What are Hormones?
- Hormones are chemical messengers produced by specialized cells known as endocrine glands. These substances are released into the bloodstream, where they travel to target cells or organs, enabling the body to regulate various biological processes. Hormones play a key role in coordinating and integrating activities across the trillions of cells in a multicellular organism, ensuring the body functions as a cohesive unit. Only cells equipped with specific receptors for a hormone will respond to it, allowing for precise control of physiological functions.
- Endocrinology, the scientific study of hormones and the glands that produce them, traces its origins to 1849, when A.A. Berthold conducted an experiment on cockerels. He discovered that the removal of the testes led to the loss of male characteristics, but reintroducing one testes restored these traits. This pivotal discovery demonstrated that certain glands secrete substances—later identified as hormones—that influence the body’s functions. Over time, more hormones were identified, each with specific roles in regulating processes such as growth, metabolism, and reproduction.
- In 1905, Ernest H. Starling and William Bayliss coined the term “hormone” from the Greek word ‘ormao,’ meaning “to excite.” They discovered the first hormone, secretin, which is produced in the small intestine and stimulates the pancreas to release digestive juices. Since then, research has uncovered a vast array of hormones, each with unique functions and roles in maintaining homeostasis, from insulin regulating blood sugar levels to estrogen controlling reproductive functions.
- The endocrine system is structurally diverse, with glands that can contain multiple types of secretory cells, each producing different hormones. These hormones may act locally or travel great distances through the bloodstream, influencing various physiological processes, including metabolism, growth, immune function, and mood. Therefore, the proper functioning of hormones is vital for overall health and well-being.
Definition of Hormones
Hormones are chemical messengers produced by endocrine glands that travel through the bloodstream to regulate various bodily functions by interacting with specific target cells or organs.
Characteristics or properties of hormone
Below are some key characteristics of hormones:
- Synthesis and Release: Hormones are produced by specific endocrine tissues or glands, such as the thyroid, pancreas, or adrenal glands. After synthesis, they are directly released into the bloodstream for distribution throughout the body.
- Target Specificity: Hormones act on specific target tissues or organs that possess receptors capable of binding to the hormone. This binding alters the function or activity of the target tissue in a controlled manner.
- Ablation and Deficiency Symptoms: If a hormone-producing gland is removed or damaged (a process known as ablation), the organism will exhibit symptoms related to the deficiency of that hormone. This indicates the essential role of the hormone in normal bodily functions.
- Replacement Therapy: Reintroducing or replacing the ablated hormone-producing tissue in another part of the body can reverse the deficiency symptoms. Similarly, administering the hormone itself through injections can relieve the symptoms caused by its absence.
- Low Molecular Weight: Hormones typically have low molecular weights, which allows them to travel easily through the bloodstream and reach their target tissues efficiently.
- High Solubility and Diffusion Rate: Hormones are small, soluble molecules with a high rate of diffusion, which enables them to move quickly through the blood to their target cells. However, their effects do not remain constant and may fluctuate based on environmental or physiological conditions.
- Effective at Low Concentrations: Hormones are highly potent and can trigger significant biological responses even at very low concentrations. This ensures that a minimal amount of hormone can regulate important body functions.
- Transport Through Blood: Hormones travel throughout the body via the circulatory system. This allows them to reach distant target tissues that are often located far from the glands where they were produced.
- Action at a Distance: The site where a hormone is produced is typically different from the site where it exerts its effects. Hormones travel to distant tissues or organs to perform their regulatory roles, acting at specific target sites.
- Non-Specific for Organisms: While hormones are highly specific in their action within the body, they may influence biological processes in other individuals of the same or different species under certain circumstances.
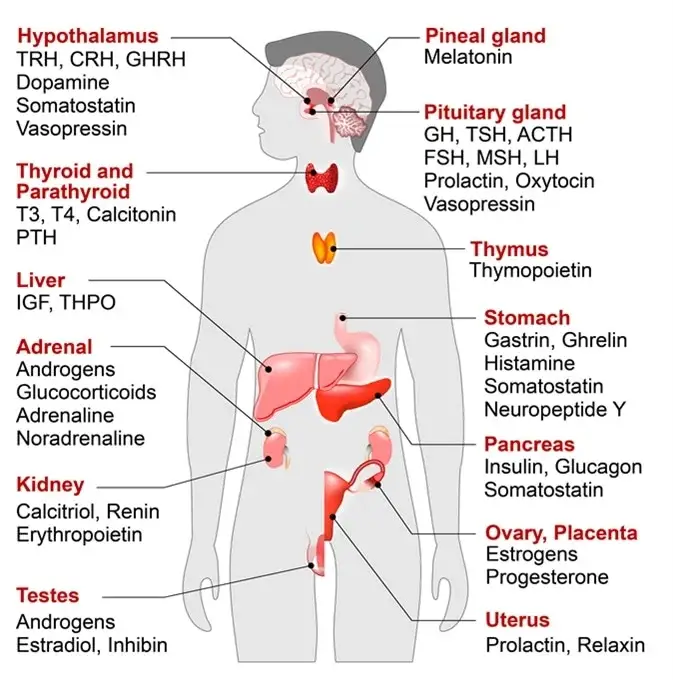
Endocrine Glands and Their Major Hormones
| Endocrine Gland | Associated Hormones | Chemical Class | Effect |
|---|---|---|---|
| Pituitary (anterior) | Growth hormone (GH) | Peptide | Promotes growth of body tissues |
| Pituitary (anterior) | Prolactin (PRL) | Peptide | Promotes milk production |
| Pituitary (anterior) | Thyroid-stimulating hormone (TSH) | Peptide | Stimulates thyroid hormone release |
| Pituitary (anterior) | Adrenocorticotropic hormone (ACTH) | Peptide | Stimulates hormone release by adrenal cortex |
| Pituitary (anterior) | Follicle-stimulating hormone (FSH) | Peptide | Stimulates gamete production |
| Pituitary (anterior) | Luteinizing hormone (LH) | Peptide | Stimulates androgen production by gonads |
| Pituitary (posterior) | Antidiuretic hormone (ADH) | Peptide | Stimulates water reabsorption by kidneys |
| Pituitary (posterior) | Oxytocin | Peptide | Stimulates uterine contractions during childbirth |
| Thyroid | Thyroxine (T4), Triiodothyronine (T3) | Amine | Stimulate basal metabolic rate |
| Thyroid | Calcitonin | Peptide | Reduces blood Ca²⁺ levels |
| Parathyroid | Parathyroid hormone (PTH) | Peptide | Increases blood Ca²⁺ levels |
| Adrenal (cortex) | Aldosterone | Steroid | Increases blood Na⁺ levels |
| Adrenal (cortex) | Cortisol, Corticosterone, Cortisone | Steroid | Increase blood glucose levels |
| Adrenal (medulla) | Epinephrine, Norepinephrine | Amine | Stimulate fight-or-flight response |
| Pineal | Melatonin | Amine | Regulates sleep cycles |
| Pancreas | Insulin | Peptide | Reduces blood glucose levels |
| Pancreas | Glucagon | Peptide | Increases blood glucose levels |
| Testes | Testosterone | Steroid | Stimulates development of male secondary sex characteristics and sperm production |
| Ovaries | Estrogens and Progesterone | Steroid | Stimulate development of female secondary sex characteristics and prepare the body for childbirth |
Classification of Hormones
Types of hormones on the basis of the distance between the site of synthesis to target site or cell
Hormones can be classified based on the distance between their site of synthesis and their target cells. These types of hormones regulate various processes by either acting on distant organs or influencing cells nearby. Below are the main types of hormones based on the proximity of their action:
- Endocrine Hormones:
Endocrine hormones act on cells located far from their site of production. After synthesis by endocrine cells, they are released into the bloodstream, where they travel long distances to reach their target tissues or organs. These hormones typically produce slower responses, but the effects are long-lasting. For example, follicle-stimulating hormone (FSH) and luteinizing hormone (LH) are produced by the anterior pituitary gland and travel through the bloodstream to regulate reproductive organs like the ovaries and testes. - Paracrine Hormones:
Paracrine hormones act on nearby cells that are adjacent to the cells that produce them. These local hormones are released into the extracellular fluid (ECF) and produce rapid but short-lived responses. An example is somatostatin, a hormone secreted by delta (δ) cells in the pancreas. It inhibits the secretion of insulin from beta (β) cells and glucagon from alpha (α) cells, which are located close to the site of somatostatin production. - Autocrine Hormones:
Autocrine hormones act on the same cells that produce them or on cells of the same type. These hormones typically influence processes within the producing cell itself. For instance, insulin-like growth factor 1 (IGF1), also known as somatomedin C, is secreted by cells like fibroblasts and osteoblasts. IGF1 binds to receptors on the same cells that produced it, promoting cell growth and proliferation.
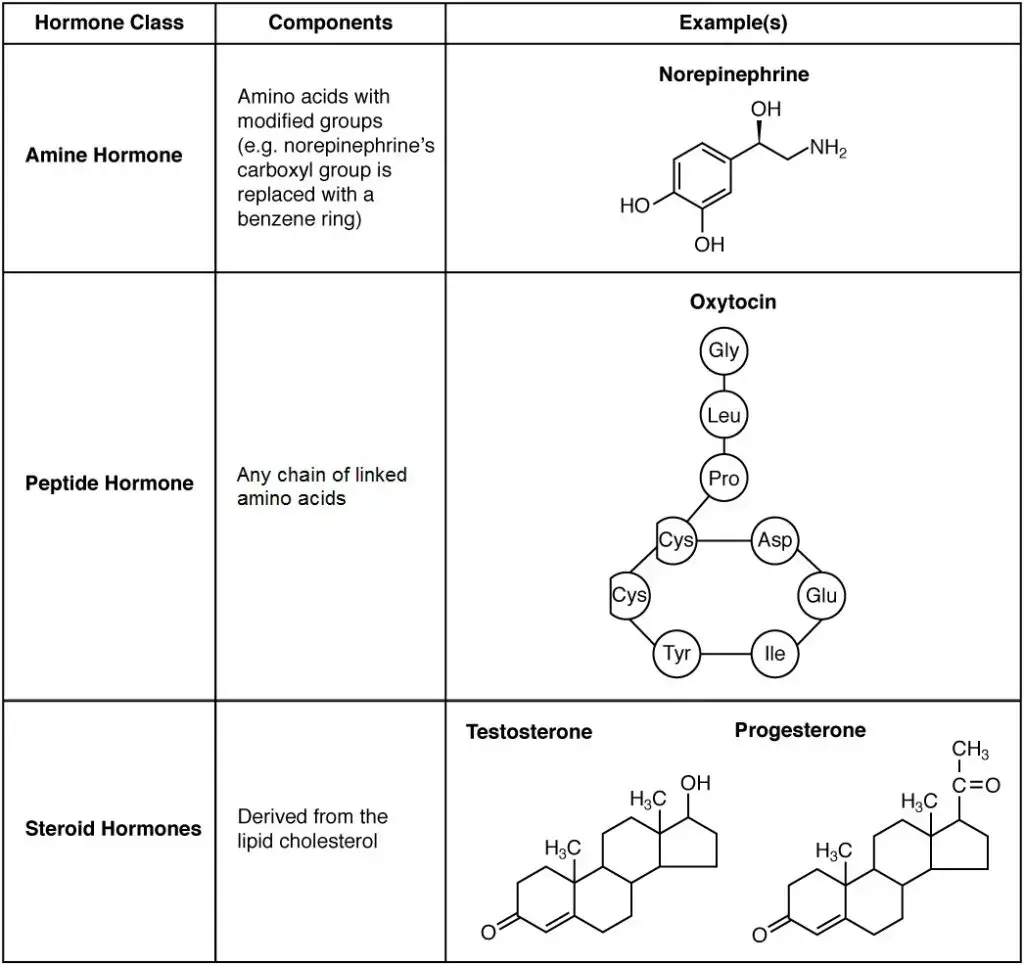
Types of hormones on the basis of their chemical nature
Hormones can be classified based on their chemical nature, which dictates their solubility, structure, mode of transport, and the way they interact with target cells. Understanding these types is key to grasping how different hormones regulate bodily functions. Below are the major types of hormones based on their chemical nature:
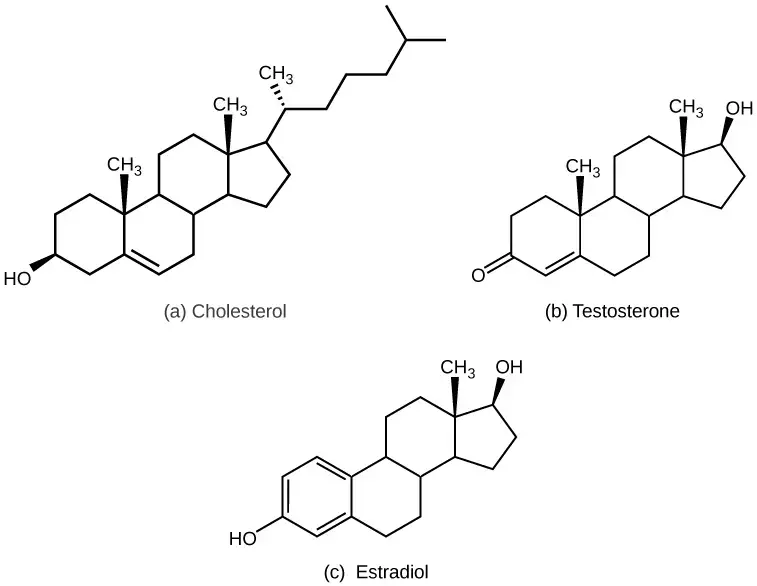
- Steroid Hormones:
Steroid hormones are lipid-soluble and derived from cholesterol. Due to their hydrophobic nature, they require carrier proteins to travel through the bloodstream. These hormones easily cross the lipid bilayer of target cells and bind to intracellular receptors, eliciting long-lasting effects. Examples of steroid hormones include:- Testosterone and Dihydrotestosterone (Androgens): Regulate male characteristics and reproductive functions.
- Estrogens (Estradiol, Estrone, Estriol): Involved in female reproductive functions and development of secondary sexual characteristics.
- Progesterone (Progestogen): Plays a crucial role in pregnancy maintenance.
- Cortisol and Cortisone (Glucocorticoids): Key in regulating glucose metabolism and anti-inflammatory responses.
- Aldosterone (Mineralocorticoid): Maintains electrolyte and water balance.
- Peptide or Protein Hormones:
Peptide hormones are composed of chains of amino acids. These can range from small peptides to large proteins, which are hydrophilic and water-soluble, circulating freely in the blood. Because they cannot pass through the lipid bilayer, their receptors are located on the surface of target cells. Peptide hormones generally have short half-lives and elicit quick responses. Notable examples include:- Insulin: Regulates blood sugar levels.
- Growth Hormone (GH): Stimulates growth and cell reproduction.
- Oxytocin: Involved in childbirth and lactation.
- Follicle-Stimulating Hormone (FSH): Regulates reproductive processes.
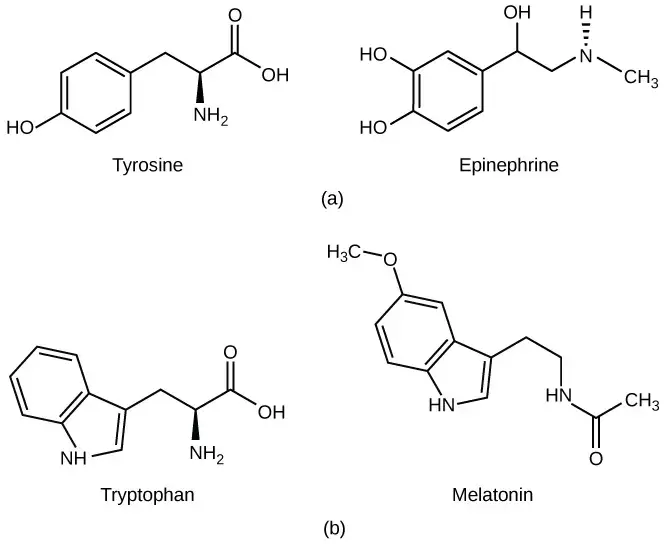
- Amino Acid-Derived Hormones:
These hormones are synthesized from amino acids like tyrosine and tryptophan. Depending on their structure, they can be either hydrophilic or hydrophobic. Hydrophilic hormones, such as catecholamines, interact with surface receptors, while hydrophobic hormones like thyroid hormones bind to intracellular receptors. Key examples include:- Epinephrine and Norepinephrine (Catecholamines): Involved in the fight-or-flight response.
- Dopamine: Functions as a neurotransmitter and hormone, playing roles in mood and movement.
- Thyroid Hormones (T3 and T4): Regulate metabolism and growth.
- Glycoprotein Hormones:
Glycoprotein hormones are composed of proteins conjugated with carbohydrate groups, such as mannose or fucose. These hormones often have complex structures and specific regulatory roles. Examples include:- Thyroid-Stimulating Hormone (TSH): Stimulates the thyroid gland.
- Luteinizing Hormone (LH): Regulates reproductive function.
- Follicle-Stimulating Hormone (FSH): Also plays a role in reproductive processes.
- Eicosanoid Hormones:
Eicosanoids are derived from fatty acids, specifically arachidonic acid. These hormones are generally short-lived and act locally, often as paracrine or autocrine signals. Eicosanoids are involved in inflammatory responses, muscle contractions, and vascular functions. Common examples include:- Prostaglandins: Regulate inflammation, muscle contractions, and cell growth.
- Thromboxanes and Prostacyclins: Play a role in blood clotting and vascular functions.
- Leukotrienes: Mediate immune responses and allergic reactions.
Types of hormones According to the mechanism of action
Hormones can also be classified based on their mechanism of action, which refers to how they interact with receptors and influence target cells. These mechanisms are crucial for understanding how hormones regulate various physiological processes in the body. Below is an explanation of hormone types according to their mechanism of action:
- Group I Hormones:
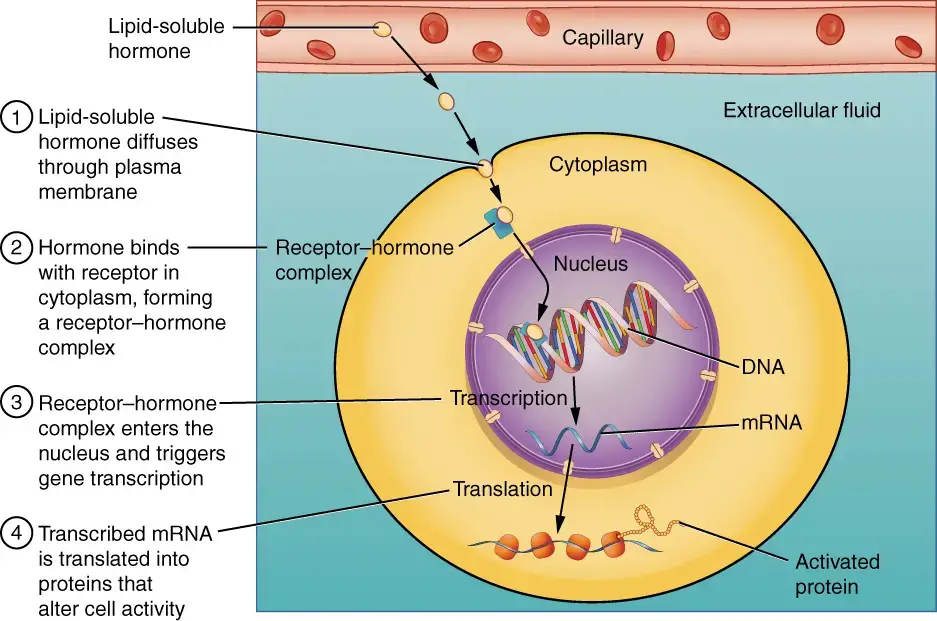
- These hormones are lipophilic, meaning they can easily pass through cell membranes. They bind to intracellular receptors, forming hormone-receptor complexes (HRCs). These complexes enter the nucleus and interact with DNA to regulate gene expression, thereby exerting their biochemical effects.
- Since these hormones are lipid-soluble, they circulate in the blood bound to transport proteins, which extends their half-lives to hours or even days. Their prolonged action allows them to maintain sustained effects in the body.
- Examples:
- Testosterone and Estrogen: Responsible for regulating reproductive functions and secondary sexual characteristics.
- Progesterone: Critical for pregnancy and maintaining the uterine lining.
- Thyroid Hormones (T3, T4): Regulate metabolism, growth, and development.
- Group II Hormones:
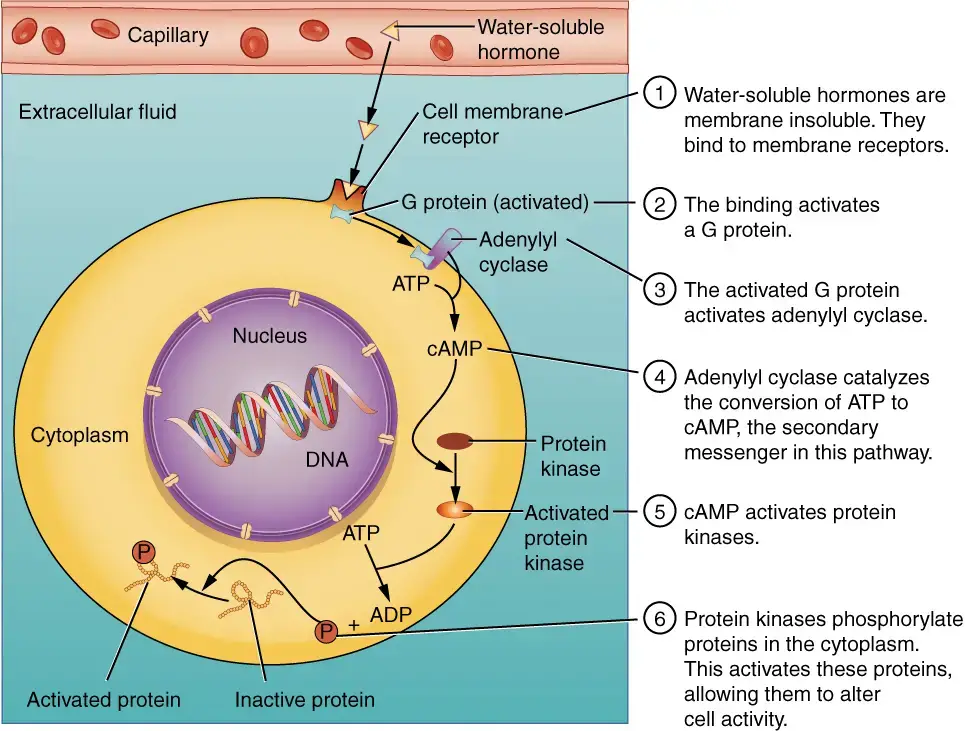
- Group II hormones are lipophobic, meaning they cannot pass through cell membranes. Instead, they bind to receptors located on the cell surface (plasma membrane). This binding triggers the release of second messengers inside the cell, which then carry out the hormone’s effects.
- These hormones generally have short half-lives, often lasting only minutes. They are usually transported in their free form, without the need for carrier proteins.
- Group II hormones are further classified based on the type of second messengers they activate:
- Hormones that use cAMP as a second messenger:
- When these hormones bind to cell surface receptors, cyclic adenosine monophosphate (cAMP) is generated as a second messenger, which then activates protein kinases, leading to various cellular responses.
- Examples:
- Luteinizing Hormone (LH): Stimulates ovulation and testosterone production.
- Follicle-Stimulating Hormone (FSH): Regulates gamete production.
- Adrenocorticotropic Hormone (ACTH): Stimulates the adrenal cortex to release cortisol.
- Hormones that use phospholipid/Inositol/Ca++ as second messengers:
- These hormones activate a different pathway, where the binding of the hormone to its receptor leads to the release of calcium ions and other molecules like inositol phosphates, which serve as second messengers to regulate cellular functions.
- Examples:
- Gonadotropin-Releasing Hormone (GnRH): Stimulates the release of FSH and LH.
- Thyrotropin-Releasing Hormone (TRH): Triggers the release of thyroid-stimulating hormone (TSH).
- Gastrin: Stimulates the secretion of gastric acid in the stomach.
- Hormones with unknown second messengers:
- In some cases, the second messengers for certain hormones remain unidentified, but their functions are well-known. These hormones still bind to cell surface receptors but do not rely on the classical cAMP or calcium pathways.
- Examples:
- Insulin: Regulates blood glucose levels by facilitating the uptake of glucose into cells.
- Oxytocin: Involved in childbirth and the stimulation of milk release during breastfeeding.
- Somatotropin (STH): Also known as growth hormone, it stimulates growth and cell reproduction.
- Hormones that use cAMP as a second messenger:
Types of hormones on the basis of their solubility in aqueous medium
Hormones can be categorized based on their solubility in aqueous mediums, which significantly affects how they travel through the bloodstream and interact with target cells. These hormones are either hydrophilic (water-soluble) or hydrophobic (lipid-soluble), and each type has unique mechanisms for reaching and acting upon their respective target sites.
- Hydrophilic Hormones (Lipophobic Hormones):
Hydrophilic hormones are soluble in water and therefore can circulate freely in the bloodstream without the need for carrier proteins. These hormones, however, cannot easily pass through the lipid bilayer of cell membranes because they are repelled by lipids. As a result, their receptors are located on the surface of the target cells. When a hydrophilic hormone binds to its receptor on the cell membrane, it triggers a signaling cascade within the cell to elicit the desired response. Peptide hormones, such as insulin and glucagon, along with certain amino acid-derived hormones like epinephrine, fall into this category. Since hydrophilic hormones cannot enter the cell directly, they rely on secondary messengers to transmit their signals within the target cell. - Hydrophobic Hormones (Lipophilic Hormones):
Hydrophobic hormones are lipid-soluble and are therefore poorly soluble in water. To travel through the bloodstream, they bind to hydrophilic carrier proteins that protect them from degradation and transport them to their target sites. Once they reach their target cells, hydrophobic hormones can easily pass through the lipid bilayer of the cell membrane due to their lipophilic nature. Their receptors are located inside the cell, often in the cytoplasm or nucleus. After the hormone detaches from its carrier protein and enters the cell, it binds to its receptor and directly influences gene expression or cellular function. Examples of hydrophobic hormones include steroid hormones such as cortisol and testosterone, as well as thyroid hormones like T3 (triiodothyronine) and T4 (thyroxine). These hormones are synthesized from cholesterol or amino acids like tyrosine, and their lipid solubility comes from their chemical structure, such as the benzene ring of tyrosine or attached iodine atoms in thyroid hormones.
Types of hormones on the basis of stimulating endocrine glands
Trophic, tropic, and non-tropic hormones are categorized based on their specific functions and target sites within the body. These classifications help in understanding how hormones regulate different physiological processes, from tissue growth to direct metabolic regulation.
- Trophic Hormones:
Trophic hormones primarily promote the growth and development of tissues and organs. They stimulate the proliferation and enlargement of cells in target tissues. For instance, thyroid-stimulating hormone (TSH) promotes the growth and function of the thyroid gland, while adrenocorticotropic hormone (ACTH) enhances the size and activity of cells in the adrenal gland. Overproduction of trophic hormones, such as TSH, can result in abnormal growth, like goiter, which is the enlargement of the thyroid gland. - Tropic Hormones:
Tropic hormones, unlike trophic hormones, target other endocrine glands, triggering them to release their hormones. These hormones act as intermediaries in hormonal cascades. For example, Gonadotropin-releasing hormone (GnRH) is produced by the hypothalamus and stimulates the anterior pituitary gland to secrete hormones like follicle-stimulating hormone (FSH) and luteinizing hormone (LH). These, in turn, act on the gonads, regulating reproductive functions. Tropic hormones are essential in maintaining communication between different endocrine glands to coordinate complex bodily processes. - Non-Tropic Hormones:
Non-tropic hormones act directly on non-endocrine target cells to elicit physiological responses. Unlike tropic hormones, they do not influence other endocrine glands. For example, glucocorticoids released from the adrenal cortex regulate glucose metabolism in the bloodstream. Similarly, antidiuretic hormone (ADH), produced by the posterior pituitary gland, acts directly on the kidneys to maintain water balance in the body. These hormones directly affect specific tissues or organs, modulating their function in response to various stimuli.
Types of hormones Based on the nature of the action
Hormones can be categorized based on the nature of their action, specifically how they exert their effects in the body. This classification helps elucidate their specific roles and mechanisms of action. The two primary types of hormones based on their action are local hormones and general hormones.
- Local Hormones:
- These hormones function primarily in a localized manner, exerting effects on nearby cells rather than traveling long distances through the bloodstream. Their action is often described as paracrine, indicating that they influence neighboring cells within the same tissue.
- Characteristics:
- Typically, local hormones act quickly and have a short duration of action, which is suitable for immediate physiological responses.
- They are produced and released in specific tissues, allowing for targeted effects without systemic involvement.
- Examples:
- Testosterone: While it has systemic effects, it can also function locally, influencing surrounding cells in the testes to support spermatogenesis and other local functions.
- Prostaglandins: These are lipid compounds derived from fatty acids that play significant roles in inflammation, pain signaling, and other local responses.
- General Hormones:
- Unlike local hormones, general hormones travel through the circulatory system to reach distant target organs and tissues. Their effects are systemic, affecting multiple physiological processes across various body systems.
- Characteristics:
- General hormones typically have a longer half-life and can maintain their effects over extended periods, making them crucial for regulating long-term physiological functions.
- They can have widespread effects and are often involved in maintaining homeostasis or initiating complex responses in the body.
- Examples:
- Thyroid Hormones (T3 and T4): These hormones regulate metabolism and energy production throughout the body, influencing various organs such as the heart, liver, and muscles.
- Insulin: Released from the pancreas, insulin plays a critical role in regulating blood glucose levels by facilitating glucose uptake in tissues across the body, thereby maintaining energy balance.
Types of hormones Based on By effect
Hormones can also be classified based on their effects on physiological processes within the body. This classification highlights the diverse roles hormones play in regulating various biological functions. The primary categories based on effect include kinetic hormones, metabolic hormones, and morphogenetic hormones.
- Kinetic Hormones:
- Kinetic hormones are primarily responsible for facilitating movement and physiological changes in the body. They trigger various activities such as color migration in certain cells, muscle contractions, and glandular secretions.
- Characteristics:
- These hormones often have immediate effects, enabling rapid physiological responses to stimuli.
- They can influence a wide range of actions, including those involving the muscular, integumentary, and endocrine systems.
- Examples:
- Melanocyte-Stimulating Hormone (MSH): Involved in regulating skin pigmentation by stimulating the production of melanin in melanocytes.
- Epinephrine (Adrenaline): A key hormone in the “fight or flight” response, it enhances muscle contraction and increases heart rate and blood flow to muscles.
- Pineal Hormones: These hormones, particularly melatonin, influence circadian rhythms and sleep patterns, affecting various physiological processes.
- Metabolic Hormones:
- Metabolic hormones play a crucial role in regulating the body’s metabolism and maintaining energy balance. They influence how the body utilizes nutrients and manages energy stores.
- Characteristics:
- These hormones often work to either increase or decrease metabolic rates, depending on the body’s needs.
- They are critical in processes such as glucose regulation, fat metabolism, and overall energy homeostasis.
- Examples:
- Glucagon: Secreted by the pancreas, glucagon raises blood glucose levels by promoting glycogenolysis and gluconeogenesis in the liver.
- Insulin: Also produced by the pancreas, insulin facilitates the uptake of glucose by cells, lowering blood sugar levels and enabling cellular respiration.
- Parathyroid Hormone (PTH): Regulates calcium and phosphate metabolism, influencing bone health and metabolic functions related to minerals.
- Morphogenetic Hormones:
- Morphogenetic hormones are essential for growth, differentiation, and development within the body. They orchestrate the processes that lead to structural changes and maturation in various tissues.
- Characteristics:
- These hormones are vital during developmental stages and also play roles in tissue repair and regeneration.
- They often influence the growth of organs and systems, establishing appropriate cellular functions.
- Examples:
- Follicle-Stimulating Hormone (FSH): Promotes growth and maturation of ovarian follicles in females and stimulates spermatogenesis in males.
- Somatotropic Hormone (STH) or Growth Hormone (GH): Stimulates growth, cell reproduction, and regeneration in humans and other animals.
- Thyroid Hormones (T3 and T4): Regulate various metabolic processes and are essential for normal growth and development, particularly in the nervous system.
Synthesis of Hormones
Hormone synthesis is a complex, multi-step process regulated at the genetic level. Depending on the type of hormone—peptide, amine, or steroid—the synthesis pathway varies. Peptide hormones follow a specific gene expression pathway, while non-peptide hormones like thyroid and steroid hormones involve distinct biochemical processes.
- Synthesis of Peptide Hormones:
- Peptide hormones are synthesized in the rough endoplasmic reticulum (ER), where mRNA translation begins. This mRNA is coded by specific genes, which direct the production of a precursor protein called a prohormone or preprohormone.
- The prohormone contains an additional sequence known as a signal or leader peptide at its amino terminal, which helps guide it across the ER membrane.
- Once in the ER, the signal peptide is removed, allowing the prohormone to fold into its secondary structure as it travels to the Golgi apparatus.
- In the Golgi, enzymes may further process the prohormone into a mature hormone. Additional modifications, such as the addition of carbohydrates in glycoprotein hormones like FSH and LH, may occur.
- The hormone is stored in vesicles within the cell until its release, typically through the process of exocytosis.
- Synthesis of Non-Peptide Hormones:
- Amine and steroid hormones differ from peptide hormones as they are synthesized from specific precursor molecules—tyrosine for amine hormones and cholesterol for steroid hormones.
- Inside the cells, these precursors undergo several enzymatic reactions, forming intermediate products that may also function as hormones.
- Unlike peptide hormones, amine and steroid hormones are not packaged in vesicles but instead diffuse freely across cell membranes due to their lipid solubility.
- The final hormone is either actively transported out of the cell or passively diffused into the bloodstream.
- Post-Synthesis Hormone Modifications:
- Some hormones may be converted into their active forms after they leave their site of synthesis. For example, a less active hormone can be activated in the bloodstream or by target tissues through enzymatic action.
- This modification allows for additional layers of control, ensuring hormones are activated only where and when needed.
What is Hormone signaling?
- Hormone signaling is a fundamental process where hormones are secreted directly into the extracellular space by endocrine glands. These hormones enter the bloodstream through capillaries and are transported to target cells throughout the body. This system allows hormones to affect tissues and organs far from their origin, creating both local and systemic effects.
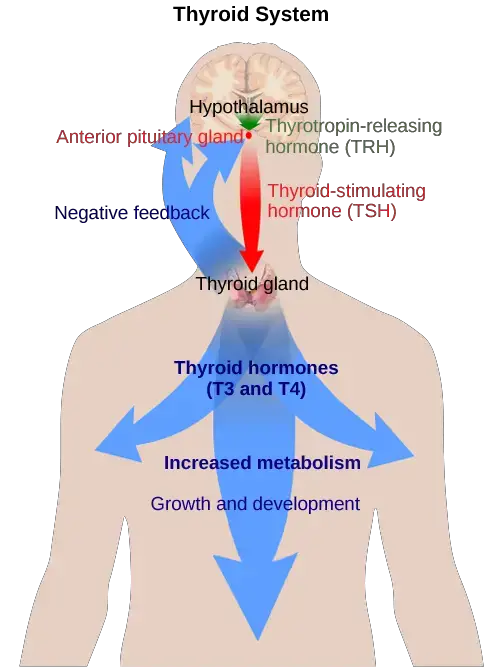
- For example, in the thyroid gland, hormone-producing cells called thyrocytes release thyroid hormones, which travel through the blood to regulate metabolism in distant tissues. Hormones exit their origin cells via exocytosis or other transport mechanisms, ensuring efficient delivery. Different tissues have varied responses to the same hormone, as seen in conditions like diabetes, where insulin affects multiple body systems.
- The complexity of hormone signaling lies in how hormones interact with target cells. Hormones either bind to receptors on the cell membrane or enter the cell to interact with cytoplasmic receptors. This binding initiates a cascade of events, ultimately leading to changes in gene expression. Feedback mechanisms, such as negative feedback loops, help regulate hormone production, ensuring homeostasis.
- Lipid-soluble hormones, like steroid hormones, can pass through the plasma membrane and activate nuclear receptors inside the cell. This direct interaction with the nucleus plays a crucial role in controlling specific cellular functions and regulating overall physiological processes.
Steps of hormone signaling
Here are the essential steps involved in hormone signaling:
- Synthesis of the Hormone:
- Hormones are synthesized by specialized cells within endocrine glands or tissues. Each hormone is produced in response to specific physiological needs, such as stress, growth, or changes in metabolic states.
- For instance, the adrenal glands synthesize cortisol in response to stress signals.
- Storage and Secretion of the Hormone:
- After synthesis, hormones may either be stored in secretory vesicles or immediately released into the bloodstream. The release of the hormone depends on the signals that trigger secretion, such as neural inputs or changes in blood composition.
- For peptide hormones like insulin, storage in vesicles is common, allowing rapid release when blood glucose levels rise.
- Transport to Target Cells:
- Once secreted, hormones travel through the bloodstream to reach their target cells, tissues, or organs. Hormones can be transported in a free form (as in the case of hydrophilic hormones) or bound to carrier proteins (as seen with hydrophobic hormones like steroids).
- Transport is crucial to ensure that hormones reach distant parts of the body, such as thyroid hormone traveling from the thyroid gland to regulate metabolism in peripheral tissues.
- Recognition by Receptors:
- Hormones exert their effects by binding to specific receptors located either on the surface of target cells or inside the cell. Hydrophilic hormones (such as peptide hormones) bind to receptors on the cell membrane, while hydrophobic hormones (like steroid hormones) enter the cell and bind to intracellular receptors.
- The binding of a hormone to its receptor initiates a conformational change that activates downstream signaling pathways within the target cell.
- Signal Transduction and Amplification:
- After the hormone binds to its receptor, a cascade of signaling events occurs inside the target cell. This process, known as signal transduction, amplifies the initial hormone signal to elicit a significant biological response.
- For instance, in the case of G-protein-coupled receptors (GPCRs), binding of the hormone activates secondary messengers like cAMP, which further amplifies the signal and activates cellular processes such as enzyme activity or gene expression.
- Cellular Response:
- Once the signal is amplified, the cell produces the desired physiological response, which may include alterations in gene expression, changes in enzymatic activity, or modifications in cellular function.
- For example, insulin binding to its receptor on muscle cells stimulates glucose uptake and glycogen synthesis, regulating blood sugar levels.
- Feedback Mechanism:
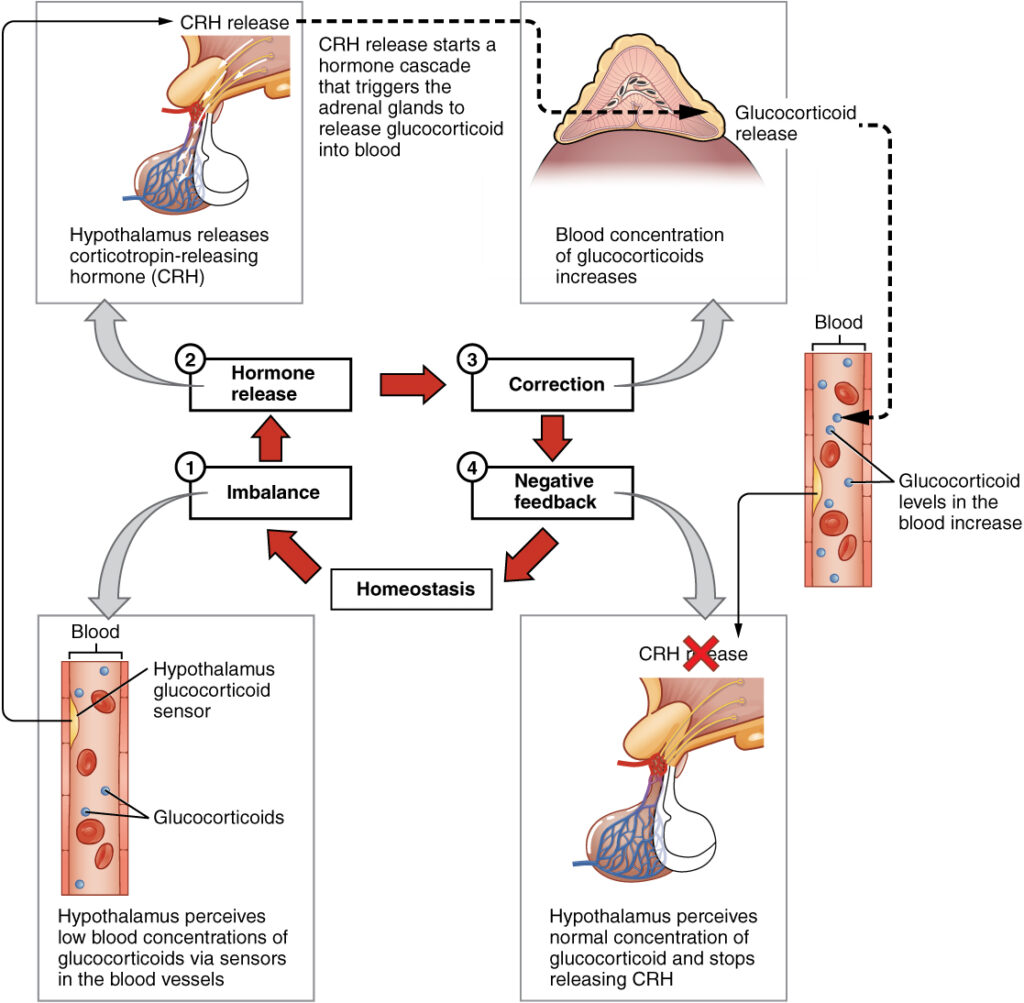
- To maintain balance and prevent excessive hormone activity, feedback mechanisms are in place. Negative feedback loops are most common, where the outcome of the hormone signaling inhibits further hormone production.
- For instance, elevated cortisol levels inhibit the release of corticotropin-releasing hormone (CRH) from the hypothalamus, reducing cortisol production and preventing an over-response.
Hormone classes
Hormones are vital chemical messengers in the body, responsible for regulating numerous physiological processes. Based on their chemical composition, hormones can be classified into three main categories: peptide hormones, lipid-derived hormones, and monoamine hormones. Each of these classes has distinct characteristics that determine how they function, their solubility, and their method of signaling within the body.
- Peptide Hormones:
- Peptide hormones are composed of amino acids and can exist either as short peptide chains or as long proteins. They may also include additional chemical groups, such as carbohydrates, making them glycoproteins in some cases.
- Characteristics:
- These hormones are hydrophilic (water-soluble), meaning they cannot pass through the lipid bilayer of cell membranes directly. Therefore, their receptors are located on the cell surface.
- Due to their hydrophilic nature, peptide hormones are often transported freely in the bloodstream without the need for carrier proteins.
- Their actions are typically fast-acting, with relatively short half-lives, which means they are quickly broken down and removed from circulation.
- Examples:
- Insulin: A protein hormone produced by the pancreas that regulates blood glucose levels by facilitating cellular uptake of glucose.
- Oxytocin: A small peptide hormone that stimulates uterine contractions during childbirth and promotes lactation.
- Lipid-Derived Hormones:
- Lipid-derived hormones are synthesized from cholesterol or fatty acid precursors, which gives them their lipid-soluble properties.
- Characteristics:
- These hormones are hydrophobic (lipid-soluble), allowing them to easily diffuse through the lipid bilayer of cell membranes. As a result, they typically bind to intracellular receptors located within the cytoplasm or nucleus of target cells.
- Due to their hydrophobic nature, lipid hormones must bind to carrier proteins in the bloodstream to be transported effectively.
- Lipid-derived hormones tend to have longer half-lives, remaining in circulation for extended periods before being broken down.
- Examples:
- Steroid Hormones: These hormones, such as testosterone and cortisol, are derived from cholesterol and play crucial roles in regulating metabolism, immune function, and reproduction.
- Eicosanoids: These lipid hormones, derived from fatty acids in the plasma membrane, such as prostaglandins, regulate inflammatory responses and other local tissue effects.
- Monoamine Hormones:
- Monoamine hormones are derived from aromatic amino acids like tyrosine, phenylalanine, and tryptophan. They include important signaling molecules in both the central nervous system and peripheral tissues.
- Characteristics:
- Depending on their structure, monoamines can be either water-soluble (hydrophilic) or lipid-soluble (hydrophobic). This distinction determines whether their receptors are located on the cell surface or within the cell.
- Monoamines often act as neurotransmitters as well as hormones, influencing both neural and hormonal signaling pathways.
- Examples:
- Epinephrine (Adrenaline): A hormone and neurotransmitter derived from tyrosine that is crucial for the body’s “fight or flight” response.
- Serotonin: A monoamine derived from tryptophan, involved in mood regulation and gastrointestinal function.
Transport and Metabolism of Hormones
The transport and metabolism of hormones are critical processes that determine their efficacy and duration of action within the body. After hormones are synthesized and released, they must navigate the bloodstream to exert their physiological effects. This overview examines the modes of transport, the role of carrier proteins, and the metabolic processes that regulate hormone levels.
- Modes of Transport:
- Hormones can circulate in the bloodstream in two primary forms: free (unbound) and bound to carrier proteins.
- Amines, Peptides, and Protein Hormones:
- These types of hormones typically circulate in a free form, allowing them to quickly reach their target tissues and initiate responses.
- Steroids and Thyroid Hormones:
- These hormones are generally bound to transport proteins. This binding helps to stabilize their plasma concentrations and prolong their half-life.
- Common carrier proteins include:
- Thyroid Hormone-Binding Globulin (TBG): Transports thyroid hormones.
- Testosterone-Binding Globulin (TeBG): Transports testosterone.
- Cortisol-Binding Globulin (CBG): Transports cortisol.
- An exception is insulin-like growth factors, which, although they are polypeptides, circulate attached to specific proteins, emphasizing the diversity in hormone transport mechanisms.
- Mechanisms of Hormone Action:
- Upon reaching their target tissues, hormones can trigger immediate physiological responses or initiate longer-term changes.
- This action underscores the necessity for hormones to be inactivated after their physiological functions are fulfilled; otherwise, continuous activation could lead to pathological conditions.
- Metabolic Clearance Rate (MCR):
- The MCR quantifies the rate at which a hormone is removed from the plasma, reflecting its effectiveness and duration of action.
- Under steady-state conditions, MCR is defined as the volume of plasma cleared of the hormone per unit of time, providing a critical measure for understanding hormonal dynamics.
- The plasma half-life of a hormone is inversely related to its MCR. A higher MCR indicates a shorter half-life, meaning the hormone is rapidly cleared from circulation.
- Sites of Hormone Clearance:
- The liver and kidneys are the primary organs responsible for hormone clearance. They utilize various enzymatic degradation processes to metabolize hormones effectively.
- These processes include:
- Hydrolysis: The breakdown of compounds due to reaction with water.
- Oxidation: The addition of oxygen or the removal of hydrogen.
- Hydroxylation: The introduction of hydroxyl groups into the hormone structure.
- Methylation: The addition of methyl groups, often altering the hormone’s activity.
- Decarboxylation: The removal of carboxyl groups, impacting hormone structure and function.
- Sulfation: The addition of sulfate groups, which can enhance solubility and excretion.
- Glucuronidation: The conjugation of glucuronic acid, facilitating urinary excretion.
- It is noteworthy that less than 1% of circulating hormones are typically excreted unchanged in urine or feces, highlighting the efficiency of the metabolic processes involved.
Patterns of Hormone Secretion
Hormone secretion is not a continuous process but rather exhibits distinct patterns characterized by episodic releases. Understanding these patterns is crucial for grasping how hormones regulate various physiological processes. The secretion of hormones follows several rhythmic patterns, each defined by its frequency and timing. Below is a detailed exploration of these patterns.
- Pulsatile Secretion:
- Most hormones are secreted in a pulsatile manner, with episodes of release that can occur every 5 to 10 minutes.
- Following each release, plasma hormone levels typically decline back toward basal values during quiescent periods.
- This cyclic pattern allows for precise regulation of hormone levels, ensuring that the body’s needs are met without constant high levels of hormones.
- Rhythmic Patterns:
- The frequency and amplitude of hormone release can vary widely depending on physiological demands and regulatory mechanisms.
- Circadian Rhythm:
- Hormones that are released approximately every 24 hours follow a circadian rhythm.
- An example includes adrenocorticotropic hormone (ACTH), which peaks in the early morning and declines throughout the day, aligning with the body’s sleep-wake cycle.
- Ultradian Rhythm:
- Hormones exhibiting a frequency of release occurring more than once every 24 hours but less than once every hour are termed ultradian rhythms.
- This includes certain hormones whose release can vary throughout the day based on metabolic demands or environmental cues.
- Circhoral Rhythm:
- A specific type of ultradian rhythm, circhoral secretion refers to hormone release occurring approximately every hour.
- This regularity aids in maintaining consistent physiological functions throughout the day.
- Circatrigintan Rhythm:
- Some hormones, like gonadotropins, follow a monthly release pattern, occurring approximately every 30 days.
- This is especially relevant in female reproductive physiology, where hormonal fluctuations play a critical role in the menstrual cycle.
- Circannual Rhythm:
- Hormones with a yearly periodicity, termed circannual rhythms, exhibit changes over months or seasons.
- These patterns are often related to reproductive cycles, metabolic adjustments, and adaptations to seasonal environmental changes.
- Long-Term Variations:
- Hormones such as thyroxine demonstrate changes in plasma levels over extended periods, reflecting the body’s long-term regulatory needs rather than short-term responses.
- Influence of Feedback Mechanisms:
- The secretion patterns of hormones are influenced by feedback mechanisms, particularly negative feedback.
- Removal of an inhibitory signal can lead to increased amplitude and frequency of hormone secretion, illustrating the dynamic nature of hormonal control.
- This responsiveness is essential for adjusting hormone levels based on the body’s current physiological state and external stimuli.
Control of Hormone Secretion
The regulation of hormone secretion is a complex and finely tuned process essential for maintaining homeostasis and coordinating bodily functions. Hormonal levels are influenced by a variety of factors, including neural signals, other hormones, and feedback mechanisms. Below is a detailed overview of the control mechanisms governing hormone secretion.
- Neural Control:
- Certain endocrine secretions are directly regulated by nerve impulses, indicating the importance of the nervous system in endocrine function.
- For instance, during periods of stress or emotional response, the splanchnic nerve triggers the adrenal medulla to synthesize and release catecholamines, such as adrenaline and noradrenaline.
- Additionally, osmoreceptors in the hypothalamus can evoke the release of vasopressin from the neurohypophysis (posterior pituitary) when changes in osmotic pressure are detected.
- Neural impulses originating from brain structures, including the hippocampus and amygdala, can stimulate the release of neurotransmitters, such as acetylcholine and biogenic amines, which in turn regulate the secretion of hypothalamic hormones, including growth hormone-releasing hormone (GHRH), corticotropin-releasing hormone (CRH), and thyrotropin-releasing hormone (TRH).
- Endocrine Control:
- Hormones often regulate the secretion of other hormones, establishing a hierarchical control system among endocrine glands.
- For example, adrenocorticotropic hormone (ACTH) from the anterior pituitary stimulates the release of adrenal cortex hormones, such as cortisol. Similarly, gonadotropins (GTH) stimulate the secretion of gonadal hormones, and thyrotropin (TSH) promotes thyroid hormone release.
- These tropic hormones from the anterior pituitary are themselves regulated by hypothalamic hormones (CRH, GnRH, TRH), creating a feedback loop that ensures hormonal balance and response to physiological demands.
- Feedback Controls:
- Feedback mechanisms play a crucial role in modulating hormone secretion, ensuring that hormone levels remain within optimal ranges.
- Negative Feedback Control:
- In negative feedback loops, an increase in the concentration of a hormone can inhibit further secretion of that hormone. This is a common mechanism used to maintain homeostasis.
- For example, elevated cortisol levels from the adrenal cortex can suppress the release of both pituitary ACTH and hypothalamic CRH, ultimately reducing cortisol secretion.
- Additionally, high levels of tropic hormones can inhibit their corresponding releasing factors from the hypothalamus, exemplifying a short-loop feedback mechanism.
- Furthermore, certain metabolites and ions can influence hormone release through feedback. For instance, increased serum calcium levels lead to decreased secretion of parathyroid hormone, while elevated blood glucose levels can result in decreased glucagon secretion.
- Positive Feedback Control:
- Conversely, positive feedback mechanisms stimulate hormone secretion in response to elevated levels of a hormone or metabolite.
- A classic example of positive feedback occurs during the menstrual cycle, where a surge in estradiol triggers a sharp increase in luteinizing hormone (LH) secretion from the anterior pituitary.
- Similarly, high serum calcium concentrations can stimulate the release of calcitonin from the thyroid gland.
- Some hormones may also exert a form of auto-inhibition, wherein they inhibit their own synthesis within the cells, adding another layer of regulation to their secretion.
General Mechanisms of Hormone Action
The action of hormones in the body relies on intricate mechanisms that allow them to interact effectively with target cells. Each hormone, produced by various glands, must bind to specific receptors on target cells to exert its effects. Understanding these mechanisms is crucial for grasping how hormones regulate numerous physiological processes. Below is an overview of the general mechanisms of hormone action.
- Hormone-Receptor Interaction:
- Hormones act as signaling molecules that initiate responses in target cells through specific interactions with receptors.
- These receptors are specialized proteins located in various cellular compartments, including the plasma membrane, cytosol, and nucleus.
- Each receptor is characterized by a unique hormone-binding site that recognizes and binds specific hormones, thereby initiating a signaling cascade.
- Types of Receptors:
- Receptors can be broadly categorized into two types: membrane-bound receptors and intracellular receptors.
- Membrane-bound receptors are located on the cell surface and interact with hydrophilic (water-soluble) hormones, such as peptides and catecholamines.
- Intracellular receptors are found within the cell, often in the cytoplasm or nucleus, and typically bind lipophilic (fat-soluble) hormones, such as steroid hormones and thyroid hormones.
- Receptors can be broadly categorized into two types: membrane-bound receptors and intracellular receptors.
- Recognition and Specificity:
- A primary function of hormone receptors is to recognize specific hormones, distinguishing them from other molecules in the bloodstream or extracellular fluid.
- For instance, insulin receptors specifically recognize insulin, facilitating its action in promoting glucose uptake in target cells such as hepatocytes, adipocytes, and muscle cells.
- Signal Transduction:
- Upon hormone binding, the receptor undergoes a conformational change that activates intracellular signaling pathways, leading to various cellular responses.
- This process can involve second messengers, such as cyclic AMP (cAMP) or calcium ions, which amplify the signal and elicit a physiological response.
- Tissue Response:
- Not all cells express the same receptors; thus, hormone action is tissue-specific. This selective expression allows for diverse physiological responses to the same hormone.
- For example, while insulin promotes glucose uptake in muscle and fat cells, it also has distinct effects on liver cells, emphasizing the importance of receptor distribution.
- Physiological Complementarity:
- When a hormone stimulates multiple tissues simultaneously, the varied responses can work synergistically to achieve a coordinated physiological effect.
- For example, the action of estradiol on its specific estrogen receptors leads to distinct effects in different tissues, such as promoting ovulation in the ovaries and influencing bone density.
- Feedback Regulation:
- Hormonal signaling is often regulated through feedback mechanisms, which maintain homeostasis. Negative feedback loops are common, where the end product of a hormonal action inhibits further hormone secretion.
- This regulatory mechanism ensures that hormone levels remain within physiological ranges, preventing over- or underactivity of hormonal pathways.
- Diversity of Hormonal Effects:
- Each hormone can have multiple effects across various tissues. For instance, glucagon primarily raises blood glucose levels but also influences fat metabolism in adipose tissues.
- Therefore, the interaction of hormones with their receptors can lead to complex and integrated physiological responses.
- Biological Outcomes:
- The end result of hormone-receptor interactions typically includes changes in cellular metabolism, growth, and activity. This can manifest in various forms, including alterations in gene expression, enzyme activity, and cell division.
How Hormones Work
Hormones are essential chemical messengers that regulate numerous physiological processes within the body. Their actions are highly specific and governed by intricate mechanisms that ensure appropriate responses to varying internal and external stimuli. Understanding how hormones work provides insight into their crucial roles in maintaining homeostasis and overall health.
- Receptor Specificity: Each hormone is characterized by a unique chemical structure, enabling it to bind selectively to specific hormone receptors on target cells. The number and type of receptors present on a cell can vary significantly, influencing that cell’s sensitivity to the hormone. For instance, cells with a high density of receptors for a particular hormone will exhibit a more pronounced response compared to those with fewer receptors.
- Cell-Surface Receptors: Many hormones, particularly water-soluble peptides and amines, interact with receptors located on the cell surface. These receptors are often linked to intracellular signaling pathways, initiating a cascade of biochemical events once the hormone binds. This interaction typically results in the activation or inhibition of various cellular processes through the generation of secondary messengers, which amplify the signal within the cell.
- Intracellular Receptors: Conversely, lipid-soluble hormones, such as steroids, have the ability to diffuse across the cell membrane. Once inside, they bind to receptors found in the cytoplasm or nucleus of target cells. The hormone-receptor complex formed then translocates to the nucleus, where it directly influences gene transcription, thus regulating the synthesis of proteins essential for mediating the hormone’s effects.
- Gene Transcription: Hormones that bind to intracellular receptors can function as transcription factors. These complexes attach to specific DNA sequences in the promoter regions of target genes, thereby enhancing or repressing gene transcription. The resulting alterations in gene expression lead to changes in cellular function and the production of proteins required for the hormone’s biological effects.
- Modulation of Cellular Processes: The binding of hormones to their receptors orchestrates a wide array of cellular processes. These can include modulation of metabolic activities, enzymatic reactions, ion transport mechanisms, cellular growth, proliferation, and the secretion of other hormones or signaling molecules. Each of these processes is finely tuned to respond to the needs of the organism.
- Feedback Mechanisms: Hormonal regulation frequently employs feedback loops to maintain homeostasis within the body. For instance, elevated levels of a specific hormone can induce down-regulation, leading to a decrease in the number of available receptors on target cells. This adaptive response reduces cellular sensitivity to the hormone, thereby preventing overstimulation. Conversely, when hormone levels are low, up-regulation may occur, increasing the receptor density and enhancing sensitivity to the hormone.
- Integration of Multiple Signals: Target cells are often exposed to signals from various hormones simultaneously, resulting in complex regulatory mechanisms. Hormones can work synergistically to enhance cellular responses or may exert opposing effects to balance physiological processes. This integration allows the body to finely tune its responses to maintain optimal function in a constantly changing environment.
Pathways Involving Intracellular Hormone Receptors
- Intracellular hormone receptors play a crucial role in mediating the effects of lipid-derived (soluble) hormones within target cells. Unlike water-soluble hormones that bind to cell surface receptors, lipid-derived hormones, such as steroid hormones, are able to diffuse across the membranes of endocrine cells. Once outside the cell, these hormones bind to transport proteins that keep them soluble in the bloodstream, facilitating their transport to target cells.
- Upon reaching the target cell, the hormone molecules are released from the carrier proteins and can freely diffuse across the lipid bilayer of the cell’s plasma membrane. This ability to pass through the plasma membrane is a unique characteristic of lipid-derived hormones, as they are able to interact with intracellular receptors.
- Intracellular receptors for lipid-derived hormones can be found in two primary locations within the cell: the cytoplasm or the nucleus. In the cytoplasm, the hormone-receptor complex interacts with receptors residing in this compartment. Alternatively, some receptors are located within the nucleus itself.
- Once the hormone binds to its specific receptor, a complex is formed. This hormone-receptor complex initiates a series of intracellular signaling pathways that ultimately lead to the regulation of gene expression. The complex acts as a transcription regulator, influencing the synthesis of mRNA molecules from specific genes.
- By altering gene expression, the hormone-receptor complex determines the amount of corresponding protein that is synthesized within the cell. This protein may contribute to structural changes in the cell or act as enzymes that catalyze important chemical reactions. Ultimately, the regulation of specific cell processes is achieved through the modulation of gene expression by the hormone-receptor complex.
- While steroid hormones are a well-known example of lipid-derived hormones that utilize intracellular receptors, other lipid-soluble hormones like vitamin D and thyroxine also follow a similar mechanism. These hormones, despite not being steroids, are able to diffuse across both the plasma membrane and the nuclear envelope. They subsequently bind to receptors located in the nucleus, where the hormone-receptor complex stimulates the transcription of specific genes.
Pathways Involving Cell Membrane Hormone Receptors
- Plasma membrane hormone receptors are essential for mediating the effects of amino acid-derived hormones and polypeptide hormones, which are not lipid-derived and therefore cannot diffuse through the plasma membrane of cells.
- Unlike lipid-derived hormones such as steroid hormones, which act through intracellular receptors, lipid-insoluble hormones bind to receptors located on the outer surface of the plasma membrane. These receptors are known as plasma membrane hormone receptors. When a hormone binds to its specific receptor, it initiates a signaling pathway that triggers intracellular activity and leads to the specific effects associated with the hormone.
- In this mechanism, the hormone does not enter the target cell but instead remains bound to the cell surface receptor. Similarly, the intracellular products resulting from the signaling pathway remain inside the cell. The hormone that initiates the signaling pathway is referred to as the first messenger, while the intracellular molecules involved in the signaling cascade are known as second messengers.
- One example of amino acid-derived hormones is epinephrine and norepinephrine, which bind to beta-adrenergic receptors on the plasma membrane of cells. Binding of these hormones to the receptor activates a G-protein associated with the receptor. The G-protein, when activated, stimulates the activity of an enzyme called adenylyl cyclase. Adenylyl cyclase converts ATP to cyclic AMP (cAMP), which serves as a second messenger.
- cAMP then activates a group of proteins known as protein kinases. These protein kinases catalyze phosphorylation, which involves transferring a phosphate group from ATP to a substrate molecule. Phosphorylation leads to changes in the structural orientation and activation of the substrate molecule. These activated molecules can then mediate changes in cellular processes.
- The signaling pathway initiated by hormone-receptor binding results in an amplification of the hormonal effect. The binding of a single hormone molecule to a receptor leads to the activation of multiple G-proteins, which subsequently activate adenylyl cyclase. Each molecule of adenylyl cyclase generates numerous molecules of cAMP. Additionally, protein kinases, once activated by cAMP, can catalyze multiple reactions. This amplification process allows a small amount of hormone to trigger the formation of a significant amount of cellular product.
- To regulate hormone activity and prevent overproduction of cellular products, cAMP is deactivated by an enzyme called phosphodiesterase (PDE), which is present in the cytoplasm. PDE breaks down cAMP, terminating the signaling cascade.
- The specific response of a cell to a lipid-insoluble hormone depends on the types of receptors present on the cell membrane and the substrate molecules within the cytoplasm. Cellular responses to hormone-receptor binding include alterations in membrane permeability and metabolic pathways, stimulation of protein and enzyme synthesis, and activation of hormone release.
- In summary, plasma membrane hormone receptors play a vital role in mediating the effects of lipid-insoluble hormones. Through the activation of signaling pathways and the involvement of second messengers, these receptors initiate intracellular activity and regulate various cellular processes in response to hormone binding.
Functions of hormones
Below is a detailed breakdown of the major roles of hormones in the body:
- Regulation and Homeostasis Functions:
- Hormones maintain a stable internal environment by regulating processes such as blood pressure, fluid balance, and electrolyte composition.
- Key hormones involved in homeostasis include vasopressin and aldosterone, which control water and electrolyte balance, affecting blood pressure and extracellular fluid volume.
- Parathyroid hormone (PTH), calcitonin, and 1,25-dihydroxy-vitamin D3 regulate plasma calcium and phosphate levels, ensuring proper bone health and muscle function.
- Growth and Development:
- Hormones like growth hormone (GH), thyroid hormones, and insulin-like growth factors (IGFs) are pivotal in controlling body growth and tissue development.
- GH stimulates growth through IGFs, but it requires thyroxine for optimal function. Without thyroxine, GH cannot effectively promote skeletal growth.
- Hormones also regulate early stages of cell division and differentiation, crucial for proper fetal development.
- Permissive Functions:
- Hormones enable or enhance the actions of other hormones or substances, ensuring proper cellular function and movement of materials in and out of cells.
- For example, thyroxine permits GH to exert its full effect on skeletal growth, highlighting their interconnected roles in physiological processes.
- Reproduction:
- Hormones are central to regulating reproductive processes, including the growth and function of reproductive organs, gamete production, and sexual behavior.
- Estrogens and testosterone govern the development of primary and secondary sexual characteristics. Gonadotropins like luteinizing hormone (LH) and follicle-stimulating hormone (FSH) regulate ovulation in females and spermatogenesis in males, ensuring fertility and reproductive health.
- Maintenance of Internal Environment:
- Hormones like aldosterone and vasopressin regulate the body’s fluid and electrolyte balance, which in turn controls blood pressure and cellular hydration.
- Hormonal control extends to the regulation of bone, muscle, and fat stores through a combination of PTH, estrogens, androgens, GH, insulin, glucagon, and catecholamines, ensuring the structural integrity and metabolic health of tissues.
- Energy Balance Regulation:
- Hormones play a pivotal role in maintaining energy homeostasis by balancing food intake and energy expenditure.
- The hypothalamus integrates hormonal signals to regulate both hunger and metabolic rate. Hormones like insulin, glucagon, and thyroid hormones influence how energy is stored and used by the body.
List of List of Female and Male Hormones
Here’s a list of key hormones typically associated with females and males, along with their functions:
Female Hormones
- Estrogens
- Estradiol: Main estrogen; regulates the menstrual cycle and affects secondary sexual characteristics.
- Estrone: A weaker form of estrogen; also involved in reproductive functions.
- Estriol: Produced during pregnancy; helps prepare the body for childbirth.
- Progesterone
- Prepares the uterus for implantation of a fertilized egg and maintains pregnancy.
- Follicle-Stimulating Hormone (FSH)
- Stimulates ovarian follicle development and estrogen production.
- Luteinizing Hormone (LH)
- Triggers ovulation and stimulates the production of progesterone.
- Prolactin
- Promotes milk production in breastfeeding.
- Oxytocin
- Stimulates uterine contractions during labor and milk ejection during breastfeeding.
- Testosterone (in smaller amounts)
- Contributes to libido and bone density.
Male Hormones
- Testosterone
- Primary male sex hormone; responsible for the development of male reproductive tissues and secondary sexual characteristics.
- Dihydrotestosterone (DHT)
- A derivative of testosterone; crucial for the development of male characteristics and prostate health.
- Luteinizing Hormone (LH)
- Stimulates testosterone production from Leydig cells in the testes.
- Follicle-Stimulating Hormone (FSH)
- Stimulates sperm production in the testes.
- Prolactin
- While primarily associated with females, it is also present in males, influencing reproductive and immune function.
- Dehydroepiandrosterone (DHEA)
- A precursor hormone that can be converted into testosterone and estrogens.
- Growth Hormone
- Influences growth, metabolism, and muscle mass.
Examples of Important Hormones with their Functions and Source
Hormones are crucial biochemical messengers that regulate various physiological processes in the body. Here’s a detailed list of some important hormones, along with their primary functions and sources:
- Insulin
- Source: Pancreas (beta cells of the islets of Langerhans)
- Functions:
- Lowers blood glucose levels by facilitating cellular uptake of glucose.
- Promotes the storage of glucose as glycogen in the liver and muscle.
- Stimulates lipid synthesis and storage in adipose tissue.
- Glucagon
- Source: Pancreas (alpha cells of the islets of Langerhans)
- Functions:
- Raises blood glucose levels by promoting glycogenolysis (breakdown of glycogen) in the liver.
- Stimulates gluconeogenesis (synthesis of glucose from non-carbohydrate sources).
- Facilitates lipolysis (breakdown of fats) in adipose tissue.
- Cortisol
- Source: Adrenal cortex
- Functions:
- Regulates metabolism by promoting gluconeogenesis and fat breakdown.
- Enhances the body’s response to stress and inflammation.
- Modulates immune responses.
- Thyroxine (T4)
- Source: Thyroid gland
- Functions:
- Increases the basal metabolic rate (BMR), affecting the speed of metabolic processes.
- Promotes growth and development, particularly in the nervous system.
- Enhances protein synthesis and the degradation of lipids.
- Estradiol (Estrogen)
- Source: Ovaries (also produced in the adrenal glands and fat tissues)
- Functions:
- Regulates the menstrual cycle and reproductive system in females.
- Promotes secondary sexual characteristics (e.g., breast development).
- Influences bone density and cardiovascular health.
- Testosterone
- Source: Testes (also produced in the adrenal glands)
- Functions:
- Regulates the development of male reproductive tissues and secondary sexual characteristics.
- Influences libido, muscle mass, and bone density.
- Plays a role in sperm production.
- Adrenocorticotropic Hormone (ACTH)
- Source: Anterior pituitary gland
- Functions:
- Stimulates the adrenal cortex to produce and release cortisol.
- Plays a role in stress response and regulating metabolism.
- Luteinizing Hormone (LH)
- Source: Anterior pituitary gland
- Functions:
- Triggers ovulation and the formation of the corpus luteum in females.
- Stimulates testosterone production in males.
- Follicle-Stimulating Hormone (FSH)
- Source: Anterior pituitary gland
- Functions:
- Stimulates the growth and maturation of ovarian follicles in females.
- Promotes spermatogenesis (sperm production) in males.
- Growth Hormone (GH)
- Source: Anterior pituitary gland
- Functions:
- Stimulates growth and cell reproduction.
- Promotes protein synthesis and the utilization of fat for energy.
- Plays a role in maintaining muscle mass and bone density.
- Vasopressin (Antidiuretic Hormone, ADH)
- Source: Hypothalamus (stored and released from the posterior pituitary)
- Functions:
- Regulates water balance by promoting water reabsorption in the kidneys.
- Increases blood pressure by constricting blood vessels.
- Oxytocin
- Source: Hypothalamus (stored and released from the posterior pituitary)
- Functions:
- Stimulates uterine contractions during childbirth.
- Promotes milk ejection during breastfeeding.
- Involved in social bonding and emotional responses.
Practice
[flashcard id=”59943″]
Fun Facts
- Did you know that hormones are often called “chemical messengers” because they transmit signals throughout the body to regulate various functions?
- Did you know that some hormones can act within just seconds after being released, leading to rapid changes in the body?
- Did you know that there are two main types of hormones—peptide hormones, which are water-soluble and cannot cross cell membranes, and steroid hormones, which are lipid-soluble and can easily enter cells?
- Did you know that even in very low concentrations, hormones can have powerful effects on growth, metabolism, and mood?
- Did you know that insulin and glucagon are hormones that work in opposition to each other to maintain blood sugar levels?
- Did you know that hormones like serotonin and dopamine are crucial for regulating our mood and emotions, and imbalances can lead to mood disorders?
- Did you know that cortisol is known as the “stress hormone” and is released in response to stressful situations?
- Did you know that melatonin, often referred to as the “sleep hormone,” helps regulate sleep-wake cycles by signaling to the body when it’s time to rest?
- Did you know that growth hormone, produced by the pituitary gland, is essential for normal physical growth in children and adolescents?
- Did you know that hormones like cortisol and melatonin play a key role in regulating our circadian rhythm, influencing sleep patterns and energy levels?
- Did you know that oxytocin, often called the “love hormone,” is associated with bonding and social behaviors, particularly between mothers and their children?
- Did you know that during menopause, the decline in estrogen levels can lead to symptoms like hot flashes and mood changes?
- Did you know that hormonal responses can vary significantly from person to person, influenced by genetics, environment, and lifestyle?
- Did you know that ghrelin, known as the hunger hormone, and leptin, the satiety hormone, work together to regulate appetite and energy balance?
- Did you know that hormones have played a critical role in human evolution, influencing behaviors related to survival, reproduction, and social interaction?
FAQ
What is the definition of a hormone?
Hormones are chemical messengers produced by glands in the endocrine system. They are released into the bloodstream and regulate various physiological processes in the body.
What is the structure of hormones?
Hormones can have different structures depending on their classification. They can be proteins, peptides, steroids, or amino acid derivatives.
What are the main types of hormones?
The main types of hormones are protein/peptide hormones (e.g., insulin), steroid hormones (e.g., estrogen), and amino acid derivative hormones (e.g., adrenaline).
What are the functions of hormones?
Hormones have diverse functions, including regulation of growth and development, metabolism, reproduction, mood, and stress response. They help maintain homeostasis and coordinate various body processes.
How do hormones work in the body?
Hormones bind to specific receptors on target cells or organs. This binding triggers a series of cellular responses that influence gene expression, enzyme activity, or other signaling pathways, resulting in physiological effects.
What are some examples of hormones?
Examples of hormones include insulin, estrogen, testosterone, cortisol, adrenaline, growth hormone, thyroid hormone, progesterone, and melatonin.
How are hormones regulated in the body?
Hormone production and release are regulated through complex feedback mechanisms. Negative feedback loops involve the hormone inhibiting its own production, maintaining hormone levels within a certain range.
Can hormone imbalances occur?
Yes, hormone imbalances can occur due to various factors such as diseases, hormonal disorders, stress, medications, or aging. Imbalances can lead to various health issues and may require medical intervention.
Can hormones be used as medications?
Yes, hormones can be used therapeutically to supplement or replace naturally occurring hormones. Examples include hormone replacement therapy (HRT) for menopause, insulin therapy for diabetes, and corticosteroids for inflammatory conditions.
How are hormone levels tested?
Hormone levels can be tested through blood, urine, or saliva tests. These tests can help diagnose hormonal disorders, monitor treatment efficacy, or assess fertility and reproductive health.
- https://dhingcollegeonline.co.in/attendence/classnotes/files/1603564542.pdf
- https://epgp.inflibnet.ac.in/epgpdata/uploads/epgp_content/S000035ZO/P001805/M027335/ET/1518689368M14ClassificationofHormonesQuad1.pdf
- https://www.pharmaguideline.com/2021/11/classification-of-hormones-mechanism-of-hormone-action.html
- https://www.biologydiscussion.com/hormones/hormones-definition-characteristics-and-synthesis-notes/18433
- https://www.geeksforgeeks.org/hormones/
- https://myendoconsult.com/learn/classification-of-hormones/
- https://www.biologydiscussion.com/hormones/classification-hormones/classification-of-hormones-5-categories/18429
- https://www.slideshare.net/hephz/classification-of-35705749
- https://pressbooks-dev.oer.hawaii.edu/biology/chapter/types-of-hormones/
- https://www.vedantu.com/biology/hormones
- https://oncohemakey.com/classification-of-hormones/
- https://www.ncbi.nlm.nih.gov/books/NBK20/
- https://www.notesonzoology.com/endocrinology/hormones-biology-notes-on-hormones/3496
- https://www.onlinebiologynotes.com/hormones-properties-functions-and-classification/
- https://opentextbc.ca/biology/chapter/18-1-types-of-hormones/
https://dhingcollegeonline.co.in/attendence/classnotes/files/1603564542.pdf
https://pcsstudies.com/chemical-classification-of-hormones/
https://www.pharmaguideline.com/2021/11/classification-of-hormones-mechanism-of-hormone-action.html
https://myendoconsult.com/learn/classification-of-hormones/
https://courses.lumenlearning.com/suny-ap2/chapter/hormones/
https://www.onlinebiologynotes.com/hormones-properties-functions-and-classification/
https://www.biologydiscussion.com/hormones/classification-hormones/classification-of-hormones-5-categories/18429
https://pressbooks-dev.oer.hawaii.edu/biology/chapter/types-of-hormones/
http://www.rajasinghcollegesiwan.com/Zoology/Classification%20of%20hormones.pdf
https://collegedunia.com/exams/hormones-in-animals-biology-articleid-1368