What is Coronary circulation?
- Coronary circulation refers to the system of blood flow specifically designed to supply oxygenated blood to the heart muscle, known as the myocardium. This circulatory pathway is crucial, as the heart requires a continuous supply of oxygen to maintain its function and ensure that the entire body receives adequate blood flow.
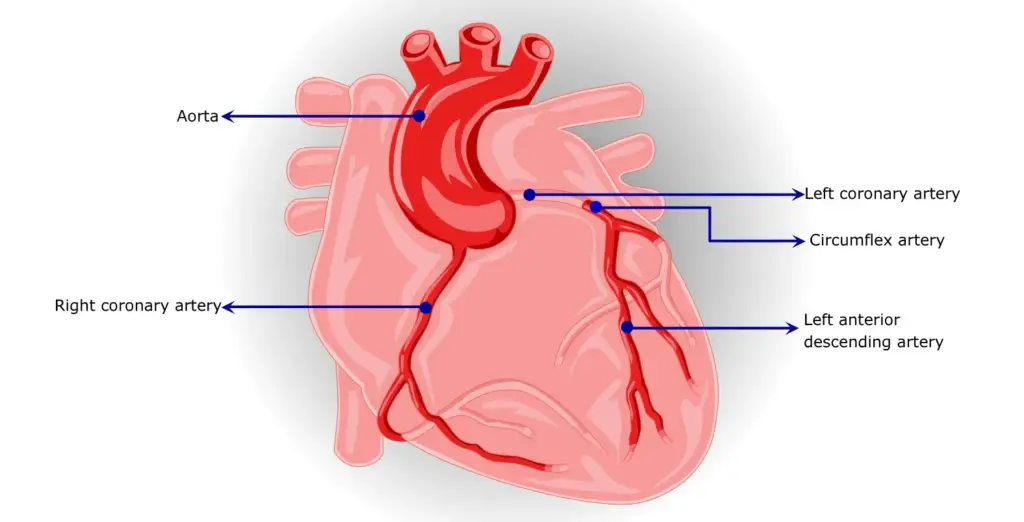
- The coronary arteries are responsible for delivering oxygen-rich blood to the myocardium. These arteries branch off from the aorta, which is the main artery leaving the heart. The primary coronary arteries include the left main coronary artery, which further divides into the left anterior descending artery and the circumflex artery, and the right coronary artery. Each of these arteries plays a vital role in nourishing different regions of the heart. Consequently, the health of these arteries is paramount, as any compromise can lead to severe consequences.
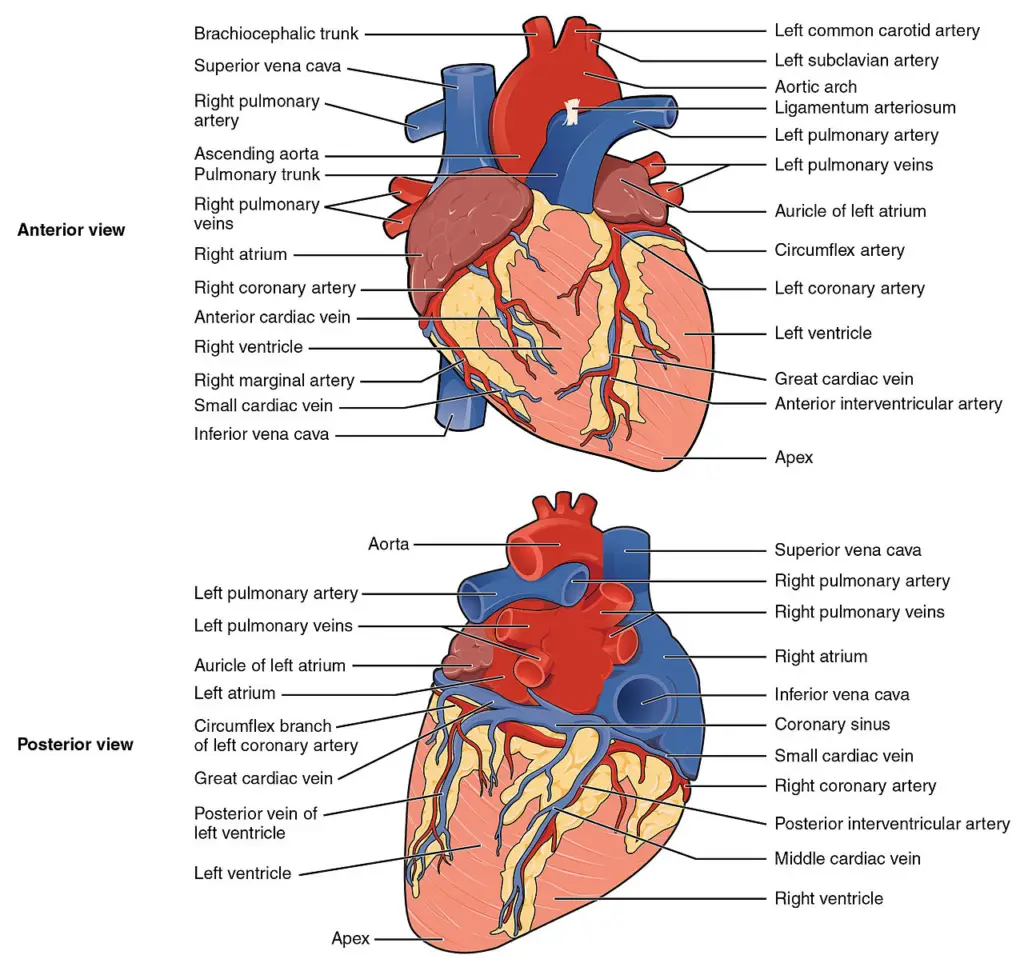
- Once the heart muscle has utilized the oxygen, it produces deoxygenated blood, which needs to be efficiently removed. The cardiac veins are responsible for this task, draining the deoxygenated blood away from the myocardium and directing it back toward the right atrium of the heart. This process is essential for maintaining the overall balance of oxygen and carbon dioxide levels in the blood, which is critical for the heart’s and the body’s function.
- The significance of coronary circulation extends beyond the heart itself; it plays a vital role in the overall well-being of the body and the brain. The heart’s continuous operation ensures that oxygenated blood reaches all organs, especially the brain, which is highly sensitive to fluctuations in oxygen supply. Therefore, any interruption in coronary circulation can have immediate and catastrophic consequences.
- One of the most severe outcomes of disrupted coronary circulation is a heart attack, or myocardial infarction. This condition occurs when the blood supply to a part of the heart muscle is obstructed, leading to oxygen deprivation and subsequent tissue damage. Typically, such obstructions result from coronary ischemia, a condition associated with coronary artery disease, characterized by the narrowing of the coronary arteries due to atherosclerosis. In some cases, embolisms can also block blood flow, further complicating coronary circulation.
Anatomy Of the coronary circulation
The anatomy of the coronary circulation is crucial for understanding how the heart receives its blood supply. This system consists of the coronary arteries and veins, which work together to deliver oxygen-rich blood to the myocardium and return deoxygenated blood back to the heart.
- Coronary Arteries:
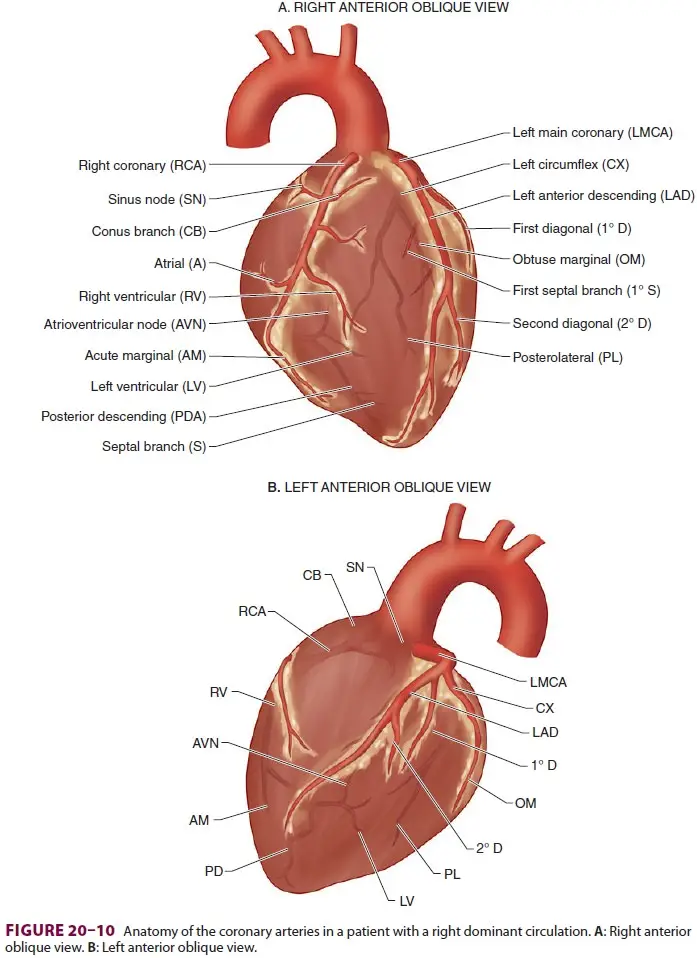
- The myocardial blood supply is exclusively derived from the right and left coronary arteries. These arteries originate from the aortic sinuses and extend across the surface of the heart, where they branch into smaller vessels.
- Blood flows from the epicardial arteries to the endocardial vessels, ensuring that all layers of the heart muscle are perfused.
- Right Coronary Artery (RCA):
- The RCA typically supplies blood to the right atrium, the majority of the right ventricle, and a variable portion of the left ventricle, specifically the inferior wall.
- In approximately 85% of individuals, the RCA branches into the posterior descending artery (PDA), which provides blood to the superior–posterior interventricular septum and inferior wall, characteristic of a right dominant coronary circulation.
- In the remaining 15%, the PDA branches from the left coronary artery, indicating a left dominant circulation.
- Left Coronary Artery (LCA):
- The LCA generally supplies blood to the left atrium, most of the interventricular septum, and the left ventricle, which includes the septal, anterior, and lateral walls.
- After a brief course, the left main coronary artery bifurcates into the left anterior descending artery (LAD) and the circumflex artery (CX). The LAD primarily supplies the septum and anterior wall, while the CX supplies the lateral wall.
- In a left dominant circulation, the CX wraps around the atrioventricular (AV) groove and continues as the PDA, providing blood to most of the posterior septum and inferior wall.
- Supply to Conduction System:
- The arterial supply to the sinoatrial (SA) node can come from either the RCA (60% of individuals) or the LAD (40%).
- The atrioventricular (AV) node is primarily supplied by the RCA (85% to 90%), with a smaller contribution from the CX (10% to 15%).
- The bundle of His receives a dual blood supply from both the PDA and LAD, ensuring its function is preserved.
- The anterior papillary muscle of the mitral valve has a dual supply from diagonal branches of the LAD and marginal branches of the CX, while the posterior papillary muscle is generally supplied only by the PDA, making it more susceptible to ischemic dysfunction.
- Venous Drainage:
- After perfusing the myocardium, deoxygenated blood returns to the right atrium primarily via the coronary sinus and the anterior cardiac veins. A small volume of blood also returns directly into the heart chambers through the Thebesian veins.
Coronary Arteries
Coronary arteries are crucial components of the cardiovascular system, responsible for supplying oxygenated blood to the heart muscle, or myocardium. The two primary coronary arteries are the left and right coronary arteries, which branch off from the aorta and are essential for the heart’s function.
- Arterial Origins: The left and right coronary arteries originate from the aortic sinuses, which are small openings located behind the flaps of the aortic valve. Specifically, when the heart relaxes, the backflow of blood fills these sinuses, allowing blood to enter the coronary arteries. This anatomical feature is critical for ensuring that the myocardium receives a continuous supply of oxygen-rich blood.
- Left Coronary Artery (LCA): The LCA further branches into several significant arteries:
- Left Anterior Descending (LAD) Artery: Also referred to as the anterior interventricular artery, it is a major branch that supplies blood to the anterior wall of the left ventricle and the interventricular septum.
- Left Circumflex Artery (Cx): This artery runs along the coronary sulcus and supplies blood to the left atrium and portions of the left ventricle. In approximately 20-25% of individuals, the Cx contributes to the formation of the posterior interventricular artery (PIv).
- Left Marginal Artery (LMA): This artery branches off the LCA and supplies the lateral wall of the left ventricle.
- Right Coronary Artery (RCA): The RCA also branches into vital arteries:
- Right Marginal Artery (RMA): This artery supplies the anterior portion of the right ventricle.
- Posterior Interventricular Artery (PIv): In 80-85% of individuals, the RCA gives rise to the PIv, which runs along the posterior interventricular sulcus and supplies blood to the posterior walls of both ventricles and the interventricular septum.
- Distribution and Function:
- The LCA primarily distributes blood to the left side of the heart, including the left atrium, left ventricle, and the interventricular septum.
- The RCA supplies the right atrium, parts of both ventricles, and the cardiac conduction system, which is essential for maintaining a coordinated heartbeat.
- The coronary arteries follow the grooves or sulci of the heart, with branches termed epicardial coronary arteries. These arteries remain on the surface of the heart and play a crucial role in supplying blood to the myocardium.
- Anastomoses: Both coronary arteries form small interconnections called anastomoses. These connections allow for collateral circulation, which can provide blood to areas of the heart if another branch is partially blocked. However, the small size of these anastomoses limits their effectiveness. Consequently, blockages in coronary arteries can lead to myocardial infarctions, which result in the death of cardiac muscle cells supplied by the affected vessel.
Cardiac Veins
Cardiac veins play a vital role in the venous drainage system of the heart, ensuring the efficient removal of deoxygenated blood from the myocardium. The primary pathway for this venous return is the coronary sinus, a significant venous structure located on the heart’s posterior aspect. This structure ultimately empties into the right atrium, allowing for the reoxygenation of blood in the pulmonary circulation.
- Coronary Sinus: The coronary sinus is the main vessel responsible for collecting blood from the heart’s cardiac veins. It serves as the central conduit for deoxygenated blood returning from the myocardium. Once filled, it drains into the right atrium, where the blood will be sent to the lungs for oxygenation.
- Major Tributaries of the Coronary Sinus:
- Great Cardiac Vein: Known as the anterior interventricular vein, this is the largest tributary of the coronary sinus. It originates at the heart’s apex, ascends along the anterior interventricular groove, and then curves to the left to continue onto the posterior surface of the heart. It gradually enlarges to form the coronary sinus.
- Small Cardiac Vein: This vein is located on the heart’s anterior surface, situated in a groove between the right atrium and the right ventricle. It travels along this groove to the posterior surface, where it drains into the coronary sinus.
- Middle Cardiac Vein: Also known as the posterior interventricular vein, this vessel begins at the apex of the heart and ascends in the posterior interventricular groove, draining into the coronary sinus.
- Posterior Cardiac Vein: Located on the posterior surface of the left ventricle, this vein runs adjacent to the middle cardiac vein and also empties into the coronary sinus.
- Additional Cardiac Veins:
- Smallest Cardiac Veins: These small veins, also referred to as Thebesian veins, drain directly into the right atrium. Their precise anatomy may vary, but they play a crucial role in venous drainage.
- Anterior Cardiac Veins: These veins directly transport deoxygenated blood from the heart muscle to the right atrium, bypassing the coronary sinus.
- Function and Importance: Cardiac veins are essential for transporting deoxygenated blood from the myocardium back to the right atrium. They include several significant vessels, such as the great cardiac vein, middle cardiac vein, small cardiac vein, posterior vein of the left ventricle, and the oblique vein of Marshall. The majority of the deoxygenated blood from the coronary veins returns to the right atrium through the coronary sinus.
Determinants of Coronary Perfusion
Determinants of coronary perfusion are critical for understanding the blood flow dynamics in the heart. Unlike other organs, coronary perfusion occurs intermittently, primarily during the diastolic phase of the cardiac cycle. This unique pattern has significant implications for myocardial blood flow and overall heart function.
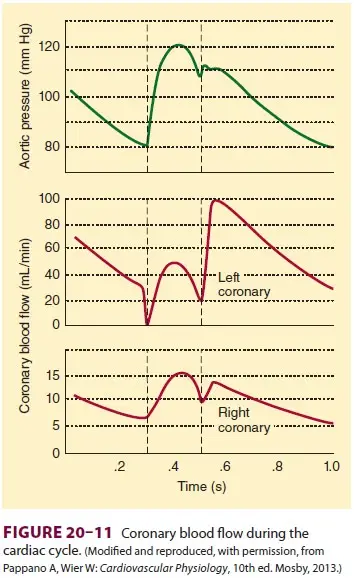
- Intermittent Nature of Coronary Perfusion:
- Coronary perfusion differs from continuous perfusion observed in other organs. During systole (the contraction phase), the intramyocardial pressures in the left ventricle rise to levels approaching systemic arterial pressure. This high pressure effectively occludes the intramyocardial portions of the coronary arteries, which can even lead to transient reversal of blood flow in epicardial vessels.
- As the left ventricle contracts, it exerts pressure that limits coronary blood flow, indicating that perfusion mainly occurs when the heart muscle is relaxed, or during diastole.
- Perfusion Pressure Dynamics:
- The coronary perfusion pressure is fundamentally determined by the difference between aortic pressure and left ventricular pressure. As a result, coronary blood flow is predominantly facilitated during diastole when the left ventricular pressure is lower than aortic pressure.
- Conversely, during systole, the pressure in the left ventricle exceeds that of the aorta, significantly reducing blood flow through the coronary arteries.
- Perfusion in Right vs. Left Ventricle:
- The right ventricle is perfused throughout both systole and diastole, while the left ventricle primarily receives blood during diastole. This distinction highlights the varying perfusion patterns in different heart chambers based on pressure changes.
- Influence of Blood Pressure:
- Several factors influence coronary perfusion pressure, including:
- Aortic Pressure: Decreases in aortic pressure can lead to reduced coronary perfusion pressure. This situation may arise in conditions such as hypotension.
- Ventricular End-Diastolic Pressure: Increases in this pressure can also diminish coronary perfusion pressure. High end-diastolic pressures can indicate issues such as heart failure.
- Several factors influence coronary perfusion pressure, including:
- Heart Rate Effects:
- An increase in heart rate reduces coronary perfusion due to a disproportionate decrease in diastolic time. As heart rate elevates, the duration of diastole shortens, limiting the time available for coronary blood flow to occur. This relationship is crucial in understanding how tachycardia can compromise myocardial oxygen supply.
- Vulnerability of the Endocardium:
- The endocardium, the innermost layer of the heart muscle, is particularly susceptible to ischemia, especially during periods of reduced coronary perfusion pressure. This is due to the significant intramural pressures it experiences during systole, making it more vulnerable to oxygen deprivation when coronary blood flow is compromised.
The regulation of coronary circulation
The regulation of coronary circulation is a complex interplay of various physiological factors that ensure an adequate blood supply to the heart muscle. Understanding these regulatory mechanisms is essential for appreciating how the heart adapts to different metabolic demands and maintains its function.
- Heart Rate:
- A fundamental determinant of coronary circulation is heart rate. As heart rates increase, the duration of diastole decreases. Consequently, this reduction in diastolic time limits the time available for coronary blood flow, leading to a decrease in perfusion to the myocardium. Therefore, maintaining an optimal heart rate is critical for ensuring sufficient coronary blood supply.
- Aortic Blood Pressure:
- The relationship between aortic blood pressure and coronary flow is direct. An increase in aortic pressure typically results in enhanced coronary flow. This is because higher aortic pressure increases the pressure gradient driving blood into the coronary arteries during diastole, facilitating greater perfusion of the heart muscle.
- Peripheral Resistance:
- Peripheral resistance also influences coronary circulation. As peripheral resistance rises, it leads to an increase in aortic pressure, thereby enhancing coronary blood flow. Thus, the interplay between systemic vascular resistance and coronary perfusion is vital in regulating blood supply to the heart.
- Autonomic Control:
- Autonomic nervous system control is pivotal in regulating coronary circulation.
- The sympathetic nervous system plays a dual role through the activation of adrenergic receptors:
- Beta (β) Adrenergic Receptors: Stimulation of β1 and β2 adrenergic receptors results in vasodilation in major portions of the coronary arteries, promoting increased blood flow to the myocardium.
- Alpha (α) Adrenergic Receptors: In contrast, α-adrenergic receptors are associated with vasoconstriction, contributing to the regulation of resting coronary blood flow. Despite this, the net effect of sympathetic stimulation typically favors vasodilation, allowing the heart to receive adequate blood supply during periods of increased activity.
- The sympathetic nervous system plays a dual role through the activation of adrenergic receptors:
- Autonomic nervous system control is pivotal in regulating coronary circulation.
- Neurotransmitters Involved:
- Neurotransmitters play significant roles in mediating the effects of the autonomic nervous system:
- Norepinephrine and neuropeptide Y are the key neurotransmitters released from sympathetic nerves, with neuropeptide Y acting as a potent vasoconstrictor, particularly within the coronary vasculature.
- On the other hand, acetylcholine, the neurotransmitter of the parasympathetic system, interacts with cholinergic receptors on the endothelium, stimulating the release of endothelium-derived relaxing factor (EDRF). This factor induces vasodilation of coronary arteries, facilitating increased blood flow.
- Neurotransmitters play significant roles in mediating the effects of the autonomic nervous system:
Distribution of the Coronary Arteries
The distribution of the coronary arteries is essential for understanding how blood is supplied to various regions of the heart muscle. The two primary coronary arteries, the right coronary artery (RCA) and the left coronary artery (LCA), branch out to perfuse specific areas of the myocardium.
- Right Coronary Artery (RCA):
- The RCA typically travels to the right of the pulmonary trunk and follows the coronary sulcus, which is the groove that separates the atria from the ventricles.
- As the RCA continues its course, it gives rise to the right marginal artery, which moves along the right and inferior border of the heart towards the apex.
- The RCA further extends to the posterior surface of the heart, maintaining its path along the coronary sulcus.
- Here, the posterior interventricular artery branches off from the RCA, descending within the posterior interventricular groove toward the apex, ensuring that the inferior wall of the heart receives adequate blood supply.
- Left Coronary Artery (LCA):
- The LCA originates between the left side of the pulmonary trunk and the left auricle, immediately branching into two major components: the anterior interventricular branch (commonly known as the left anterior descending artery, or LAD) and the circumflex branch.
- The LAD follows the anterior interventricular groove toward the heart’s apex. After reaching the apex, it continues onto the posterior surface where it anastomoses with the posterior interventricular artery, providing collateral circulation.
- The circumflex branch proceeds along the coronary sulcus towards the left border of the heart, subsequently moving onto the posterior surface.
- It gives rise to the left marginal branch, which follows the left border of the heart, contributing additional blood supply to that area.
- General Considerations:
- The area of the heart that a coronary artery covers corresponds directly to the region it perfuses. Understanding this anatomical layout is crucial for recognizing the implications of blockages or diseases affecting these vessels.
- The distribution of coronary arteries varies among individuals, which can lead to variations in myocardial perfusion patterns.
Factors influencing
Coronary circulation is essential for delivering oxygen-rich blood to the myocardium, ensuring its proper function. Several factors influence coronary circulation, which can affect blood flow dynamics and the overall health of the heart. Understanding these factors is critical for students and educators in the field of cardiovascular physiology.
- Perfusion Pressure:
- Coronary blood flow is directly related to perfusion pressure, defined as the difference between arterial pressure and venous pressure.
- Arterial Pressure:
- The coronary arteries originate from the base of the aorta. Therefore, the left ventricle propels blood directly into these arteries.
- As a result, the coronary arterial pressure is equivalent to the aortic pressure, facilitating effective blood flow to the myocardium.
- Venous Pressure:
- Most veins from the heart drain directly into the right atrium, which means that coronary venous pressure mirrors right atrial pressure.
- Coronary Perfusion Pressure:
- The coronary perfusion pressure during systole can be calculated as the systolic aortic pressure minus the right atrial pressure.
- Conversely, during diastole, the formula changes to the diastolic aortic pressure minus right atrial pressure.
- Generally, the coronary perfusion pressure is greater during systole due to higher systolic aortic pressure compared to diastolic pressure.
- Notably, despite higher perfusion pressure during systole, blood flow is predominantly greater during diastole. This phenomenon occurs because the subendocardial vessels are compressed during ventricular contraction, restricting flow, while they open during relaxation.
- Resistance:
- The relationship between coronary blood flow and vascular resistance is inversely proportional, meaning that as resistance increases, blood flow decreases.
- The formula for coronary blood flow can be expressed as coronary perfusion pressure divided by vascular resistance.
- High Resistance During Systole:
- During systole, myocardial contraction and the resultant squeezing of the coronary vessels lead to increased vascular resistance.
- This increased resistance during systole results in diminished coronary blood flow.
- Conversely, during diastole, resistance is lower, facilitating increased coronary blood flow.
Functions of Coronary circulation
The functions of coronary circulation are critical for maintaining the overall health and functionality of the heart. The intricate network of coronary arteries is responsible for supplying oxygen-rich blood to the myocardium, ensuring efficient cardiac performance. This circulation is vital for the proper functioning of various cardiac structures, adapting to changes in the heart’s oxygen demands and facilitating the intricate processes of contraction and relaxation.
- Supply to Papillary Muscles:
- Papillary muscles play a crucial role in the functioning of the mitral and tricuspid valves by anchoring these structures to the heart walls.
- If the blood supply to these muscles is compromised, it may lead to conditions such as mitral regurgitation, where blood leaks from the left ventricle into the left atrium during contraction.
- The anterolateral papillary muscle often receives dual blood supply from the left anterior descending (LAD) artery and the left circumflex artery (LCX), making it more resistant to ischemia.
- In contrast, the posteromedial papillary muscle is typically supplied solely by the posterior descending artery (PDA), rendering it more vulnerable to ischemic damage. A myocardial infarction affecting the PDA is particularly concerning as it can lead to significant mitral regurgitation.
- Changes in Diastole:
- During ventricular contraction (systole), high pressures in the myocardium compress the subendocardial coronary vessels, temporarily reversing blood flow and reducing perfusion.
- This compression causes blood flow in the subendocardium to halt during systole, while epicardial coronary vessels remain open and unobstructed.
- Consequently, the majority of myocardial perfusion occurs during diastole when pressures are lower, and the subendocardial vessels can open, allowing for increased blood flow.
- Notably, blood flow in the right coronary artery does not cease entirely during systole due to lower right ventricular pressures compared to diastolic blood pressure.
- Changes in Oxygen Demand:
- The coronary circulation responds to the heart’s oxygen requirements through the mechanisms of vasodilation and vasoconstriction, adjusting the blood supply accordingly.
- If the coronary arteries cannot meet the increased oxygen demands, it leads to tissue ischemia, characterized by a deficiency of oxygen.
- Brief episodes of ischemia can cause intense chest pain, known as angina, while severe ischemia may result in myocardial infarction, leading to irreversible damage to heart tissue from hypoxia.
- Chronic moderate ischemia can weaken the heart’s contraction ability, a condition referred to as myocardial hibernation, which affects overall cardiac efficiency.
- Pharmacological Reactivity:
- The coronary circulation is uniquely reactive to adrenergic stimulation, which plays a significant role in regulating coronary blood flow in response to varying physiological demands.
- This reactivity allows for rapid adjustments to coronary perfusion, facilitating the heart’s ability to respond to changes in workload or oxygen requirements effectively.
Control of Coronary Blood Flow
Coronary blood flow (CBF) plays a critical role in maintaining the heart’s functionality by delivering oxygen-rich blood to myocardial tissues. The control of CBF is a complex interplay of autoregulatory mechanisms and autonomic influences that ensure sufficient blood supply corresponding to the heart’s metabolic demands.
- Autoregulation of Coronary Blood Flow:
- CBF exhibits two primary forms of autoregulation: myogenic and metabolic.
- Myogenic Autoregulation:
- This phenomenon is observed in various organ systems, including the coronary circulation.
- As transmural pressure increases, it causes the smooth muscle membranes of the coronary vessels to become more permeable, leading to depolarization.
- Consequently, resistance within the vessels increases in proportion to the pressure, allowing CBF to remain relatively constant despite fluctuations in systemic blood pressure.
- Metabolic Autoregulation:
- This form of regulation is predominantly responsible for maintaining appropriate blood flow within the heart.
- During anaerobic metabolism, particularly in states of increased myocardial oxygen demand, byproducts such as lactate and adenosine are produced.
- These vasoactive mediators induce vasodilation, facilitating increased blood flow and enhancing oxygen delivery to the myocardium.
- Given that the typical myocardial oxygen extraction rate is about 70%, further increasing this extraction becomes challenging. Therefore, to meet heightened oxygen demands, an increase in blood flow is essential.
- Autonomic Control of Coronary Blood Flow:
- Autonomic mechanisms also play a significant role in modulating CBF through both direct and indirect effects.
- Direct Effects:
- The coronary vessels receive both parasympathetic and sympathetic innervation.
- The release of neurotransmitters such as acetylcholine (ACh) from parasympathetic fibers generally leads to a decrease in coronary blood flow.
- Conversely, sympathetic stimulation results in the release of norepinephrine (NA), which can increase coronary blood flow.
- Indirect Effects:
- Indirect effects are considered more significant than direct effects in the control of CBF.
- These effects arise from the autoregulation mechanisms that respond to changes in myocardial workload, which can be influenced by varying levels of parasympathetic and sympathetic stimulation.
- For instance, during periods of increased heart activity, sympathetic stimulation enhances blood flow through the mechanisms described in metabolic autoregulation.
- https://www.brainkart.com/article/Anatomy—Physiology-of-the-Coronary-Circulation_26946/
- https://www.vetscraft.com/coronary-circulation-in-animals/
- https://medicoapps.org/m-coronary-circulation/
- https://www.getbodysmart.com/heart-anatomy/coronary-arteries/
- https://standardofcare.com/coronary-arteries/
- https://teachmeanatomy.info/thorax/organs/heart/heart-vasculature/