What Is Reproduction?
Reproduction refers to the process where organisms create more of themselves. However, although the reproductive system is vital to maintaining a species’ existence, unlike other body systems it is not essential for keeping an individual alive.
Two types of sex cells (GAH-meetz) are involved in the human reproductive process. In the female’s reproductive system, the male gamete (or sperm) and the female gamete (or egg or ovum), meet. The fertilized egg, also known as a ZYE-goat, is created when sperm fertilizes an egg (pronounced ZYE’-goat). The zygote develops into an embryo and a fetus.
Both the male and female reproductive systems are required for reproduction.
Like all organisms, humans pass on some traits to their children. This is done through genes, which are the special carriers of human traits. Parents pass on genes to their children. These genes make them similar, but each child is unique. These genes are derived from the male’s eggs and the female’s sperm.
Definition of Female Reproductive System
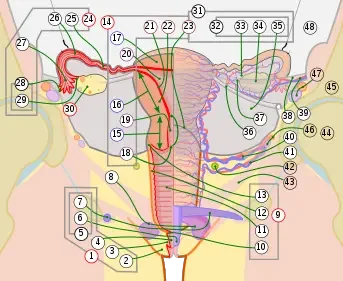
The female reproductive system is a group of cells, hormones, and organs that work together to form the female gamete. The female reproductive system is divided into two parts: the external organs and the internal organs.
- External organs of the female reproductive system; Labia majors, Labia minora, Clitoris, Vaginal orifice, Vestibular gland (Bartholin’s gland), Hymen
- Internal organs of the female reproductive system: Vagina, Uterus, Uterine tubes (Fallopian tubes), Ovaries
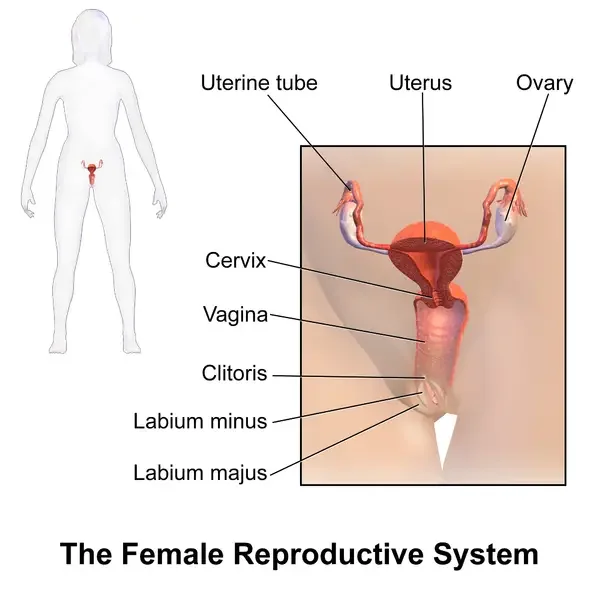
External Genitalia (Vulva)
Collectively, the external organs of the female reproductive system are called vulva. They include labia majora and minora, clitoris and vaginal orifice.
1. Labia majors
These large muscle folds surround the vulva and are made up of fibrous tissue, fat, akin, and many sebaceous glands. The folds merge with the perineum in the anterior, while they join to the pubis.
2. Labia minora
The labia minora is a smaller fold that lies beneath the labia majora. You will also find a lot of sebaceous cells. The vestibule is located between the folds. It is the entrance to the vagina, vestibular and urethra.
3. Clitoris
Clitoris is a complex sensory nerve ending that corresponds to the penis of Male. They are not of reproductive importance.
4. Hymen
The hymen is a thin membrane of mucosal material that lies in front of the opening to the vagina.
5. Vestibular glands
Vestibular glands, also known as Bartholin’s gland, are tiny glands about the size of a pea. They have ducts that open into the vestibule. These glands are located on either side the vaginal opening. Their secretion helps keep the vagina moist.
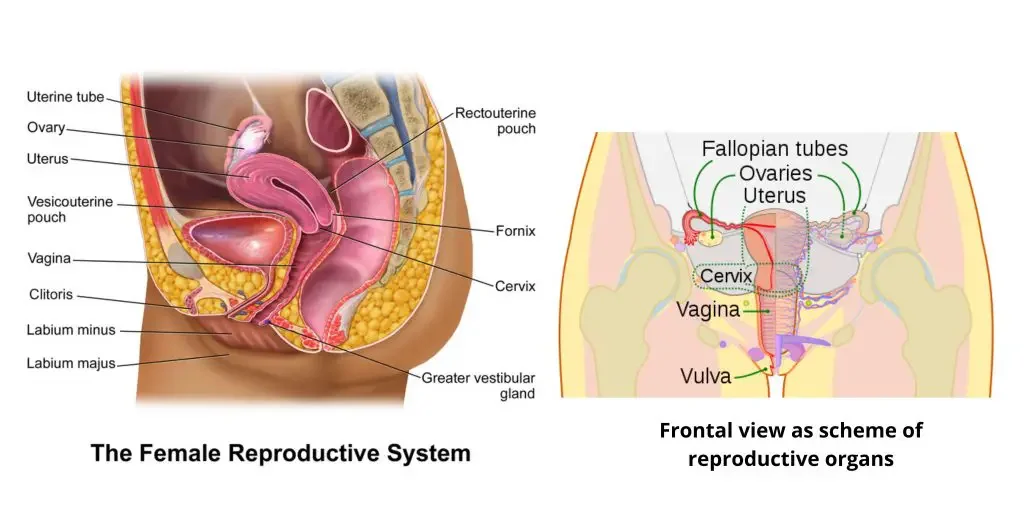
Internal Genitalia
The female’s internal genitalia can be found in the pelvic cavity. It consists of a uterus and a vagina. There are two uterine tubes and two ovaries.
Ovaries
An ovary, the gonad in the female reproductive system, produces an ovum which develops into fertilization.
Structure of Ovaries
Ovaries are female glands, or gonads, that occur in pairs in humans. They lie on the lateral wall and pelvis walls on the ovarian fossa. Birds only have one functional ovary, the other being inactive. They measure 2-3 cm in length, 2 cm in width, and 1 cm thick. The ovarian ligament, also known as mesovarium, attaches the ovaries to the upper part. They are also connected to the fallopian tubes via a deep tissue called the infundibulopelvic.
The capsule surrounds the ovary and encloses an inner medulla and an outer cortex. Tunica albuginea, a fibrous connective tissue, is the capsule.
- Medulla: The Medulla is located in the middle of an ovary. It consists of blood vessels and fibrous tissue as well as nerves. Reptiles and amphibians have an ovarian medulla that is not filled with lymph.
- Cortex: The Cortex surrounds the Medusa. It is made up of a fibrous tissue, stroma, and germinal epithelium. It is home to ovarian follicles at different stages of their development, as well as an ovum. Follicular cells are epithelial cells that have been flattened from the germinal epithelium around the ovary.
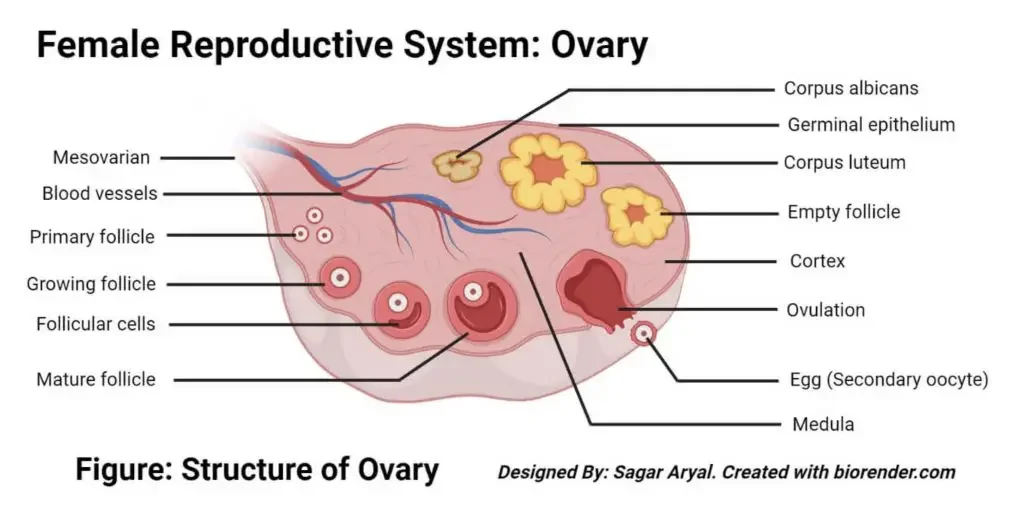
Function of ovaries
Two functions serve the ovaries.
- Gamete production: The ovaries are where the egg cell and female gamete are periodically developed and released by ovulation. The fluid-filled follicles are where the egg cells mature. Only one egg cell can be released at a time. But, multiple cells can mature simultaneously.
- Hormone secretion: The ovaries secrete a number of hormones, including estrogen, testosterone and progesterone. These hormones are responsible for secondary sexual characteristics development and maintaining the reproductive function.
Uterine tubes (Fallopian tubes)
The uterine tubes (also known as oviducts) are a part of the female reproductive systems that transport ova from the egg to the uterus every month. These tubes carry the fertilized egg from the ovary to the uterus for fertilization.
Structure of uterine tubes
Each uterine tube measures between 10-13 cm in length and has a diameter of 1-2 cm that extends laterally from its superior end.
The Uterine tube is made up of four parts.
- Infundibulum, a funnel-shaped structure, opens into the peritoneum in abdominal Ostia. It is often found with associated fimbriae, which are mucosal projections that look like fingernails. These fimbriae project over the ovaries and are the longest, called ovarian fimbriae. They attach to the superior side of the ovum.
- The longest tube part is the ampulla, measuring 5cm in length. This lumen has a thin wall and a folded luminal surface. Fertilization takes place in it.
- The tube’s narrower end that extends towards your uterus is called the isthmus.
- The intramural (interstitial), part that crosses the myometrium.
A layer of mucous membrane is folded into papillae surrounds the channel. The inner layer is simple columnar epithelium and contains cells with tiny hair-like structures known as cilia. Between the ciliated cells is a layer of peg cells, which secrete a fluid that provides nutrients to spermatozoa and oocytes as well as zygotes.
Functions of uterine tubes
- Urinary tubes are designed to transport ovum from ovary to uterus. This is made possible by the peristaltic movements of the muscles and rhythmic movement in the ciliated cell.
- The spermatozoa move through the tube to fertilize the eggs. Fertilization usually takes place in the ampulla. The tubes’ secretions provide nutrients for the zygote after fertilization.
Uterus
The female reproductive system’s hollow, muscular pear-shaped uterus is narrow at the anterior and posterior.
Structure of uterus
- It is located between the rectum and the urinary bladder. The uterus is about 7.5cm in length, 5cm wide, 2.5cm thick, and weighs approximately 30-40g in an adult female.
- The wall of your uterus is composed of three layers: Perimetrium myometrium, endometrium, and the third layer.
- The outermost layer of the female uterus, the perimetrium, is folded anteriorly into the vesicouterine bag. It extends posteriorly from the uterus to create the rectouterine pouch.
- The middle layer of the uterine wall is called myometrium. It is composed of connective tissues, smooth muscles and blood vessels.
- The endometrium, the innermost layer of the body, is made up of columnar epithelium and a large number mucus-secreting tubular cells.
- The endometrium can be further divided into its layers, with the top layer thickening during the first half. The myometrium is surrounded by the basal layer. The basal layer, which is the upper layer of the endometrium, is lost during menstruation.
- Externally, there are three parts to the uterus: the fundus (the body), the cervix (the cervix), and the corpus (the fundus). The dome-shaped fundus is located above the opening for the tubes. The main part of the body is the uterus and is connected to its cervix. Through the anterior wall, the vaginal wall, the cervix (or ‘the neck” of the uterus) protrudes from the cervix.
Functions of uterus
- The primary function of the uterus, is to provide a safe environment for a baby’s development.
- Uterine secretions supply nourishment to the ovum prior to its implantation on the wall. Later, after fertilization the rapidly expanding ball cells are nourished with endometrial cells.
- After puberty in the male, the uterus experiences periodic shedding. This is known as the menstrual cycle. This shedding helps prepare the uterus for fertilization and protection.
Vagina
The vagina, a fibromuscular tube with a stratified squamous epithelium, connects the female reproductive system’s internal and external organs. The vagina is positioned obliquely upwards, with the bladder in front and the rectum and anus in behind.
Structure of the vagina
- Three layers surround the vagina: the outer layer is made of areolar tissue and the middle layer is made of smooth muscle. The inner layer contains stratified squamous epithelium, which forms ridges and rugae.
- The secretory cells in the vagina are not present; however, cervical secretions keep the surface moist.
- Lactobacillus Acidophilus can be found in vaginal tissue between puberty, menopause and adulthood. This organism secretes lactobacillus acidophilus, which maintains the vaginal pH between 4.9 and 3.7. This acidity prevents other microorganisms from reaching the vagina via the perineum.
Functions of vagina
- During coitus or sexual reproduction, the vagina acts as the receptor for the penis.
- During childbirth, the vagina provides a flexible passageway for the baby.
Hormones involved in the female reproductive system
Gonadotropic hormone (GnRH), hypothalamic hormone releasing hormone: This hormone stimulates anterior pituitary to produce sex hormones Follicle Stimulating hormone (FSH) & Luteinizing hormone (LH).
- FSH and LH: FSH and LH are hormones that stimulate the production of estrogen and progesterone in the ovary. They also promote the growth of follicles along the wall of the ovary.
- Estrogen hormone: This hormone promotes the growth of egg follicles, and aids in the maintenance and development female characteristics in the body.
- Progesterone hormone: The hormone progesterone regulates the endometrium (internal lining) of the uterus. It also helps in the release and maintenance of eggs during ovulation.
Physiology of Female Reproductive System
The lumen of the reproductive tract, also known as the genital tract, is the one that begins in the vagina and splits into two lumens. These lumens then continue through the Fallopian tubes and end at the distalostia, which opens into the abdominal cavity.
The ovum will eventually travel the entire reproductive tract, from the fallopian tube to the end of the vaginal canal, if there is no fertilization.
Transluminal procedures can use the reproductive tract for a variety of purposes, including fertiloscopy and intrauterine injections.
Development of Female Reproductive System
The chromosome characteristics of a fetus determine its genetic sex at conception. This is determined primarily on the 23rd pair chromosomes that are inherited. The sex of the fetus is determined by the male, as the egg contains an Xchromosome and the sperm from the father either an Xchromosome or a Ychromosome. The fetus that inherits the X-chromosome from its father will be a girl. This will mean that testosterone will not be made, and the Wolffian conduit will become ineffective. The Mullerian duct, however, will eventually develop into female sex. The Wolffian remnants are called the clitoris. The Y chromosome will make the fetus a male if it is passed on from the father. The Wolffian gland will be stimulated by testosterone, which will result in the development of male sex organs. However, the Mullerian drain will become less effective.
Some Clinical significance of Female Reproductive System
1. Vaginitis
Vaginal inflammation is a condition that causes inflammation and can be caused by infection. This is the most common gynaecological condition. Vaginitis is difficult to diagnose because the organisms involved vary in age, sexual activity and method of microbial identification. As there are many infectious agents who make use of close proximity to mucous membranes or secretions, vaginitis does not always result from a sexually transmitted disease. Vaginal discharge is the most common way to diagnose vaginitis. This can be of a particular color, smell, or quality.
2. Bacterial vaginosis
This is a female vaginal infection. This is different from vaginitis because there is no inflammation. Bacterial Vaginosis is multimicrobial and includes many species of bacteria. If three of the following criteria are present, bacterial vaginosis can be diagnosed: (1) Homogenous, thin drainage, (2) pH of 4.5 within the vagina, (3) epithelial cell in the vagina with bacteria attached, or (4) fishy odor. This has been linked to an increased risk of developing other genital tract infections, such as endometritis.
3. Yeast infection
This is a common cause for vaginal irritation and 75% of women who have had it at least once in their lives, according to the Centers for Disease Control and Prevention. Candida overgrowth in the vagina can cause yeast infections. Acidic vaginal pH is the most common cause of yeast infections. Other factors like pregnancy, diabetes, weak immune systems, tight clothing or douching may also contribute to yeast infections. Itching, burning, irritation and white cottage cheese-like vaginal discharge are all symptoms of yeast infections. Some women also report painful intercourse or urination. A yeast infection can be diagnosed by taking a sample from the vaginal secretions, and placing it under a microscope to see if there is any evidence. There are many options for treatment, from creams that can apply to the area or oral tablets that will stop the growth of yeast.
4. Genital mutilation
Many cultures have different ways of mutilating females’ genitalia. There are two main types of genital abuse: clitoridectomy and circumcision of clitoris. The prepuce is the skin surrounding the clitoris. All of them can have serious health consequences, including bleeding, tissue damage irreparable, and sepsis, which can sometimes prove fatal.
5. Genital surgery
Genitoplasty is a type of surgery that repairs damaged sex organs, especially after cancer treatment. You can also opt for elective procedures to change the external appearance of your genitals.
6. Birth control
Females have many options for birth control. There are two types of birth control: hormonal and physical. Oral contraception is a way to manage various medical conditions such as menorrhagia. Oral contraceptives can cause depression, among other side effects.
How Does the Female Reproductive System Work?
A woman’s reproductive system allows her to:
- produce eggs (ova)
- have sexual intercourse
- protect and nourish a fertilized egg until it is fully developed
- give birth
The gonads are the sexual organs that allow for sexual reproduction. The gonads are often thought of as the male testicles. Both sexes have the gonads. In females, the gonads (or ovaries) are responsible for making female eggs. Male gonads are responsible for making male gametes (sperm).
A baby girl’s ovaries are filled with hundreds of thousands of eggs. These eggs remain inactive until puberty. The pituitary gland, located in the central part of your brain, starts to produce hormones that stimulate the production of female sex hormones. These hormones are responsible for a girl becoming a mature sexually.
Girls begin to release eggs towards the end of puberty as part of their monthly period, the menstrual cycle. An ovary releases a small egg about once per month during ovulation.
The egg will leave the body approximately 2 weeks after it is fertilized by the sperm in the fallopian tubes. This is called menstruation. The menstrual cycle is formed when blood and tissue from the inner lining combine to form the menstrual flow. It lasts for most girls between 3 to 5 days. Menarche is the first period for a girl.
Both girls and women often feel discomfort during the days before their period. Premenstrual syndrome (PMS), which can be both physical and emotionally distressing, is something many women and girls experience right before they have periods.
- acne
- bloating
- tiredness
- backaches
- sore breasts
- headaches
- constipation
- diarrhea
- food cravings
- depression
- irritability
- trouble concentrating or handling stress
PMS usually occurs 7 days before a girl has her period and then disappears once it starts.
Prostaglandins are chemicals that cause the smooth muscles in the uterus to contract. Many girls experience belly cramps in the first few days after their period. These involuntary contractions may be either dull or intense.
A girl’s body can take up 2 years to establish a regular menstrual cycle. Her body adjusts to the hormonal changes that puberty brings. The average monthly cycle of an adult woman lasts 28 days. However, it can vary from 23 to 35 days.
What Happens If an Egg Is Fertilized?
Fertilization can occur if a male and a female sex within a few days of each other’s ovulation. A small amount of the semen is released into the vagina when the male ejaculates, which is when the penis releases its semen. Millions upon millions of sperm reside in this tiny amount of semen. They “swim up” from the vagina through uterus and cervix to reach the egg in the fallopian tubes. To fertilize an egg, it takes one sperm.
The fertilized egg (pronounced: Zygote) is a multicelled blastocyst that forms about 5-6 days after the sperm fertilizes it. A blastocyst, pronounced BLAS-tuh’sist, is about the same size as a pinhead and is a hollow ball of cells that has fluid inside. The blastocyst burrows into the lining and uterus of the uterus. Endometrium, pronounced en-dohm-EE-tree um, is a thickened and rich in blood by the hormone estrogen. Another hormone, progesterone, is released by the ovaries. It keeps the endometrium rich in blood so that the blastocyst may attach to the uterus and take nutrients from it. This is known as implantation.
The blastocyst cells begin to take in nutrients, and another stage of development is underway. The embryonic stage is when the inner cells create a flattened, circular shape known as the embryonic disc, which will eventually become a baby. The baby’s outer cells are covered by thin membranes made of the cell membranes. The cells multiply many times and then move to new positions, eventually becoming the embryo (pronounced: EMBREE-oh).
The embryo will be about the same size as a raspberry after 8 weeks. However, almost all its parts, including the brain, nerves, heart and blood, stomach and intestines, muscles and skin, have formed by then.
The fetal stage is the time when cells continue to develop and move. It lasts approximately 9 weeks from fertilization until birth. The amniotic fluid (pronounced am-neeAH-tik) surrounds the amniotic sac and floats within it. The placenta, which is pronounced pluh-SENtuh, provides oxygen and nutrition to the fetus from the mother’s milk. This disc-shaped structure attaches to the uterine lining and connects to it via the umbilical cord (pronounced: umBIL-ih kul). The membrane and amniotic fluid cushion the fetus from bumps and provide jolts for the mother’s body.
On average, pregnancy lasts 280 days. That’s about nine months. When the baby is ready to give birth, it presses its head on the cervix. The cervix begins to relax and expand to prepare for the baby’s passage into and through the vagina. Mucus had clogged the cervix and now it is loose. When the mother gives up her water, it and the amniotic fluid escape through the vagina.
The contractions of labor cause the walls of the uterus to contract when they are stimulated with the pituitary hormone, oxytocin (pronounced: AHK-see-TOEsin). The contractions cause the cervical area to expand and then to open. After several hours, the cervix has dilated enough to allow the baby through. The baby is then pushed out of the uterus through the cervix and into the birth canal. The baby’s head is usually the first to go. The baby’s umbilical cord is removed with it. After the baby is born, the umbilical cord is clamped and then cut near the navel.
The delivery of the placenta is the last stage in the birth process. This is known as the afterbirth. Once it is separated from the uterine lining, the contractions push it out along with its fluids and membranes.
What happens during the menstrual cycle?
Women of reproductive age, which can be between 11 and 16 years old, experience hormonal activity cycles that last approximately one month. Menstruation is a term that means “monthly”, which leads to the term menstrual cycles. Every cycle prepares a woman for pregnancy. Menstruation is the term for the periodic shedding or tearing of the uterine membrane. Women often refer to the periods or cycles that occur when they experience vaginal bleeding as their “period,” “menstrual”, or “cycle.”
On average, the menstrual cycle lasts 28 days. It is divided into phases. These phases are:
- The follicular phase (development of the egg)
- The ovulatory phase (release of the egg)
- The luteal phase (hormone levels decrease if the egg does not implant)
The menstrual cycle is governed by four hormones, which are chemicals that regulate or stimulate the activity of cells and organs. These hormones are:
- Follicle-stimulating hormone
- Luteinizing hormone
- Estrogen
- Progesterone
Follicular phase
This phase begins on the first day after your period. The following events take place during the follicular stage of your menstrual cycle:
- Two hormones, the follicle stimulating hormone and the luteinizinghormone (LH), are released by the brain and travel through the blood to reach the ovaries.
- Hormones stimulate the growth and development of approximately 15 to 20 eggs within the ovaries. Each egg is called a “shell” or a follicle.
- These hormones (FSH, LH) can also increase the production of estrogen in women.
- The production of follicle stimulating hormone is shut down when estrogen levels rise. It acts like a switch. The body can regulate the amount of hormones needed to prepare eggs for release by balancing the hormones.
- As the follicular stage progresses, one dominant follicle becomes dominant in each ovary and continues to mature. The dominant follicle will suppress all the rest of the follicles. They stop growing and eventually die. The estrogen-producing dominant follicle still produces estrogen.
Ovulatory phase
The ovulatory (or ovulation phase) begins approximately 14 days after the follicular phases ended. However, this can vary. The ovulatory period falls between the luteal and follicular phases. The majority of women will experience a menstrual period between 10 and 16 days after ovulation. The following events can occur during this period:
- The brain produces more luteinizing hormone when there is an increase in estrogen in the dominant follicle.
- This causes the dominant foollicle to release its eggs from the ovary.
- The fimbriae project finger-like projections onto the ends of the fallopian tubes to capture the egg as it is released (a process known as ovulation). The egg is swept into the tube by the fimbriae.
- Many women will notice an increase of egg white cervical mucus for one to five days before ovulation. This is the vaginal mucus that helps to capture and nourish the sperm as it travels to fertilization.
Luteal phase
The luteal phase starts right after ovulation. It involves the following processes:
- After it has released its egg, the empty Ovarian Follicle forms into a new structure known as the Corpus Lutum.
- The hormones estrogen, progesterone and sperm are secreted by the corpus luteum. Progesterone prepares your uterus to allow a fertilized egg and implant.
- If intercourse took place and a man’s fertilized egg (a process known as conception) travels through the fallopian tube to implant itself in the uterus. Now, the woman is considered to be pregnant.
- The egg will not be fertilized if it isn’t fertilized. The uterine lining does not need to be fertilized. It then breaks down and is shed.
How many eggs does a woman have?
There are approximately 6 million to 7 millions eggs during fetal life. No new eggs are made after this point. There are about 1 million eggs at birth. By the time you reach puberty, it will be down to 300,000. Only 300 to 400 of these eggs will be fertilized during a woman’s reproductive life. As a woman gets older, her fertility can decline due to a decrease in the number and quality eggs.
Human Female Reproductive System Diagram
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.