What is Cardiac Output?
- Cardiac output (CO) is a key physiological measure that refers to the amount of blood the heart pumps in one minute. This output is essential for delivering oxygen and nutrients to tissues throughout the body, including vital organs like the brain. Cardiac output plays a crucial role in maintaining the body’s homeostasis by ensuring a consistent flow of blood, which adjusts to meet the body’s varying demands for oxygen and energy. For instance, during physical activities such as exercise, the body requires more oxygen, and cardiac output increases accordingly.
- Cardiac output is calculated by multiplying heart rate (HR)—the number of heartbeats per minute—by stroke volume (SV), which is the amount of blood ejected from the heart with each beat. In a healthy adult, the average heart rate is about 70 beats per minute, and the stroke volume is approximately 70 milliliters per beat. Therefore, the normal cardiac output is typically around 4.9 to 5 liters per minute. This means that, under normal conditions, the heart pumps approximately 5 liters of blood each minute, an amount shared equally between the right ventricle (which sends blood to the lungs for oxygenation) and the left ventricle (which sends oxygen-rich blood to the body).
- Cardiac output is not a static number; it varies according to the body’s needs. This is achieved by modulating heart rate and stroke volume, which are influenced by several physiological mechanisms, including the autonomic nervous system and hormonal signals. For example, during times of stress or exercise, the sympathetic nervous system increases heart rate and stroke volume, boosting cardiac output. Conversely, during rest, the parasympathetic system lowers heart rate, reducing the cardiac output.
- The cardiac index provides a more individualized measure of cardiac output by relating it to the body surface area (BSA). This adjustment is important because cardiac output is influenced by body size, making it more accurate to compare cardiac function across individuals using this index rather than the absolute output value.
- Understanding cardiac output is vital for assessing cardiovascular health. Insufficient cardiac output can lead to poor tissue perfusion, affecting organ function and potentially leading to conditions like heart failure. In clinical practice, measuring cardiac output helps physicians evaluate the severity of heart disease, guide treatments, and monitor patient outcomes.
- In summary, cardiac output represents the dynamic relationship between heart rate and stroke volume, reflecting the heart’s ability to meet the body’s circulatory demands. Its regulation is complex, involving nervous and hormonal systems, and any dysfunction in this process can lead to serious health consequences.
What is Cardiac Index?
Cardiac Index (CI) is a crucial measure in cardiovascular physiology that expresses cardiac output in relation to the individual’s body surface area (BSA). This index provides a more accurate understanding of heart function by accounting for the size of the person, making it a more individualized and useful measure than absolute cardiac output alone. Here is a detailed explanation of the cardiac index and its calculation:
- Expression of Cardiac Output in Relation to Body Surface Area (BSA): Cardiac index relates the amount of blood the heart pumps each minute (cardiac output) to the body surface area of an individual. This adjustment is necessary because cardiac output varies with body size, and larger individuals naturally have a higher cardiac output than smaller individuals. By incorporating body surface area into the equation, the cardiac index gives a standardized measure of cardiac performance that can be compared across different individuals, regardless of their size.
- Unit of Measurement for Cardiac Index: Typically, the cardiac index is expressed in terms of liters per minute per square meter (L/min/m²). This unit indicates the volume of blood pumped by the heart each minute per square meter of body surface area.
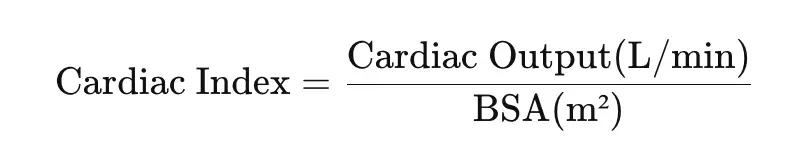
- Formula for Calculating Cardiac Index: To calculate the cardiac index, one must first know the cardiac output (the total volume of blood pumped by the heart per minute) and the individual’s body surface area (BSA), which is generally determined based on height and weight. The cardiac index is derived using the following formula:
- Example Calculation of Cardiac Index: Consider a scenario where the cardiac output is 5 liters per minute, and the individual’s body surface area is 1.7 square meters. Using the formula for cardiac index, the calculation would be:
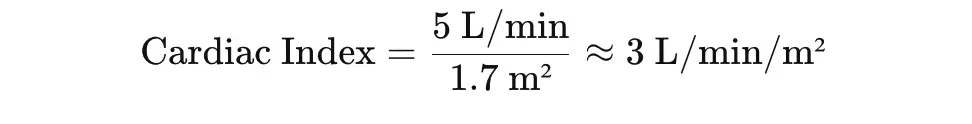
- This means that, for this particular individual, the heart pumps approximately 3 liters of blood per minute for every square meter of their body surface area.
- Significance of the Cardiac Index: By providing a cardiac performance measure relative to body size, the cardiac index offers a more precise indication of heart function, especially in clinical settings. It is particularly useful for diagnosing and monitoring patients with heart conditions, as it helps determine whether the heart is pumping sufficient blood for the body’s needs when size is taken into account. A normal cardiac index usually ranges between 2.5 to 4 L/min/m², and values outside this range may indicate an underlying cardiac issue requiring medical attention.
Mechanism of Cardiac Output
Cardiac output (CO) refers to the volume of blood pumped by the heart per minute and is a crucial measure of cardiovascular function. It is determined by two primary factors: heart rate (HR) and stroke volume (SV). Heart rate is the number of heartbeats per minute, while stroke volume is the amount of blood ejected from the ventricle with each beat. Cardiac output in humans typically ranges from 5-6 liters per minute at rest and can increase to over 35 liters per minute in elite athletes during intense exercise. The relationship between heart rate and stroke volume is influenced by several physiological factors that regulate cardiac function.
- Heart Rate (HR):
- HR is controlled by the sinoatrial (SA) node, which acts as the heart’s natural pacemaker. The SA node generates electrical impulses that cause the heart to contract, normally at an intrinsic rate of 60 to 100 beats per minute.
- Several factors, including neural and hormonal signals, can modulate the SA node’s firing rate, thus altering heart rate and, consequently, cardiac output.
- Stroke Volume (SV):
- Stroke volume is the difference between the end-diastolic volume (EDV) and end-systolic volume (ESV):
- EDV is the amount of blood in the ventricle at the end of diastole (before contraction), while ESV is the remaining blood volume after systole (after contraction).
- Stroke volume is calculated by subtracting ESV from EDV (SV = EDV – ESV).
- Stroke volume is influenced by several factors, including preload, contractility, and afterload:
- Preload:
- Preload refers to the tension in the heart’s ventricular muscle at the end of diastole, determined by the amount of blood filling the ventricles before contraction.
- Preload is directly proportional to EDV—the greater the EDV, the more the ventricular muscle fibers are stretched. This stretching increases the force of contraction through the Frank-Starling mechanism, which states that the heart will contract more forcefully in response to greater filling.
- Contractility:
- Contractility refers to the strength of the heart’s contraction, independent of preload. It is influenced by the condition of the cardiac muscle and external factors, such as inotropy (the effect of substances like catecholamines that increase contraction strength).
- Increased contractility allows the heart to eject a greater volume of blood, thereby increasing stroke volume. The ability to enhance contractility ensures that the heart can pump more efficiently when needed.
- Afterload:
- Afterload represents the resistance the heart must overcome to eject blood during systole. It is influenced by systemic vascular resistance (the resistance within the body’s blood vessels) and blood pressure.
- High afterload, such as in hypertension, makes it harder for the heart to eject blood, reducing stroke volume. Thus, afterload is inversely related to stroke volume, unlike preload and contractility.
- Preload:
- Stroke volume is the difference between the end-diastolic volume (EDV) and end-systolic volume (ESV):
- Mechanisms Increasing Cardiac Output:
- Sympathetic Nervous System (SNS):
- Sympathetic stimulation increases heart rate and stroke volume, enhancing cardiac output. It exerts positive effects on chronotropy (timing of heartbeats), dromotropy (speed of electrical conduction through the heart), and lusitropy (rate of myocardial relaxation).
- The SNS also increases venous return through receptor-mediated vasoconstriction, enhancing preload and stroke volume.
- Catecholamines (e.g., Adrenaline):
- Catecholamines released from the adrenal glands increase both heart rate and myocardial contractility by acting on beta-receptors in the heart. These actions amplify the force of contraction, leading to an increase in stroke volume.
- Thyroid Hormone:
- Thyroid hormone increases the sensitivity of the heart to catecholamines, thereby enhancing the heart’s response to sympathetic stimulation. It also increases heart rate and cardiac output.
- Frank-Starling Mechanism:
- This mechanism adjusts stroke volume based on changes in ventricular filling (preload). When more blood returns to the heart, the ventricular muscle fibers stretch more, leading to stronger contractions and greater stroke volume.
- Sympathetic Nervous System (SNS):
- Mechanisms Decreasing Cardiac Output:
- Parasympathetic Nervous System (PNS):
- In contrast to the sympathetic system, the parasympathetic nervous system (via the vagus nerve) reduces heart rate and stroke volume when oxygen demand decreases, such as during rest.
- This negative chronotropic effect decreases cardiac output, allowing the body to conserve energy.
- Parasympathetic Nervous System (PNS):
Determination of Cardiac Output
Cardiac output (CO) refers to the amount of blood the heart pumps per minute, which is a crucial measure for assessing cardiovascular health. Several methods can be used to determine cardiac output, each based on different principles and approaches. Below is a detailed explanation of these methods:
- Fick’s Principle:
- Fick’s principle states that the quantity of a substance taken up by or released from an organ is proportional to the concentration difference of the substance in arterial and venous blood, multiplied by blood flow through the organ per minute.
- When applied to the heart, Fick’s principle measures cardiac output by calculating the amount of a substance, such as oxygen, consumed by the body, in relation to the difference in oxygen concentration between arterial and venous blood. The formula used is:
- CO = Q/(Ca – Cv)
- Where:
- CO is cardiac output,
- Q is the volume of oxygen used per minute,
- Cais the arterial oxygen concentration, and
- Cv is the venous oxygen concentration.
- Steps to Determine CO Using Fick’s Principle:
- Measure the volume of oxygen used by the body per minute (Q). This can be done by having the subject breathe from a bag containing 100% oxygen.Estimate arterial oxygen content (Ca) by taking a sample of arterial blood.Estimate venous oxygen content (Cv) by sampling mixed venous blood, typically from the pulmonary artery.Plug the values into the formula and calculate the cardiac output.
- Oxygen consumed: Q=250 ml/minArterial oxygen content: Ca=20 ml/100 mlVenous oxygen content: Cv=15 ml/100 ml
- Dye Dilution Method:
- This method involves injecting a dye into the bloodstream and measuring its concentration over time to estimate cardiac output.
- Steps:
- A non-toxic dye (such as Evan’s blue, T1824) is dissolved in an isotonic fluid.
- A known quantity of dye is injected into a peripheral vein.
- Blood samples are collected from an artery at regular intervals (e.g., every 3 seconds).
- The concentration of the dye in these samples is measured.
- A graph is plotted showing dye concentration versus time, and the time for one complete circulation of blood is determined.
- Quantity of dye injected: 3 mg3 \text{ mg}3 mg
- Concentration of dye: 1.5 mg/ml1.5 \text{ mg/ml}1.5 mg/ml
- Circulation time: 30 sec30 \text{ sec}30 sec
- Thermodilution Method:
- This method measures changes in blood temperature following the injection of cold saline into the right atrium.
- Steps:
- A double-lumen catheter with a thermistor is inserted into the heart.
- Cold saline of known temperature and volume is injected into the right atrium.
- The temperature change is measured as the saline flows through the right ventricle and into the pulmonary artery.
- The magnitude of temperature change is proportional to cardiac output.
- Advantages:
- Since cold saline is used as the indicator, repeated measurements can be easily performed without significantly altering blood temperature.
- The method minimizes errors related to temperature fluctuations, making it highly reliable.
Factors Influencing Cardiac Output
- Increased Cardiac Output:
- Muscular Exercise: During intense exercise, cardiac output can increase up to 35 L/min, representing a seven-fold increase.
- Sympathetic Stimulation: Emotions like anxiety, anger, or fear trigger the sympathetic nervous system, leading to increased heart rate and cardiac output.
- Pregnancy, Anemia, Hyperthyroidism: These conditions also elevate cardiac output due to increased metabolic demands.
- Recumbent Posture: Cardiac output tends to be higher in a lying-down position compared to standing up.
- Decreased Cardiac Output:
- Hemorrhage: Blood loss leads to reduced cardiac output.
- Arrhythmias: Abnormal heart rhythms disrupt normal cardiac function and lower output.
- Left Ventricular Failure: The inability of the left ventricle to pump effectively results in diminished output.
- Sleep: Cardiac output decreases during sleep as the body’s metabolic demands are lower.
- Hypothyroidism: A low thyroid hormone level leads to reduced metabolism and decreased cardiac output.
Factors Influencing Cardiac Output
Cardiac output (CO) is the amount of blood the heart pumps per minute, and it can be influenced by various physiological and pathological conditions. These factors can either increase or decrease cardiac output depending on the body’s needs and the underlying circumstances.
- Muscular Exercise:
- During intense exercise, cardiac output can increase significantly, often reaching levels 6 to 10 times higher than at rest. The increase is due to both an elevated stroke volume (170-200 ml per beat) and a higher heart rate (150-180 beats per minute). The heightened demand for oxygen and nutrients by working muscles drives this sharp rise in cardiac output.
- Posture:
- The body’s position can affect cardiac output. In a recumbent (lying down) posture, the minute volume is higher compared to standing. This is because gravity reduces venous return in the standing position, making it harder for blood to flow back to the heart. In contrast, lying down promotes better venous return, thereby enhancing cardiac output.
- Fever, Hyperthyroidism, and Excitement:
- Various physiological conditions such as fever, hyperthyroidism, and emotional excitement can increase cardiac output. These conditions typically elevate the metabolic rate, leading to an increased demand for oxygen and nutrients throughout the body. For example, adrenaline released during excitement or stress raises both heart rate and stroke volume, directly boosting cardiac output. Similarly, the metabolic changes in hyperthyroidism result in a 10-25% increase in cardiac output.
- Besides, other factors like the ingestion and digestion of food, increased levels of carbon dioxide (CO2), and intravenous saline infusion also elevate cardiac output. Pregnancy, particularly in the late stages, can increase cardiac output by 45-85%, as the growing fetus demands more blood flow and oxygen from the maternal circulation.
- Hypothyroidism, Hemorrhage, Shock, and Heart Failure:
- Conditions such as hypothyroidism, where the metabolic rate is lowered, reduce cardiac output. Hemorrhage (severe blood loss) and shock drastically decrease venous return, impairing the heart’s ability to pump blood efficiently, thereby lowering cardiac output. In heart failure, the heart’s weakened state prevents it from maintaining an adequate stroke volume, leading to a reduction in overall cardiac output.
Regulation of Cardiac Output
Cardiac output (CO), the volume of blood pumped by the heart per minute, is regulated by a variety of factors. These determinants include heart rate (HR) and stroke volume (SV), both of which are influenced by neural and hormonal mechanisms, peripheral resistance, and myocardial contractility. Understanding the regulation of cardiac output involves analyzing how each of these factors contributes to changes in blood flow through the heart.
- Determinants of Cardiac Output:
- The two primary determinants of cardiac output are heart rate and stroke volume.
- Any factor that affects either heart rate, stroke volume, or both will, therefore, alter cardiac output.
- Peripheral resistance also impacts cardiac output by affecting stroke volume due to the after-load effect.
- Heart Rate Regulation:
- The heart rate can be modified through neural and hormonal mechanisms:
- Neural Mechanism:
- Parasympathetic stimulation (vagus nerve) exerts a negative chronotropic effect, reducing heart rate. This decreases cardiac output. However, a moderate decrease in heart rate may not significantly reduce cardiac output due to increased ventricular filling time, which enhances end-diastolic volume (EDV) and stroke volume via Starling’s law.
- Sympathetic stimulation increases heart rate and stroke volume through positive chronotropic effects, thereby raising cardiac output. However, if heart rate rises beyond a certain threshold, ventricular filling time is reduced, leading to decreased EDV, stroke volume, and ultimately, cardiac output.
- Hormonal Mechanism:
- Thyroxin increases the sensitivity of beta-receptors in the heart for catecholamines and elevates the number of these receptors in cardiac muscle. This results in an increased heart rate and cardiac output, especially in hyperthyroidism.
- Catecholamines (e.g., adrenaline and noradrenaline) also increase heart rate by stimulating beta-receptors in cardiac muscle. Their effect mirrors sympathetic stimulation, increasing both heart rate and the force of contraction, thus significantly boosting cardiac output.
- Neural Mechanism:
- The heart rate can be modified through neural and hormonal mechanisms:
- Stroke Volume Regulation:
- Stroke volume is the difference between end-diastolic volume (EDV) and end-systolic volume (ESV).
- EDV is the volume of blood in the ventricle at the end of diastole, typically about 140 ml.
- ESV is the volume of blood remaining in the ventricle at the end of systole, normally around 70 ml.
- The ejection fraction (SV/EDV) reflects the proportion of EDV ejected during systole, which is typically 50%. Stroke volume can be influenced by changes in EDV, ESV, or ejection fraction.
- Several factors affect stroke volume:
- Preload Effect (Venous Return):
- Preload refers to the load on the cardiac muscle before it contracts, which is determined by venous return and directly related to EDV. As venous return increases, the heart chambers distend, stretching the ventricular muscle fibers. This enhances the force of contraction based on Starling’s law, which states that the force of contraction is proportional to the initial length of the muscle fibers, within physiological limits. Hence, any factor affecting venous return will modify stroke volume and cardiac output.
- After-load Effect (Peripheral Resistance):
- After-load is the load on the muscle after it begins to contract. For the heart, this occurs when the ventricular pressure exceeds that of the diastolic blood pressure, allowing the semilunar valves to open. When after-load is high, such as in cases of hypertension, the volume of blood ejected by the ventricle decreases because more energy is spent overcoming resistance. Chronic after-load increases can lead to left ventricular failure, particularly if the ventricle becomes overstretched due to continuous high venous return combined with decreased ejection fraction.
- Myocardial Contractility:
- Myocardial contractility is the force with which the heart muscle contracts, influenced by several factors such as:
- Sympathetic stimulation increases myocardial contractility through a positive inotropic effect, increasing stroke volume by reducing ESV.
- Hypoxia, hypercapnia, and acidosis, often resulting from decreased coronary blood flow, reduce contractility and stroke volume.
- Myocardial infarction leads to the death of cardiac muscle cells, reducing muscle mass and thereby decreasing stroke volume.
- Inotropic agents like digitalis enhance contraction, while calcium channel blockers such as verapamil reduce contraction strength by decreasing calcium influx.
- Catecholamines simulate sympathetic stimulation, enhancing myocardial contractility and increasing cardiac output.
- Myocardial contractility is the force with which the heart muscle contracts, influenced by several factors such as:
- Preload Effect (Venous Return):
- Stroke volume is the difference between end-diastolic volume (EDV) and end-systolic volume (ESV).
- Distensibility of Cardiac Muscle:
- The heart’s ability to stretch, or distensibility, also influences stroke volume. Conditions like pericardial effusion and hemopericardium reduce distensibility, limiting stroke volume and cardiac output. Similarly, patients recovering from myocardial infarction may have decreased distensibility, impacting overall heart function.
- Heart-Lung Preparation:
- The regulation of cardiac output can be studied through heart-lung preparation, which allows detailed examination of how various factors influence heart function.
- Cardiac Catheterization:
- Cardiac catheterization is an invasive technique for measuring pressure and volume changes in the heart. It can be used to study septal defects, administer drugs directly to the heart, and stimulate pacemaker regions. However, catheterization may induce ventricular fibrillation, a potential risk of this procedure.
Alterations in Cardiac Output
Cardiac output (CO) refers to the volume of blood pumped by the heart per minute, and various physiological and pathological conditions can cause significant alterations in its level. These alterations result from changes in heart rate, stroke volume, and overall circulatory demands. Understanding these changes is essential for assessing cardiovascular function and the body’s adaptive mechanisms.
- Physiological Factors:
- Exercise:
- During exercise, the body’s skeletal muscles require more oxygen, which increases overall metabolic demand.
- Increased blood flow to the muscles reduces peripheral resistance, while muscle contractions and respiratory movements enhance venous return.
- As a result, cardiac output can increase by 4 to 6 times compared to resting levels.
- Despite decreased peripheral resistance, arterial pressure is maintained due to the baroreceptor reflex.
- Emotional States:
- Emotional stress, such as anxiety or fear, can lead to elevated cardiac output.
- This increase is due to heightened sympathetic nervous system activity, which raises heart rate and stroke volume.
- Posture:
- When transitioning from sitting or lying down to standing, cardiac output may drop by as much as 20%.
- This reduction is caused by the pooling of blood in the veins of the legs, leading to decreased venous return to the heart.
- Pregnancy:
- During pregnancy, cardiac output can rise by approximately 10%.
- This increase is due to the higher body mass, increased blood volume, and the low resistance of the placental and uterine blood vessels, which create a shunt from the arterial to venous systems.
- A reflexive increase in cardiac output helps maintain arterial pressure during pregnancy.
- Digestion:
- Around 1 to 3 hours after a meal, cardiac output increases.
- This rise supports the digestive system, which requires increased blood flow during the process of nutrient absorption and metabolism.
- Temperature:
- In high environmental temperatures, cardiac output increases to help regulate body temperature.
- Enhanced blood flow to the skin allows for heat dissipation, while also maintaining oxygen delivery to vital organs.
- Exercise:
- Pathological Factors:
- Anemia:
- In anemia, cardiac output increases due to two main factors:
- Reduced blood viscosity leads to marginally lower resistance to blood flow.
- More significantly, the reduction in oxygen content of the blood forces the heart to pump more blood to meet the body’s oxygen demands.
- In anemia, cardiac output increases due to two main factors:
- Hemorrhage:
- A significant loss of blood volume, as seen in hemorrhage, decreases venous return.
- This results in a reduction of cardiac output, as there is less blood available for the heart to pump.
- Metabolic Disorders:
- Conditions such as hyperthyroidism raise tissue metabolic activity and oxygen demand, similar to the effects of fever or exercise.
- The body compensates by increasing cardiac output to meet the elevated metabolic needs.
- Cardiac Failure:
- In cardiac failure, the heart’s ability to pump blood is compromised due to weakened myocardial cells.
- This condition leads to a decrease in cardiac output, as the heart can no longer contract with sufficient force to meet the body’s circulatory demands.
- Anemia:
Factors Determining Cardiac Output
Cardiac output, which refers to the amount of blood the heart pumps per minute, is influenced by several physiological factors. These factors interact to regulate the volume of blood the heart can circulate under different conditions. The key factors determining cardiac output include venous return, force of contraction, heart rate, and peripheral resistance.
- Venous Return:
- Venous return is the amount of blood returning to the right atrium via the veins in one minute. It plays a critical role in determining cardiac output, as over time, cardiac output equals venous return.
- At rest, venous return is approximately 5 liters per minute but can increase up to 35 liters per minute during exercise.
- Respiratory Pump:
- During inspiration, intrathoracic pressure decreases and intrathoracic volume increases, expanding thoracic veins and increasing venous return to the heart.
- Simultaneously, the diaphragm descends during inspiration, raising intra-abdominal pressure and pushing blood from the splanchnic veins into the thorax.
- The negative intrathoracic pressure, known as vis a fronte (force from the front), helps draw blood toward the heart. In contrast, if intrathoracic pressure becomes positive, venous return decreases (as in positive pressure breathing or during a Valsalva maneuver).
- Muscle Pump:
- When skeletal muscles contract, they compress the veins within the muscles, driving blood toward the heart, thereby enhancing venous return.
- Venous Tone:
- Increased venous tone, often through vasoconstriction, raises intrathoracic blood volume and venous return. This is referred to as vis a tergo (force from behind), while venous distension has the opposite effect, reducing venous return.
- Gravity:
- In an upright posture, gravity causes blood pooling in the lower extremities, reducing venous return.
- Blood Volume:
- Blood volume is directly proportional to venous return, meaning that greater blood volume increases the return of blood to the heart.
- Force of Contraction:
- The force with which the heart contracts directly influences stroke volume and, in turn, cardiac output. Several factors determine the force of contraction:
- Initial Length of Cardiac Muscle Fiber:
- The initial length of cardiac muscle fibers is determined by the end-diastolic volume (EDV), also known as preload. According to Frank-Starling’s law, the greater the initial muscle fiber length, the stronger the contraction, within physiological limits.
- An increase in venous return leads to greater diastolic filling, increasing EDV (preload). This stretches the heart muscle, lengthens muscle fibers, and results in a stronger contraction, known as heterometric regulation.
- Autonomic Nerve Activity:
- Sympathetic nervous system stimulation increases the force of contraction, while parasympathetic stimulation decreases it. This regulation of contraction without changes in fiber length is known as homometric regulation.
- Ions:
- The concentration of ions in the body is essential for heart function. Sodium (Na) is necessary for excitability, calcium (Ca) for muscle contraction, and potassium (K) for promoting diastole.
- Heart Rate:
- Heart rate also affects cardiac output. When the heart beats faster, cardiac output increases, provided that venous filling is not significantly reduced.
- In a rapidly beating heart, the diastolic phase shortens, reducing the initial fiber length, stroke volume, and overall cardiac output.
- Conversely, when the heart beats more slowly, the diastolic phase is prolonged, leading to increased venous filling and EDV. As a result, stroke volume and cardiac output increase.
- During physical exercise, although the heart rate increases significantly, stroke volume also rises moderately, leading to a substantial increase in cardiac output.
- Peripheral Resistance (Afterload):
- Afterload refers to the resistance the ventricles must overcome to eject blood. If resistance increases, the heart pumps out less blood, reducing cardiac output.
- Aortic pressure, and in some cases, the diameter of the aortic valve, are primary determinants of afterload for the left side of the heart.
The effects of venous return, heart muscle fiber length, and peripheral resistance on cardiac output have been studied through various experimental models, such as heart-lung preparations in animals. These studies demonstrate how altering venous pressure and peripheral resistance can change cardiac output, even when the heart’s nerves are not functioning.
Distribution of Cardiac Output
Cardiac output, the volume of blood pumped by the heart per minute, is distributed to various organs and tissues to meet their metabolic demands. The distribution of cardiac output varies depending on the body’s physiological state, such as rest, exercise, or specific metabolic conditions. Certain organs receive a greater proportion of blood due to their critical roles in maintaining essential functions like filtration, nutrient absorption, and oxygen supply. Below is a detailed breakdown of how cardiac output is distributed to various organs.
- Liver (Splanchnic Circulation):
- The liver receives the highest amount of blood flow per minute, approximately 1400 ml/min. This high volume is essential for the liver’s functions in metabolism, detoxification, and storage of nutrients. Blood reaches the liver mainly via the portal vein, which brings blood from the gastrointestinal tract, and to a lesser extent from the hepatic artery.
- Kidneys:
- While the kidneys receive 1000 ml/min of blood in total, they are unique in that they receive the highest amount of blood per unit weight—350-400 ml/100 gm of tissue per minute. This is due to their role in filtering the blood, removing waste products, and regulating electrolytes, fluids, and blood pressure.
- Skeletal Muscle:
- Skeletal muscles receive 800 ml/min of blood under resting conditions. Blood flow to skeletal muscle increases substantially during exercise to meet the increased demand for oxygen and nutrients, as well as to remove metabolic byproducts.
- Brain:
- The brain receives 750 ml/min of blood, which is crucial for maintaining constant oxygen and glucose supply. Even though the brain represents only about 2% of the body’s weight, it requires a steady and significant portion of cardiac output due to its high metabolic rate and sensitivity to oxygen deprivation.
- Heart:
- The heart itself receives 250 ml/min of blood through the coronary arteries. This blood flow is critical for providing oxygen to the myocardium, which is essential for sustaining the continuous pumping action of the heart.
- Skin:
- The skin receives 300 ml/min of blood under normal conditions. This blood flow is crucial for thermoregulation, allowing the body to dissipate heat or retain warmth, depending on environmental temperatures and the body’s needs.
- Other Tissues:
- Other organs and tissues, including the gastrointestinal tract, spleen, and the reproductive organs, receive a combined total of 600 ml/min of blood. The distribution of blood to these areas can vary depending on specific physiological demands, such as digestion or hormonal activity.
- King J, Lowery DR. Physiology, Cardiac Output. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470455/
- https://www.hansrajcollege.ac.in/hCPanel/uploads/elearning/elearning_document/Cardiac_Output_and_it_s_Regulation.pdf
- https://www.nejm.org/doi/abs/10.1056/NEJM196710122771509
- https://ksumsc.com/download_center/Archive/1st/439/4.%20Cardiovascular%20Block/Male%20Group/Physiology/L7%29%20Cardiac%20output%20%26%20Regulation%20of%20Stroke%20volume.pdf
- https://www.biologydiscussion.com/human-physiology/cardiovascular-system/cardiac-output-meaning-determination-and-regulation/62472
- https://www.biologydiscussion.com/human-physiology/cardiovascular-system/cardiac-output-meaning-and-measurement-cardiovascular-system-biology/85191
- https://www.biologydiscussion.com/animals-2/cardiac-output/cardiac-output-control-and-methods-heart-animals-biology/81756