What is Blood pressure?
- Blood pressure (BP) refers to the force exerted by circulating blood against the walls of blood vessels. This pressure predominantly arises from the heart’s rhythmic contractions as it pumps blood through the circulatory system. When the term “blood pressure” is used without any qualifiers, it typically denotes the pressure measured in the brachial artery, which is the most common site for such assessments.
- Blood pressure is quantified in terms of two distinct measurements: systolic pressure and diastolic pressure. Systolic pressure represents the maximum pressure in the arteries during a heartbeat, while diastolic pressure indicates the minimum pressure that occurs between heartbeats. These values are expressed in millimeters of mercury (mmHg) or kilopascals (kPa). The disparity between systolic and diastolic pressures is termed pulse pressure, while the average pressure throughout a complete cardiac cycle is referred to as mean arterial pressure.
- As one of the vital signs—alongside respiratory rate, heart rate, oxygen saturation, and body temperature—blood pressure is integral to evaluating an individual’s health status. The typical resting blood pressure for a healthy adult is approximately 120 mmHg systolic over 80 mmHg diastolic, commonly represented as “120/80 mmHg.” Globally, the average blood pressure has remained relatively stable since 1975, with values around 127/79 mmHg for men and 122/77 mmHg for women. However, these averages can mask significant regional variations in blood pressure trends.
- Traditionally, blood pressure measurement is performed non-invasively through auscultation, where a healthcare provider listens to arterial sounds using a stethoscope while the artery is compressed by a sphygmomanometer. This method is regarded as the gold standard for accuracy in clinical settings. Nonetheless, the use of semi-automated devices has gained popularity due to concerns over mercury toxicity, cost-effectiveness, and ease of use, particularly in home or ambulatory settings. Modern automated devices, validated against international standards, provide accurate readings with an average difference of 5 mmHg or less from standardized methods.
- Blood pressure is influenced by several physiological factors, including cardiac output, systemic vascular resistance, blood volume, and arterial stiffness. Additionally, it can fluctuate based on a person’s emotional state, physical activity, and overall health. In the short term, blood pressure regulation involves baroreceptors that relay information to the brain, which subsequently adjusts the nervous and endocrine systems to maintain stable pressure levels.
- Blood pressure can manifest as hypotension, characterized by abnormally low values, or hypertension, defined as persistently elevated readings. Normal blood pressure is referred to as normotension. Both hypotension and hypertension can arise from various causes, with hypertension being more prevalent and recognized as a significant risk factor for severe health conditions, including stroke, heart disease, and kidney failure. Understanding blood pressure dynamics is essential for effective health assessment and management.
Factors Regulating Blood Pressure
The regulation of blood pressure is a complex and dynamic process that involves multiple systems working together to maintain homeostasis. Even under normal physiological conditions, arterial blood pressure can exhibit variability. However, the body employs four primary regulatory systems to ensure that blood pressure remains within acceptable ranges. These systems include the nervous system, the renal system, the hormonal system, and local/regional mechanisms.
- The Nervous System (Short-Term Regulatory System):
- The nervous system represents the fastest mechanism for regulating blood pressure.
- It responds within minutes to changes in blood pressure, returning it to normal levels through rapid adjustments.
- Although the nervous system reacts quickly, its effect is short-lived. Over time, the system adapts to the new blood pressure level and becomes less effective in controlling further fluctuations.
- The vasomotor system plays a crucial role in this regulatory process, controlling arterial blood pressure primarily through vasoconstriction and vasodilation of blood vessels.
- Renal System (Long-Term Regulatory System):
- The renal system primarily governs the long-term regulation of blood pressure, functioning effectively over days, weeks, or even years.
- As blood pressure gradually changes, the nervous system’s ability to manage these fluctuations diminishes, making the renal system crucial for sustained blood pressure control.
- The kidneys regulate blood pressure through two main mechanisms:
- Control of Extracellular Fluid (ECF) Volume:
- When blood pressure increases, the kidneys enhance the excretion of water and sodium (pressure diuresis and pressure natriuresis), leading to a reduction in blood and ECF volume. This reduction helps normalize arterial blood pressure.
- Renin-Angiotensin System:
- This complex multi-organ endocrine system regulates vascular resistance, fluid balance, and electrolyte levels to control blood pressure.
- It influences sodium and water absorption in the kidneys and directly affects overall blood pressure.
- Control of Extracellular Fluid (ECF) Volume:
- The Hormonal System:
- Blood pressure regulation is significantly influenced by various hormones that either increase or decrease arterial blood pressure:
- Hormones that Increase Blood Pressure:
- Noradrenaline
- Adrenaline
- Aldosterone
- Vasopressin
- Thyroxine
- Serotonin
- Angiotensin
- Hormones that Decrease Blood Pressure:
- Bradykinin
- Histamine
- Acetylcholine
- Prostaglandin
- Brain Natriuretic Peptide (BNP)
- Atrial Natriuretic Peptide (ANP)
- C-type Natriuretic Peptide (CNP)
- Vasoactive Intestinal Polypeptide (VIP)
- Hormones that Increase Blood Pressure:
- Specifically, thyroxine and adrenaline increase systolic pressure while decreasing diastolic pressure, demonstrating the complexity of hormonal interactions in blood pressure regulation.
- Blood pressure regulation is significantly influenced by various hormones that either increase or decrease arterial blood pressure:
- Regional System:
- Local chemicals also play a significant role in blood pressure regulation, acting independently of the nervous, renal, and hormonal systems.
- These local chemicals can induce vasodilation or vasoconstriction in blood vessels, influencing blood flow and pressure.
- Medications designed to regulate blood pressure often target these mechanisms:
- Vasodilators expand blood vessels to enhance blood flow, lowering blood pressure.
- Vasoconstrictors narrow blood vessels, which raises blood pressure.
Disorders of Blood Pressure Control
Blood pressure disorders encompass conditions of both elevated and reduced blood pressure, as well as fluctuations that are considered abnormal. Understanding these disorders is essential for recognizing their implications on health, as they can lead to significant complications and chronic health issues.
- High Blood Pressure (Hypertension)
- Hypertension is characterized by persistent elevated blood pressure levels, often exceeding 130/80 mmHg, with severe cases classified as hypertensive emergencies when the systolic pressure exceeds 180 mmHg or diastolic pressure exceeds 120 mmHg.
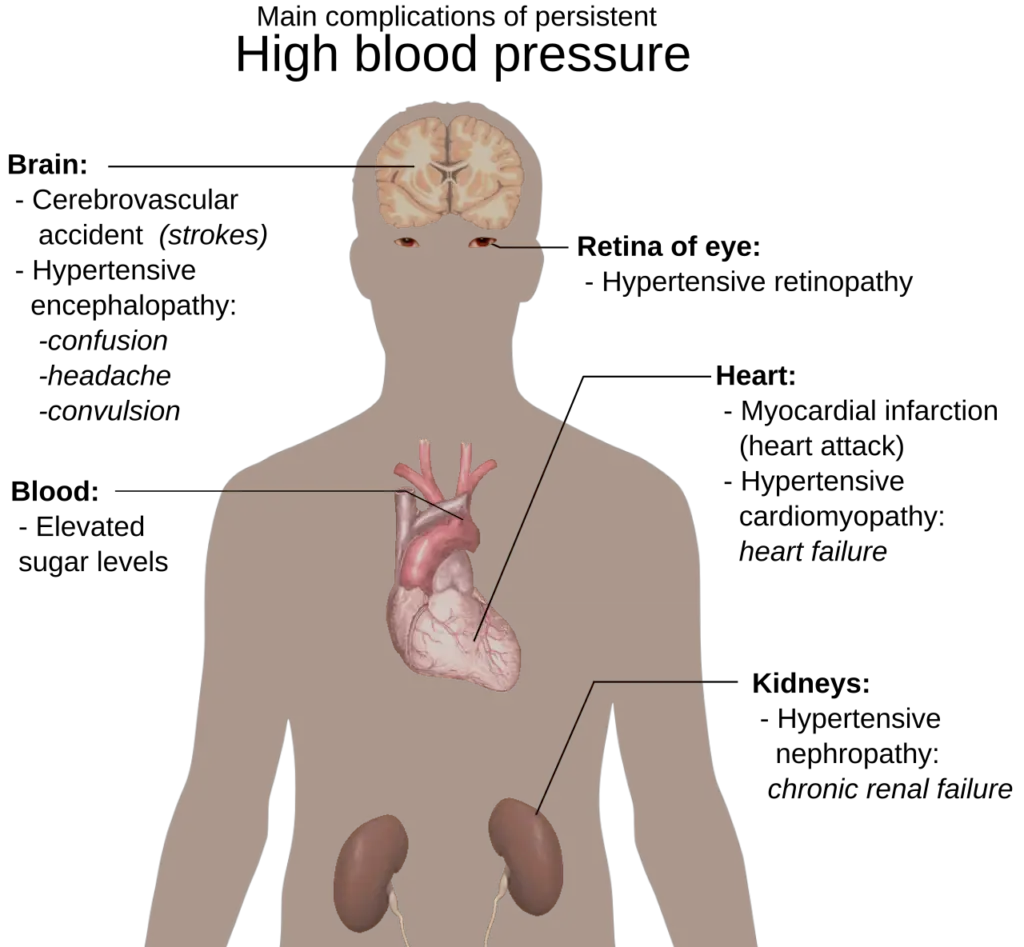
- Long-term high blood pressure can exert mechanical stress on arterial walls, leading to a range of complications:
- Increased workload on the heart, contributing to the thickening and weakening of the heart muscle over time.
- Promotion of atheroma formation (unhealthy tissue growth) within arterial walls, further exacerbating arterial stiffness.
- Persistent hypertension is a significant risk factor for severe cardiovascular events, including strokes, heart attacks, heart failure, and arterial aneurysms. It is also the leading cause of chronic kidney failure.
- Even moderate elevations in blood pressure can shorten life expectancy, with severely high mean arterial pressures significantly reducing survival rates without appropriate management.
- A notable correlation exists between high heart rate variability (HRV) and atrial fibrillation in individuals with hypertension.
- Risk factors for hypertension include both elevated systolic pressure and increased pulse pressure (the difference between systolic and diastolic pressures). Elevated pulse pressure has been identified as a strong predictor of cardiovascular events, particularly in older populations.
- Isolated systolic hypertension occurs when systolic blood pressure exceeds 140 mmHg, while diastolic blood pressure remains below 90 mmHg, raising health concerns.
- Changes in diastolic blood pressure can impact the severity of heart valve regurgitation, indicating a complex relationship between pressure levels and cardiac health.
- Low Blood Pressure (Hypotension)
- Low blood pressure, known as hypotension, is characterized by readings that are insufficient to maintain adequate blood flow and oxygen delivery, leading to symptoms such as dizziness, fainting, and in severe cases, circulatory shock.
- Various causes contribute to hypotension, including:
- Sepsis and hypovolemia (low blood volume), which can result from bleeding or dehydration.
- Cardiogenic shock and hormonal abnormalities, such as Addison’s disease.
- Eating disorders, particularly anorexia nervosa and bulimia, which can affect overall health and blood pressure regulation.
- Orthostatic Hypotension
- Orthostatic hypotension, also known as postural hypotension, is characterized by a significant drop in blood pressure (typically >20/10 mmHg) upon standing, reflecting the body’s failure to adjust to the gravitational effects on circulation.
- When an individual stands, blood pools in the lower extremities, causing a reduction in central blood volume and, consequently, a decrease in stroke volume and mean arterial pressure.
- Normally, compensatory mechanisms, including autonomic nervous system activation and the skeletal muscle pump, stabilize blood pressure within a minute. If these mechanisms fail, perfusion to the brain may become critically compromised, leading to symptoms like lightheadedness and fainting.
- Common causes of failure in compensation include underlying diseases and medications that affect the sympathetic nervous system.
- Variable or Fluctuating Blood Pressure (Labile Hypertension)
- Some degree of blood pressure fluctuation is normal; however, labile hypertension refers to significantly greater variability than typical levels.
- Increased fluctuation is associated with a higher risk of cardiovascular disease, brain small vessel disease, and dementia, regardless of average blood pressure levels.
- Recent studies indicate a link between blood pressure variability and adverse health outcomes, including mortality, strokes, and heart failure.
- Older adults and those on antihypertensive medications often exhibit more significant blood pressure fluctuations. The effects of different antihypertensive agents on variability and their potential impact on clinical outcomes remain areas of ongoing investigation.
- Johnson, R.H. (1976). Blood Pressure and Its Regulation. In: Caird, F.I., Dall, J.L.C., Kennedy, R.D. (eds) Cardiology in Old Age. Springer, Boston, MA. https://doi.org/10.1007/978-1-4615-8777-4_5
- National High Blood Pressure Education Program. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Bethesda (MD): National Heart, Lung, and Blood Institute (US); 2004 Aug. Classification of Blood Pressure. Available from: https://www.ncbi.nlm.nih.gov/books/NBK9633/
- https://ksumsc.com/download_center/Archive/1st/437/4.Cardiovascular%20Block/Teamwork/Physiology/11-%20regulation%20of%20blood%20pressure.pdf
- https://cdn.ps.emap.com/wp-content/uploads/sites/3/2016/11/091116_Orthostatic-hypotension-2_The-physiology-of-blood-pressure-regulation.pdf
- https://byjus.com/biology/factors-regulating-blood-pressure/
- https://en.wikipedia.org/wiki/Blood_pressure
- https://ksumsc.com/download_center/Archive/1st/438/4.%20Cardiovascular%20Block/Male/Physiology/11-%20Arterial%20Blood%20Pressure%20Regulation.pdf
- https://geekymedics.com/regulation-of-blood-pressure/
- https://www.hansrajcollege.ac.in/hCPanel/uploads/elearning/elearning_document/Blood_Pressure_and_it_s_Regulation.pdf