The male reproductive system includes a number of hormones and organs that are involved in reproduction. These hormones and organs can be found either inside or outside of the pelvis.
Organs of the Male Reproductive System
External male reproductive structures:
- Penis
- Scrotum
- Testicles (testes)
- Epididymis
Internal male reproductive organs:
- Vas deferens
- Ejaculatory ducts
- Urethra
- Seminal vesicles
- Prostate gland
- Bulbourethral glands
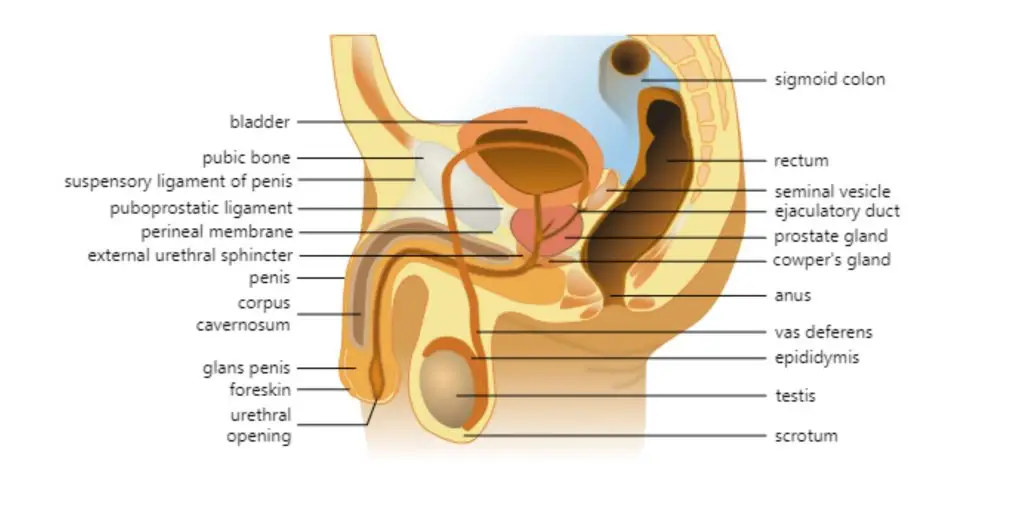
External male reproductive structures
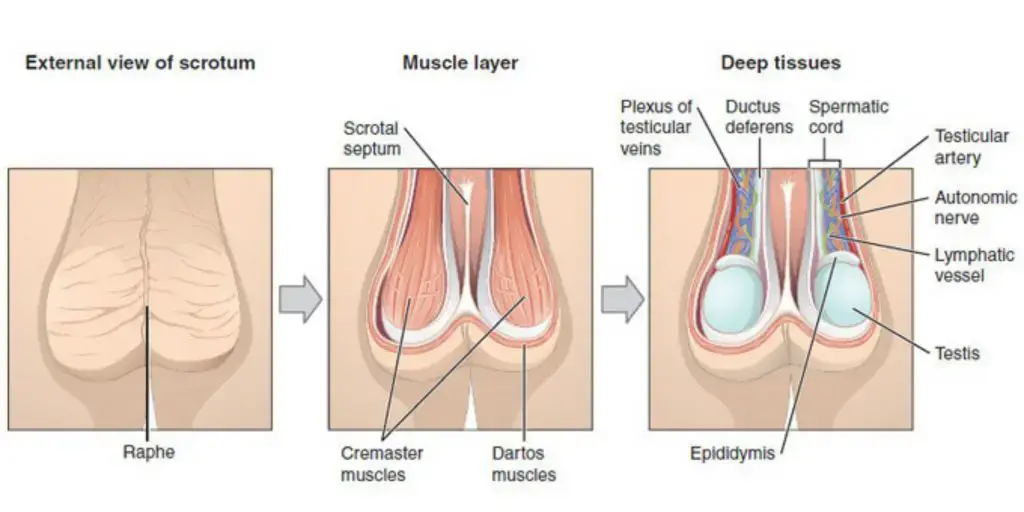
The scrotum contains the testes, epididymides and testicular ends. The scrotum, a pouch-shaped structure made up of fibrous connective tissue and smooth muscles, is called a scrotum. It is divided into two sections, each containing one testis.
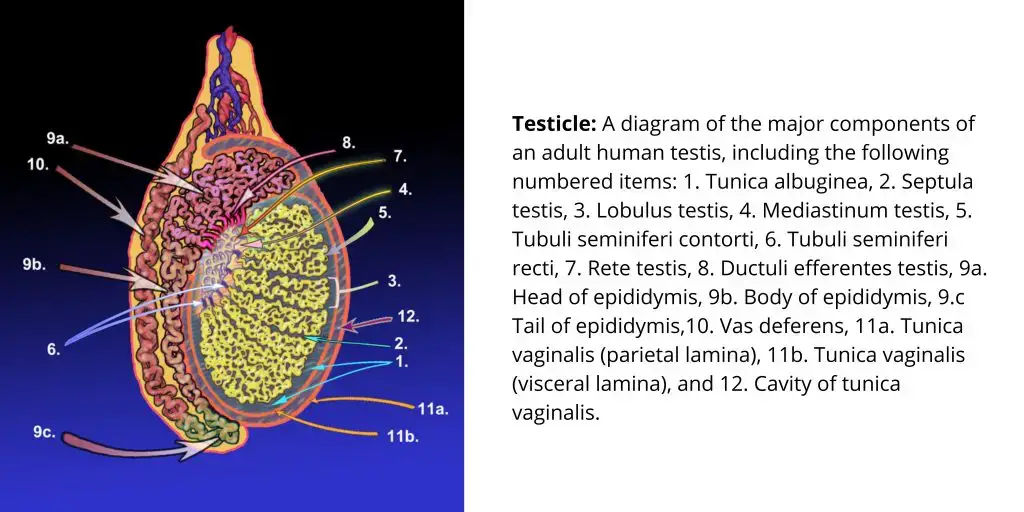
1. Testes
Birds and mammals have a pair of testes on each side. The left one is slightly larger than the right. The right testis is bigger than the left in the case of sharks. Primitive jawless fish have a single testis through the middle of their bodies. This is formed after the embryo has fused the paired structures.
The testes, which are male reproductive glands, measure approximately 4.5 cm in length, 2.5 cm in width, and 3 cm thick. They are surrounded by three layers: tunica vaginalis and tunica albuginea. The sperms are formed in a testis, which is made up of 900 seminiferous tubules. Amphibians have no seminiferous tubules, so the sperms are contained within a structure called the sperm ampullae.
Interstitial cells, also known as Leydig cells, are located between these tubules. They produce testosterone after puberty. The seminiferous tubules have been folded and packed tightly to form the epididymis, which is found in the scrotum as vas deference.
Function of Testes
- Testes play a vital role in the production of male sperms. Sperms are male gametes that fertilize female gametes during sexual reproduction.
- The production of androgens is also controlled by Sertoli cells found in the testes. Secondary sexual characteristics such as facial hair, voice and an abrupt rise in height in men are all caused by testosterone.
- The storage of sperms is also done by the testes’ seminiferous tubules. The tubules contain Leydig cells that provide nutrients to the sperms for storage.
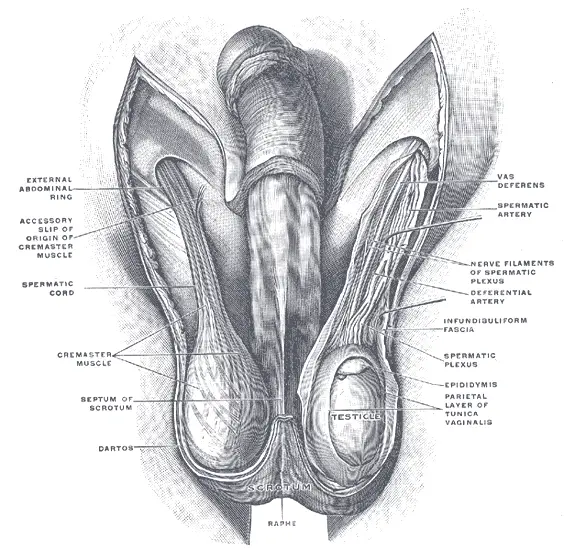
2. Spermatic Cords
With the help of the Spermatic Cords, the testes can be suspended in the scrotum. The cord is made up of the testicular artery and veins, the lymphatics, the deferent duct and testicular nerves. Smooth muscles and connective tissue cover the spermatic cords.
The function of Spermatic Cords
- Vas deferens is a component of the spermatic chord that allows for the transfer of sperm between the testes and the ejaculatory tube.
- The cords have many blood vessels and nerves that allow for continuous blood flow throughout the male reproductive system.
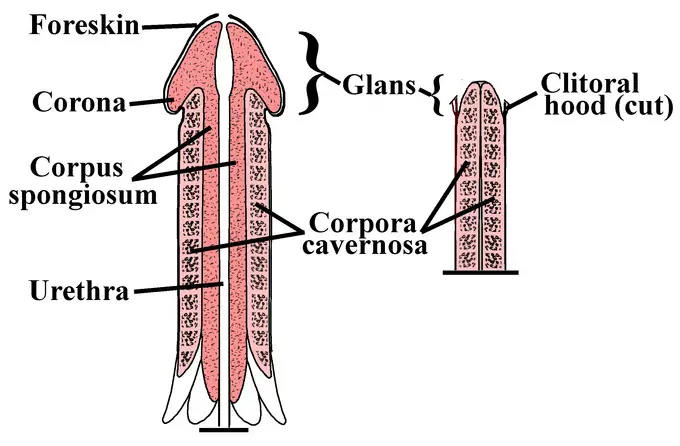
3. Penis
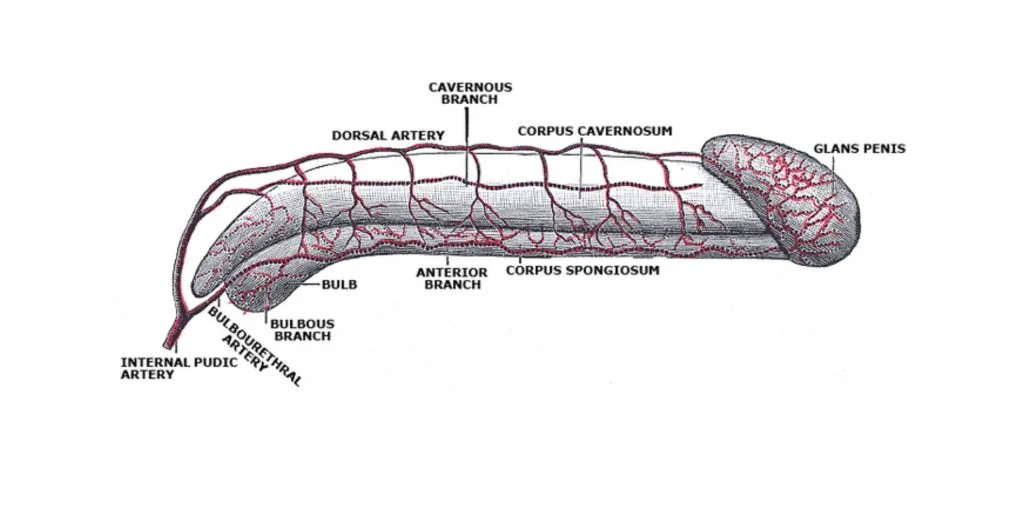
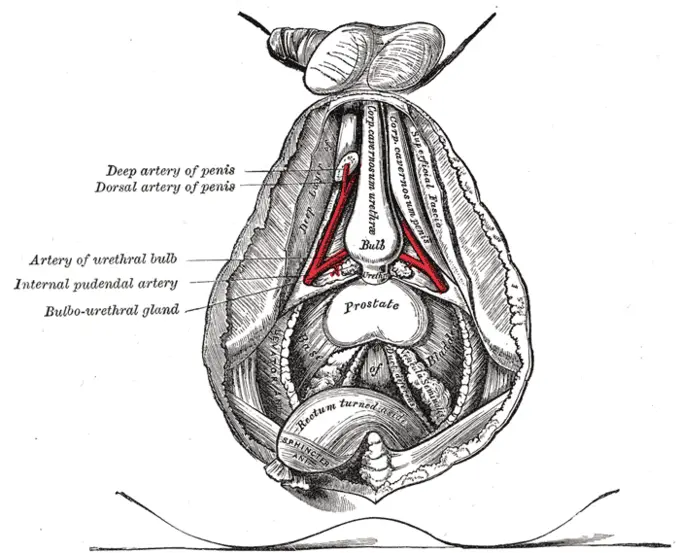
A penis is made up of two parts: a root and a part called the body. The body surrounds the bladder and the root is located within the perineum. It is composed of three cylindrical masses known as erectile tissues and some involuntary muscle. The fibrous connective tissue that makes up the erectile tissue is covered with skin which has a high blood supply. The penis is divided into two columns, the corpora cavernosa column and the corpora spongiosum column.
The penis tip is formed into a triangular structure known as glans penis. Above it is a foldable skin called a prepuce. The penis receives blood from the deep, dorsal and bulbar veins, while the blood is then drained through the penis’ bundle of veins. It also has somatic and autonomic nerves.
The function of the penis
- Penile Erection, an important function in the penis, is caused by the parasympathetic nervous system.
- Parasympathetic impulses, which can be physical or psychic stimulation, reach the penis via the spinal duct as a result.
- The same nervous impulses cause the blood vessels to dilate in the penis, resulting in rapid arterial blood flow through them. Rapid blood flow causes fibrous tissues to balloon to the point that the penis becomes hardened and erect.
The penis is the male organ of copulation, responsible for sexual intercourse. In its flaccid state, the penis is soft and relaxed, primarily used for urination. However, with sexual arousal, it becomes engorged and rigid. This turgid and rod-like state allows the penis to penetrate the vagina during sexual intercourse and deposit semen into the female reproductive tract.
The shaft of the penis encompasses the urethra and consists of three columns of erectile tissue. These chambers of erectile tissue span the length of the shaft. The two larger chambers on the sides are called corpora cavernosa, which make up the majority of the penis. The smaller chamber, known as the corpus spongiosum, surrounds the penile urethra and can be felt as a raised ridge on an erect penis. The glans penis, located at the tip of the penis, is highly sensitive due to a concentration of nerve endings. This sensitivity influences the likelihood of ejaculation. The skin from the shaft extends over the glans, forming a collar known as the prepuce or foreskin. The foreskin provides lubrication and protection to the sensitive skin of the glans penis. Circumcision, a surgical procedure often performed for religious or social reasons, involves the removal of the prepuce, typically in infancy.
Erections can be induced by sexual arousal or during rapid eye movement (REM) sleep, which is associated with dreaming. The process of penile erection involves vasocongestion, which is the engorgement of tissues due to increased arterial blood flow into the penis compared to venous outflow. During sexual arousal, nerve endings release nitric oxide (NO) near blood vessels within the corpora cavernosa and spongiosum. NO activates a signaling pathway that causes relaxation of the smooth muscles surrounding the penile arteries, leading to their dilation. This dilation allows a greater amount of blood to enter the penis. The endothelial cells in the penile arterial walls also secrete NO, perpetuating the vasodilation. The rapid influx of blood fills the erectile chambers, and the increased pressure from the filled chambers compresses the thin-walled penile venules, preventing venous drainage from the penis. This increased blood flow to the penis and reduced blood return results in an erection. The size of the erect penis varies among individuals, but on average, it measures approximately 15 cm (6 inches) in length, depending on the flaccid dimensions of the penis.
4. Scrotum
The purpose of the Scrotum is for the testes to have a temperature chamber that allows them to produce optimal sperm.
- The fastest way to disperse excess heat is to move the testes away form the abdomen and increase the surface area.
- Constant pressure from the abdominal muscles could cause testes to be empty before the epididymis and testes are mature enough for fertilization.
- The scrotum seems to have the function of keeping the body’s temperature slightly lower than the rest.
Anatomical Considerations
The scrotum, a suspended sack of skin with smooth muscle and dual-chambered suspension sack, contains the testes and is homologous in females to the labia majora. It is located between penis and anus and is an extension to the perineum. In humans, as well as other mammals, the increased testosterone secretion in puberty results in darkening the skin and the development of pubic hairs on the scrotum. The testis on the left side is typically lower than that on the right. This may help to prevent compression in the event there is an impact. This may allow for more efficient cooling.
Function
The scrotum seems to have a function to maintain a slightly lower temperature in the testes than the rest of your body. The temperature of the testes should be at least one to two degrees Celsius lower than the body temperature (around 35° Celsius or 95° Fahrenheit). Higher temperatures can cause damage to sperm counts.
Temperature is controlled by the scrotal movement, which moves the testes towards or away from the body according to the environment. The faster dispersion and movement of the testes from the abdomen to increase the surface area allows for a greater heat exchange. This is achieved by the contraction and relaxation of both the cremaster muscle in the scrotum and the dartos fascia.
The scrotum may also be responsible for temperature regulation. According to some studies, testes located within the abdomen cavity would be more likely to experience the frequent changes in abdominal pressure caused by the abdominal muscles. This would result in a faster emptying of the testes, and an epididymis of fertilized sperm, before the spermatozoa mature enough for fertilization. Some mammals, such as elephants and marine mammals, keep their testes in the abdomen to avoid accidental emptying.
Internal male reproductive organs
1. Prostate Gland
The prostate gland is located in the pelvic cavity, in front of the heart. It is enclosed by an outer fibrous layer and a smooth muscle layer.
The function of the prostate gland
- The thin milky liquid that the prostate gland produces is made up of calcium ions and citrate ions. It also contains phosphate and phosphate.
- The fluid’s slightly alkaline properties play a crucial role in successful fertilization. Acidic due to citric acid and other metabolic products in the sperm, the liquid in the ejaculatory tube results in sperm fertility inhibition.
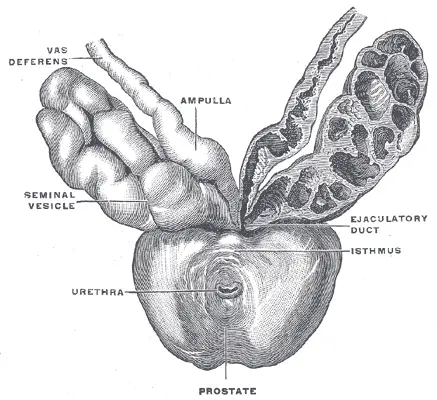
2. Seminal Vesicles
Seminal Vesicles, a small fibromuscular organ, are surrounded by a columnar epithelium on either side. A small duct that connects to each seminal vein to form the ejaculatory conduit is formed from each one.
The function of Seminal Vesicles
- The seminal veins’ secretory columnar epithelium secreted mucoid fluid rich with fructose, citric and other essential nutrients.
- After the sperms have been brought to the ejaculatory tube via spermatid cords each seminal vein expels its contents onto the ejaculatory tube.
- The mucoid provides nutrients and energy to the sperms, until one of them fertilizes the egg.
3. Other Internal Organs
- Epididymis: The epididymis, which is a long, coiled tube found on each testicle’s backside, is the epididymis. It stores and transports sperm cells from the testes. The epididymis is also responsible for maturing the sperm, as the sperm from the testes is immature and ineligible for fertilization. Contractions push the sperm into vas deferens during sexual arousal.
- Vas deferens: This is the long, muscular tube that runs from the epididymis to the pelvic cavity and just below the bladder. In preparation for ejaculation, the vas deferens transports mature or unmature sperm to its urethra.
- Ejaculatory ducts: These are formed from the fusion between the seminal and vas deferens (see below). The ejaculatory tubes drain into the urethra.
- Urethra: This tube carries urine from bladder to the outside of the body. It also serves the purpose of ejaculating the sperm when a man has had an affair. The flow of urine becomes blocked by the urethra when the penis is raised during sex. This allows only the semen to be ejaculated at the orgasm.
- Bulbourethral glands: These are small structures about the size of a pea and located just below the prostate. The clear, slippery fluid produced by these glands is able to drain directly into the bladder. This fluid is used to lubricate and neutralize acidity in the urethra from any urine residual.
Hormones involved in Male Reproductive System
- Testosterone: Testosterone is a hormone is secreted in the testes by Leydig cells, or interstitial cells. It is responsible for the development and division germinal cells in the early stages of the spermatogenesis process.
- Luteinizing hormone: This hormone is produced by the pituitary, which stimulates the Leydig cells to release testosterone hormone.
- Follicle Stimulating hormone: Also secreted from the anterior pituitary, this hormone functions in stimulating Sertoli cells. This allows for the conversion of spermatids to sperms.
- Estrogen: Estrogen from Sertoli cells plays a role in spermatogenesis.
- Growth hormone: This hormone allows for the overall development and protection of the background activities in the tests.
How Does the Male Reproductive System Work?
The male reproductive system:
- makes semen (pronounced: SEE-mun)
- During sexual intercourse, semen is released into the reproductive system by the female.
- Produces sex hormones that help a boy become a sexually mature male during puberty
A baby boy’s reproductive system is already in place when he is born. However, it is not until puberty that he can reproduce. The pituitary gland, located near the brain, secretes hormones to stimulate the production of testosterone. This happens between 9 and 15. Many physical changes are caused by testosterone production.
While every man experiences these changes at a different time, most stages of puberty follow a consistent sequence.
- The scrotum grows larger during the first stage in male puberty.
- The penis grows longer, and the seminal and prostate vesicles grow.
- The pubic area, then the underarms and face, is where hair begins to grow. The voice becomes deeper during this period.
- As they grow up, puberty is also a time when men experience a growth spurt.
Can a man go through menopause?
Menopause refers to the loss of normal menstrual function in women. This is characterized by hormonal changes in women. After menopause, one of the most significant changes for women is the inability to have children. Contrary to the ovaries and testes, the testes don’t lose their ability to produce hormones. A healthy man may still be able make sperm into his 80s if he is in good health.
However, subtle changes in function can occur as early as 45-50 years old and more pronounced after 70. While hormone production can remain relatively constant for many men into old age, some may experience a decline in hormone production. Sometimes, this can be due to a disease such as diabetes.
It is not clear if a decrease in testicular function causes symptoms such as fatigue, weakness or depression.
Is it possible to treat “male menopause”?
Hormone replacement therapy can be used to treat low testosterone levels. This may include fatigue, loss of interest in sex and depression, as well as fatigue. Replacing male hormones can lead to prostate cancer and atherosclerosis (hardening the arteries).
Before you start hormone replacement therapy, you should have a thorough physical exam and lab tests. Many questions remain about whether hormone replacement therapy is beneficial for middle-aged men. Discuss with your healthcare provider all aspects of the treatment, including the pros and cons and the best choice for you.
What Do Sperm Do?
One million sperm cells are produced every day by a male once he reaches puberty. Each sperm cell is tiny, only 1/600th of an inch (0.05 mm) long. The seminiferous tube system, which is a network of tiny tubes that connect to the testicles, allows for the development of sperm. These tubules are made up of simple, round cells at birth. These cells transform into sperm cells when they are stimulated by testosterone and other hormones. Cells divide and change until they form a head and a tail like tadpoles. The head is a repository of genetic material (genes). The epididymis is where the sperm complete their development.
The sperm moves to the vas derfens (pronounced VAS DEFEE-uh-runz), which is also known as the sperm duct. Seminal vesicles, the prostate gland and sperm duct make a white fluid known as seminal fluid. This fluid mixes with sperm to create semen when a man is sexually stimulated. When a male sexually stimulates his penis, it becomes hard and hangs limp. The penis tissues become stiffer and more rigid when they are flooded with blood. It is easier to insert the penis into the female’s genital canal during sex because of its rigidity. The erect penis contracts when the stimulation is applied to it. This forces the semen through the bladder and duct system. Ejaculation is the process by which the male’s sperm is forced out of his body via his urethra. A man can ejaculate up to 500 million sperm each time.
What Is Conception?
Millions of sperm can be “swimmed” from the female’s vagina to reach the egg in the fallopian tubes when semen is ejaculated. To fertilize an egg, it takes one sperm.
The fertilized egg, also known as a zygote, contains 46 chromosomes. Half of them are from the egg while the other half come from the sperm. The male and female genetic material combine to create a new individual. As the zygote grows in the female’s body, it divides again. It matures over the course the pregnancy into an embryo and a fetus and then a baby.
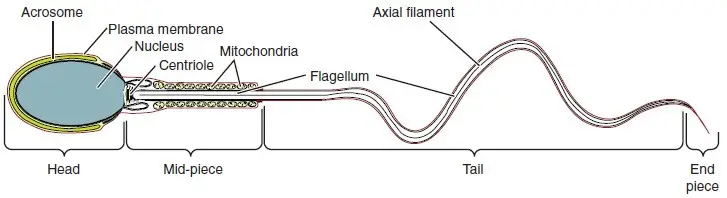
Structure of Formed Sperm
- The structure of formed sperm is specifically adapted to carry out its essential role in fertilization. Sperm cells are remarkably smaller than most cells in the body, with a volume that is approximately 85,000 times less than that of the female gamete. Despite their minuscule size, an impressive number of sperm are produced each day, ranging from 100 to 300 million, ensuring a sufficient supply for reproductive purposes.
- The structure of sperm cells is composed of three distinct regions: the head, mid-piece, and tail. Each region plays a crucial role in facilitating the sperm’s function.
- The head of the sperm is the most compact and specialized part. It contains the nucleus, which is haploid, meaning it carries only half the number of chromosomes compared to other body cells. This haploid nucleus is tightly packed and contains very little cytoplasm, contributing to the overall small size of the sperm cell. The head measures only about 5 μm in length. Covering most of the head is a structure called the acrosome. The acrosome acts as a cap and is filled with lysosomal enzymes that are vital for the sperm’s ability to participate in fertilization. These enzymes aid in the penetration of the egg’s protective layers, allowing the sperm to reach the egg and facilitate fertilization.
- Located in the mid-piece of the sperm are tightly packed mitochondria. Mitochondria are the powerhouses of cells, producing ATP (adenosine triphosphate), which serves as the energy source for various cellular activities. In the case of sperm, ATP generated by the mitochondria in the mid-piece provides the energy required for the flagellum’s movement. The flagellum is a long, whip-like tail that extends from the neck and mid-piece through the tail region of the sperm. It is responsible for propelling the entire sperm cell towards the egg. The flagellum’s central strand, known as the axial filament, is formed from one centriole inside the maturing sperm cell during the final stages of spermatogenesis. This axial filament serves as the core structure that enables the flagellum’s movement and allows the sperm to swim in a forward motion.
- In summary, the structure of formed sperm exhibits unique adaptations that align with its function in fertilization. The compact head with its acrosome facilitates penetration of the egg, the mid-piece packed with mitochondria provides the necessary energy, and the flagellum propels the sperm towards the egg for successful fertilization. These specialized structures and their coordinated functions ensure the sperm’s ability to navigate the female reproductive tract and increase the chances of fertilizing an egg.
Sperm Transport
Sperm transport is a crucial process that involves the movement of sperm from the seminiferous tubules in the testes to the female reproductive tract for fertilization to occur. This journey encompasses various structures and accessory glands of the male reproductive system.
- The epididymis plays a vital role in sperm maturation and transport. Immotile sperm from the seminiferous tubules are surrounded by testicular fluid and directed to the epididymis, a coiled tube attached to the testis. Although the epididymis appears compact due to its coiled nature, it would measure around 6 meters (20 feet) if straightened. It takes approximately 12 days for sperm to travel through the coils of the epididymis, with the shortest recorded transit time being one day in humans. As sperm traverse the epididymis, they mature further and gain the ability to move independently. The smooth muscles lining the epididymal tubes contract to propel the sperm along its length. Once mature, the sperm are stored in the tail of the epididymis until ejaculation occurs.
- During ejaculation, sperm exit the tail of the epididymis and are pushed by smooth muscle contractions into the ductus deferens (vas deferens). The ductus deferens is a thick, muscular tube bundled together with connective tissue, blood vessels, and nerves to form the spermatic cord within the scrotum. The ductus deferens extends into the abdominal cavity through the inguinal canal, continuing posteriorly into the pelvic cavity. It ends behind the bladder in a dilated region called the ampulla.
- Semen, the fluid ejaculated by males, consists of more than just sperm. Only about 5 percent of the semen volume is composed of sperm, while the majority is contributed by three accessory glands of the male reproductive system: the seminal vesicles, the prostate gland, and the bulbourethral glands.
- The seminal vesicles are paired glands that contribute approximately 60 percent of the semen volume. As sperm pass through the ampulla of the ductus deferens during ejaculation, they mix with fluid from the seminal vesicles. The fluid secreted by the seminal vesicles contains a high concentration of fructose, which serves as an energy source for the sperm’s movement through the female reproductive tract.
- Next, the mixture of sperm and seminal vesicle fluid moves into the ejaculatory duct, a short structure formed from the ampulla of the ductus deferens and the duct of the seminal vesicle. The ejaculatory ducts then transport the seminal fluid into the prostate gland.
- The prostate gland is situated in front of the rectum, at the base of the bladder, and surrounds the prostatic urethra. It is composed of muscular and glandular tissues and secretes an alkaline, milky fluid that helps coagulate and later decoagulate the semen. Coagulation of semen temporarily retains it within the female reproductive tract, providing ample time for sperm to utilize the fructose from seminal vesicle secretions. When the semen regains its fluid state, sperm can move farther into the female reproductive tract.
- The final addition to semen is made by the bulbourethral glands, also known as Cowper’s glands. These two glands release a thick, salty fluid that serves as lubrication for the urethra’s end and the vagina. It also aids in cleaning any urine residues from the penile urethra. The secretion from the bulbourethral glands, known as pre-ejaculate, is released after sexual arousal and shortly before semen is ejaculated. It is important to note that pre-ejaculate fluid may contain sperm already present in the urethra, potentially leading to pregnancy.
Overall, sperm transport involves a series of coordinated movements and contributions from various structures and accessory glands within the male reproductive system. These processes ensure that sperm are properly matured, propelled, and accompanied by the necessary fluids for successful fertilization.
Testosterone
Testosterone is an androgenic steroid hormone that is primarily produced by Leydig cells in the testes. These cells are also referred to as interstitial cells due to their location between the seminiferous tubules. Testosterone secretion begins in male embryos around the seventh week of development, with peak concentrations reached during the second trimester. This early release of testosterone is responsible for the development of male sexual organs. In childhood, testosterone levels are low, but they increase significantly during puberty, triggering characteristic physical changes and initiating spermatogenesis.
The functions of testosterone are essential for the proper functioning of the male reproductive system. Leydig cells produce approximately 6 to 7 mg of testosterone per day. Testosterone concentrations in the testes are about 100 times higher than in the circulation. Maintaining these normal concentrations of testosterone is crucial for promoting spermatogenesis, and low levels of testosterone can lead to infertility. Additionally, testosterone is released into the systemic circulation and plays a vital role in muscle development, bone growth, the development of secondary sex characteristics, and the maintenance of libido (sex drive) in both males and females. While the ovaries in females secrete small amounts of testosterone, most of it is converted to estradiol. The adrenal glands in both sexes also secrete a small amount of testosterone.
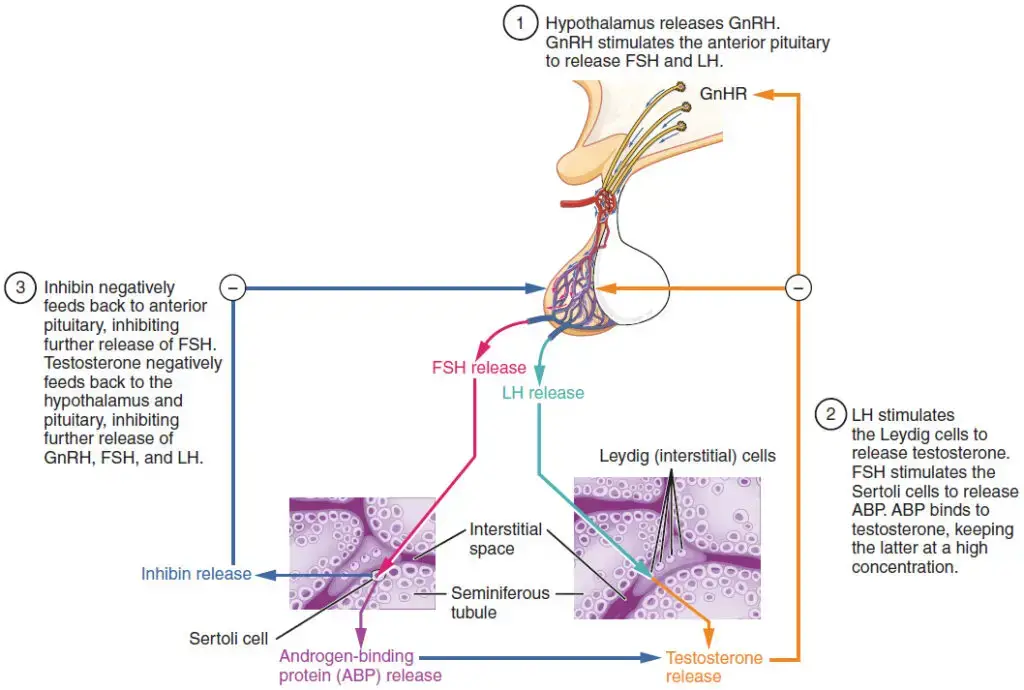
The regulation of testosterone concentrations throughout the body is critical for male reproductive function. The hypothalamus and the pituitary gland in the brain play a crucial role in controlling testosterone synthesis and secretion. The regulation begins in the hypothalamus, where the release of gonadotropin-releasing hormone (GnRH) stimulates the anterior pituitary gland to release luteinizing hormone (LH) and follicle-stimulating hormone (FSH). These two hormones are essential for reproductive function in both men and women. In men, FSH primarily acts on Sertoli cells within the seminiferous tubules, promoting spermatogenesis. FSH also stimulates the production of inhibins by Sertoli cells, which inhibit FSH release from the pituitary, thus reducing testosterone secretion. Inhibins serve as markers of spermatogenic activity. LH binds to Leydig cells in the testes, stimulating the production of testosterone.
The synthesis and secretion of FSH and LH are regulated by a negative feedback loop. Low blood concentrations of testosterone stimulate the hypothalamus to release GnRH, which then stimulates the pituitary to secrete LH into the bloodstream. LH binds to Leydig cells, promoting testosterone release. When blood concentrations of testosterone reach a critical threshold, testosterone binds to androgen receptors on the hypothalamus and pituitary, inhibiting the synthesis and secretion of GnRH and LH, respectively. As testosterone levels decline, the feedback loop is released, leading to the secretion of GnRH and LH, stimulating testosterone production. A similar feedback mechanism exists for FSH and inhibin, controlling spermatogenesis.