What is Electrocardiogram (ECG)?
- An electrocardiogram (ECG), often referred to as an EKG, is a vital diagnostic tool used in medicine to monitor and assess the heart’s electrical activity and rhythm throughout various cardiac cycles. This test is instrumental in revealing crucial information about the heart’s functionality, aiding healthcare professionals in diagnosing potential cardiovascular disorders and structural anomalies.
- The process of obtaining an ECG involves a technique called electrocardiography. This non-invasive procedure utilizes specialized electrodes strategically placed on the patient’s skin to capture the heart’s electrical impulses. The data collected from these electrodes is then transcribed onto a grid paper, known as the ECG strip or tracing. The resulting visual representation allows for a detailed examination of the heart’s electrical activity during contraction and relaxation phases.
- ECGs are routinely employed by cardiologists as part of a comprehensive assessment of a patient’s cardiac health. By analyzing the recorded electrical changes occurring within the heart during each cycle, healthcare professionals can identify various conditions, including arrhythmias, myocardial infarctions, and other significant cardiac pathologies. The significance of the ECG extends beyond mere monitoring; it serves as an indispensable tool for evaluating the heart’s electrical conduction system, providing insights into the heart’s overall health.
- Furthermore, the ECG is capable of detecting irregularities in heart rhythm, which can be indicative of underlying health issues. The instrument essentially captures the electric currents generated by the heart muscle, allowing for a thorough assessment of how well the heart is functioning. In this way, the ECG not only aids in diagnosing existing conditions but also plays a crucial role in preventive cardiology, enabling early intervention for at-risk patients.
Purpose of ECG Test
The electrocardiogram (ECG) test is a fundamental diagnostic tool utilized in cardiology to assess the heart’s electrical activity and rhythm. Its purposes are multifaceted, enabling healthcare providers to detect, diagnose, and monitor various cardiac conditions effectively.
- Detection of Bradycardia and Tachycardia: The ECG is instrumental in identifying abnormal heart rates, including bradycardia (slow heart rate) and tachycardia (rapid heart rate). By measuring the intervals between heartbeats, clinicians can discern the nature of these conditions.
- Symptom Investigation: It assists in determining whether symptoms such as chest pain, shortness of breath, or palpitations are related to heart problems. This evaluation is critical for timely and appropriate medical intervention.
- Heart Rhythm Assessment: The ECG helps to establish whether the heart rhythm is steady or irregular. Additionally, it can detect electrolyte imbalances that may affect cardiac function, allowing for targeted treatment strategies.
- Electrical Signal Analysis: This test provides insights into the strength and timing of electrical signals as they traverse different parts of the heart. Such information is vital for understanding the heart’s conduction system and identifying potential abnormalities.
- Detection of Heart Disorders: The ECG plays a key role in diagnosing various heart conditions, including heart attacks, arrhythmias, heart failure, congenital heart disease, and rheumatic heart disease. This comprehensive diagnostic capability is essential for effective management.
- Coronary Blood Flow Assessment: It aids in assessing coronary blood flow and the integrity of heart valves, providing crucial information regarding the heart’s perfusion status and structural health.
- Monitoring Sedated Patients: The ECG is used to monitor deeply sedated patients and those who are consciously sedated with compromised cardiovascular function. This monitoring is vital to ensure patient safety during procedures.
- Medication Monitoring: Certain medications affecting heart function require close monitoring through ECG to assess their effectiveness and detect potential adverse effects.
- Exercise Electrocardiography: This specialized application involves assessing heart function during exercise. It is particularly valuable for determining the correct exercise prescription, investigating angina, evaluating patients post-myocardial infarction, and conducting postoperative examinations after bypass surgery.
- Metabolic Disorder Evaluation: ECG can also assist in the evaluation of metabolic disorders and blunt cardiac trauma, providing insights that guide treatment decisions.
- Role in Cardiopulmonary Resuscitation (CPR): The ECG is vital during CPR, as it helps to identify the underlying cardiac rhythm and determine appropriate interventions.
- Anesthesia Monitoring: It is essential in monitoring patients under anesthesia during surgery, as well as in preoperative, intraoperative, and postoperative settings. This monitoring helps ensure that cardiovascular function remains stable throughout the surgical process.
- Sports Physical Exams: Finally, ECG is employed during sports physical examinations to rule out cardiomyopathy, thus ensuring that athletes are fit to participate in physical activities safely.
Working principle of electrocardiograph/Electrocardiogram
- The working principle of an electrocardiograph (ECG) is grounded in the concept that contracting cardiac muscle fibers generate minute electrical currents. These currents can be detected and measured using electrodes strategically placed on the patient’s body. The arrangement of these electrodes is crucial, as it allows for the accurate capture of the heart’s electrical activity.
- For a standard resting electrocardiogram, the patient lies in a supine position, facilitating ease of access for electrode placement. Electrodes are affixed to the skin on the arms, legs, and specifically at six designated positions on the chest, directly above the heart. The attachment of electrodes is often aided by a conductive gel, which enhances the quality of the electrical signal captured by reducing skin resistance.
- Once the electrodes are in place, they detect the electrical currents generated by the heart. These currents are then transmitted to an amplifier within the electrocardiograph. The amplifier’s role is critical, as it enhances the weak electrical signals to a level suitable for recording and analysis. The amplified currents are recorded on a moving sheet of paper, resulting in a graphical representation known as an ECG tracing, which appears as a wavy line.
- In contemporary electrocardiography, the system may also incorporate an oscilloscope, an instrument that provides real-time visual feedback of the electrical signals on a screen. This feature allows healthcare professionals to monitor the electrical activity more dynamically, facilitating immediate analysis during diagnostic procedures. The sensitivity of the electrocardiograph is crucial, as it employs a sensitive lever mechanism to trace the changes in electrical currents accurately.
- Thus, the working principle of an electrocardiograph not only involves the detection and amplification of cardiac electrical activity but also emphasizes the precise arrangement and function of electrodes. This process culminates in the generation of a detailed ECG tracing, which serves as a vital tool for assessing cardiac health and diagnosing potential heart-related conditions. By understanding the electrocardiograph’s operation, healthcare professionals can better interpret the electrical signals that reflect the heart’s rhythmic activities.
Waves of Normal ECG
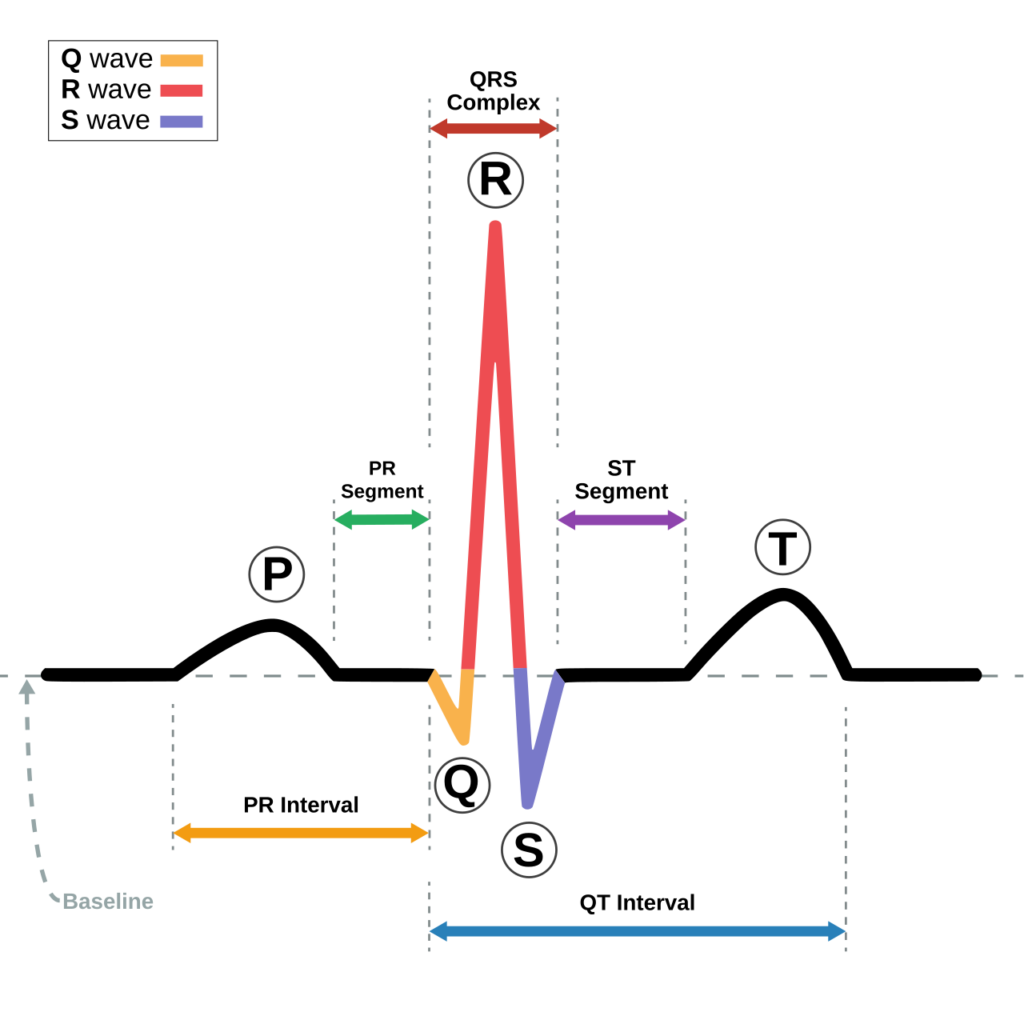
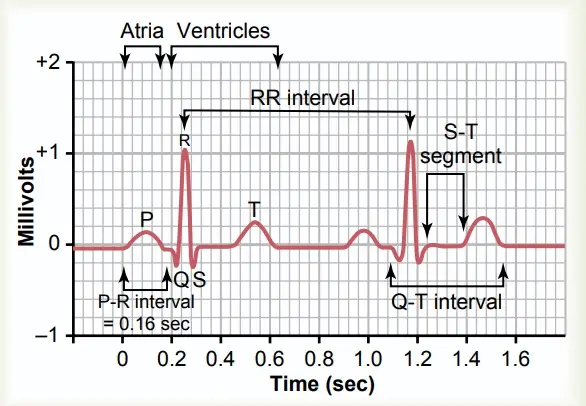
A normal electrocardiogram (ECG) depicts a characteristic pattern consisting of three distinct waves that correspond to different phases of the cardiac cycle. These waves—P wave, QRS wave, and T wave—along with the P-R interval and S-T segment, provide essential information about the heart’s electrical activity and overall function.
- P-wave:
- This wave is the first to appear in a normal ECG and is characterized as a small upward deflection.
- It signifies atrial depolarization, which occurs as the electrical excitation spreads from the sinoatrial (SA) node throughout the atria.
- Approximately 0.1 seconds after the onset of the P wave, the atria contract, thereby representing atrial systole.
- QRS wave:
- The QRS wave follows the P wave and initiates as a slight downward deflection, which then transitions into a prominent upright triangular wave before concluding with another downward deflection.
- This wave reflects ventricular depolarization, indicating that the ventricles are preparing to contract.
- The onset of the QRS wave coincides with the beginning of ventricular contraction (systole).
- T-wave:
- The third wave observed in a normal ECG is the T wave, which appears as a small, dome-shaped upward deflection.
- This wave represents ventricular repolarization, marking the heart’s transition to diastole as the ventricles prepare to fill with blood again.
- It is important to note that atrial diastole merges with the QRS wave, reflecting the overlapping nature of the cardiac cycles.
- P-R interval:
- The P-R interval is an important measure that indicates the time required for the electrical impulse to travel through the atria, the atrioventricular (AV) node, and the bundle of His before reaching the ventricles.
- This interval provides insight into the conduction speed through the heart’s electrical system.
- S-T segment:
- The S-T segment is defined as the period from the end of the S wave to the beginning of the T wave.
- This segment reflects the duration during which the ventricular fibers are fully depolarized and play a crucial role in evaluating the heart’s electrical stability.
Significance of different waves
The significance of various waves observed in an electrocardiogram (ECG) is paramount, especially when deviations from the normal ECG pattern occur. These alterations can provide critical insights into underlying cardiac conditions, guiding healthcare professionals in diagnosing and managing various heart diseases.
- Enlarged P-wave:
- An enlarged P wave indicates an enlarged atrium, often associated with conditions such as mitral stenosis. In this scenario, the narrowing of the mitral valve leads to increased pressure, causing blood to back up into the left atrium. This physiological change manifests as a pronounced P wave on the ECG.
- Enlarged Q-wave:
- A downward deflection known as an enlarged Q wave can signify a myocardial infarction (heart attack). This change indicates that the heart muscle has been damaged, typically due to insufficient blood flow, which can alter the electrical conduction patterns observed on the ECG.
- Enlarged R-wave:
- The presence of an enlarged R wave on the ECG may indicate the enlargement of the ventricles. This change can result from various factors, including hypertension or valve disorders, which increase the workload on the heart, leading to hypertrophy.
- Long P-Q interval:
- A prolonged P-Q interval suggests that the electrical impulse takes more time to travel through the atria and reach the ventricles. This condition can occur in coronary artery disease or rheumatic fever, where scar tissue may develop in the heart, impeding normal conduction.
- Elevated S-T segment:
- When the S-T segment is elevated above the baseline, it may indicate an acute myocardial infarction. This elevation reflects a critical change in the heart’s electrical activity during a heart attack, signaling the need for immediate medical intervention.
- Depressed S-T segment:
- Conversely, a depressed S-T segment indicates that the heart muscles are receiving insufficient oxygen. This situation often points to ischemia, a condition where blood flow to the heart is reduced, potentially leading to serious complications.
- Flatter T-wave:
- A flatter T wave on the ECG suggests an insufficient oxygen supply to the heart muscle, commonly seen in coronary artery disease. This change reflects the heart’s struggle to recover from depolarization and can be a warning sign of underlying cardiac issues.
- Elevated T-wave:
- An elevated T wave may indicate increased potassium ion levels in the blood, a condition known as hyperkalemia. Elevated potassium can significantly impact cardiac function, leading to dangerous arrhythmias if not addressed promptly.
Types of Electrocardiogram
There are three primary types of ECGs, each serving distinct purposes in the assessment of cardiac health.
- Resting ECG: This is the most common type of ECG and is routinely utilized for diagnostic purposes in hospital environments. During a resting ECG, the patient lies still in a supine position while electrodes are placed on the skin to record the heart’s electrical signals. This test captures a snapshot of the heart’s activity under resting conditions, allowing healthcare providers to identify arrhythmias, ischemic changes, and other cardiac abnormalities.
- Exercise ECG: Also known as a stress test, the exercise ECG is conducted while the patient engages in physical activity, typically by walking on a treadmill or pedaling a stationary bicycle. This type of ECG monitors the heart’s electrical activity under conditions of increased workload, providing valuable information about how the heart responds to physical stress. It is particularly useful for diagnosing coronary artery disease, as it can reveal changes in the heart’s rhythm or blood supply that may not be apparent at rest.
- Ambulatory ECG: This type of ECG captures the continuous electrical activity of the heart over a prolonged period, typically 24 hours or more. During an ambulatory ECG, a small portable device known as a Holter monitor is attached to the patient’s waist. This allows for normal daily activities while continuously recording the heart’s electrical signals. After the monitoring period, the collected data is analyzed to identify any intermittent arrhythmias or other cardiac issues that may have occurred during regular activities.
Instrumentation of Electrocardiogram
Electrocardiogram (ECG) instrumentation is a crucial aspect of cardiac health assessment, facilitating the accurate recording and interpretation of the heart’s electrical activity. The ECG test employs a sophisticated machine that consists of several key components working in harmony to ensure reliable data collection and analysis.
- ECG Machine: The core of the instrumentation is the ECG machine, which integrates multiple components, including electrodes, a central signal processor, a monitor, and a printer. This machine is designed to capture and analyze the electrical signals produced by the heart.
- Electrodes: A standard 12-lead ECG typically utilizes 10 electrodes that are strategically placed on the patient’s body. These electrodes are responsible for receiving, collecting, and transmitting biopotentials (the electrical potentials generated by the heart) from the skin. Each electrode captures specific electrical activity from different areas of the heart, enabling a comprehensive assessment of its function.
- Lead Wires: The biopotentials collected by the electrodes are transmitted through lead wires to a central impulse processing unit. These lead wires ensure a secure and effective connection between the electrodes and the ECG machine, allowing for accurate signal transmission.
- Central Signal Processor: Once the biopotentials reach the ECG machine, they undergo several processes. The central signal processor amplifies the received signals, enhancing the strength of the biopotentials for clearer interpretation. Subsequently, the signals are filtered to remove any noise or interference that could distort the data.
- Data Processing: After amplification and filtering, the processed signals are transformed into recognizable ECG waves. This involves organizing the data into specific intervals and segments that correspond to the different phases of the cardiac cycle.
- Display and Printing: The final processed signals are displayed on a monitor, allowing healthcare professionals to visualize the heart’s electrical activity in real-time. Additionally, the ECG can be printed on grid paper for further analysis and documentation. The printed output serves as a permanent record of the heart’s activity and can be used for diagnosis and follow-up care.
The procedure of obtaining an electrocardiogram (ECG)
he following steps outline the procedure for obtaining an ECG:
- Patient Preparation: The patient is guided to lie flat on a bed in a comfortable and relaxed position. It is essential to ensure that the patient is not wearing any metallic objects or electrical devices, as these can interfere with the ECG readings.
- Electrode Placement: The next step involves attaching electrodes to the patient’s body in their respective locations. For a standard 12-lead ECG, a total of 10 electrodes are used, which include both limb and chest electrodes.
- Limb Electrodes:
- Four arm electrodes are used:
- RA (Right Arm): This electrode is placed on the right arm.
- LA (Left Arm): This electrode is placed on the left arm.
- RL (Right Leg): This electrode is placed on the right leg.
- LL (Left Leg): This electrode is placed on the left leg.
- Four arm electrodes are used:
- Chest Electrodes:
- Six chest electrodes are designated as V1 to V6:
- V1: Positioned in the fourth intercostal space to the right of the sternum.
- V2: Positioned in the fourth intercostal space to the left of the sternum.
- V3: Placed between V2 and V4.
- V4: Positioned in the fifth intercostal space in the mid-clavicular line.
- V5: Placed horizontally to the left of V4 in the left anterior axillary line.
- V6: Positioned horizontally to the left of V5 in the mid-axillary line.
- Six chest electrodes are designated as V1 to V6:
- Limb Electrodes:
- Connecting Lead Wires: After the electrodes are securely attached, lead wires are connected from the electrodes to the ECG machine.
- Starting the ECG Machine: The ECG machine is then turned on. This automated device is designed to record the cardiac electrical impulse activity and generate the ECG waveform.
- Recording the ECG: The machine captures the heart’s electrical signals over a specific duration, producing an ECG tracing that represents the heart’s electrical activity. This tracing includes various segments and intervals essential for interpretation.
- Post-Procedure: Once an adequate ECG has been recorded, the leads are carefully disconnected from the electrodes. Following this, the electrodes are detached from the patient’s body, completing the procedure.
Intervals and Segments in a Normal Electrocardiogram
Intervals and segments in a normal electrocardiogram (ECG) are critical components that provide insights into the heart’s electrical activity. These time measurements and flat horizontal lines between waves indicate the functioning of the heart’s conduction system. The understanding of these intervals and segments aids in the assessment of cardiac health and the identification of potential abnormalities.
- Intervals in a Normal Electrocardiogram:
- In an ECG, intervals refer to the time periods between the beginnings of two waves. These intervals reflect the duration required for electrical impulses to travel through the cardiac conduction pathway, orchestrating the coordinated cycle of depolarization and repolarization of the heart’s walls. The primary intervals analyzed in a normal ECG are the PR interval and the QT interval.
- PR Interval:
- The PR interval is represented in the ECG by the gap between the beginning of the P-wave and the onset of the QRS complex. This interval measures the time taken for the cardiac impulse to travel from the sinoatrial (SA) node, through the atria, and the atrioventricular (AV) bundle, to reach the ventricles. Typically, the PR interval ranges from 120 to 200 milliseconds.
- QT Interval:
- The QT interval is illustrated by the gap extending from the start of the QRS complex to the end of the T-wave. It indicates the duration between consecutive ventricular depolarization and repolarization. The normal QT interval is usually shorter than 440 milliseconds.
- PR Interval:
- In an ECG, intervals refer to the time periods between the beginnings of two waves. These intervals reflect the duration required for electrical impulses to travel through the cardiac conduction pathway, orchestrating the coordinated cycle of depolarization and repolarization of the heart’s walls. The primary intervals analyzed in a normal ECG are the PR interval and the QT interval.
- Segments in a Normal Electrocardiogram:
- Segments are defined as flat horizontal lines that occur between two successive waves in the ECG, specifically from the end of one wave to the beginning of another. The two main segments included in the ECG analysis are the PR segment and the ST segment.
- PR Segment:
- The PR segment is the flat line found between the conclusion of the P-wave and the onset of the QRS complex. This segment represents the time delay between atrial systole (contraction) and ventricular systole. The duration of the PR segment is slightly longer than 440 milliseconds.
- ST Segment:
- The ST segment lies between the QRS complex and the T-wave, signifying the electrically neutral area following ventricular depolarization and preceding ventricular repolarization. This segment typically measures around 80 milliseconds.
- PR Segment:
- Segments are defined as flat horizontal lines that occur between two successive waves in the ECG, specifically from the end of one wave to the beginning of another. The two main segments included in the ECG analysis are the PR segment and the ST segment.
Interpreting the ECG Results
Interpreting ECG results is a critical skill for healthcare professionals, as it enables the identification of various cardiac conditions. The interpretation process involves analyzing specific components of the ECG waveform and correlating these findings with clinical information to provide a comprehensive understanding of a patient’s cardiac health.
- Key Components for Analysis:
- P Wave: Represents atrial depolarization. In a normal ECG, the P wave should be upright, uniform, and consistent before each QRS complex. The duration should be less than 0.12 seconds, and the amplitude should be less than 2.5 mm.
- QRS Complex: Indicates ventricular depolarization. The duration typically ranges from 0.06 to 0.10 seconds.
- T Wave: Reflects ventricular repolarization. It should be upright in leads I, II, V3 to V6, while appearing inverted in lead aVR.
- PR Interval: The duration between the beginning of the P wave and the beginning of the QRS complex, which should be between 0.12 and 0.20 seconds.
- QT Interval: Measured from the beginning of the QRS complex to the end of the T wave, this interval is usually around 0.40 seconds.
- ST Segment: A flat line between the end of the QRS complex and the beginning of the T wave, typically lasting about 0.08 seconds.
- Heart Rate and Rhythm:
- The heart rate should be between 60 to 100 beats per minute, and the rhythm should be consistent and even. Deviations from these norms can indicate underlying cardiac issues.
- Possible Abnormal Findings:
- Cardiac Arrhythmias: Deviations in the normal rhythm may suggest conditions such as tachycardia, bradycardia, or atrial fibrillation.
- Conduction Disorders: Abnormalities in the PR interval can signal issues like heart block or long QT syndrome, where electrical signals are not properly conducted.
- Myocardial Infarction: An ECG can detect current heart attacks or previously undiagnosed silent heart attacks by analyzing changes in the ST segment or T wave.
- Angina: This condition, characterized by chest pain from reduced blood flow to the heart, may be indicated by specific patterns in the ECG.
- Hypertrophic Cardiomyopathy: Abnormal enlargement of the heart muscle may result in a downward-sloping ST segment visible on the ECG.
- Congenital Heart Disease: Conditions like a ventricular septal defect can be identified through characteristic changes in the ECG waveform.
- Electrolyte Imbalances: Abnormal levels of potassium and magnesium can influence the T waves, highlighting the importance of electrolyte balance in cardiac function.
- Heart Infections: Conditions such as pericarditis, myocarditis, and endocarditis can produce alterations in the ST segment.
- Interpreting the Report:
- While the ECG report will describe wave patterns, it typically does not provide a detailed diagnosis of heart conditions. Therefore, it is essential for healthcare providers to consider the patient’s symptoms and medical history when interpreting the results. A holistic approach ensures that any abnormalities identified on the ECG are contextualized within the broader clinical picture.
What Does Abnormal Rhythm Mean?
Abnormal heart rhythm, commonly referred to as arrhythmia, signifies an irregularity in the heart’s electrical activity, leading to alterations in the heart’s rate or rhythm. Such abnormalities can have significant implications for cardiovascular health, necessitating a thorough understanding of their potential causes and consequences.
- Potential Causes of Abnormal Rhythm:
- Heart Enlargement: The enlargement of the heart can alter the normal electrical pathways, leading to arrhythmias. This condition often arises from chronic hypertension or heart valve disease.
- Heart Attack (Current or Previous): A history of heart attack can result in scar tissue formation within the heart muscle, disrupting the usual electrical conduction and potentially causing arrhythmias.
- Arteries with Poor Blood Supply: Insufficient blood flow to the heart, often due to coronary artery disease, can affect the heart’s ability to maintain a normal rhythm. This reduced perfusion can compromise the heart muscle and lead to abnormal electrical impulses.
- Congenital Heart Defects: Structural abnormalities present at birth can affect the heart’s electrical system, leading to arrhythmias. Such defects may include septal defects or malformations of the heart valves.
- Muscle Damage of the Heart: Damage to the heart muscle, whether from ischemia or inflammation (such as myocarditis), can disrupt the electrical conduction pathways, resulting in irregular rhythms.
- Fluctuations in Electrolyte Levels: Electrolytes like calcium and potassium play a crucial role in the heart’s electrical conduction. Imbalances in these electrolytes can lead to significant changes in heart rhythm, manifesting as arrhythmias.
- Swelling Around the Heart: Conditions such as pericarditis can cause swelling in the pericardial sac surrounding the heart, potentially leading to changes in rhythm due to increased pressure on the heart muscle.
- Fluid in the Sac Around the Heart: Accumulation of fluid around the heart can also impede its function, leading to irregular heart rhythms.
- Interpreting ECG Results:
- It is essential to recognize that the accuracy of an ECG result may vary depending on the testing conditions. Factors such as patient positioning, electrode placement, and patient activity level can all influence the outcome.
- Moreover, while ECGs are valuable tools for diagnosing arrhythmias, not all heart problems are detectable through this method. Certain cardiac conditions may not present discernible changes in ECG results, emphasizing the importance of comprehensive cardiac evaluation beyond ECG findings.
Limitations of electrocardiography (ECG)
The electrocardiogram (ECG) is a widely utilized diagnostic tool for assessing the heart’s electrical activity; however, it has several limitations that must be recognized to ensure accurate interpretation and effective clinical decision-making.
- Limited Anatomical Information: While the ECG provides valuable insights into the electrical activity of the heart, it does not offer any information regarding the heart’s anatomical structure. As a result, healthcare providers must rely on other imaging techniques, such as echocardiography or cardiac MRI, to assess structural abnormalities.
- Potential for False Results: ECG reports are susceptible to inaccuracies that may arise from various factors. Issues with electrode placement, the body’s electric potential, and interference from nearby metallic or electronic devices can lead to false positives or negatives. Such inaccuracies can misguide diagnosis and treatment strategies.
- Subjective Interpretation: The interpretation of ECG results can be subjective, as it often depends on the clinician’s experience and expertise. Consequently, variations may exist in reporting among different healthcare professionals, potentially leading to inconsistent diagnoses and management plans.
- Transient Data: The ECG records electrical activity for only a brief period. This limitation means that transient cardiac events may go undetected, especially if they occur outside the time frame of the test. Continuous monitoring may be necessary for patients with intermittent symptoms to capture these fleeting occurrences.
- Inability to Predict Future Events: The ECG is primarily a diagnostic tool, and while it can identify existing cardiac conditions, it cannot predict future cardiac events. Additionally, it may not detect the formation of abnormal tissues or blood clots, nor can it assess cardiac events that are unrelated to electrical activity.
Possible risks of ECG
Below is a comprehensive overview of the possible risks associated with ECG procedures.
- Irritation or Allergic Reaction:
- Patients may experience skin irritation or allergic reactions due to the adhesive properties of the electrodes attached to their arms and chest. This reaction can range from mild redness to more significant discomfort, necessitating careful monitoring and, if necessary, alternative adhesives or electrode types.
- Tissue Breakdown:
- Prolonged use of electrodes, particularly during an ambulatory ECG, can lead to tissue breakdown at the site of electrode placement. This issue may result in discomfort or skin integrity problems, requiring healthcare providers to evaluate the duration of electrode wear carefully.
- Cardiac Events During Stress Tests:
- While performing an exercise ECG, commonly known as a stress test, patients may experience adverse heart-related events. Symptoms such as lightheadedness or fainting can occur, indicating that the heart may be under undue stress. In rare instances, more severe complications, including a heart attack, may occur during physical exertion. Therefore, it is crucial for medical personnel to be present during these tests to monitor patients closely for any signs of distress.
Application of electrocardiography (ECG)
The application of electrocardiography (ECG) is fundamental in cardiology, providing valuable insights into the heart’s electrical activity, rhythm, and overall health. This diagnostic tool is instrumental in various clinical scenarios, allowing healthcare professionals to evaluate and manage a range of cardiovascular conditions effectively.
- Rate and Rhythm Assessment: The ECG serves as a primary means of indicating the heart rate and rhythm, offering critical information about the pattern of heart contractions.
- Diagnosis of Heart Disorders: It provides clues regarding the condition of the heart muscle, facilitating the diagnosis of various heart disorders. By analyzing the ECG waveform, clinicians can discern potential abnormalities that may indicate underlying health issues.
- Evaluation of Heart Size and Damage: The ECG aids doctors in determining whether the heart is normal in size or if it is enlarged. It can also indicate whether certain regions of the heart have sustained damage, enhancing the diagnostic process.
- Detection of Arrhythmias: One of the key applications of ECG is to identify irregularities in the heart’s rhythm, known as arrhythmias. These disturbances can signify significant cardiovascular concerns that require further evaluation and management.
- Assessment of Heart Damage: ECG is essential for diagnosing heart damage resulting from conditions such as high blood pressure, rheumatic fever, and congenital heart defects. This diagnostic capability is vital in developing appropriate treatment plans.
- Identifying Injury from Heart Attacks: The ECG is instrumental in determining the location and extent of injury caused by heart attacks. Following an incident, it plays a crucial role in assessing the extent of recovery and the effectiveness of therapeutic interventions.
- Study of Cardiac Activity: The ECG allows for the study of the heart’s electrical activity, providing insights into the cardiac cycle and overall heart function. This detailed analysis is essential for understanding various cardiovascular diseases.
- Monitoring Treatment Progress: ECG is employed to evaluate the progress of patients after medication or cardiac surgery, helping healthcare providers determine the effectiveness of treatment regimens.
- Complementary Use with Echocardiography: In conjunction with echocardiography (ECHO), ECG is used to assess the overall structural and functional health of the heart and its valves. This combined approach enhances diagnostic accuracy and treatment planning.
- Stress Testing: ECG is also utilized to examine how the heart performs under stress, enabling healthcare providers to identify potential issues that may not be apparent under resting conditions.
- Wang, Fei & Syeda-Mahmood, Tanveer & Beymer, David. (2009). Information Extraction from Multimodal ECG Documents. Proceedings of the International Conference on Document Analysis and Recognition, ICDAR. 381-385. 10.1109/ICDAR.2009.189.
- Pham B-T, Le PT, Tai T-C, Hsu Y-C, Li Y-H, Wang J-C. Electrocardiogram Heartbeat Classification for Arrhythmias and Myocardial Infarction. Sensors. 2023; 23(6):2993. https://doi.org/10.3390/s23062993
- https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/electrocardiogram
- https://www.onlinebiologynotes.com/electrocardiogram-ecg-working-principle-normal-ecg-wave-application-of-ecg/
- https://www.physio-pedia.com/Electrocardiogram
- https://www.verywellhealth.com/electrocardiogram-ekg-ecg-1745304
- https://www.brainkart.com/article/Characteristics-of-the-Normal-Electrocardiogram_19237/
- https://en.wikipedia.org/wiki/Electrocardiography