What is Carbon Monoxide Poisoning?
- Carbon monoxide (CO) poisoning is a critical medical concern characterized by the accumulation of carbon monoxide in the bloodstream. This insidious gas, produced by the incomplete combustion of carbon-containing fuels such as gas, wood, propane, and charcoal, poses significant health risks due to its ability to displace oxygen in hemoglobin. When inhaled, carbon monoxide binds to hemoglobin more effectively than oxygen, thereby reducing the blood’s oxygen-carrying capacity. Consequently, tissues become starved for oxygen, leading to potential cellular damage and, in severe cases, death.
- Carbon monoxide is particularly dangerous because it is tasteless, odorless, and colorless. These properties make it difficult to detect, and individuals may not recognize they are being poisoned until they experience severe symptoms or loss of consciousness. Common symptoms of CO poisoning include headache, weakness, dizziness, nausea, tachycardia (rapid heartbeat), and tachypnea (increased breathing rate). Due to the nonspecific nature of these symptoms, carbon monoxide poisoning often mimics other medical conditions, complicating diagnosis.
- The primary sources of carbon monoxide in residential and industrial settings include malfunctioning appliances, poorly vented engines, and confined spaces where combustion occurs. Inadequate ventilation exacerbates the risk, leading to the accumulation of carbon monoxide to harmful levels. Therefore, it is essential to ensure that living and working environments are equipped with proper ventilation and functioning carbon monoxide detectors.
- Upon exposure, the immediate course of action is to remove the individual from the source of carbon monoxide and into fresh air. Prompt medical attention is crucial, especially in cases of severe exposure where the person may be unconscious or unresponsive. Emergency medical services should be contacted without delay to provide necessary interventions.
- The management of carbon monoxide toxicity involves a multidisciplinary approach, often requiring collaboration among healthcare professionals. Treatment typically includes administering oxygen, which helps to displace carbon monoxide from hemoglobin, thereby restoring the oxygen-carrying capacity of the blood. In severe cases, hyperbaric oxygen therapy may be indicated to expedite recovery and reduce the risk of long-term neurological damage.
Pathophysiology of Carbon Monoxide Poisoning
The pathophysiology of carbon monoxide (CO) poisoning involves complex interactions within the body that result in severe physiological disturbances. The following points summarize the key aspects of how carbon monoxide affects human health:
- Entry Mechanism: Carbon monoxide enters the body primarily through inhalation via the lungs. Upon exposure, it can interact directly with lung parenchyma, potentially causing tissue damage independent of blood transport.
- Delivery via Hemoglobin: Once in the bloodstream, carbon monoxide binds with hemoglobin to form carboxyhemoglobin (COHgb). This binding inhibits the ability of hemoglobin to transport oxygen effectively, leading to systemic hypoxia.
- Capillary Leakage: Exposure to carbon monoxide can cause capillary leakage of macromolecules from both the lungs and the systemic vasculature. This phenomenon can occur even at relatively low concentrations of carbon monoxide when exposure is prolonged, contributing to edema and further complications.
- Cerebral Effects: As carboxyhemoglobin levels rise, the body responds by dilating cerebral blood vessels, which increases coronary blood flow and capillary density. While this initially appears to mitigate hypoxia, continued exposure leads to central respiratory depression, primarily due to cerebral hypoxia. This condition affects the central nervous system’s ability to regulate breathing.
- Cardiac Effects: Carbon monoxide poisoning also has significant cardiac implications. Ventricular arrhythmias are a common complication and are often implicated as a primary cause of death in cases of CO poisoning. This is due to the heart’s increased demand for oxygen amid the compromised oxygen transport caused by elevated COHgb levels.
- Myocardial Impairment: Research indicates that myocardial impairment can begin at relatively low levels of carboxyhemoglobin, specifically around 20%. This impairment can lead to further cardiovascular complications and contributes to the overall morbidity associated with carbon monoxide poisoning.
- Cause of Death: The primary causes of mortality in cases of carbon monoxide poisoning often stem from a combination of hypoxia (lack of oxygen) and ischemia (insufficient blood supply) during the acute event. This dual effect exacerbates the damage to vital organs, especially the heart and brain.
Toxicokinetics of Carbon Monoxide Poisoning
The toxicokinetics of carbon monoxide (CO) poisoning encompasses the absorption, distribution, metabolism, and elimination of carbon monoxide within the body. Understanding these processes is critical for effective management and treatment of carbon monoxide exposure.
- Binding Affinity: Hemoglobin (HGB) has a binding affinity for carbon monoxide that is 220 times greater than its affinity for oxygen. This high binding affinity results in the formation of carboxyhemoglobin (COHgb), significantly impairing the blood’s ability to transport oxygen.
- Absorption: Carbon monoxide is absorbed through the lungs upon inhalation. Once in the bloodstream, it rapidly binds with hemoglobin, forming COHgb and thereby reducing the availability of oxygen to tissues.
- Half-Life in Ambient Air: In a standard room environment, which typically contains 21% oxygen, the half-life of carbon monoxide is approximately 320 minutes. This means that it takes a significant amount of time for half of the carbon monoxide in the body to be eliminated under normal atmospheric conditions.
- Half-Life in 100% Oxygen: When an individual is provided with 100% oxygen, the half-life of carbon monoxide is markedly reduced to less than 90 minutes. The increased availability of oxygen facilitates the displacement of carbon monoxide from hemoglobin, allowing for quicker elimination from the body.
- Half-Life with Hyperbaric Oxygen: The use of hyperbaric oxygen therapy (HBOT) at a pressure of 3 ATA (atmospheres absolute) significantly decreases the half-life of carbon monoxide to approximately 23 minutes. This accelerated elimination is crucial in cases of severe carbon monoxide poisoning, as it can mitigate the toxic effects more effectively than standard oxygen therapy.
- Treatment Protocol: The only adequate treatment for significant carbon monoxide poisoning is hyperbaric oxygen therapy. This method not only enhances the removal of carbon monoxide from the bloodstream but also helps restore normal oxygen levels in tissues, thereby preventing potential long-term complications.
Diagnosis of Carbon Monoxide Poisoning
Below are the key conditions that should be considered:
- Alcohol Toxicity: Symptoms of alcohol intoxication, such as confusion, dizziness, and headache, can overlap with those of carbon monoxide poisoning. Therefore, a thorough history of alcohol consumption is important in evaluating the patient.
- Depression and Suicide: Mental health conditions, particularly severe depression, can lead to symptoms such as lethargy and cognitive impairment, which may mimic those seen in CO poisoning. Evaluating the patient’s psychological state is essential for accurate diagnosis.
- Diabetic Ketoacidosis (DKA): DKA can present with altered mental status, weakness, and abdominal pain. Blood glucose levels and ketone bodies should be assessed to differentiate this condition from carbon monoxide toxicity.
- Encephalitis: This inflammation of the brain can result in neurological symptoms similar to those of CO poisoning, including confusion and altered consciousness. Diagnostic imaging and cerebrospinal fluid analysis may be necessary to confirm or exclude this diagnosis.
- Hypothyroidism: Patients with hypothyroidism may exhibit symptoms such as fatigue, confusion, and depression. Thyroid function tests should be conducted to rule out this condition.
- Labyrinthitis: Inflammation of the inner ear, or labyrinthitis, can cause dizziness and balance issues, which may be confused with the effects of carbon monoxide exposure. A detailed history and physical examination can aid in distinguishing these conditions.
- Meningitis: Symptoms of meningitis, including fever, headache, and stiff neck, may overlap with those of CO poisoning. A lumbar puncture and analysis of cerebrospinal fluid can help confirm the diagnosis of meningitis.
- Methemoglobinemia: This condition arises when hemoglobin is altered and cannot effectively carry oxygen, leading to symptoms such as cyanosis and altered mental status. A specific blood test can confirm methemoglobinemia, facilitating differentiation from carbon monoxide poisoning.
- Migraine Headache: Migraine episodes can manifest with headache, nausea, and photophobia, similar to CO poisoning symptoms. A detailed patient history regarding headache patterns can assist in distinguishing between the two conditions.
- Opioid Toxicity: Opioid overdose can present with respiratory depression, altered consciousness, and pinpoint pupils, resembling some effects of carbon monoxide poisoning. A thorough drug history and specific toxicology screening can clarify this diagnosis.
Prevention of Carbon Monoxide Poisoning
Preventing carbon monoxide (CO) poisoning is essential for ensuring the safety of individuals in homes, vehicles, and recreational environments. Effective measures can mitigate the risks associated with this colorless, odorless gas. Below are key strategies for preventing carbon monoxide poisoning:
- Install Carbon Monoxide Detectors: It is crucial to have carbon monoxide detectors installed in the home, particularly near sleeping areas on every level. Regularly checking the batteries—at least twice a year, ideally coinciding with smoke detector maintenance—ensures that these devices function properly.
- Respond Promptly to Alarms: If a carbon monoxide alarm sounds, it is vital to take it seriously. Individuals should immediately evacuate the premises and contact emergency services (911 or the fire department) to address the situation. Detectors are also available for use in motor homes and boats, emphasizing the need for vigilance in all living environments.
- Practice Safe Vehicle Use: To minimize carbon monoxide exposure from vehicles, always open the garage door before starting the car. It is crucial never to leave a running vehicle in an attached garage, even with the door open, as CO can accumulate rapidly.
- Proper Use of Gas Appliances: Gas appliances must be used solely for their intended purposes. For instance, gas stoves or ovens should never be utilized for heating spaces. Additionally, gas camp stoves should only be used outdoors. Fuel-burning space heaters should only be operated when someone is awake to monitor them, and proper ventilation (open doors or windows) is essential.
- Ensure Adequate Space Around Appliances: Maintaining appropriate spacing around fuel-burning appliances and engines, such as gas appliances, space heaters, and wood-burning stoves, is vital. These appliances must be properly vented to prevent CO accumulation.
- Professional Installation and Maintenance: All gas, oil, or coal-burning appliances should be installed by qualified professionals. Furthermore, routine servicing by a qualified service provider at least once a year is necessary to ensure safe operation.
- Maintain Fireplaces: Fireplaces require regular maintenance to function safely. Annual cleaning of the chimney and flue is necessary to remove any obstructions or buildup that could contribute to CO production.
- Keep Vents and Chimneys Clear: During home renovations or remodeling, it is crucial to ensure that vents and chimneys remain unblocked. Verify that they are not obscured by tarps, debris, or other materials that could impede proper airflow.
- Repair Sources of Carbon Monoxide: In the event of carbon monoxide poisoning occurring in the home, it is critical to locate and repair the source before reoccupying the space. Engaging a qualified service professional to inspect and repair any appliances suspected of causing the leak is essential for safety.
Symptoms of Carbon Monoxide Poisoning
Carbon monoxide (CO) poisoning poses a significant risk due to its insidious nature and potential for severe health impacts. Understanding the symptoms of CO poisoning is essential for prompt recognition and intervention. The effects primarily target the brain and heart, leading to a range of clinical manifestations that can be easily confused with other conditions, such as influenza.
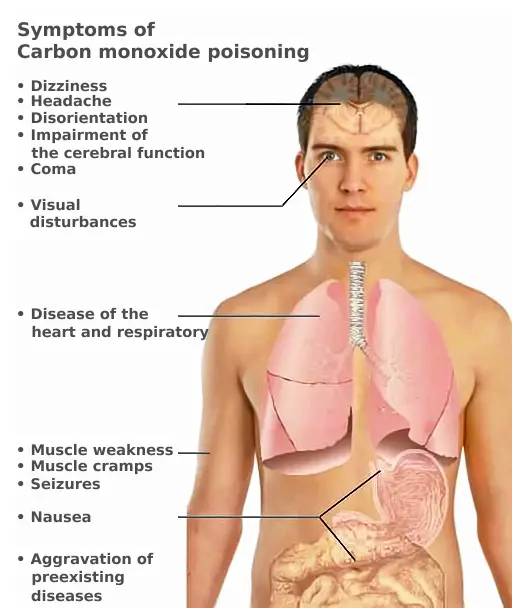
- Initial Symptoms:
- Headache: Often one of the first signs, a headache may occur as CO interferes with oxygen delivery to the brain.
- Weakness: Individuals may experience an unusual sense of fatigue or weakness, reflecting the body’s struggle to obtain sufficient oxygen.
- Dizziness: This symptom arises from impaired oxygenation, leading to a feeling of lightheadedness or unsteadiness.
- Nausea or Vomiting: Gastrointestinal disturbances, such as nausea or vomiting, may occur as the body reacts to the toxic effects of CO.
- Shortness of Breath: Increased respiratory effort may be required as the body attempts to compensate for reduced oxygen availability.
- Confusion: Cognitive impairments, including confusion and disorientation, can develop as brain oxygen levels diminish.
- Blurred Vision: Visual disturbances may also be present, resulting from the effects of hypoxia on the optic pathways.
- Drowsiness: A sense of extreme tiredness may occur, making individuals less responsive to their environment.
- Loss of Muscle Control: Coordination may be compromised, leading to difficulty in controlling movements.
- Loss of Consciousness: In severe cases, exposure can lead to unconsciousness, a critical emergency requiring immediate medical attention.
- Delayed Neurological Symptoms:
- After recovering from initial poisoning, some individuals may experience persistent neurological symptoms, especially those who had lost consciousness during exposure or were older.
- Symptoms may include:
- Memory Loss: Difficulty recalling recent events or information may persist.
- Personality Changes: Alterations in behavior and mood can occur, affecting interpersonal relationships and daily functioning.
- Movement Problems: Motor control issues may develop, leading to tremors or difficulties in coordination.
- Risk Factors:
- CO poisoning can be especially dangerous for individuals who are asleep, drugged, or intoxicated, as they may not recognize the symptoms until it is too late. Therefore, serious complications, such as brain damage or death, can occur before any awareness of a problem is established.
- Complications of Carbon Monoxide Toxicity:
- The consequences of carbon monoxide poisoning can extend beyond immediate symptoms, potentially leading to long-term complications, including:
- Amnesia: Difficulty in recalling past events may persist.
- Dementia: Cognitive decline can develop as a result of neurological damage.
- Irritability: Increased emotional instability may be observed.
- Psychosis: Severe disturbances in perception or thought processes can occur.
- Memory Loss: Continued challenges with short-term and long-term memory may be experienced.
- Loss of Executive Function: Individuals may struggle with planning, organization, and decision-making skills.
- Speech Deficit: Impairments in communication abilities may arise.
- Parkinson’s Disease: Symptoms resembling Parkinson’s disease, such as tremors and rigidity, may develop.
- Depression: Mood disorders may emerge following the traumatic experience of CO poisoning.
- Cortical Blindness: In some cases, damage to the visual cortex can result in visual impairments.
- The consequences of carbon monoxide poisoning can extend beyond immediate symptoms, potentially leading to long-term complications, including:
Treatment and Management of Carbon Monoxide Poisoning
The management of carbon monoxide (CO) poisoning is crucial due to the serious health risks associated with the condition. Prompt treatment is vital to minimize potential complications, especially neurological impairments. The foundational approach to treatment involves the administration of supplemental oxygen, which facilitates the elimination of carbon monoxide from the bloodstream and enhances oxygen delivery to tissues.
- Immediate Treatment with Supplemental Oxygen:
- Supplemental oxygen should be initiated as soon as CO poisoning is suspected. This treatment is essential for all patients and must be continued throughout the management process to ensure effective detoxification and oxygenation.
- Emergency Treatment Protocol:
- Patients exhibiting significant symptoms, including transient loss of consciousness, cardiac ischemia, altered mental status, tachycardia, hypotension, and elevated carboxyhemoglobin (COHgb) levels, require emergent intervention.
- In these cases, hyperbaric oxygen therapy (HBOT) is recommended. This treatment involves placing the patient in a hyperbaric chamber where they breathe 100% oxygen at increased atmospheric pressure, significantly enhancing the elimination of carbon monoxide from the body.
- Availability and Timing of Hyperbaric Oxygen Therapy:
- Although hyperbaric oxygen centers are available in every state, only a limited number of these facilities exist in the United States. Therefore, accessibility can be a concern.
- The best clinical outcomes are achieved when patients receive their first hyperbaric treatment within six hours of the poisoning event. This timely intervention is critical for reducing the risk of long-term neurological damage.
- Treatment Regimen:
- Most hyperbaric physicians typically prescribe three treatments within the first 24 hours. Following these initial sessions, the patient’s symptoms and responses are reassessed to determine if additional daily treatments are necessary.
- Despite the use of hyperbaric therapy, it is important to note that up to 40% of patients may still experience chronic neurocognitive impairments post-recovery. Consequently, a neuropsychological evaluation is recommended approximately one to two months after recovery to assess cognitive function and any lasting effects.
- Exploration of Alternative Therapies:
- While hyperbaric oxygen remains the primary treatment for severe CO poisoning, there is a lack of easily accessible alternative therapies. Ongoing research includes case reports and studies on novel treatments, such as lung phototherapy, although these options are still in developmental stages.
- Blumenthal I. Carbon monoxide poisoning. J R Soc Med. 2001 Jun;94(6):270-2. doi: 10.1177/014107680109400604. PMID: 11387414; PMCID: PMC1281520.
- Hanley ME, Patel PH. Carbon Monoxide Toxicity. [Updated 2023 Jan 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430740/
- https://www.mayoclinic.org/diseases-conditions/carbon-monoxide/symptoms-causes/syc-20370642
- https://www.verywellhealth.com/carbon-monoxide-poisoning-symptoms-4161052
- https://en.wikipedia.org/wiki/Carbon_monoxide_poisoning