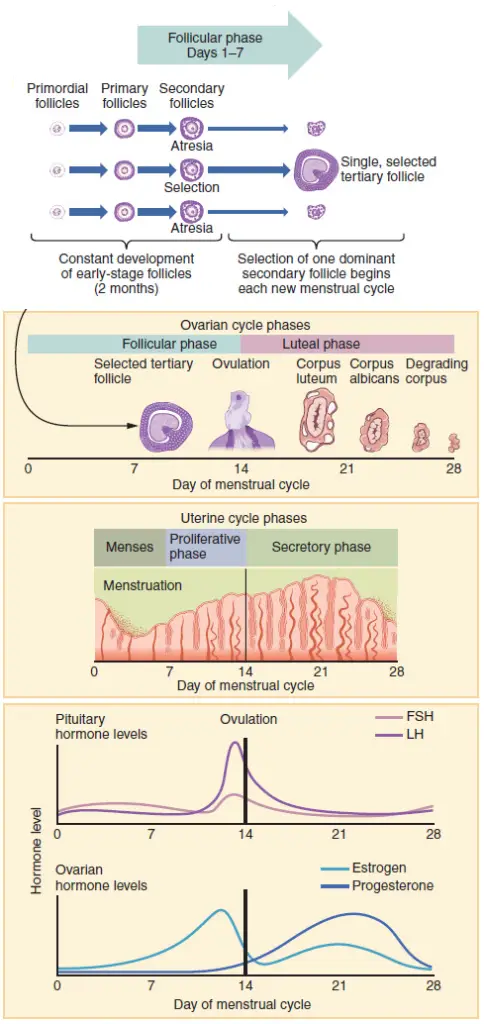
The menstrual cycle consists of a series of interconnected physiological changes that occur in the ovaries and the uterus, typically lasting about 28 days. These changes are categorized into two primary cycles: the ovarian cycle and the uterine cycle. Each of these cycles is further divided into distinct phases, each characterized by specific hormonal and physical transformations.
Ovarian Cycle
The ovarian cycle encompasses the development and maturation of ovarian follicles. It is divided into three key phases:
- Follicular Phase
- Initiation: This phase begins on day 1 of the menstrual cycle, coinciding with the onset of menstrual bleeding. It generally lasts from days 1 to 14 in a typical cycle.
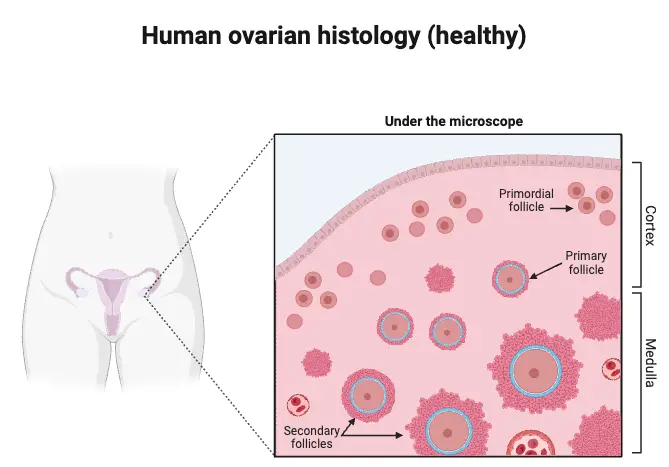
- Follicular Development: The release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the pituitary gland stimulates the growth of ovarian follicles. Initially, primordial follicles enlarge, transitioning into primary follicles.
- Dominance and Atresia: As FSH levels peak, several primary follicles mature into Graafian follicles. However, only one follicle typically dominates, a process known as atresia, which is crucial for preventing multiple pregnancies.
- Hormonal Production: The dominant follicle produces increasing amounts of estradiol, which promotes further follicular growth and prepares the endometrium for potential implantation.
- Ovulation Phase
- Timing: Ovulation occurs approximately 14 days after the start of menstruation. During this phase, the follicle swells, and a protrusion known as the stigma forms.
- Hormonal Surge: The surge in LH, triggered by elevated estradiol levels, causes the mature follicle to rupture, releasing the secondary oocyte into the peritoneal cavity. The oocyte then travels through the fallopian tube.
- Potential for Fertilization: If sperm are present, fertilization can occur, transforming the oocyte into a mature ovum. If fertilization does not take place, the oocyte degenerates within the fallopian tube.
- Luteal Phase
- Formation of Corpus Luteum: Following ovulation, the remaining follicular cells transform into lutein cells, forming the corpus luteum. This structure is crucial for hormone production.
- Hormonal Secretion: The corpus luteum produces progesterone, which is essential for maintaining the uterine lining. Progesterone inhibits FSH and LH secretion, preventing the maturation of additional follicles.
- Cycle Continuation: If pregnancy occurs, human chorionic gonadotropin (hCG) maintains the corpus luteum. In the absence of pregnancy, the corpus luteum degenerates, leading to decreased progesterone levels and the onset of menstruation.
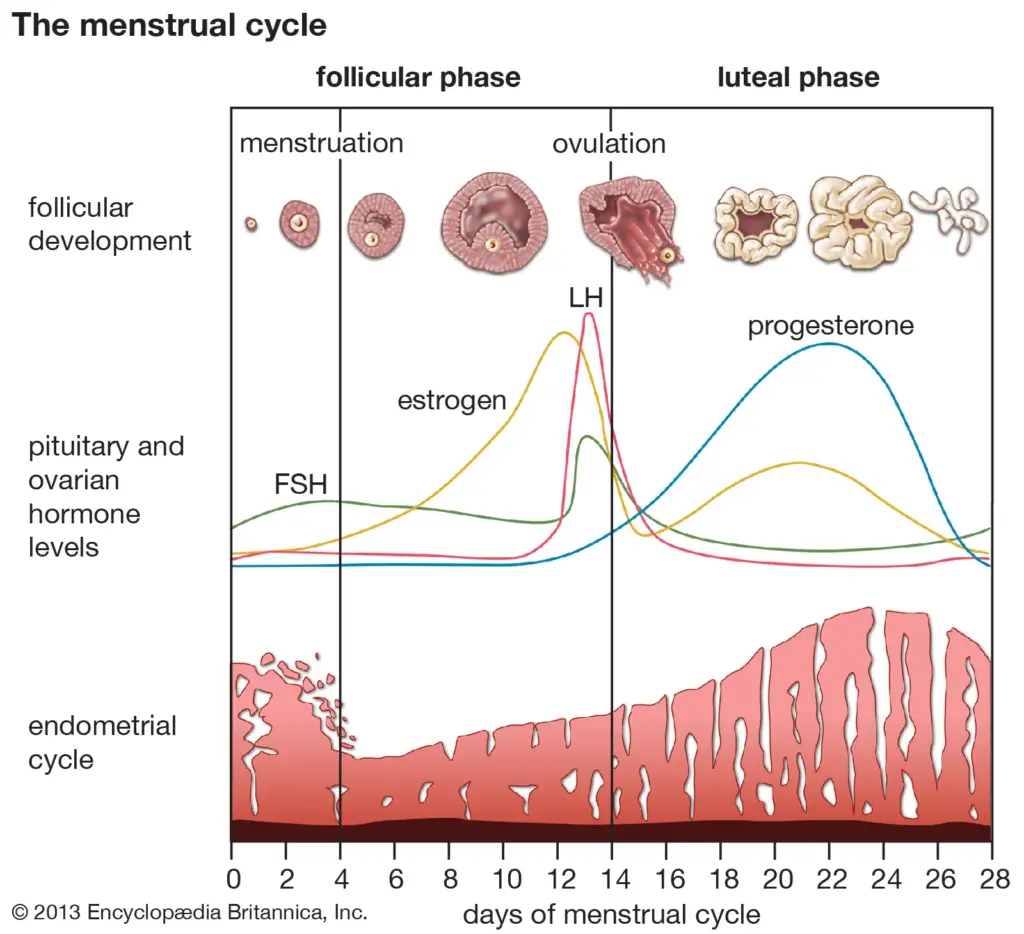
Uterine Cycle
The uterine cycle reflects changes in the endometrial lining of the uterus, also divided into three phases:
- Menstruation
- Onset: Menstruation marks the beginning of the uterine cycle and coincides with the follicular phase. It typically lasts from 3 to 7 days.
- Physiological Changes: As progesterone levels fall due to the degeneration of the corpus luteum, the endometrial lining sheds, resulting in menstrual bleeding. The fluid consists of blood, endometrial tissue, and secretions.
- Proliferative Phase
- Growth of Endometrium: Following menstruation, rising estrogen levels from the maturing follicles stimulate the proliferation of the endometrial lining. This phase typically lasts from day 6 to day 14.
- Endometrial Thickening: The endometrium thickens due to increased cell division and the formation of blood vessels, preparing the uterus for potential implantation.
- Secretory Phase
- Preparation for Implantation: This phase occurs after ovulation and aligns with the luteal phase of the ovarian cycle. It lasts from days 15 to 28.
- Hormonal Influence: Progesterone from the corpus luteum causes the endometrium to become more vascularized and glandular, enhancing its receptivity to a fertilized ovum.
- Outcome: If fertilization occurs, the fertilized ovum implants into the thickened endometrium. If not, the decrease in progesterone levels leads to the onset of menstruation, restarting the cycle.
Role of Hormones in the Menstrual Cycle
The menstrual cycle is a complex interplay of hormones that orchestrate various physiological changes essential for reproduction. Hormones such as estrogen, progesterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH) are critical in regulating the phases of the cycle. Their varying concentrations determine the progression of the cycle and the preparation of the female body for potential pregnancy.
- Follicle-Stimulating Hormone (FSH)
- Produced by the anterior pituitary, FSH initiates the growth of ovarian follicles.
- As these follicles mature, they secrete estrogen, which plays a crucial role in the cycle.
- The secretion of FSH gradually increases during the follicular phase, stimulating the development of multiple follicles.
- Luteinizing Hormone (LH)
- Also secreted by the anterior pituitary, LH works in tandem with FSH.
- The levels of both hormones peak mid-cycle, which is pivotal for ovulation.
- Just prior to ovulation, a significant surge in LH triggers the release of the mature ovum from the dominant follicle.
- Estrogen
- As follicles mature, they produce increasing amounts of estrogen, particularly 17-β estradiol.
- This hormone stimulates the proliferation of the endometrial lining, preparing it for potential implantation.
- Estrogen levels rise throughout the follicular phase, promoting both follicular growth and endometrial thickening.
- Progesterone
- After ovulation, the ruptured follicle transforms into the corpus luteum, which secretes progesterone.
- This hormone is essential for maintaining the endometrium, making it receptive for a fertilized ovum.
- Progesterone levels rise during the luteal phase, supporting the endometrial lining and preventing menstruation if fertilization occurs.
- Cyclical Changes in Hormone Levels
- The increase in estrogen and progesterone prepares the endometrium for a potential pregnancy.
- If fertilization does not occur, the corpus luteum degenerates, leading to a decline in progesterone and estrogen levels.
- The drop in these hormones triggers the disintegration of the endometrium, resulting in menstrual flow.
- Feedback Mechanisms
- The hormonal interplay also involves feedback mechanisms. For example, rising estrogen levels provide negative feedback to the anterior pituitary, reducing FSH production as the dominant follicle matures.
- Once ovulation occurs, the shift to positive feedback results in the surge of LH necessary for releasing the ovum.
Significance of Menstrual Cycle
The menstrual cycle is a critical physiological process that plays a fundamental role in various aspects of female health, particularly concerning reproduction and general well-being. It encompasses a series of hormonal changes that not only facilitate reproduction but also serve as indicators of broader health issues.
- Reproductive Health
- The menstrual cycle is essential for preparing the female body for ovulation and potential pregnancy. Hormonal fluctuations stimulate the maturation of ovarian follicles, culminating in the release of a mature egg during ovulation.
- Should fertilization occur, the cycle supports the implantation of the fertilized egg and early pregnancy through the hormonal support provided by the corpus luteum. This process is vital for ensuring successful conception and maintaining pregnancy.
- Indicator of Fertility
- Regular menstrual cycles are crucial for assessing female fertility. They serve as a clear indicator of balanced hormone levels and proper functioning of the reproductive system.
- Irregularities in menstrual cycles can signify underlying health issues such as polycystic ovary syndrome (PCOS) or endometriosis, both of which can negatively impact fertility.
- Overall Health Indicator
- The menstrual cycle has emerged as a vital sign of overall health. Regular cycles are associated with good hormonal balance, optimal bone density, cardiovascular health, and mental well-being.
- Variations in cycle patterns can reflect broader health concerns, including stress levels, nutritional status, and the presence of systemic diseases. Monitoring these changes can provide insights into an individual’s overall health.
- Clinical Relevance
- Healthcare providers often assess menstrual cycles during medical evaluations to identify potential health issues. A thorough understanding of menstrual physiology is crucial for diagnosing and managing various gynecological conditions.
- Knowledge of the menstrual cycle can assist in fertility planning and navigating the complexities of menopause.
- Psychological and Social Implications
- The menstrual cycle can significantly impact emotional well-being and overall quality of life. Many individuals experience premenstrual syndrome (PMS) or dysmenorrhea, conditions that can disrupt daily functioning and mental health.
- Recognizing and understanding these cyclical patterns enables better management strategies and interventions to improve quality of life.
- Cultural Significance
- Beyond its biological functions, menstruation carries profound cultural and social implications across different societies. Understanding its significance is essential for addressing stigma and promoting better reproductive health education.
- By fostering awareness and dialogue about menstruation, societies can work towards breaking down barriers and improving access to health education and resources.
Disorders Related to Menstrual Cycle
Menstrual cycle disorders encompass a variety of conditions that can significantly impact women’s health, affecting their physical well-being, emotional state, and overall quality of life.
- Dysmenorrhea
- Dysmenorrhea is characterized by painful menstrual cramps that can arise before or during menstruation.
- It can be divided into two types:
- Primary Dysmenorrhea: This type involves common menstrual cramps not linked to any underlying reproductive health issues. Symptoms typically decrease with age or following childbirth.
- Secondary Dysmenorrhea: This form is associated with underlying conditions, such as endometriosis or uterine fibroids, which cause more severe pain.
- Symptoms may include pelvic pain, headaches, nausea, vomiting, diarrhea, and fatigue, significantly affecting daily activities.
- Premenstrual Syndrome (PMS)
- PMS encompasses a range of physical and emotional symptoms that manifest during the luteal phase of the menstrual cycle.
- Common symptoms include bloating, breast tenderness, mood swings, irritability, fatigue, and depression. Approximately 30-40% of women report symptoms severe enough to disrupt their daily lives.
- Premenstrual Dysphoric Disorder (PMDD)
- PMDD is a more severe variant of PMS that can profoundly affect daily functioning.
- Symptoms are similar to those of PMS but are intensified and may include severe mood swings, irritability, anxiety, and depression, alongside physical discomfort. The severity of PMDD requires a more comprehensive management approach.
- Amenorrhea
- Amenorrhea refers to the absence of menstruation and is classified into two categories:
- Primary Amenorrhea: This occurs when an individual has not started menstruating by age 16.
- Secondary Amenorrhea: This is defined as the absence of menstrual periods for three months or longer in someone who previously had regular cycles.
- Various factors can lead to amenorrhea, including hormonal imbalances (such as those seen in polycystic ovary syndrome or PCOS), stress, extreme weight fluctuations, and certain medical conditions.
- Amenorrhea refers to the absence of menstruation and is classified into two categories:
- Abnormal Uterine Bleeding (AUB)
- AUB refers to any bleeding that deviates from normal menstrual patterns in terms of timing or volume.
- Types include:
- Menorrhagia: This condition is marked by heavy menstrual bleeding that interferes with daily activities.
- Metrorrhagia: This involves bleeding that occurs between menstrual periods.
- The causes of AUB can range from hormonal imbalances and uterine fibroids to polyps and certain medications.
- Irregular Periods (Oligomenorrhea)
- Oligomenorrhea is characterized by infrequent menstruation, defined as menstrual cycles that are more than 35 days apart.
- Hormonal changes due to conditions like PCOS, stress, significant weight changes, and excessive exercise often contribute to this irregularity.
- Thiyagarajan DK, Basit H, Jeanmonod R. Physiology, Menstrual Cycle. [Updated 2024 Sep 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK500020/
- https://byjus.com/biology/menstrual-cycle/
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/menstrual-cycle
- https://en.wikipedia.org/wiki/Menstrual_cycle
- https://www.healthline.com/health/womens-health/stages-of-menstrual-cycle
- https://my.clevelandclinic.org/health/articles/10132-menstrual-cycle
- https://www.mayoclinic.org/healthy-lifestyle/womens-health/in-depth/menstrual-cycle/art-20047186
- https://www.womenshealth.gov/menstrual-cycle/your-menstrual-cycle
- https://www.yourperiod.ca/normal-periods/menstrual-cycle-basics/
- https://www.sciencedirect.com/topics/medicine-and-dentistry/menstrual-cycle
- https://www.nhs.uk/conditions/periods/fertility-in-the-menstrual-cycle/
- https://www.ncbi.nlm.nih.gov/books/NBK279054/
- https://medlineplus.gov/menstruation.html
- https://www.webmd.com/women/normal-period
- https://www.hopkinsmedicine.org/health/wellness-and-prevention/menstrual-cycle-an-overview
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.