What is Digestive System?
- Cell lines, essential tools in biological research and biomedical applications, are established from human, animal, or plant cells. These lines provide a controlled environment for studying cellular functions, genetic modifications, drug responses, and disease mechanisms. Characterizing cell lines involves assessing their biological, morphological, and genetic properties, which is crucial for ensuring the reliability and reproducibility of experimental outcomes.
- The initial step in the characterization of a cell line is morphological analysis. This involves observing the shape, size, and growth patterns of the cells under a microscope. Morphological characteristics can provide insights into the cell line’s identity and differentiation status. For instance, epithelial cells typically exhibit a polygonal shape, while fibroblasts may appear more elongated. Consistency in these morphological features is vital for confirming the authenticity of a cell line.
- Next, growth characteristics are evaluated. This includes assessing the cell line’s doubling time, which indicates how quickly the cells replicate. The growth rate can vary significantly among different cell lines, influencing experimental timelines and conditions. Furthermore, the capacity for anchorage dependence or independence is assessed. Anchorage-dependent cells require attachment to a surface for proliferation, whereas anchorage-independent cells can grow in suspension. Understanding these growth characteristics is essential for determining the appropriate culture conditions.
- Another critical aspect of cell line characterization is the assessment of metabolic activity. This can be measured using assays that determine cellular respiration and viability. The metabolic profile reflects the cell line’s functional state and can indicate responses to drugs or environmental changes. Metabolic assays, such as the MTT assay, provide quantitative data on cell viability, allowing researchers to evaluate the cytotoxicity of various compounds.
- Genetic characterization is equally important in cell line analysis. Techniques such as karyotyping, DNA sequencing, and genotyping help identify genetic abnormalities or mutations present in the cell line. For example, cancer cell lines often exhibit chromosomal abnormalities that contribute to their malignant properties. Furthermore, the expression of specific genes or proteins can be analyzed through methods like Western blotting or quantitative PCR (qPCR). This genetic profiling informs researchers about the lineage and potential applications of the cell line in various studies.
- Moreover, immunophenotyping, a technique that identifies specific cell surface markers, is employed to further characterize cell lines. Flow cytometry is commonly used for this purpose, allowing the identification of distinct cell populations based on their surface marker expression. This is particularly useful in the characterization of hematopoietic cell lines, where specific markers indicate lineage and differentiation status.
- In addition to these primary characteristics, researchers must also assess the stability and reproducibility of cell lines over time. Continuous culture of a cell line can lead to genetic drift or phenotypic changes that may alter its properties. Therefore, periodic characterization is necessary to ensure that the cell line remains true to its original characteristics. Authentication methods, such as short tandem repeat (STR) profiling, provide a reliable means of verifying cell line identity and preventing cross-contamination.
How Does the Digestive System Work?
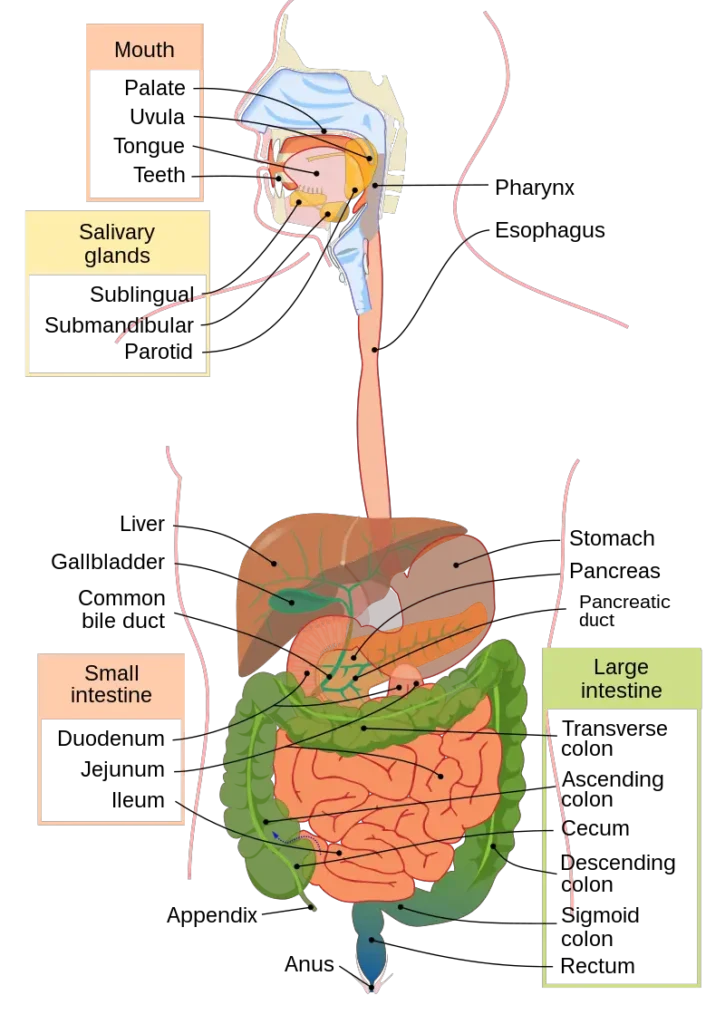
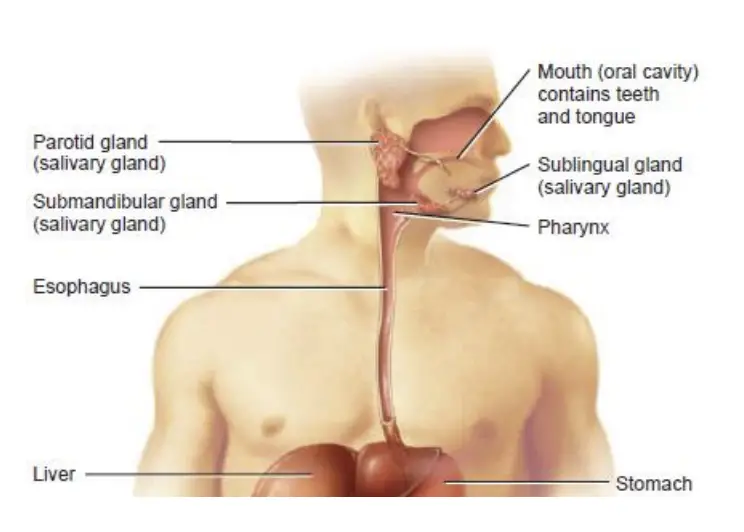
- The digestive system is a complex network of organs and tissues that work together to break down food and absorb nutrients for the body’s growth, energy, and maintenance. It consists of the gastrointestinal (GI) tract and various glands, including the tongue, salivary glands, liver, gall bladder, and pancreas.
- The GI tract, a long tube of varying diameter, begins at the mouth and ends in the anus. The process of digestion can be divided into three stages based on the position of food within the digestive tract: the oral phase, the gastric phase, and the intestinal phase.
- The oral phase, also known as the mouth phase, is where digestion begins. It starts with the process of chewing and mixing food with saliva. The tongue helps move the food around the mouth, while the salivary glands secrete saliva that contains enzymes, such as amylase, which begins the breakdown of carbohydrates. The food then forms a small, soft mass called a bolus, which is ready to be swallowed.
- Swallowing triggers the next phase of digestion, the gastric phase. The food bolus enters the stomach, where it is further broken down by stomach acid and digestive enzymes. The stomach muscles churn and mix the food, creating a semi-liquid mixture called chyme. The gastric phase primarily focuses on the breakdown of proteins with the help of the enzyme pepsin.
- From the stomach, the partially digested chyme enters the small intestine, marking the beginning of the intestinal phase. The small intestine is where most of the digestion and absorption of nutrients occur. The chyme mixes with digestive enzymes from the pancreas and bile from the liver and gall bladder. The pancreas releases enzymes that break down proteins, fats, and carbohydrates, while bile emulsifies fats for better digestion. The small intestine has specialized structures called villi and microvilli, which increase the surface area for nutrient absorption. Nutrients, such as amino acids, glucose, vitamins, and minerals, are absorbed into the bloodstream and transported to various parts of the body for use.
- After the small intestine, any remaining waste material moves into the large intestine, or colon. The colon absorbs water and electrolytes from the waste, forming solid stool. The waste is then eliminated from the body through the rectum and anus in the process of defecation.
- It is worth noting that the digestive system begins to develop early in the human body, starting around the third week after fertilization. The primitive gut forms through invaginations of embryonic cells, extending from the buccopharyngeal membrane to the cloacal membrane. The mouth forms when the buccopharyngeal membrane breaks down, allowing the digestive tract to open to amniotic fluid. Throughout fetal development, the amniotic fluid is actively swallowed, preparing the digestive system for its crucial role after birth.
- In summary, the digestive system is a remarkable mechanism that enables the body to break down food, extract nutrients, and eliminate waste. It involves the coordinated effort of various organs, glands, and enzymes throughout the GI tract. Understanding how the digestive system works can help us make informed choices about our diet, maintain our health, and support overall well-being.
Types of Digestive System
The digestive system can be categorized into two primary components: the gastrointestinal (GI) tract and the accessory digestive organs. Understanding these components is essential for comprehending how the body processes food and absorbs nutrients. Each part plays a distinct role in digestion, ensuring the body receives the necessary nourishment.
- Gastrointestinal (GI) Tract:
- The GI tract, also known as the alimentary canal, is a continuous tube that spans from the mouth to the anus. Its primary function is to facilitate the mechanical and chemical breakdown of food, allowing for nutrient absorption.
- Components of the GI Tract:
- Mouth: The digestive process begins here, where teeth break down food into smaller pieces through chewing. Saliva, produced by the salivary glands, moistens food, making it easier to swallow.
- Pharynx: This muscular passage connects the mouth to the esophagus and serves as a pathway for food. It plays a critical role in swallowing, guiding food toward the esophagus.
- Esophagus: A muscular tube that transports food from the pharynx to the stomach. Peristaltic movements in the esophagus push the food downward.
- Stomach: A muscular sac that stores and further breaks down food. It produces gastric acid and digestive enzymes that contribute to the chemical digestion of food.
- Small Intestine: A long, coiled tube where the majority of digestion and nutrient absorption occurs. Enzymes from both the pancreas and the small intestine break down food into smaller molecules, which are then absorbed into the bloodstream.
- Large Intestine: Also known as the colon, this organ absorbs water and electrolytes from the remaining undigested material. It plays a significant role in forming and storing waste products until elimination.
- Rectum: The final part of the large intestine, it temporarily stores waste before it is expelled from the body through the anus.
- Anus: The opening at the end of the digestive tract, it regulates the expulsion of waste from the body.
- Accessory Digestive Organs:
- These organs assist in the digestion of food but do not come into direct contact with it. They produce secretions that facilitate the chemical breakdown of food, making the digestive process more efficient.
- Components of Accessory Digestive Organs:
- Teeth: Essential for the mechanical breakdown of food, they chew and grind food into smaller particles, increasing the surface area for enzymatic action.
- Tongue: A muscular organ that aids in chewing and swallowing. It helps mix food with saliva, forming a bolus that is easier to swallow.
- Salivary Glands: These glands secrete saliva, which contains enzymes that initiate the digestion of carbohydrates. Saliva also moistens food, aiding in the swallowing process.
- Liver: Produces bile, a substance crucial for the emulsification and digestion of fats. The liver also plays a vital role in metabolism and detoxification.
- Gallbladder: Stores bile produced by the liver until it is needed for digestion. During meals, the gallbladder releases bile into the small intestine to aid in fat digestion.
- Pancreas: Produces digestive enzymes that break down carbohydrates, proteins, and fats. It also secretes bicarbonate to neutralize stomach acid in the small intestine, creating an optimal environment for enzymatic activity.
Layers of the GI Tract
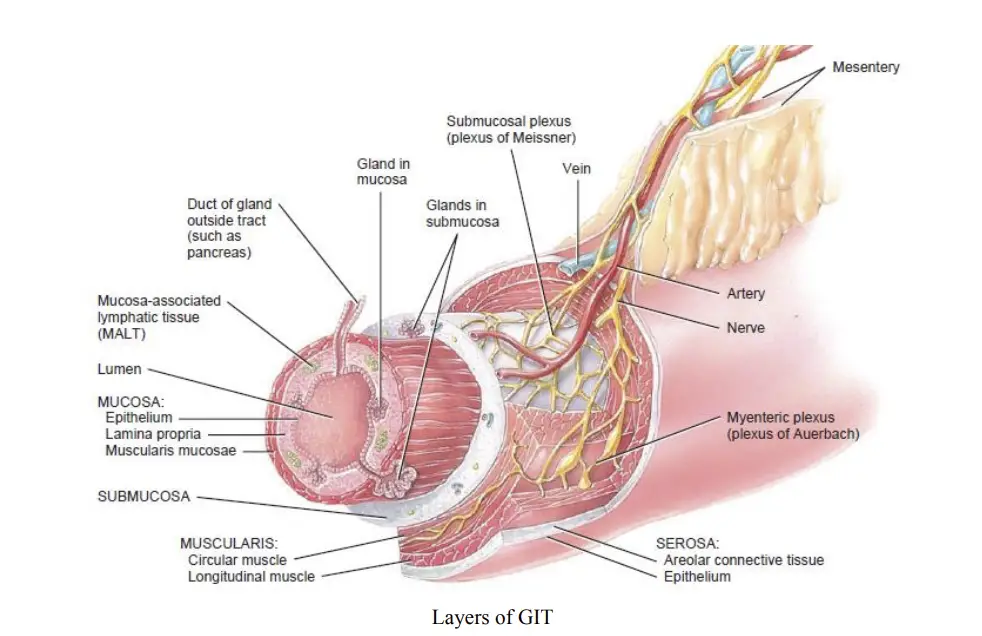
The gastrointestinal (GI) tract is composed of four distinct layers, each serving specific functions crucial for digestion and nutrient absorption. Understanding these layers provides insight into how the GI tract operates and maintains homeostasis. The four layers, from deep to superficial, are the mucosa, submucosa, muscularis, and serosa.
- Mucosa:
- The mucosa is the innermost lining of the GI tract and is essential for various functions such as protection, secretion, and absorption. It is further subdivided into three layers:
- Epithelium: This layer may consist of simple or stratified epithelial cells that play a critical role in protecting the underlying tissues. Additionally, these cells secrete mucus and fluids into the lumen of the tract, aiding in the digestive process.
- Lamina Propria: Composed of areolar connective tissue, the lamina propria houses numerous blood and lymphatic vessels that facilitate the transfer of absorbed nutrients to other tissues throughout the body. It also contains mucosa-associated lymphatic tissue (MALT), which houses immune cells that protect against pathogens.
- Muscularis Mucosae: This is a thin layer of smooth muscle fibers that enhance the surface area of the stomach and small intestine through various folds. This increase in surface area significantly improves digestion and absorption efficiency.
- The mucosa is the innermost lining of the GI tract and is essential for various functions such as protection, secretion, and absorption. It is further subdivided into three layers:
- Submucosa:
- The submucosa is a layer of areolar connective tissue that binds the mucosa to the muscularis layer. It contains a network of blood and lymphatic vessels that receive absorbed food molecules. Additionally, the submucosa houses an extensive network of neurons known as the submucosal plexus (or plexus of Meissner), which is a part of the enteric nervous system (ENS). This network is crucial for regulating digestive functions.
- Muscularis:
- The muscularis layer consists of both skeletal and smooth muscle fibers. Skeletal muscles are responsible for voluntary actions, such as swallowing and defecation. In contrast, the involuntary contractions of smooth muscle are vital for breaking down food, mixing it with digestive secretions, and propelling it through the tract. This layer also contains the myenteric plexus, a bundle of neurons that coordinates peristalsis and other movements within the GI tract.
- Serosa:
- The serosa forms the outermost layer of the GI tract and consists of protective connective tissue. This layer envelops the GI organs, providing support and protection as they are suspended within the abdominopelvic cavity.
- Peritoneum:
- The peritoneum is the largest serous membrane in the body. It is divided into two parts: the parietal peritoneum, which lines the walls of the abdominopelvic cavity, and the visceral peritoneum, which covers the organs within the cavity, serving as their serosa.
Organs of Human Digestive System
1. Mouth
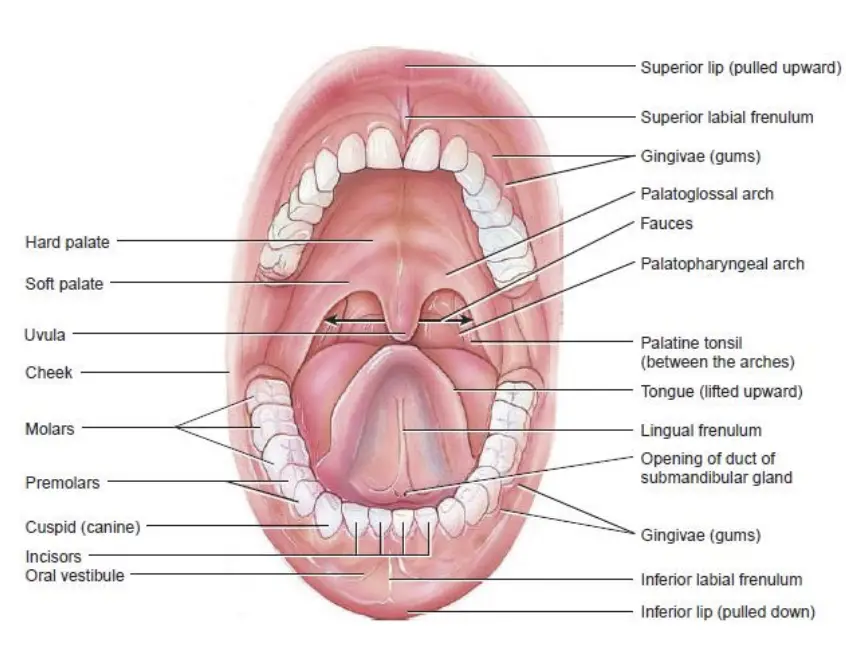
The mouth, also known as the oral cavity or buccal cavity, serves as the entry point for food and plays a crucial role in the digestive process. This complex structure is formed by various components, including the cheeks, hard palate, soft palate, and tongue.
- Structure of the Mouth:
- The cheeks form the lateral walls of the mouth and are composed of skin on the outside and a mucous membrane on the inside. This configuration aids in the overall function of the mouth, particularly in food manipulation.
- The hard palate constitutes the anterior portion of the roof of the mouth. It is made up of palatine and maxillae bones and is covered by a mucous membrane. The hard palate serves as a bony partition between the oral cavity and the nasal cavity, facilitating the separation of food from the respiratory tract.
- The soft palate makes up the posterior portion of the roof of the mouth and is also covered with a mucous membrane. It plays a vital role in separating the oropharynx from the nasopharynx during swallowing.
- The uvula, a small muscular process hanging from the soft palate, prevents the entrance of swallowed food and liquids into the nasal cavity, thus directing them towards the esophagus.
- Parts of the Mouth:
- The human mouth consists of two main parts:
- Vestibule: This is a slit-like space bounded externally by the lips and cheeks and internally by the gums and teeth. It serves as an area for food collection and initial manipulation.
- Oral Cavity (Buccal Cavity): This is the inner portion of the mouth and includes several components:
- Palate: The roof of the oral cavity, with the anterior part (hard palate) featuring transverse ridges called rugae. The posterior part (soft palate) is smooth and is marked by the uvula.
- Tongue: Attached to the floor of the mouth by the lingual frenulum, the tongue is divided into two parts by the sulcus terminalis—an anterior oral part and a posterior pharyngeal part. The apex of the sulcus terminalis is marked by the foramen caecum.
- The human mouth consists of two main parts:
2. Salivary Glands
Salivary glands are vital structures within the oral cavity that release saliva, a secretion essential for various functions in the digestive process. The primary role of saliva is to keep the mucous membranes of the mouth and pharynx moist, to cleanse the mouth and teeth, and to facilitate the initial stages of digestion when food enters the mouth. Salivation increases upon food intake, leading to the lubrication, dissolution, and chemical breakdown of food.
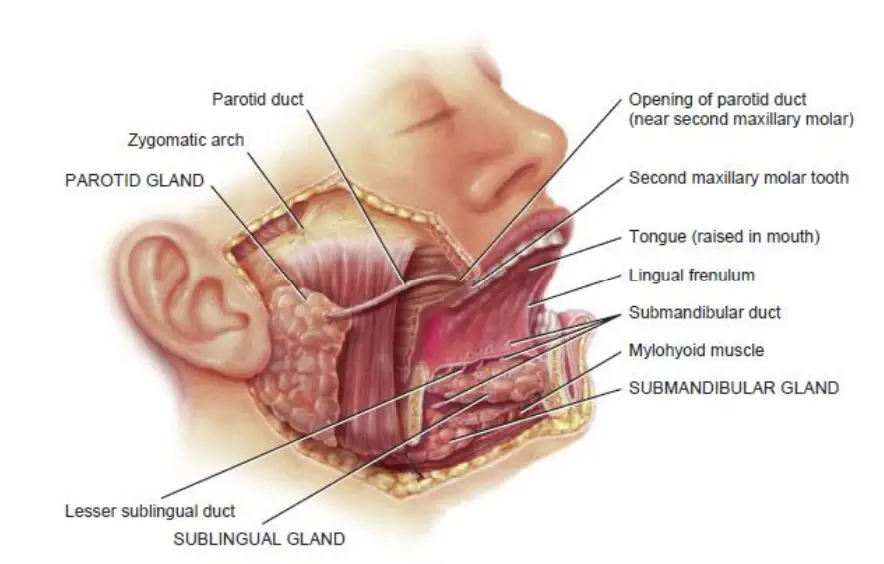
- Major Salivary Glands: The human body has three pairs of major salivary glands that contribute significantly to saliva production:
- Parotid Glands: Located near the ears, these glands are the largest of the salivary glands. They secrete saliva into the oral cavity via the parotid duct, which opens into the vestibule opposite the second upper molar tooth. The secretion from the parotid glands contains a higher amount of serous fluid than mucus.
- Submandibular Glands: Found in the floor of the mouth below the lower jaw, these glands have ducts that open into the oral cavity, lateral to the lingual frenulum. Their secretions contain both serous and mucus components.
- Sublingual Glands: The smallest of the major salivary glands, the sublingual glands are located beneath the tongue and above the submandibular glands. They primarily secrete mucus through their ducts that open into the floor of the mouth.
- Minor Salivary Glands: In addition to the major glands, several minor salivary glands are distributed throughout the cheeks, palates, tongue, and lips, producing smaller amounts of saliva.
- Process of Salivation: The secretion of saliva is a continuous process influenced by reflexes triggered by the presence of food.
- Composition of Saliva: Saliva is primarily composed of 99.5% water and 0.5% solutes, which include:
- Ions: Chloride, sodium, potassium, bicarbonate, and phosphate ions.
- Organic Substances: Saliva contains urea, uric acid, mucus, immunoglobulin A (IgA), lysozyme (a bacteriolytic enzyme), and salivary amylase.
- Functions of Saliva:
- Digestion: Salivary amylase is a carbohydrate-digesting enzyme that initiates the breakdown of polysaccharides into monosaccharides in the mouth.
- Lubrication: Mucus in saliva moistens food particles, facilitating swallowing by holding the food together and providing lubrication.
- Antibacterial Action: Lysozymes in saliva exhibit antibacterial properties, destroying certain bacteria by breaking down their cell walls.
- Taste Detection: Saliva serves as a solvent, allowing taste buds to detect flavors by dissolving food particles.
- Moisture Maintenance: Saliva keeps the mouth moist, which aids in speech and overall oral comfort.
- Cleaning Action: Saliva contributes to the cleanliness of the mouth and teeth, helping to wash away food particles and debris.
- pH Regulation: Rich in bicarbonates, saliva neutralizes acids from food and those produced by bacteria in the mouth, thereby helping to prevent dental caries.
3. Tongue
The tongue is a crucial accessory digestive organ comprised of skeletal muscle and covered with a mucous membrane. It plays essential roles in tasting, swallowing, and speaking, serving multiple functions in the oral cavity. The tongue’s structure and associated muscles form the floor of the mouth, highlighting its significance in various physiological processes.
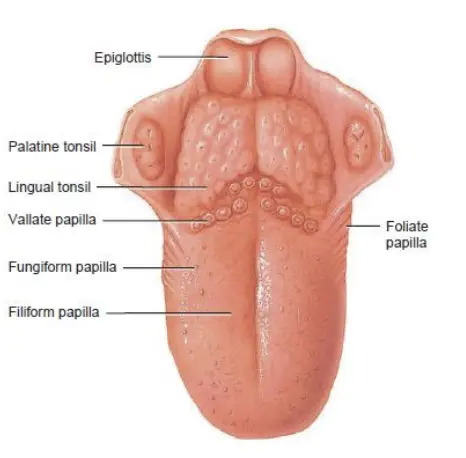
- Structure of the Tongue:
- The tongue is divided into two symmetrical lateral parts by a median septum that runs the entire length of the organ.
- It consists of two primary types of muscles:
- Extrinsic Muscles: These muscles facilitate the movement of the tongue from side to side and in and out. They are responsible for maneuvering food during chewing, shaping food into a rounded mass, and propelling food to the back of the mouth for swallowing. Additionally, these muscles form the floor of the mouth and help maintain the tongue’s position.
- Intrinsic Muscles: These muscles allow for alterations in the shape and size of the tongue, which are essential for speech and swallowing.
- Lingual Frenulum:
- A fold of mucous membrane known as the lingual frenulum attaches the tongue to the floor of the mouth. This structure controls the posterior movement of the tongue, ensuring it remains in a functional position during various activities such as eating and speaking.
- Surface Structure:
- The upper surface and lateral surfaces of the tongue are covered with structures called papillae.
- Many of these papillae contain taste buds, which are specialized receptors responsible for gustation (the sense of taste).
- Some papillae lack taste buds; however, they contain receptors for touch and serve to increase friction between the tongue and food. This increased friction aids the tongue in effectively maneuvering food within the oral cavity.
- Lingual Glands:
- The tongue contains lingual glands that secrete mucus and a fluid rich in the enzyme lingual lipase.
- Lingual lipase plays a significant role in the breakdown of triglycerides, initiating the digestion of fats even before they reach the stomach.
4. Teeth
Teeth, or dentes, serve as vital accessory digestive organs responsible for cutting, tearing, and pulverizing solid food, thereby reducing it into smaller, manageable particles for easier swallowing and digestion. Positioned in the alveolar processes of the mandible and maxillae, teeth play a crucial role in the digestive system.
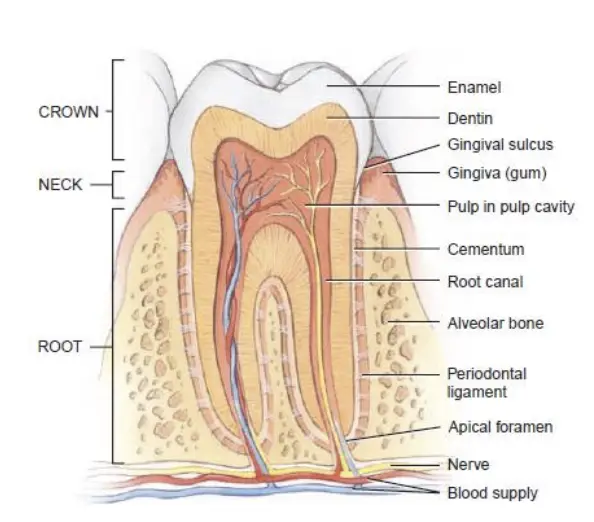
- Anatomy of Teeth:
- Alveolar Processes and Gingivae: The alveolar processes house the teeth, and these processes are covered by gingivae, commonly known as gums. The gums extend into each socket where the teeth reside.
- Periodontal Ligaments: Each socket is lined with periodontal ligaments, which are composed of dense fibrous connective tissue. These ligaments anchor the teeth securely within their sockets.
- Parts of a Tooth:
- Crown: This is the visible portion of the tooth that extends above the gum line.
- Root: The root comprises the part of the tooth embedded within the socket.
- Neck: The neck is the constricted region located at the junction of the crown and root, near the gum line.
- Internal Structure:
- Dentin: Dentin forms the majority of the tooth, providing its basic shape and rigidity. It is harder than bone due to a higher concentration of calcium salts.
- Enamel: The crown’s dentin is covered by enamel, which is primarily composed of calcium phosphate and calcium carbonate. Enamel is the hardest substance in the human body, containing about 95% calcium salts in its dry weight. Its primary function is to protect the tooth from the wear and tear associated with chewing, as well as to shield against acids that can dissolve dentin.
- Cementum: The root’s dentin is covered by cementum, a bone-like substance that connects the root to the periodontal ligament, facilitating stability within the socket.
- Pulp Cavity:
- The dentin encases a space known as the pulp cavity. This cavity contains blood vessels, nerves, and lymphatic vessels, which are essential for the tooth’s health.
- Root Canals: Narrow extensions of the pulp cavity, called root canals, extend through the tooth’s root. Each root canal has an opening at its base, termed the apical foramen.
- Function of Blood Vessels and Nerves: Blood vessels within the pulp cavity provide nourishment to the tooth, while lymphatic vessels help in protection. Additionally, nerves within the pulp cavity facilitate sensation, allowing the tooth to respond to various stimuli.
Mechanical and Chemical Digestion in the Mouth
Mechanical and chemical digestion are essential processes that initiate the breakdown of food in the mouth, preparing it for further digestion in the gastrointestinal tract. Mechanical digestion begins as soon as food enters the mouth, while chemical digestion relies on specific enzymes to break down complex molecules into simpler forms.
- Mechanical Digestion:
- The process of mechanical digestion begins with the chewing of food, also known as mastication. Teeth play a critical role in this phase, as they cut, tear, and pulverize food into smaller particles.
- After chewing, food is mixed with saliva, a process that helps transform it into a soft, flexible mass called a bolus. This bolus is easier to swallow, facilitating the passage of food through the digestive tract.
- During mastication, small food molecules are dissolved in saliva, allowing them to interact with digestive enzymes more effectively.
- Chemical Digestion:
- Chemical digestion in the mouth is primarily facilitated by two key enzymes:
- Salivary Amylase:
- This enzyme is secreted by the salivary glands and plays a crucial role in breaking down starch into simpler units, namely monosaccharides and disaccharides.
- Foods typically contain a mix of monosaccharides, disaccharides, and polysaccharides. However, only monosaccharides can be absorbed by the body.
- Salivary amylase begins the process of hydrolyzing polysaccharides into smaller sugar units until it becomes inactivated by the acidic environment in the stomach.
- Lingual Lipase:
- Lingual lipase is secreted by glands located in the tongue and is responsible for breaking down triglycerides into diglycerides and fatty acids.
- This enzyme remains inactive in the mouth; however, it is activated in the acidic environment of the stomach. Therefore, while lingual lipase begins its role in lipid digestion, its primary function occurs after the food has been swallowed.
- Salivary Amylase:
- Chemical digestion in the mouth is primarily facilitated by two key enzymes:
5. Pharynx
The pharynx is a vital anatomical structure functioning as a funnel-shaped tube that connects the nasal and oral cavities to the esophagus and larynx. Composed of skeletal muscle and covered with mucous membrane, it plays essential roles in both respiration and digestion. The pharynx can be divided into three distinct parts, each contributing to its overall function.
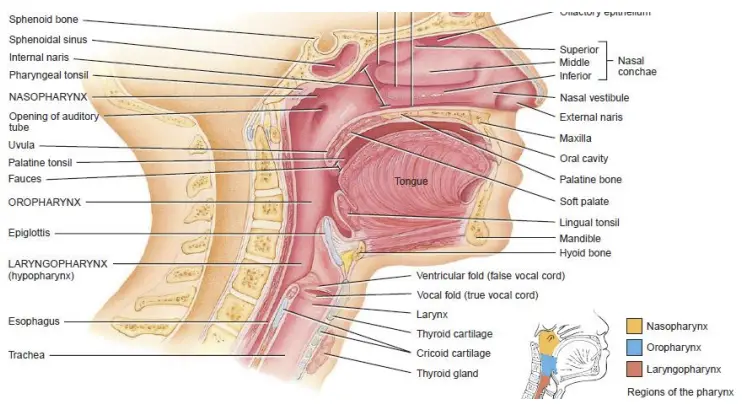
- Anatomical Divisions:
- Nasopharynx:
- This section is located behind the nasal cavities and above the soft palate.
- It plays a crucial role in respiration, allowing air to flow from the nasal cavity to the larynx and lungs.
- The Eustachian tube (auditory tube) connects the nasopharynx to the middle ear, helping to equalize pressure.
- Oropharynx:
- Positioned behind the oral cavity (buccal cavity), the oropharynx serves as a common passageway for both food and air.
- It connects the nasopharynx and the oral cavity, facilitating the swallowing process.
- Laryngopharynx:
- The most inferior part of the pharynx, it leads into the esophagus posteriorly and into the larynx anteriorly.
- This region is critical for directing food to the esophagus and air to the larynx for respiration.
- Nasopharynx:
- Functions:
- The primary function of the pharynx is to serve as a common passageway for food and air, allowing both processes to occur efficiently.
- It also aids in swallowing by coordinating the movement of food from the oral cavity to the esophagus.
- Waldeyer’s Ring:
- The pharynx contains lymphatic tissues organized in a ring-like structure known as Waldeyer’s ring, which includes:
- Pharyngeal Tonsil: Located in the nasopharynx, this tonsil can enlarge in children, resulting in adenoids that may obstruct breathing.
- Tubal Tonsils: Situated around the opening of the Eustachian tube, these tonsils contribute to immune defense.
- Palatine Tonsils: Attached to the palate, these tonsils are commonly infected, leading to tonsillitis, which can necessitate surgical removal (tonsillectomy).
- Lingual Tonsil: Located at the base of the tongue, this tonsil also plays a role in the immune response.
- The pharynx contains lymphatic tissues organized in a ring-like structure known as Waldeyer’s ring, which includes:
- Immune Function:
- The lymphoid tissues within Waldeyer’s ring are significant for the production of immunoglobulin A (IgA), an essential component of the immune system. This immunoglobulin helps protect against pathogens entering through the respiratory and digestive tracts.
6. Oesophagus
The human oesophagus, commonly referred to as the food pipe, serves a crucial role in the digestive system by transferring food from the pharynx to the stomach. It is approximately 25 centimeters long and is anatomically positioned behind the trachea and the heart. The structure of the oesophagus can be divided into three distinct parts, each with specific characteristics and functions.
- Anatomical Structure:
- Cervical Part:
- This section is located in the neck region.
- It is responsible for receiving food from the pharynx and initiating the swallowing process.
- Thoracic Part:
- Situated in the thorax, this portion of the oesophagus extends through the chest cavity.
- It plays a critical role in transporting food downward toward the abdominal cavity.
- Abdominal Part:
- This segment passes through the diaphragm, the muscular barrier between the thoracic and abdominal cavities.
- It opens into the stomach, allowing the transition of food from the oesophagus into the gastric environment for further digestion.
- Cervical Part:
- Functions:
- The primary function of the oesophagus is to facilitate the transfer of food from the pharynx to the stomach.
- This process involves a series of coordinated muscular contractions known as peristalsis, which propel the food bolus down through the oesophagus.
- The oesophagus also contains mucous glands that secrete mucus, which lubricates the food bolus and eases its passage.
7. Stomach (Gaster)
The stomach, or gaster, is a J-shaped enlargement of the gastrointestinal tract, located directly inferior to the diaphragm. This organ serves as a critical mixing chamber and holding reservoir for food, connecting the esophagus to the duodenum, which is the first part of the small intestine. The stomach is responsible for the initial stages of digestion, where ingested food is processed into a liquid form known as chyme.
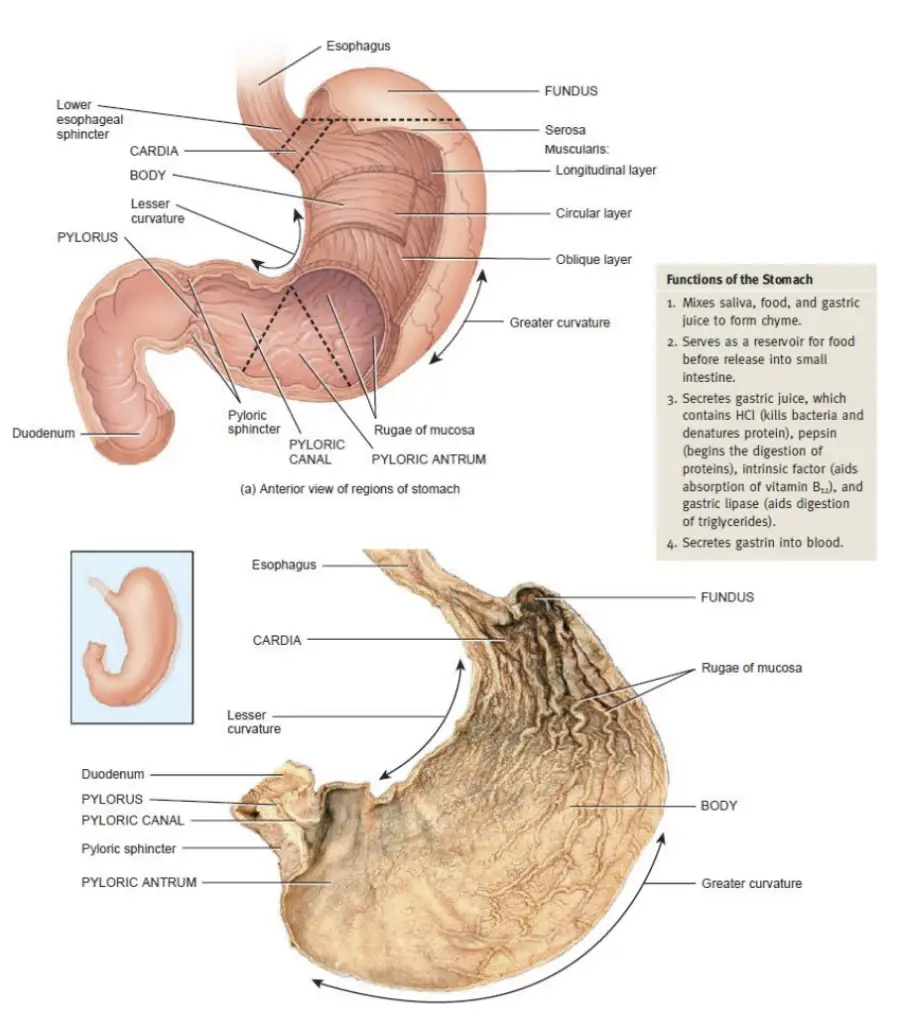
- Anatomical Structure:
- Regions of the Stomach:
- Cardiac Part: This region surrounds the superior opening of the stomach and is named for its proximity to the heart. It includes the gastroesophageal sphincter, or cardiac sphincter, which is a functional sphincter rather than a true valve.
- Fundus: Positioned superior and to the left of the cardia, the fundus is the rounded portion of the stomach that is often filled with air or gas.
- Body: The body constitutes the largest central portion of the stomach, located inferior to the fundus.
- Pyloric Part: This segment connects the stomach to the duodenum. It consists of the pyloric antrum, which connects to the body, and the pyloric canal, which leads to the duodenum. The pyloric sphincter regulates the passage of chyme into the small intestine.
- Regions of the Stomach:
- Histological Structure:
- The stomach wall is composed of four primary layers:
- Mucosa: This innermost layer contains gastric glands that are essential for digestion. The glands are made up of several types of cells:
- Mucous Neck Cells: These cells secrete mucus, which protects the stomach lining.
- Chief Cells: They produce pepsinogen and gastric lipase, initiating protein and fat digestion.
- Parietal Cells: Responsible for producing intrinsic factor (essential for vitamin B12 absorption) and hydrochloric acid (HCl), which creates a highly acidic environment for digestion.
- G Cells: These endocrine cells secrete the hormone gastrin into the bloodstream, stimulating digestive processes.
- Submucosa: Composed of areolar connective tissue, providing structural support.
- Muscularis: This layer includes three types of smooth muscle—oblique, circular, and longitudinal—allowing for the mechanical mixing and movement of food.
- Serosa: The outermost layer that protects and encases the stomach.
- Mucosa: This innermost layer contains gastric glands that are essential for digestion. The glands are made up of several types of cells:
- The stomach wall is composed of four primary layers:
- Functions of the Stomach:
- The stomach serves multiple functions, including:
- Storage: It temporarily holds food, allowing for a controlled release into the duodenum.
- Mixing: Mechanical digestion occurs as the stomach churns and mixes food with gastric juices, converting it into chyme.
- Digestion:
- Partial digestion of starch begins in the fundus with salivary amylase, but this enzyme is inactivated as food moves into the body of the stomach.
- As the food mixes with gastric juices, triglycerides begin to be digested by activated lingual lipase, breaking them down into diglycerides and fatty acids.
- Proteins are further digested by pepsin, which is activated from pepsinogen in the presence of hydrochloric acid.
- Absorption: Although limited, the stomach absorbs certain substances, including water, ions, alcohol, and some lipid-soluble drugs.
- The stomach serves multiple functions, including:
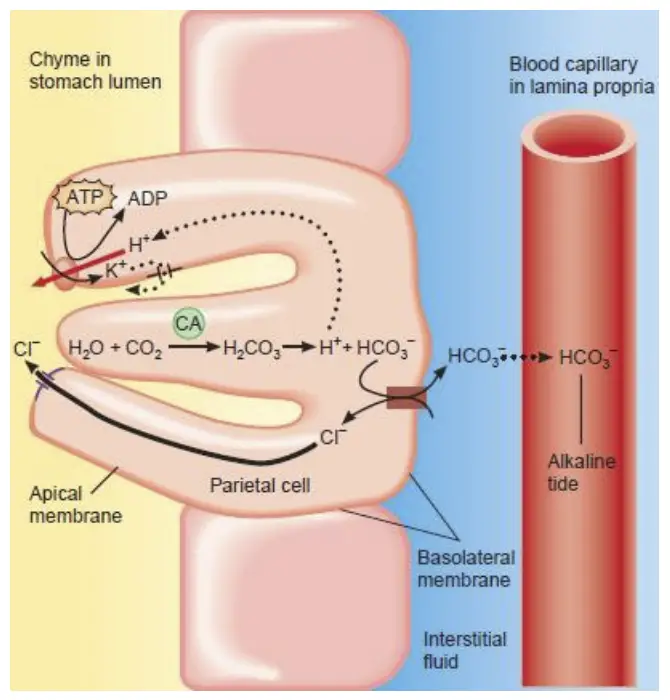
- Mechanism of HCl Secretion:
- Parietal cells secrete hydrogen (H+) and chloride (Cl-) ions separately, resulting in the production of hydrochloric acid (HCl) in the stomach lumen.
- This process is facilitated by proton pumps that transport H+ ions into the lumen while bringing potassium (K+) ions back into the cell.
- Additionally, carbonic anhydrase converts carbon dioxide (CO2) and water (H2O) into carbonic acid, which dissociates into H+ and bicarbonate (HCO3-).
- The H+ moves into the lumen, while HCO3- is released into the bloodstream. The secretion of HCl can be stimulated by various factors, including gastrin, acetylcholine, and histamine.
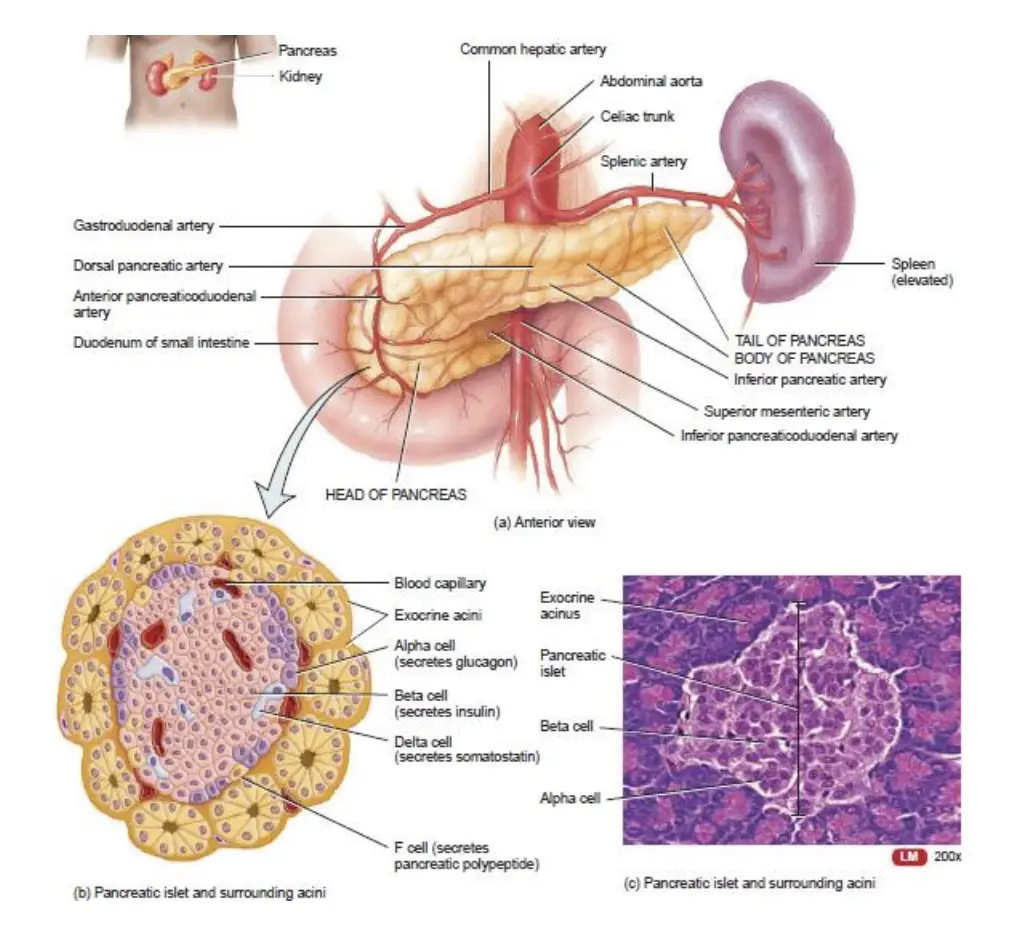
8. Pancreas
The pancreas, derived from the Greek words “pan” (all) and “creas” (flesh), is a retroperitoneal gland located posterior to the greater curvature of the stomach. This organ measures approximately 12-15 cm in length and 2-3 cm in thickness. The pancreas plays a critical role in digestion and metabolism, and its anatomical structure is divided into three primary sections: the head, body, and tail.
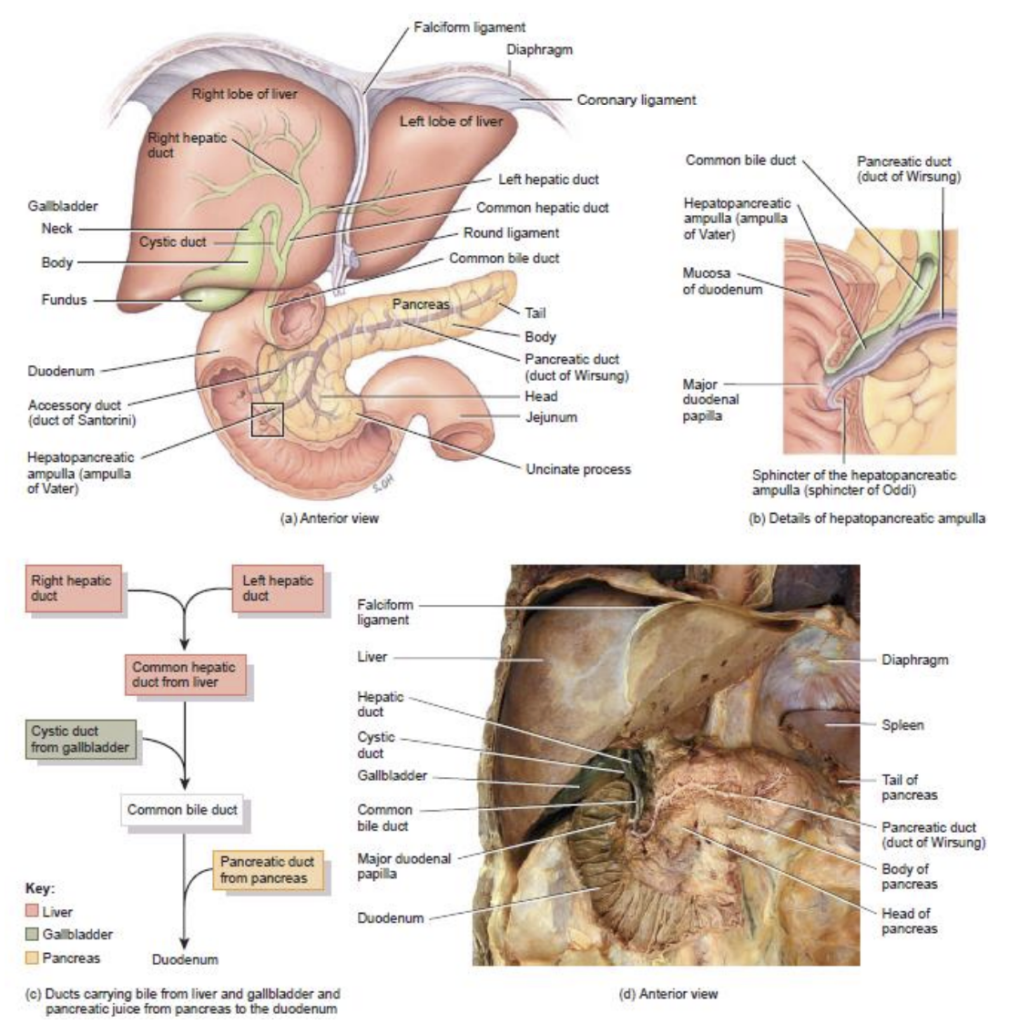
- Anatomical Structure:
- Head: This expanded portion of the pancreas is situated near the curve of the duodenum, the first section of the small intestine.
- Body: The central part of the pancreas, positioned to the left and superior to the head.
- Tail: The tapering end of the pancreas, which extends toward the spleen.
- Ductal System:
- The pancreas contains two main ducts that transport pancreatic juices into the duodenum:
- Pancreatic Duct: The larger duct that merges with the common bile duct from the liver, forming the hepatopancreatic ampulla. This ampulla opens into the duodenum, facilitating the flow of digestive enzymes.
- Accessory Duct: A smaller duct that also opens into the duodenum, providing an additional pathway for pancreatic juices.
- The pancreas contains two main ducts that transport pancreatic juices into the duodenum:
- Histology of the Pancreas:
- The pancreas is composed predominantly of small clusters of glandular epithelial cells known as acini. Approximately 99% of these acini are exocrine cells that secrete a mixture of fluids and digestive enzymes, collectively referred to as pancreatic juice.
- The remaining 1% consists of endocrine cells known as the pancreatic islets or islets of Langerhans. These islets are responsible for the secretion of four key hormones:
- Glucagon: Increases blood sugar levels.
- Insulin: Decreases blood sugar levels.
- Somatostatin: Regulates the levels of glucagon and insulin in the body.
- Pancreatic Polypeptide: Controls the secretion of somatostatin.
- Composition and Functions of Pancreatic Juice:
- Pancreatic juice is a clear, colorless fluid composed of water, salts, sodium bicarbonate, and various digestive enzymes. The pancreas produces between 1200 and 1500 ml of pancreatic juice daily.
- The sodium bicarbonate in pancreatic juice renders it slightly alkaline (with a pH of 7.1-8.2), neutralizing the acidity of gastric juice from the stomach. This alkalinity halts the action of pepsin and creates an optimal pH for the activity of digestive enzymes in the small intestine.
- The enzymes present in pancreatic juice include:
- Pancreatic Amylase: An enzyme responsible for digesting starch.
- Trypsin, Chymotrypsin, Carboxypeptidase, and Elastase: A group of enzymes that facilitate protein digestion.
- Pancreatic Lipase: The primary enzyme for triglyceride digestion.
- Ribonuclease and Deoxyribonuclease: Enzymes that digest nucleic acids.
9. Liver and Gall Bladder
The liver, the second-largest organ in the human body, plays a vital role in numerous physiological processes, including metabolism, detoxification, and bile production. It is located inferior to the diaphragm. The gall bladder, a pear-shaped sac, is situated inferiorly and posteriorly to the liver, functioning primarily as a storage reservoir for bile.
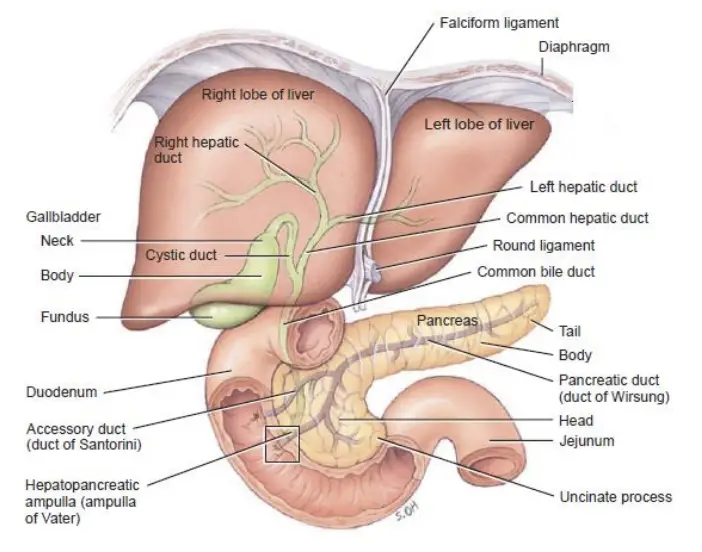
- Anatomy:
- Liver: The liver is divided into two lobes:
- Right Lobe: The larger of the two lobes.
- Left Lobe: The smaller lobe, separated from the right lobe by the falciform ligament.
- Gall Bladder: This organ consists of three portions:
- Fundus: The broad, inferior portion.
- Body: The middle portion.
- Neck: The upper, tapering portion.
- Liver: The liver is divided into two lobes:
- Histology:
- Liver: The liver is composed of lobes made up of smaller functional units known as lobules. Each lobule contains specialized cells called hepatocytes (hepato = liver, cytes = cells). Within the lobules, there are highly permeable capillaries that supply blood to the hepatocytes. These capillaries contain stellate reticuloendothelial cells, also referred to as Kupffer cells, which act as phagocytes. Kupffer cells play a crucial role in destroying worn-out red blood cells (RBCs), white blood cells (WBCs), bacteria, and other foreign materials.
- Hepatocytes secrete bile into bile canaliculi, which transport bile to bile ductules. These ductules channel bile into the left and right hepatic ducts, which converge to form the common hepatic duct. The common hepatic duct further combines with the cystic duct from the gall bladder to create the common bile duct.
- Gall Bladder: Composed of simple epithelial cells, the gall bladder’s smooth muscles contract to eject its contents into the cystic duct. The primary functions of the gall bladder are to store and concentrate bile until it is required in the duodenum. This concentration occurs through the absorption of water and ions.
- Liver: The liver is composed of lobes made up of smaller functional units known as lobules. Each lobule contains specialized cells called hepatocytes (hepato = liver, cytes = cells). Within the lobules, there are highly permeable capillaries that supply blood to the hepatocytes. These capillaries contain stellate reticuloendothelial cells, also referred to as Kupffer cells, which act as phagocytes. Kupffer cells play a crucial role in destroying worn-out red blood cells (RBCs), white blood cells (WBCs), bacteria, and other foreign materials.
- Role and Composition of Bile:
- The liver secretes approximately 1 liter of bile daily, a yellow, brownish, or olive-green liquid with a pH ranging from 7.6 to 8.6. Bile is primarily composed of water, bile salts, cholesterol, a phospholipid called lecithin, bile pigments, and various ions.
- Bile Salts: These consist of sodium and potassium salts of bile acids and are crucial for emulsification, which is the breakdown of large lipid molecules into smaller globules. This process enhances the digestion of fats by pancreatic lipase. Bile salts also facilitate lipid absorption.
- The liver secretes approximately 1 liter of bile daily, a yellow, brownish, or olive-green liquid with a pH ranging from 7.6 to 8.6. Bile is primarily composed of water, bile salts, cholesterol, a phospholipid called lecithin, bile pigments, and various ions.
- Functions of the Liver:
- Carbohydrate Metabolism: The liver maintains normal blood glucose levels by:
- Breaking down glycogen (the storage form of glucose) into glucose when blood sugar levels are low.
- Converting lactic acid and amino acids into glucose.
- Transforming fructose, galactose, and other sugars into glucose.
- Converting excess glucose into glycogen and triglycerides for storage when blood sugar levels rise.
- Lipid Metabolism: Hepatocytes:
- Store triglycerides.
- Break down fatty acids to generate ATP.
- Synthesize lipoproteins for the transport of fatty acids, triglycerides, and cholesterol to and from body cells.
- Synthesize cholesterol and utilize it to produce bile salts.
- Protein Metabolism: Hepatocytes:
- Remove the amino group (NH2) from amino acids, allowing them to be used for ATP production or conversion into carbohydrates or fats.
- Convert the harmful free amino group into urea for excretion through urine.
- Processing of Drugs and Hormones: The liver detoxifies substances such as alcohol and excretes drugs like penicillin, erythromycin, and sulfonamides into bile. It also chemically alters or excretes thyroid hormones and steroid hormones, including estrogens and aldosterone.
- Excretion of Bilirubin: The liver absorbs bilirubin, derived from the heme of aged red blood cells, from the blood and secretes it into bile. Most bilirubin in bile is metabolized by bacteria in the small intestine and eliminated in feces.
- Synthesis of Bile Salts: Bile salts are critical for emulsification and absorption of lipids in the small intestine.
- Storage: Besides glycogen, the liver serves as a major storage site for certain vitamins (A, B12, D, E, and K) and minerals (iron and copper).
- Phagocytosis: The Kupffer cells in the liver phagocytize aged red blood cells, white blood cells, and some bacteria.
- Activation of Vitamin D: The liver, along with the skin and kidneys, plays a role in synthesizing the active form of vitamin D.
- Carbohydrate Metabolism: The liver maintains normal blood glucose levels by:
10. Small Intestine
The small intestine is a crucial component of the digestive system, commencing at the pyloric sphincter of the stomach and extending through the central and inferior parts of the abdominal cavity until it connects with the large intestine. This organ plays a significant role in the digestion and absorption of nutrients from food.
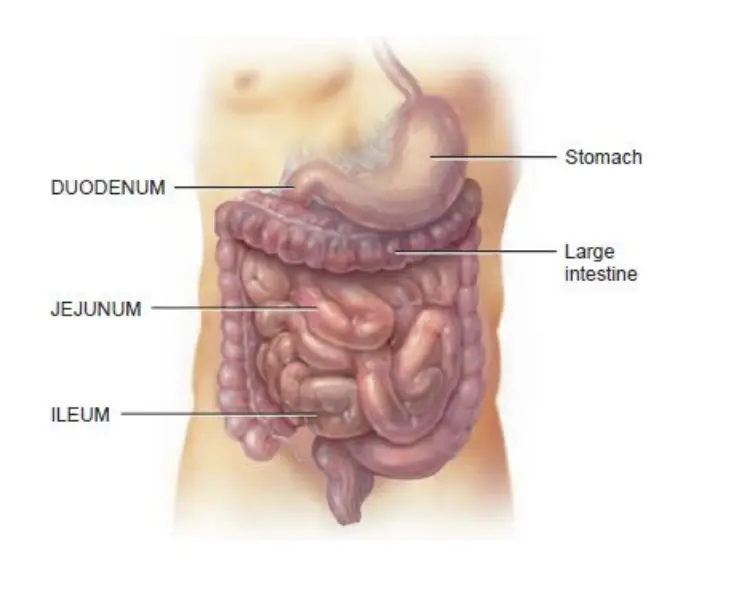
- Anatomy: The small intestine consists of three primary sections:
- Duodenum:
- This is the first part of the small intestine, beginning at the pyloric sphincter.
- It measures approximately 25 cm in length and connects to the jejunum.
- Jejunum:
- This section is the middle part of the small intestine, extending from the duodenum to the ileum.
- Ileum:
- This is the final section of the small intestine, concluding at the ileocecal junction where it meets the large intestine.
- Duodenum:
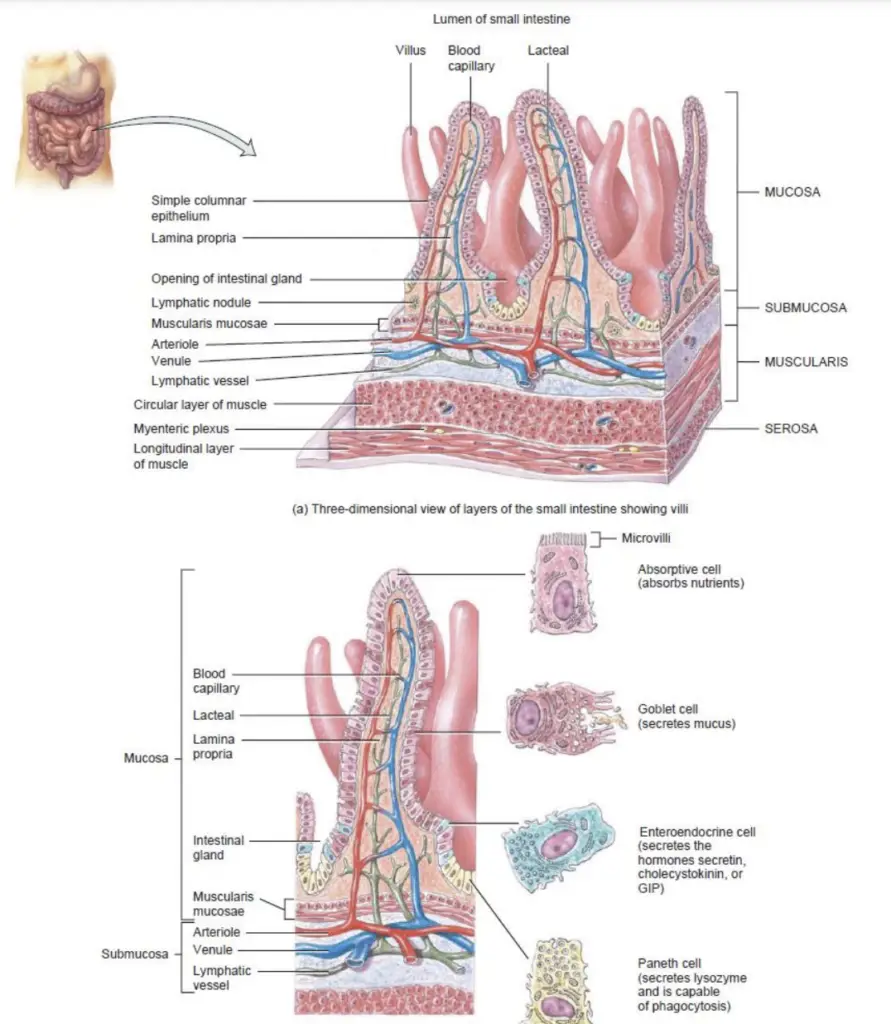
- Histology: The small intestine is composed of four basic layers:
- Mucosa:
- The mucosa contains several types of cells:
- Absorptive Cells: These cells are responsible for digesting and absorbing nutrients.
- Goblet Cells: These cells secrete mucus, which lubricates the intestinal contents.
- Paneth Cells: These cells secrete the bactericidal enzyme lysozyme, which plays a role in phagocytosis.
- Endocrine Cells: These cells release hormones into the bloodstream. Key types include:
- S Cells: Secrete secretin, which regulates the pH of the intestine.
- CCK Cells: Secrete cholecystokinin (CCK), which aids in digestion.
- K Cells: Secrete glucose-dependent insulinotropic peptide (GIP), which stimulates insulin release.
- The mucosa also features structural adaptations that enhance digestion and absorption:
- Circular Folds: These folds of mucosa and submucosa increase surface area and cause the chyme to move in a spiral pattern, facilitating digestion.
- Villi: These are fingerlike projections of the mucosa that significantly increase the surface area for absorption, covering about 20-40 square millimeters.
- Microvilli: These tiny projections from the free membrane of absorptive cells form a brush border, which cannot be seen individually under a microscope. This brush border also contains brush border enzymes that contribute to digestion.
- The mucosa contains several types of cells:
- Submucosa:
- The submucosa of the duodenum includes specialized glands that secrete alkaline mucus, helping to neutralize gastric acid in the chyme.
- Muscularis:
- The muscularis layer consists of two layers of smooth muscle: an outer longitudinal layer and an inner circular layer, which coordinate to facilitate peristalsis.
- Serosa:
- The serosa, or visceral peritoneum, envelops the small intestine entirely, providing protection and support.
- Mucosa:
- Role of Intestinal Juice and Brush Border Enzymes:
- Approximately 1 to 2 liters of intestinal juice with a pH of 7.6 are secreted daily, containing water and mucus. This intestinal juice mixes with pancreatic juices to create a liquid medium essential for the absorption of substances from chyme into the small intestine.
- Brush Border Enzymes: Secreted by the absorptive cells in the small intestine, these enzymes include:
- Carbohydrate-Digesting Enzymes:
- α-Dextrinase
- Maltase
- Sucrase
- Lactase
- Protein-Digesting Enzymes:
- Peptidases (including aminopeptidase and dipeptidase)
- Nucleotide-Digesting Enzymes:
- Nucleosidases
- Phosphatases
- Carbohydrate-Digesting Enzymes:
Mechanical and Chemical Digestion in the Small Intestine
Mechanical and chemical digestion in the small intestine are vital processes that ensure the efficient breakdown and absorption of nutrients from food. This section of the digestive system utilizes specific movements and enzymes to achieve optimal digestion.
- Mechanical Digestion: The mechanical breakdown of food in the small intestine involves two primary types of movements:
- Segmentation:
- Segmentation consists of localized mixing contractions occurring in regions of the small intestine that are distended with a large volume of chyme.
- This process enhances the mixing and absorption of chyme but does not propel it forward through the intestine.
- Migrating Motility Complex (MMC):
- The MMC is a peristaltic movement activated when the volume of chyme in the distended portions of the small intestine decreases.
- This type of movement functions to push the chyme forward, facilitating its progression through the digestive tract.
- Chyme typically remains in the small intestine for approximately 3 to 5 hours, allowing sufficient time for both mechanical and chemical digestion.
- Segmentation:
- Chemical Digestion: The chemical digestion of nutrients in the small intestine is a coordinated effort involving pancreatic juice, bile, and intestinal juice. The chyme entering the small intestine contains partially digested carbohydrates, proteins, and lipids due to the enzymatic action in the mouth and stomach. The completion of the digestion of these macromolecules occurs through the following mechanisms:
- Digestion of Carbohydrates:
- Starches are initially broken down into maltose, maltriose, and α-dextrin units by the enzyme pancreatic amylase.
- Subsequently, brush border enzymes act on these smaller units:
- α-Dextrinase converts α-dextrin into glucose.
- Maltase splits maltose and maltriose into 2-3 units of glucose.
- Lactase digests lactose into glucose and galactose.
- Sucrase breaks sucrose into molecules of glucose and fructose.
- It is important to note that cellulose, a polysaccharide, is not digested by amylase enzymes, thus it is referred to as roughage.
- Digestion of Proteins:
- Proteins are processed by enzymes such as trypsin, chymotrypsin, carboxypeptidase, and elastase, converting them into peptide units.
- These peptides are further broken down into small amino acids by the action of enzymes known as aminopeptidase and dipeptidase, which facilitate the breakdown of peptides into single amino acids.
- Digestion of Lipids:
- The majority of triglycerides in food are broken down into long-chain and short-chain fatty acids, as well as monoglycerides, through the action of pancreatic lipase.
- In the small intestine, bile salts emulsify long-chain fatty acids into shorter-chain fatty acids, enhancing their absorption.
- Digestion of Nucleic Acids:
- Pancreatic juice contains nucleic acid-digesting enzymes, specifically ribonuclease (which digests RNA) and deoxyribonuclease (which digests DNA), breaking them down into nucleotides.
- These nucleotides are subsequently digested by brush border enzymes known as nucleosidases and phosphatases, yielding pentoses, phosphates, and nitrogenous bases.
- Digestion of Carbohydrates:
Absorption in the Small Intestine
Absorption in the small intestine is a crucial process wherein digested nutrients are transferred from the gastrointestinal tract (GIT) into the bloodstream or lymphatic system. This phase follows the mechanical and chemical digestion, which converts large macromolecules into smaller, absorbable units, enabling the body to utilize essential nutrients effectively.
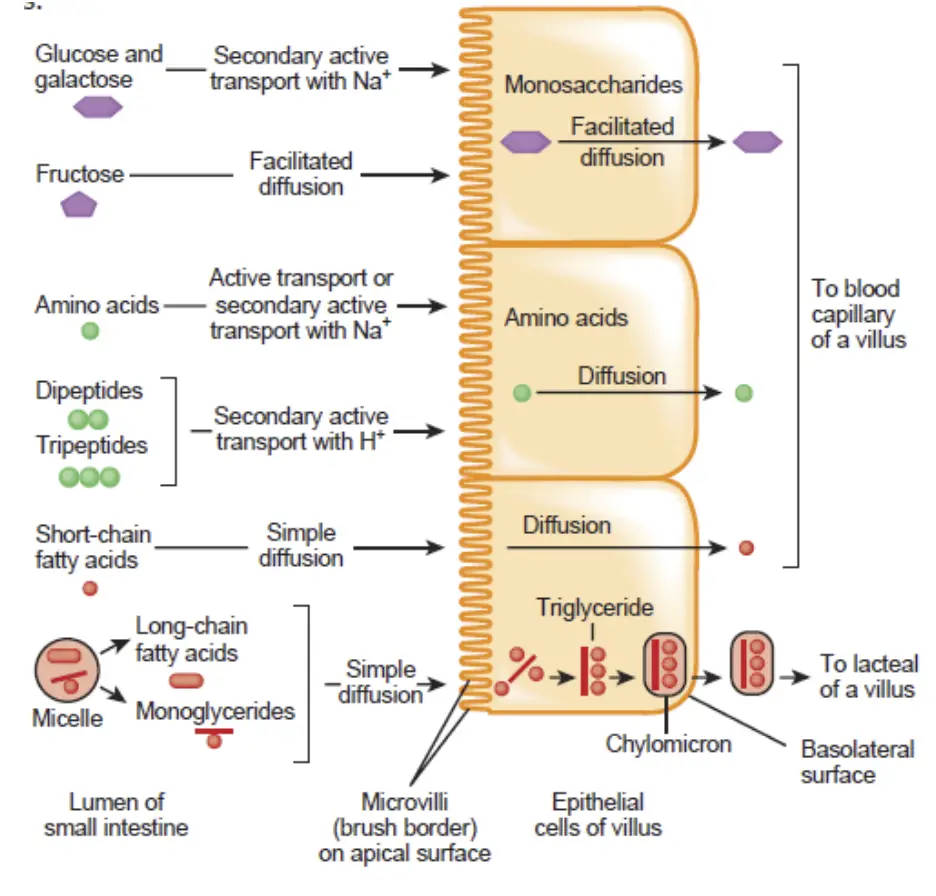
- Digestive Conversion: During digestion, macromolecules are broken down into smaller components:
- Carbohydrates are converted into monosaccharides, such as glucose, fructose, and galactose.
- Proteins are degraded into single amino acids, dipeptides, and tripeptides.
- Triglycerides are transformed into fatty acids, glycerol, and monoglycerides.
- Definition of Absorption: The passage of these digested nutrients from the GIT into the blood or lymph is termed absorption. Nutrients move from the intestinal lumen into absorptive cells lining the small intestine and then into blood or lymph capillaries, specifically the lacteals found within the villi.
- Lacteals: Lacteals are specialized lymphatic capillaries that absorb dietary fats. Their milky appearance, resulting from the absorption of fat, is where the term “lacteals” originates (from “lact,” meaning milky).
- Extent of Absorption: Approximately 90% of all nutrient absorption occurs in the small intestine, emphasizing its pivotal role in nutrient assimilation.
- Mechanisms of Absorption: Nutrient absorption involves various processes, including diffusion, facilitated diffusion, osmosis, and active transport. Each nutrient type utilizes specific mechanisms for effective absorption:
- Absorption of Monosaccharides:
- All carbohydrates are absorbed as monosaccharides.
- Fructose is absorbed through facilitated diffusion, while glucose and galactose are absorbed via secondary active transport into the absorptive cells.
- Once inside the absorptive cells, monosaccharides exit into the bloodstream via facilitated diffusion.
- Absorption of Amino Acids, Dipeptides, and Tripeptides:
- Most proteins are absorbed as amino acids through active transport.
- Dipeptides and tripeptides that enter the absorptive cells are further broken down into single amino acids.
- Amino acids then diffuse out of the absorptive cells into the bloodstream.
- Absorption of Lipids:
- All dietary lipids are absorbed by simple diffusion.
- Triglycerides are broken down into monoglycerides and fatty acids (both long-chain and short-chain).
- Short-chain fatty acids are easily absorbed, while long-chain fatty acids and monoglycerides require the assistance of bile salts.
- Bile salts form tiny structures known as micelles, which facilitate the transport of fatty acids and monoglycerides to the absorptive cells for absorption.
- Micelles also help solubilize and absorb other large hydrophobic molecules, such as fat-soluble vitamins (A, D, E, K) and cholesterol.
- Absorption of Electrolytes:
- Electrolytes absorbed in the small intestine originate from ingested foods, liquids, and gastrointestinal secretions.
- Key electrolytes, including sodium (Na+), calcium (Ca2+), bicarbonate, chloride, iodide, nitrate, iron, potassium, magnesium, and phosphate, are absorbed through active or passive transport.
- Absorption of Vitamins:
- Fat-soluble vitamins (A, D, E, K) are absorbed via simple diffusion aided by micelle formation.
- Water-soluble vitamins (B and C) are also absorbed through simple diffusion.
- Vitamin B12 requires binding to intrinsic factor, produced by the stomach, for its absorption in the ileum through active transport.
- Absorption of Water:
- Water absorption in the gastrointestinal tract occurs primarily through osmosis.
- Water can move across the intestinal mucosa in both directions; thus, the absorption of water from the small intestine is influenced by the absorption of electrolytes and nutrients, maintaining an osmotic balance with the blood.
- Absorption of Monosaccharides:
11. Large Intestine
The large intestine, as the terminal segment of the gastrointestinal (GI) tract, plays a crucial role in the final stages of digestion and nutrient absorption. Its primary functions encompass the completion of absorption, the production of specific vitamins, the formation of feces, and the subsequent expulsion of feces from the body.
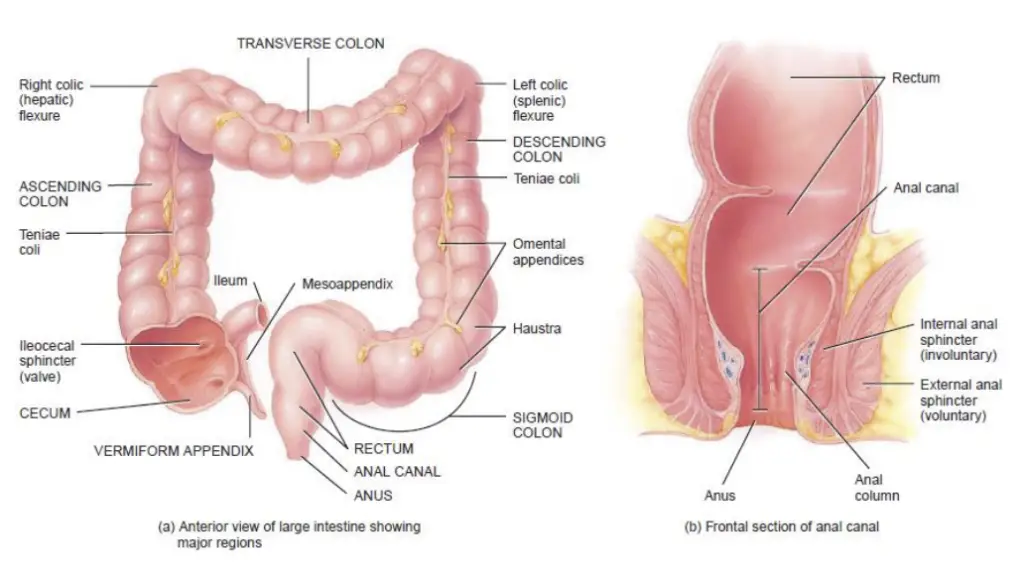
- Length and Structure:
- The large intestine measures approximately 1.5 meters in length and extends from the ileum, the last part of the small intestine, to the anus.
- The connection between the small and large intestines is facilitated by the ileocecal sphincter, which regulates the flow of materials from the small intestine into the large intestine.
- Major Regions of the Large Intestine: The large intestine is anatomically divided into four significant regions:
- Cecum:
- The cecum is a small, pouch-like structure located adjacent to the ileocecal sphincter.
- It serves as the entry point for undigested material from the small intestine.
- Attached to the cecum is the appendix, or vermiform appendix, a coiled and twisted tube with no essential digestive function, although it may play a role in immune response.
- Colon:
- The colon is a lengthy tubular structure situated next to the cecum.
- The open end of the cecum connects to the colon, which is further subdivided into four sections:
- Ascending Colon: This portion travels upward along the right side of the abdomen.
- Transverse Colon: The colon then crosses horizontally from the right to the left side of the abdomen.
- Descending Colon: It proceeds downward on the left side of the abdomen.
- Sigmoid Colon: The colon ends with a curved segment leading to the rectum.
- Rectum:
- The rectum comprises the last approximately 20 centimeters of the gastrointestinal tract.
- It serves as a temporary storage site for feces before they are expelled from the body.
- Anal Canal:
- The terminal 2-3 centimeters of the rectum constitute the anal canal, which opens to the exterior as the anus.
- The anus is encircled by two sphincters: the internal sphincter, composed of smooth muscle, and the external sphincter, made of skeletal muscle. These sphincters play vital roles in controlling the expulsion of feces from the body.
- Cecum:
- Functions of the Large Intestine:
- The large intestine completes the absorption of water and electrolytes, transforming the remaining indigestible food residues into feces.
- Additionally, certain vitamins, such as vitamin K and some B vitamins, are produced by intestinal bacteria and absorbed in this region.
- Finally, the large intestine is responsible for the formation and expulsion of feces, a process vital for maintaining the body’s homeostasis by eliminating waste.
Mechanical and Chemical Digestion in the Large Intestine
The large intestine is vital for the final stages of digestion, where mechanical and chemical processes occur to complete the breakdown of food residues and prepare them for elimination from the body. Understanding these processes is essential for grasping how the digestive system efficiently utilizes nutrients while disposing of waste.
- Mechanical Digestion:
- Passage of Contents: As food moves through the ileocecal sphincter, it fills the cecum and subsequently accumulates in the ascending colon.
- Haustral Churning: This mechanical process involves the haustra, which are pouches in the colon that relax and distend as they fill. Once a haustrum is sufficiently filled, its walls contract, pushing the contents into the next haustrum. This mechanism allows for effective mixing and movement of the material within the colon.
- Peristalsis: Peristaltic movements occur at a slow rate throughout the colon, aiding in the gradual progression of the contents.
- Mass Peristalsis: A more intense form of peristalsis known as mass peristalsis occurs approximately three to four times a day. This strong peristaltic wave originates from the middle of the transverse colon and drives the colonic contents into the rectum, preparing for eventual expulsion.
- Chemical Digestion:
- Role of Bacteria: In contrast to earlier stages of digestion, chemical digestion in the large intestine primarily relies on bacterial activity rather than enzymatic secretions. These bacteria play a crucial role in the breakdown of remaining nutrients.
- Fermentation of Carbohydrates: Bacteria ferment any residual carbohydrates, producing hydrogen, carbon dioxide (CO₂), and methane gas. Excessive production of these gases can lead to flatulence.
- Protein Breakdown: Remaining proteins are converted into amino acids by bacterial action. Further, these amino acids are transformed into simpler substances, such as indole and hydrogen sulfide, which the liver then metabolizes into less toxic compounds.
- Bilirubin Decomposition: Bacteria also facilitate the decomposition of bilirubin, a byproduct of hemoglobin breakdown, into simpler pigments like stercobilin. This pigment is responsible for the characteristic brown color of fecal material.
- Vitamin Production: Notably, certain vitamins, specifically Vitamin B and Vitamin K, are synthesized by bacteria in the large intestine. These vitamins are then absorbed in the colon, contributing to the body’s nutritional requirements.
Absorption and Feces Formation in the Large Intestine
The large intestine plays a crucial role in the final stages of digestion, particularly in the absorption of water and electrolytes, and in the formation of feces. Understanding these processes is essential for grasping how the body manages waste and maintains homeostasis.
- Absorption in the Large Intestine:
- Duration of Chyme Presence: The chyme, which is the semi-liquid mass of partially digested food, remains in the large intestine for approximately 3 to 10 hours. During this time, significant absorption occurs.
- Water Absorption: While 90% of all water absorption takes place in the small intestine, the large intestine contributes significantly to the body’s overall water balance by absorbing additional water. This absorption transforms the chyme into a solid or semi-solid form, which is referred to as feces.
- Ion Absorption: The large intestine is also responsible for absorbing various ions, including sodium and chloride. This process helps regulate the body’s electrolyte balance, which is vital for numerous physiological functions.
- Vitamin Absorption: In addition to water and ions, the large intestine absorbs certain vitamins produced by gut bacteria, further contributing to the body’s nutritional needs.
- Feces Formation:
- Composition of Feces: The resultant feces consists of several components:
- Water: Feces are primarily composed of water, which varies depending on the amount absorbed in the large intestine.
- Inorganic Salts: These salts are crucial for maintaining various bodily functions.
- Sloughed-off Epithelial Cells: The lining of the gastrointestinal tract sheds cells that are incorporated into the feces.
- Bacteria: A substantial portion of fecal matter consists of bacteria, including both live and dead cells.
- Bacterial Decomposition Products: The byproducts of bacterial metabolism contribute to the overall composition of feces.
- Unabsorbed Digested Materials: Any remnants of food that were not fully digested or absorbed in earlier digestive stages also form part of the feces.
- Indigestible Parts of Food: Fiber and other indigestible substances remain in the feces, which is important for maintaining digestive health.
- Composition of Feces: The resultant feces consists of several components:
12. Gastric Glands
Gastric glands are specialized structures located within the stomach’s epithelium, playing a crucial role in digestion. These microscopic, tubular glands are composed of various cell types, each contributing to the formation of gastric juice, which aids in the digestive process. The primary components of gastric glands include chief cells, oxyntic cells, mucous cells, endocrine cells, and stem cells. Each type of cell has specific functions essential for digestion and overall gastric health.
- Chief Cells (Peptic/Zymogenic Cells):
- Located primarily at the base of the gastric glands.
- Secrete gastric digestive enzymes in the form of pro-enzymes or zymogens, primarily pepsinogen and pro-rennin.
- Additionally produce small amounts of gastric amylase and gastric lipase.
- Gastric amylase assists in carbohydrate digestion but is inhibited by the stomach’s acidic environment.
- Gastric lipase contributes minimally to fat digestion.
- Pro-rennin is secreted in young mammals but is absent in adults.
- Oxyntic Cells (Parietal Cells):
- These cells are large and predominantly located on the side walls of the gastric glands.
- Stain strongly with eosin, hence the name oxyntic (meaning “acid-producing”).
- Secrete hydrochloric acid, which creates a highly acidic environment (pH 1.5-2.5) necessary for digestive enzyme activation.
- Produce Castle intrinsic factor, vital for vitamin B12 absorption.
- Mucous Cells (Goblet Cells):
- Present throughout the gastric epithelium.
- Secrete mucus, which provides a protective barrier against the harsh acidic environment of the stomach and aids in lubrication.
- Gastric Juice Composition:
- Gastric juice is composed of a mixture of secretions from chief cells, oxyntic cells, and mucous cells, contributing to its acidic pH and digestive capabilities.
- It typically includes pepsinogen, pro-rennin, gastric lipase, gastric amylase, mucus, and hydrochloric acid.
- In infants, gastric juice has a higher pH of about 5.0.
- Endocrine Cells:
- Located in the basal parts of gastric glands, these include argentaffin cells and gastrin cells (G-cells).
- Argentaffin Cells: Produce serotonin, somatostatin, and histamine.
- Serotonin: Functions as a vasoconstrictor and stimulates smooth muscle contraction.
- Somatostatin: Inhibits the release of hormones from the digestive tract, regulating gastric activity.
- Histamine: Causes dilation of blood vessels, enhancing blood flow.
- Gastrin Cells: Found mainly in the pyloric region, they secrete and store the hormone gastrin, which stimulates gastric glands to release gastric juice.
- Stem Cells:
- Undifferentiated cells present in the gastric epithelium.
- Responsible for the proliferation and replacement of other cells in the gastric glands.
- Their numbers increase when gastric epithelium is damaged, such as in the case of gastric ulcers, playing a significant role in the healing process.
13. Intestinal Glands
Intestinal glands are specialized structures formed by the surface epithelium of the small intestine, essential for digestion and nutrient absorption. These glands are classified into two main types: the crypts of Lieberkühn and Brunner’s glands. Each type has distinct cellular components and functions that contribute to the overall digestive process.
- Crypts of Lieberkühn:
- These are simple, tubular structures located throughout the small intestine, situated between the villi.
- They are responsible for the secretion of digestive enzymes and mucus.
- Goblet Cells (Mucous Cells): These cells within the crypts secrete mucus, which plays a crucial role in lubricating the intestinal lumen and protecting the intestinal lining.
- Enterocytes: These cells are present on the intestinal crypts and are responsible for secreting water and electrolytes, which help maintain the fluid balance in the intestine.
- At the base of the crypts are two important types of cells:
- Paneth Cells:
- Predominantly found in the duodenum, these cells are located at the bottom of the crypts of Lieberkühn.
- They are rich in zinc and contain acidophilic granules.
- Although their exact function is not entirely understood, evidence suggests that they secrete lysozyme, an antibacterial substance, and possess phagocytic capabilities, enabling them to ingest and destroy pathogens.
- Argentaffin Cells:
- These cells synthesize important hormones, including secretin and 5-hydroxytryptamine (5-HT), which play roles in digestive regulation.
- Paneth Cells:
- Brunner’s Glands:
- Unique to the duodenum, Brunner’s glands are located in the submucosa.
- They secrete a small amount of enzyme and mucus, which serve to protect the duodenal wall from the acidic chyme entering from the stomach.
- The mucus produced by these glands is vital for safeguarding the duodenum from potential digestive damage.
- The secretions from Brunner’s glands open into the crypts of Lieberkühn, integrating their functions with those of the crypts.
- Intestinal Juice:
- The combined secretion from the intestinal glands is referred to as intestinal juice or succus entericus, characterized by a pH of approximately 7.8.
- The small intestine secretes about 2,000-3,000 mL of intestinal juice daily.
- This intestinal juice contains a variety of enzymes critical for digestion, including:
- Maltase
- Isomaltase
- Sucrase
- Lactase
- α-Dextrinase
- Enterokinase
- Aminopeptidases
- Dipeptidases
- Nucleotidases
- Nucleosidases
- Intestinal Lipase
- These enzymes facilitate the breakdown of carbohydrates, proteins, and nucleic acids, ensuring efficient nutrient absorption.
- Mucous Glands:
- In addition to the crypts of Lieberkühn and Brunner’s glands, the entire alimentary canal contains mucous glands.
- These glands are responsible for producing mucus, which lubricates the digestive tract and facilitates the passage of food.
Phases of Digestion
Digestion is a complex process that occurs in three overlapping phases: the cephalic phase, the gastric phase, and the intestinal phase. Each phase plays a vital role in preparing the body for the intake and processing of food, ensuring that nutrients are effectively extracted and waste products are managed.
- Cephalic Phase:
- This initial phase is triggered by sensory stimuli associated with food. Factors such as the smell, sight, thought, or initial taste of food activate neural centers in various parts of the brain.
- Activation of Salivary and Gastric Glands: The brain stimulates the salivary glands to secrete saliva and the gastric glands to produce gastric juices.
- Preparation for Digestion: The cephalic phase essentially primes the mouth and stomach for the incoming food, enhancing the digestive processes that will follow.
- Gastric Phase:
- Once food reaches the stomach, the gastric phase commences, governed by neural and hormonal mechanisms that facilitate gastric secretion and motility.
- Neural Regulation:
- When food enters the stomach, it distends the stomach walls, activating stretch receptors.
- Chemoreceptor Activation: Chemoreceptors monitor the pH of the stomach chyme. As food distends the stomach and proteins increase pH, these receptors send nerve impulses that promote peristalsis and stimulate the flow of gastric juice.
- The resultant peristaltic waves mix food with gastric juice, facilitating gastric emptying into the duodenum.
- As this occurs, the pH of the stomach chyme becomes more acidic, and the distension of the stomach walls returns to normal.
- Hormonal Regulation:
- Gastric secretion is also regulated by the hormone gastrin, which is released from G cells when the stomach is distended by chyme or when partially digested proteins and caffeine enter the stomach.
- Gastrin Functions: Gastrin stimulates the gastric glands to secrete gastric juice, closes the lower esophageal sphincter to prevent acid reflux, and opens the pyloric sphincter to allow chyme to advance.
- The secretion of gastrin ceases when the stomach pH falls below 2, indicating sufficient acid levels.
- Intestinal Phase:
- This phase begins when food enters the small intestine and has primarily inhibitory effects that slow the exit of chyme from the stomach.
- Prevention of Overload: By controlling the flow of chyme, the intestinal phase prevents the duodenum from becoming overloaded, allowing for efficient digestion of the food that has already entered the small intestine.
- Regulation by Neural and Hormonal Mechanisms:
- Neural Regulation: The distension of the duodenum by chyme activates the enterogastric reflex. Stretch receptors in the duodenal wall send nerve impulses that inhibit gastric motility, leading to increased contraction of the pyloric sphincter and decreased gastric emptying.
- Hormonal Regulation: Two key hormones, cholecystokinin (CCK) and secretin, play critical roles:
- Cholecystokinin (CCK): Secreted by CCK cells, this hormone stimulates the secretion of pancreatic juice, contracts the gallbladder, and relaxes the sphincter of the hepatopancreatic ampulla (sphincter of Oddi), all of which enhance digestion. Additionally, CCK slows gastric emptying by promoting pyloric sphincter contraction and induces a sense of satiety.
- Secretin: Released from S cells in response to acidic chyme in the duodenum, secretin stimulates the flow of pancreatic juice rich in bicarbonate ions, which buffers the acidic chyme. Secretin also amplifies the effects of CCK and reduces the production of acid in the stomach.
Disorders of the Digestive System
The digestive system is susceptible to various disorders that can significantly impact its functionality and the overall health of individuals. Understanding these disorders helps in recognizing their symptoms, causes, and potential treatments.
- Gastroesophageal Reflux Disease (GERD):
- GERD occurs when the lower esophageal sphincter fails to close properly after food has entered the stomach, allowing stomach contents to reflux into the esophagus.
- The reflux can irritate the esophageal lining due to hydrochloric acid (HCl), leading to a burning sensation known as heartburn.
- Factors such as alcohol consumption and smoking can exacerbate this condition by relaxing the esophageal sphincter.
- Management strategies include avoiding certain foods that trigger acid secretion, such as coffee, chocolate, tomatoes, fatty foods, orange juice, peppermint, spearmint, and onions.
- Vomiting (Emesis):
- Vomiting is the forceful expulsion of contents from the upper gastrointestinal (GI) tract, including the stomach and sometimes the duodenum.
- Common stimuli for vomiting include irritation and distension of the stomach, unpleasant visual stimuli, general anesthesia, dizziness, and certain medications, such as morphine and digitalis derivatives.
- The act of vomiting involves coordinated contraction of the diaphragm and abdominal muscles, which expels the stomach contents through open esophageal sphincters.
- Prolonged vomiting can pose serious risks, especially in infants and the elderly, leading to complications such as alkalosis (elevated blood pH), dehydration, and damage to the esophagus and teeth.
- Jaundice:
- Jaundice is characterized by a yellowish discoloration of the sclerae (whites of the eyes), skin, and mucous membranes due to an accumulation of bilirubin.
- Bilirubin is produced from the breakdown of heme in aged red blood cells, transported to the liver, processed, and excreted into bile.
- The main categories of jaundice include:
- Prehepatic Jaundice: Results from excessive bilirubin production.
- Hepatic Jaundice: Caused by liver diseases such as congenital liver disease, cirrhosis, or hepatitis.
- Extrahepatic Jaundice: Occurs due to blockages in bile drainage caused by gallstones or cancers of the bowel or pancreas.
- Gallstones:
- Gallstones form when bile contains insufficient bile salts or lecithin or when there is an excess of cholesterol, leading to cholesterol crystallization.
- As gallstones grow in size and number, they can obstruct bile flow from the gallbladder to the duodenum, resulting in varying degrees of obstruction.
- Treatment options include gallstone-dissolving medications, lithotripsy (shock-wave therapy), or surgical intervention.
- Peptic Ulcer Disease (PUD):
- Peptic ulcers are sores that develop in the GI tract’s areas exposed to acidic gastric juice, commonly leading to bleeding and anemia.
- The main causes of PUD include:
- Helicobacter pylori: A bacterium that produces urease, enabling it to survive stomach acidity while damaging the protective mucous layer.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Such as aspirin, which can impair mucosal defenses.
- Hypersecretion of HCl: As seen in conditions like Zollinger-Ellison syndrome, caused by gastrin-secreting tumors.
- Therapeutic approaches for PUD emphasize avoiding irritants such as cigarette smoke, alcohol, caffeine, and NSAIDs to protect the gastric mucosa.
- Hepatitis:
- Hepatitis refers to liver inflammation caused by viruses, drugs, or chemicals, including alcohol. Several types of viral hepatitis exist:
- Hepatitis A: Caused by the hepatitis A virus, spread through the fecal-oral route, often resulting in mild illness without lasting liver damage.
- Hepatitis B: Caused by the hepatitis B virus, transmitted mainly through sexual contact and contaminated needles, can lead to chronic liver disease and cancer.
- Hepatitis C: Similar in transmission and consequences to hepatitis B, it can also result in serious liver damage.
- Hepatitis D: Requires co-infection with hepatitis B for transmission.
- Hepatitis E: Spread like hepatitis A, but poses high mortality risk among pregnant women, although it does not lead to chronic liver disease.
- Hepatitis refers to liver inflammation caused by viruses, drugs, or chemicals, including alcohol. Several types of viral hepatitis exist:
Types of Digestive Juice
Digestive juices are crucial for the breakdown and absorption of nutrients throughout the alimentary canal. There are five main types of digestive juices: saliva, gastric juice, pancreatic juice, succus entericus (intestinal juice), and bile. Each type of digestive juice is produced by specific glands and released at different points in the digestive tract, playing a significant role in the digestive process.
- Salivary Secretion:
- Salivary secretion primarily occurs through reflex mechanisms, categorized into two types: conditioned and unconditioned reflexes.
- Conditioned Reflexes: The sight or smell of food can trigger salivary secretion, demonstrating the brain’s ability to anticipate food intake.
- Unconditioned Reflexes: These reflexes originate primarily in the mouth but can also be stimulated by the esophagus or stomach, leading to the esophago-salivary and gastro-salivary reflexes, respectively. Additionally, stimuli from other visceral organs, such as the gravid uterus, can induce salivary secretion.
- Overall, salivary secretion is essential for preparing the oral cavity for digestion and swallowing, ensuring an adequate production of saliva.
- Gastric Secretion:
- Gastric secretion is a multifaceted process influenced by various stimuli and occurs in three distinct phases:
- Cephalic Phase:
- This phase starts immediately after food intake and involves reflex mechanisms (both conditioned and unconditioned). The juice secreted during this phase is known as appetite juice, which has a constant composition and does not vary with the type of food. Although small in quantity, it plays a significant role in initiating digestion.
- Gastric Phase:
- This phase commences approximately thirty minutes after food enters the stomach and is primarily chemical. Gastrin, produced by the pyloric mucous membrane, stimulates gastric glands to secrete gastric juice, resulting in the largest quantity of gastric secretion. The nature of food influences the quality and quantity of gastric juice secreted; proteins increase both the volume and hydrochloric acid (HCl) content, while fats inhibit secretion.
- Intestinal Phase:
- Initiated when food enters the duodenum, this phase involves a smaller secretion amount that is independent of neural stimulation. The chemical stimulus, although not fully understood, causes inhibition of gastric secretion due to the presence of fat in the duodenum, likely through the release of the inhibitory hormone enterogastrone.
- Cephalic Phase:
- The interconnectedness of these phases allows for a coordinated digestive response, where the cephalic phase prepares the stomach, the gastric phase maximizes digestion, and the intestinal phase regulates further secretion based on the digestive progress.
- Gastric secretion is a multifaceted process influenced by various stimuli and occurs in three distinct phases:
- Pancreatic Secretion:
- Pancreatic secretion is vital for digestion and occurs in two distinct phases:
- Nervous Phase:
- This phase begins 1-2 minutes after food intake and is purely unconditioned. It is stimulated by sensory input during chewing and swallowing, with the stomach contributing to the reflex.
- Chemical Phase:
- This phase occurs when the stomach’s contents enter the duodenum. Hormones such as secretin and pancreozymin play critical roles in regulating pancreatic juice composition. Secretin is released in response to acidic chyme and stimulates the secretion of water, alkali, and salts, while pancreozymin increases enzyme content.
- Nervous Phase:
- The composition of pancreatic juice varies with food type; for instance, meat stimulates a secretin-rich secretion, while fat promotes a higher enzyme content. Bread consumption elicits a mixed type of pancreatic secretion.
- Pancreatic secretion is vital for digestion and occurs in two distinct phases:
- Bile Secretion:
- Bile secretion, an essential function of the liver, involves the production and release of bile into the digestive system. The process can be studied through various experimental methods, such as altercursive and triple intubation.
- Bile secretion is continuous and active, with total daily production ranging from 800 to 1,000 milliliters. The rate of secretion increases about one hour after food intake and remains elevated for 2 to 5 hours, decreasing afterward to fasting levels.
- Chemical stimuli, including bile salts, foodstuffs (particularly fats and proteins), and humoral factors such as cholecystokinin and hepatocrinin, regulate bile secretion. Bile salts are chief cholagogues, promoting bile flow, while the presence of food in the intestine acts as a mechanical stimulus for bile secretion.
- Enterocrinin, a hormone produced by the intestinal mucosa, also plays a crucial role in stimulating bile secretion, which is important for digestion and absorption in the intestine. After the digestive period, which typically lasts 2 to 5 hours, the flow of bile ceases.
Secretions in the Gastro-Intestinal Tract
The gastrointestinal tract relies on various secretions regulated by humoral factors to facilitate the digestion and absorption of nutrients. Each part of the digestive system utilizes specific hormones and chemical substances that control the release of secretions, ensuring efficient digestion. Below is an organized overview of these secretions across different sections of the gastrointestinal tract.
- Gastric Secretion:
- Gastrin:
- Gastrin is a hormone secreted by G cells located in the stomach lining.
- It plays a pivotal role during the gastric phase of secretion by stimulating gastric acid production and promoting pepsin production, which aids in protein digestion.
- Hormones or Secretagogues:
- Various chemical substances act as secretagogues during the intestinal phase of gastric secretion.
- These substances are crucial for triggering gastric secretions, ensuring the digestive process continues smoothly.
- Enterogastrone:
- Released in response to chyme in the duodenum, enterogastrone inhibits gastric secretion.
- It regulates the movement of food from the stomach to the small intestine, thus supporting efficient digestion and nutrient absorption.
- Gastrin:
- Pancreatic Secretion:
- Secretin:
- Secretin is the primary chemical stimulus for pancreatic secretion.
- When acidic chyme enters the duodenum, S cells release secretin, prompting the pancreas to secrete bicarbonate-rich pancreatic juice, which neutralizes chyme acidity.
- Pancreozymin (Cholecystokinin – CCK):
- Released by the intestinal mucosa in response to fats and proteins, pancreozymin stimulates the pancreas to release digestive enzymes.
- This release is essential for the effective digestion of dietary fats and proteins.
- Foodstuffs:
- The composition of food also influences pancreatic secretion.
- Certain components, such as amino acids and fatty acids, can directly stimulate the pancreas to release specific enzymes required for digestion.
- Secretin:
- Succus Entericus (Intestinal Juice):
- Products of Protein Digestion:
- Breakdown products from protein digestion, including peptides and amino acids, stimulate the secretion of succus entericus.
- This intestinal juice contains enzymes that further decompose peptides into individual amino acids for absorption.
- Enterocrinin:
- Believed to be the chief stimulus for succus entericus secretion, enterocrinin is released by enteroendocrine cells in the small intestine in response to partially digested proteins and peptides.
- Duocrinin:
- Another important humoral factor, duocrinin, is released when fats and carbohydrates are present in the small intestine, contributing to the secretion of intestinal juice.
- Products of Protein Digestion:
- Bile Secretion:
- Bile Salts:
- Bile salts are the primary stimulus for bile secretion.
- Synthesized in the liver from cholesterol and stored in the gallbladder, they are released when fatty food enters the small intestine, facilitating the emulsification and absorption of fats.
- Fat and Protein Food:
- The presence of fat and protein in the small intestine further stimulates bile release, enhancing the digestion and absorption of dietary fats and fat-soluble vitamins.
- Hepatocrinin:
- Hepatocrinin acts on liver cells to stimulate bile secretion, supporting the digestive process.
- Cholecystokinin (CCK):
- In addition to its role in pancreatic secretion, CCK stimulates gallbladder contraction, leading to the release of stored bile into the small intestine, thereby facilitating fat digestion.
- Bile Salts:
Main Phases of Gastric Secretion
Gastric secretion consists of four distinct phases: the Nervous Phase, Gastric Phase, Intestinal Phase, and Interdigestive Phase. Each phase plays a crucial role in the digestive process, coordinating the secretion of gastric juices and enzymes essential for food digestion. Below is a detailed overview of each phase, highlighting their functions and interrelationships.
- Nervous Phase:
- This phase is initiated by the stimulation of the vagus nerve and sympathetic nerves, along with the influence of the hypothalamus on gastric secretion.
- Vagal Stimulation:
- The vagus nerve stimulates gastric cells to release acetylcholine, which promotes the secretion of pepsin, hydrochloric acid (HCl), and mucus.
- Additionally, vagal stimulation can enhance the release of histamine, further stimulating parietal cells responsible for acid secretion and promoting vasodilation of the gastric mucosa.
- Under certain conditions, vagal stimulation may decrease or inhibit gastric secretions.
- It also enhances the release of gastrin and increases the responsiveness of stomach cells to other stimuli.
- Sympathetic Stimulation:
- Stimulation of sympathetic nerves leads to vasoconstriction of gastric blood vessels.
- The effects on gastric secretion are inconsistent compared to vagal stimulation.
- Influence of the Hypothalamus:
- The hypothalamus plays a significant role in augmenting gastric secretion by increasing vagal activity.
- Hypoglycemia can also stimulate gastric secretion through similar mechanisms.
- Lesions in the hypothalamus may result in severe gastric complications, such as hemorrhages or ulcers.
- Reflex Mechanisms:
- The nervous phase includes both unconditioned and conditioned reflexes.
- Unconditioned Reflex: Triggered by sensory stimuli during chewing and swallowing, involving the trigeminal, facial, and glossopharyngeal cranial nerves.
- Conditioned Reflex: Established through the sight, smell, or sound of food, leading to gastric secretion even in the absence of food.
- Characteristics of Appetite Juice:
- The “appetite juice” or psychic juice secreted during this phase is rich in pepsin, acidic, and contains mucus.
- Its quantity varies with appetite intensity and can be inhibited by stress or anxiety.
- Although significant in animals, its quantity in humans is less critical but serves to initiate subsequent gastric phases.
- Gastric Phase (Hormonal):
- The gastric phase is characterized by the stomach’s response to food presence, involving local and vagal reflexes and the release of gastrin.
- Gastrin’s Role:
- Gastrin, produced by the pyloric area’s mucosa, stimulates gastric secretion upon food entry.
- This phase occurs independently of nervous reflexes and is primarily driven by chemical stimuli.
- Experimental evidence supports gastrin’s role, including its ability to stimulate gastric secretion upon introduction or extraction from the pyloric mucosa.
- Stimulants and Inhibitors:
- Various food substances influence gastric secretion differently:
- Meat increases both quantity and HCl content.
- Bread stimulates high digestive power secretion.
- Fat inhibits gastric secretion, likely due to enterogastrone, particularly from the duodenum.
- Substances like water, tea, and certain juices stimulate secretion, while mechanical distention (e.g., gas) also promotes it.
- Various food substances influence gastric secretion differently:
- Nature and Action of Gastrin:
- Gastrin exists in two forms, gastrin I and gastrin II, which have distinct amino acid sequences.
- It stimulates gastric secretion rich in acid but low in pepsin, also influencing bile and pancreatic secretion.
- This phase constitutes the majority of gastric juice and typically lasts about three hours, varying based on food type.
- Intestinal Phase:
- The intestinal phase occurs due to the presence of certain substances in the small intestine and can last 8-10 hours.
- Stimulation of Gastric Secretion:
- Substances like water, meat extract, and partly digested proteins can stimulate gastric secretion during digestion or upon introduction into the duodenum.
- This phase operates through chemical stimuli from the intestine, independent of nerve connections.
- Inhibition of Gastric Secretion:
- Certain substances in the duodenum can inhibit gastric secretion:
- Introduction of alkali directly inhibits secretion.
- Fats present in the duodenum inhibit secretion via enterogastrone, which also reduces gastric motility.
- Urogastrone, similar to enterogastrone, is another inhibitory substance derived from urine and is suggested for therapeutic use in gastric ulcers.
- Certain substances in the duodenum can inhibit gastric secretion:
- Interdigestive Phase:
- The interdigestive phase occurs between meals and involves regular intervals of hydrochloric acid secretion even without food intake.
- Regular Acid Secretion:
- Episodes of hydrochloric acid secretion occur periodically during fasting, influenced by stimulation of the vagus nerve.
- Hormonal and Nervous Mechanisms:
- This phase is regulated by both hormonal and nervous systems, particularly through the vagus nerve.
- Relationship to the Intestinal Phase:
- The interdigestive phase is closely related to the intestinal phase, representing a specific aspect of gastrointestinal activity during fasting.
- Spontaneous Salivary Secretion:
- Saliva secretion can occur independently of food intake and may influence acid secretion during this phase.
Gastrointestinal Hormones and Digestive Secretions
Gastrointestinal hormones play a crucial role in regulating digestive secretions and processes. Here are the ten important gastrointestinal hormones and their functions:
- Gastrin: Secreted by gastrin cells in the pyloric region of the stomach, gastrin stimulates gastric glands to secrete and release gastric juice. It also promotes gastric mobility.
- Enterogastrone (Gastric Inhibitory Peptide – GIP): Secreted by the duodenal epithelium, enterogastrone inhibits gastric secretion and motility. It slows down gastric contractions, earning it the name gastric inhibitory peptide.
- Secretin: Secretin, the first hormone discovered, is produced by the epithelium of the duodenum. It stimulates the release of bicarbonates in pancreatic juice, increases bile secretion, and decreases gastric secretion and motility.
- Cholecystokinin Pancreozymin (CCK-PZ): Secreted by the epithelium of the small intestine, CCK-PZ stimulates the gallbladder to release bile and the pancreas to secrete digestive enzymes in pancreatic juice.
- Duocrmin: Produced by the duodenal epithelium, duocrmin stimulates the Brunner’s glands to release mucus and enzymes into the intestinal juice.
- Enterocrinin: Secreted by the epithelium of the entire small intestine, enterocrinin stimulates the crypts of Lieberkuhn to release enzymes into the intestinal juice.
- Vasoactive Intestinal Peptide (VIP): VIP is secreted by the epithelium of the entire small intestine. It dilates peripheral blood vessels in the gut and inhibits gastric acid secretion.
- Villikinin: Produced by the epithelium of the entire small intestine, villikinin accelerates the movement of villi, aiding in nutrient absorption.
- Somatostatin (SS): Somatostatin, secreted by the Delta cells of the pancreatic islets of Langerhans, inhibits the secretion of glucagon by alpha cells and insulin by beta cells. Somatostatin produced by argentaffin cells of gastric and intestinal glands suppresses the release of hormones from the digestive tract.
- Pancreatic Polypeptide (PP): Pancreatic polypeptide is secreted by the pancreatic polypeptide cells (also known as PP cells or F-cells) of the islets of Langerhans. It inhibits the release of pancreatic juice from the pancreas.
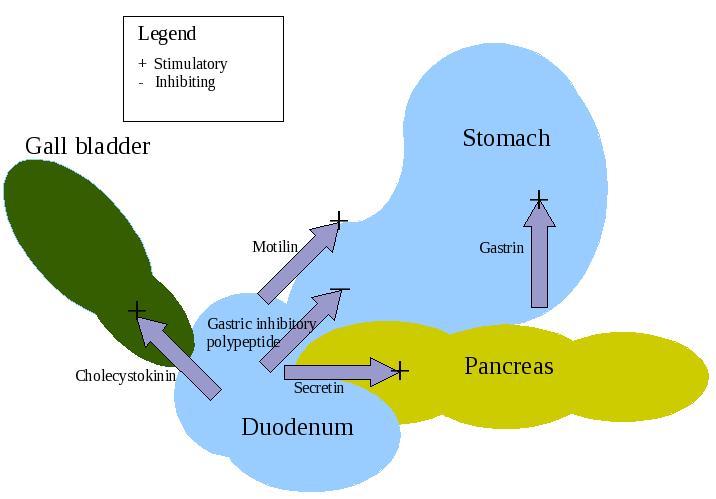
These gastrointestinal hormones play vital roles in regulating the secretion of digestive juices such as gastric juice, pancreatic juice, and bile. They also influence gastric motility and other digestive processes, ensuring effective digestion and absorption of nutrients.
Functions of the Digestive System
The digestive system performs several essential functions that enable the body to process food, absorb nutrients, and eliminate waste. Each function plays a crucial role in maintaining overall health and homeostasis. The primary functions of the digestive system can be outlined as follows:
- Ingestion: This is the initial phase of digestion, involving the intake of food and liquids through the mouth. Ingestion marks the starting point of the digestive process, as it introduces nutrients into the body.
- Secretion: Within the gastrointestinal (GI) tract and accessory digestive organs, specialized cells secrete approximately seven liters of water, acids, buffers, and digestive enzymes daily. These secretions are vital for facilitating the digestion of food, providing the necessary conditions for enzymatic action, and maintaining an optimal pH for digestive processes.
- Mixing and Propulsion: The digestive system relies on alternating contractions and relaxations of smooth muscle in the walls of the GI tract. This coordinated movement serves two main purposes: it mixes food with digestive secretions to enhance breakdown and propels the mixture toward the anus. This ability of the GI tract to mix and move materials along its length is known as motility.
- Digestion: Digestion consists of two distinct processes—mechanical and chemical.
- Mechanical Digestion: This involves the physical breakdown of food into smaller pieces. Teeth play a vital role by cutting and grinding food during chewing. Following ingestion, smooth muscle contractions in the stomach and small intestine further reduce food size and ensure it is thoroughly mixed with digestive enzymes.
- Chemical Digestion: In this process, large macromolecules such as carbohydrates, lipids, proteins, and nucleic acids are broken down into smaller molecules through hydrolysis, facilitated by digestive enzymes. It is noteworthy that certain substances, including vitamins, ions, cholesterol, and water, can be absorbed directly without undergoing chemical digestion.
- Absorption: Absorption refers to the process whereby ingested and secreted fluids, ions, and the products of digestion enter the epithelial cells lining the lumen of the GI tract. This process is crucial for the transfer of nutrients into the bloodstream or lymphatic system, enabling these substances to circulate throughout the body and nourish various cells.
- Defecation: The final function of the digestive system involves the elimination of waste. Indigestible substances, bacteria, cells shed from the lining of the GI tract, and undigested materials are expelled from the body through the anus in a process known as defecation. The material eliminated is termed feces, which represents the residues of the digestive process that the body cannot utilize.
FAQ
What is the digestive system?
The digestive system is a complex network of organs and tissues that work together to process food, extract nutrients, and eliminate waste from the body. It includes organs such as the mouth, esophagus, stomach, small intestine, large intestine, liver, gallbladder, and pancreas.
What happens in the stomach during digestion?
In the stomach, food is mixed with gastric juices containing enzymes and hydrochloric acid. This helps break down proteins and kill bacteria present in the food. The stomach’s muscular walls also aid in churning and mixing the food.
What is the role of the small intestine in digestion?
The small intestine is the primary site for nutrient absorption. Here, the partially digested food from the stomach is further broken down by enzymes from the pancreas and bile from the liver. The small intestine absorbs nutrients, such as carbohydrates, proteins, fats, vitamins, and minerals, into the bloodstream.
What does the large intestine do?
The large intestine, also known as the colon, absorbs water and electrolytes from the remaining undigested food. It also houses beneficial bacteria that help ferment indigestible fibers and produce certain vitamins. The waste material, known as feces, is formed in the large intestine and eliminated from the body through the rectum and anus.
How does the liver contribute to digestion?
The liver plays a vital role in digestion by producing bile, which is stored in the gallbladder and released into the small intestine when needed. Bile helps break down fats into smaller droplets, making them easier to digest and absorb.
How does the digestive process begin?
The digestive process begins in the mouth, where food is chewed and mixed with saliva. The enzymes present in saliva start breaking down carbohydrates.
What is the function of the pancreas in digestion?
The pancreas produces digestive enzymes that are released into the small intestine. These enzymes break down carbohydrates, proteins, and fats into simpler molecules that can be absorbed by the body. The pancreas also secretes insulin and glucagon, hormones that regulate blood sugar levels.
How long does the digestion process take?
The duration of digestion varies depending on the type of food consumed. On average, it takes about 24 to 72 hours for food to pass through the entire digestive system.
What are some common digestive disorders?
Common digestive disorders include gastroesophageal reflux disease (GERD), irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), peptic ulcers, gallstones, and constipation.
How can I maintain a healthy digestive system?
To maintain a healthy digestive system, it is important to eat a balanced diet rich in fiber, drink plenty of water, exercise regularly, manage stress, and avoid excessive alcohol consumption and smoking. It is also recommended to have regular check-ups with a healthcare provider and seek medical attention if any digestive symptoms or concerns arise.
References
- Image Source: https://en.wikipedia.org/wiki/Human_digestive_system
- https://www.medicinenet.com/digestive_disease_myths_pictures_slideshow/article.htm
- https://www.brainkart.com/article/Human-Digestive-System_39912/
- https://www.turito.com/blog/biology/human-digestive-system
- https://www.biologydiscussion.com/essay/human-digestive-system-with-diagram/1521
- https://www.biologydiscussion.com/human-physiology/human-digestive-system/main-parts-of-human-digestive-system-with-diagram/52385
- https://courses.lumenlearning.com/suny-ap2/chapter/overview-of-the-digestive-system/
- https://basicmedicalkey.com/structure-and-function-of-the-digestive-system/
- https://www.kenhub.com/en/library/anatomy/the-digestive-system
- https://biologydictionary.net/digestive-system/
- https://www.labxchange.org/library/items/lb:LabXchange:644a2c8b:html:1
- https://www.saintlukeskc.org/health-library/anatomy-digestive-system
- https://www.palmbeachstate.edu/slc/Documents/AandPch22LecturePearson.pdf
- http://www.rnlkwc.ac.in/pdf/study-material/physiology/Digestive%20system.pdf
- https://www.biologynotes.site/human-digestive-system/