What are Actinomycetes?
Actinomycetes are a diverse group of Gram-positive, catalase-positive, nonmotile bacilli that exhibit characteristics bridging bacteria and fungi. Structurally, they resemble bacteria due to their cell walls containing muramic acid and prokaryotic nuclei, making them susceptible to antibiotics. However, their filamentous growth pattern, forming structures known as hyphae, is reminiscent of fungi. These hyphal forms can be observed in cultured bacterial isolates and clinical specimens.
Actinomycetes are primarily found in soil, decaying plant matter, and as part of the microbiota of humans and animals. They include anaerobic and facultatively anaerobic species under the genus Actinomyces. Their classification depends largely on the presence or absence of mycolic acids in their cell walls, leading to two broad groups:
- Actinomycetes with Mycolic Acids
This group comprises bacteria from families such as Corynebacteriaceae, Mycobacteriaceae, and Nocardiaceae. Members of the Nocardiaceae family include genera like Nocardia, Rhodococcus, Tsukamurella, and Gordonia. These organisms often stain poorly with Gram stain but exhibit partial acid-fastness due to the mycolic acids in their cell walls. - Actinomycetes without Mycolic Acids
This group contains various opportunistic pathogens such as Actinomadura, Nocardiopsis, Streptomyces, Dermatophilus, Oerskovia, Rothia, Tropheryma, and several thermophilic genera like Saccharopolyspora, Saccharomonospora, and Thermoactinomyces. These bacteria lack mycolic acids, differentiating them from the first group.
The ecological and medical significance of actinomycetes lies in their adaptability and functional diversity. Many soil-dwelling actinomycetes play a role in decomposing organic matter, while others, such as Streptomyces, are pivotal in producing antibiotics and other bioactive compounds. Some species, however, act as pathogens, causing infections in humans and animals.
Actinomycetes are remarkable for their ability to thrive in diverse environments, their role in natural biodegradation, and their contributions to medicine and agriculture through the production of various secondary metabolites.
| Taxonomic Rank | Classification |
| Domain | Bacteria |
| Phylum | Actinobacteria |
| Class | Actinobacteria |
| Order | Actinomycetales |
| Family | Actinomycetaceae |
What is Actinomyces?
- Actinomyces refers to a genus of Gram-positive, facultatively anaerobic or strictly anaerobic bacteria known for their filamentous, branching morphology. These bacteria are nonmotile and exhibit characteristics that position them between true bacteria and fungi. They are a natural component of the human and animal microbiota, residing predominantly in the oral cavity, gastrointestinal tract, and female genital tract.
- Among the species, Actinomyces israelii is the most frequently implicated in human infections. Other medically relevant species include Actinomyces gerencseriae, Actinomyces turicensis, Actinomyces radingae, Actinomyces europaeus, Actinomyces naeslundii, Actinomyces odontolyticus, Actinomyces viscosus, Actinomyces meyeri, and Propionibacterium propionicum. These species can occasionally transition from their commensal state to pathogenic, particularly when mucosal barriers are disrupted.
- Actinomyces infections, collectively termed actinomycosis, are characterized by the formation of chronic, suppurative abscesses and the presence of sulfur granules in discharge. These infections most commonly occur in the cervicofacial region but can also affect the thorax, abdomen, or pelvis. Treatment typically involves prolonged antibiotic therapy, often with penicillin, and, in some cases, surgical intervention.
- The genus Actinomyces holds ecological importance as well. It contributes to the degradation of organic matter in soil, illustrating its dual significance in natural environments and clinical microbiology.
Morphology of Actinomyces
Actinomyces exhibits unique structural characteristics that distinguish it from other bacteria. These features are crucial for understanding its role in both commensal and pathogenic settings.
- Gram-positive Structure
The cell wall of Actinomyces stains Gram-positive, indicating a thick peptidoglycan layer. This structural feature reinforces the cell’s rigidity and resistance to physical stress. - Nonmotile Nature
These organisms lack flagella or other motility structures, making them nonmotile. Their growth is typically confined to their immediate environment. - Non-sporing Bacteria
Unlike some other bacilli, Actinomyces does not form spores. Its survival depends on its ability to adapt to host environments rather than producing resistant forms. - Non–Acid-Fast Properties
Actinomyces species do not retain acid-fast stains, as they lack mycolic acids in their cell walls. This differentiates them from genera like Nocardia. - Size and Dimensions
These bacteria measure between 0.5 to 1 micrometer in diameter, placing them within the typical size range for prokaryotes. - Filamentous Growth
A defining feature of Actinomyces is its ability to grow in filaments. These elongated structures often fragment into bacillary and coccoid forms, reflecting a degree of morphological variability.
Characteristics of Actinomycetes
Actinomycetes are a group of bacteria with distinct characteristics that set them apart from other microbial groups. They are primarily known for their filamentous structure and slow growth rate, making them unique within the bacterial world.
- Size and Shape:
- Actinomycetes typically have a diameter of 1-2 µm.
- Their shape is rod-like with a filamentous or branched structure.
- The filaments contain mumaric acid, a compound unique to some of these organisms.
- Growth and Reproduction:
- Growth and reproduction occur more slowly compared to both bacteria and fungi, which is why actinomycetes are often referred to as “slow growers.”
- Aerobic and Anaerobic Nature:
- Most species of actinomycetes are aerobic, meaning they require oxygen to grow.
- A smaller number are anaerobes or facultative aerobes, capable of surviving without oxygen or in low-oxygen environments.
- Cell Wall Composition:
- The cell wall of actinomycetes contains mycolic acid, which is a characteristic feature of these bacteria, differentiating them from other bacterial groups.
- Genetic Composition:
- Actinomycetes have a G+C content ranging from 60-78%, indicating the proportion of guanine and cytosine in their DNA.
- Habitat and Abundance:
- Actinomycetes are highly abundant in soil (ranging from 10^6 to 10^8/g).
- They are also found in marine habitats, where they play significant ecological roles.
- Motility and Encapsulation:
- The majority of actinomycetes are non-motile, meaning they do not move actively.
- They are also non-capsulated, lacking the protective outer layers that some other bacteria possess.
- They are generally non-acid fast, meaning they do not retain certain dyes used in bacterial identification.
- Optimal Growth Conditions:
- Actinomycetes prefer to grow in alkaline pH environments, which influences their distribution and survival.
Actinomycetes are a group of bacteria that can cause a variety of infections in humans. These infections often stem from bacteria that naturally inhabit the environment, such as soil, and can be opportunistic, affecting people with weakened immune systems or those with other risk factors.
- Actinomyces species:
- Cervicofacial actinomycosis: Often referred to as “lumpy jaw,” this infection occurs in the jaw, neck, or face. It is frequently associated with poor oral hygiene and dental procedures.
- Thoracic actinomycosis: This type affects the lungs and chest, often causing a persistent cough, chest pain, and sometimes mimicking tuberculosis.
- Abdominal and pelvic actinomycosis: Can lead to severe pain and inflammation in the abdominal and pelvic regions. It is often linked to intra-abdominal surgeries or the use of intrauterine devices (IUDs).
- Nocardia species:
- Primary cutaneous nocardiosis: Infection typically occurs through traumatic injury to the skin, leading to abscess formation and slow-healing wounds.
- Bronchopulmonary infections: Nocardia can cause lung infections, leading to symptoms like cough, fever, and difficulty breathing.
- Secondary central nervous system infection: In immunocompromised individuals, Nocardia can spread to the brain, causing meningitis or abscess formation.
- Rhodococcus species:
- Pulmonary infections: Often seen in individuals with pre-existing lung conditions, Rhodococcus species can cause severe lung infections, resulting in symptoms like cough and shortness of breath.
- Opportunistic infections: Includes traumatic endophthalmitis, peritonitis in dialysis patients, and post-traumatic skin infections.
- Gordonia species:
- Known for causing opportunistic infections, particularly in immunocompromised individuals. These infections can affect various body systems and are often challenging to treat.
- Tsukamurella species:
- This genus also contributes to opportunistic infections, affecting people with weakened immune defenses. The infections may manifest in various body areas, particularly in those who are immunocompromised.
- Tropheryma whippelii:
- The causative agent of Whipple’s disease, a rare infection that affects the small intestine, causing malabsorption, weight loss, and gastrointestinal symptoms.
- Dermatophilus species:
- Responsible for exudative dermatitis, a skin condition that causes inflammation, lesions, and exudation, typically seen in animals but can also affect humans.
- Oerskovia species:
- Known to cause opportunistic infections such as catheter-associated bacteremia, traumatic endophthalmitis, and CNS shunt infections. These infections typically affect individuals with pre-existing conditions or those who have undergone invasive medical procedures.
Culture of Actinomyces
Actinomyces organisms are facultative anaerobes that thrive in environments with low oxygen levels. Their growth conditions and culture requirements are crucial for successful cultivation.
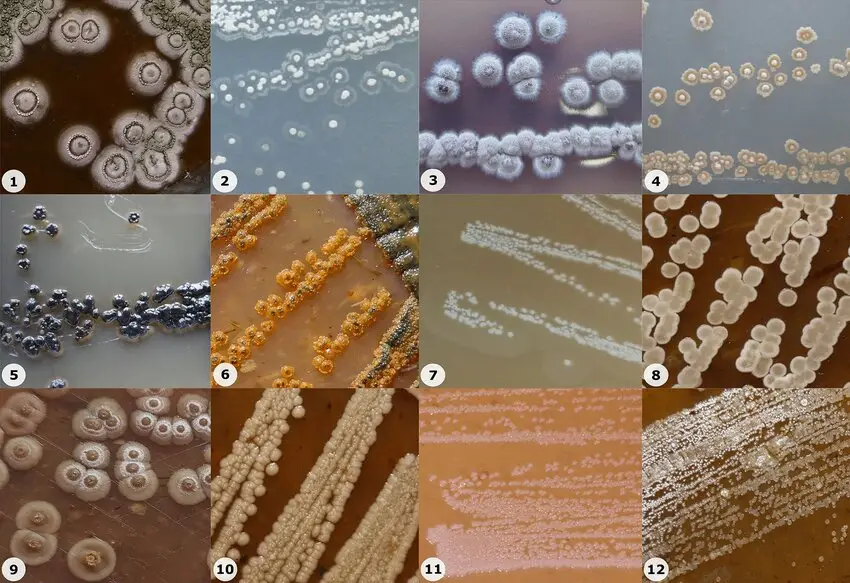
- Growth Conditions:
- Actinomyces grow best under anaerobic or microaerophilic conditions, meaning they require low levels of oxygen.
- The optimal temperature for growth is 35–37°C.
- The presence of 5–10% CO2 in the environment promotes better growth.
- Actinomyces species grow slowly, often requiring 3–4 days for visible growth.
- Some species, like Actinomyces israelii, may need as long as 7–14 days to show growth.
- Culture Media:
- Brain Heart Infusion (BHI) Agar: This is an enriched medium commonly used for culturing Actinomyces. The medium is often supplemented with 5% defibrinated rabbit, sheep, or horse blood.
- Under anaerobic to microaerophilic conditions, Actinomyces colonies on BHI agar exhibit a distinctive molar-tooth appearance.
- Liquid Media:
- Heart Infusion Blood and Thioglycollate Blood are commonly used as liquid media.
- These can be supplemented with 0.1–0.2% sterile rabbit serum to enhance growth.
- Brain Heart Infusion (BHI) Agar: This is an enriched medium commonly used for culturing Actinomyces. The medium is often supplemented with 5% defibrinated rabbit, sheep, or horse blood.
Life Cycle of Actinomycetes
The life cycle of actinomycetes is characterized by distinct stages that begin with spore germination and end with the release of mature spores into the environment.
- Germination:
- Actinomycetes start their life cycle as free spores, which remain dormant in the environment until favorable conditions trigger germination.
- When conditions are right, the spores begin to germinate by forming a germ tube.
- Vegetative Growth:
- The germ tube develops into primary mycelium (substrate hyphae), which grows within the medium.
- As the primary mycelium grows, secondary mycelium (aerial hyphae) forms above the substrate.
- Coiling:
- In unfavorable conditions, the aerial hyphae undergo a transformation, forming a spiral shape.
- Septation:
- As the vegetative hyphae mature, septation occurs, where a septum forms between the hyphae, segmenting them into distinct regions.
- Spore Maturation:
- The septum within the vegetative hyphae matures, leading to the formation of a chain of spores.
- Spores are formed via fragmentation or swelling of the hyphae.
- Release of Spores:
- When conditions worsen, the mature spores detach from the vegetative hyphae and become free spores in the environment, ready to begin the cycle anew.
Classification of Actinomycetes
Actinomycetes are a diverse group of bacteria that are categorized into several families based on their hyphal and reproductive structures. These families are distinguished by unique features, such as the presence of non-segmented or segmented hyphae, the structure of spores, and their growth characteristics.
- Streptomycetaceae:
- Characterized by non-segmented hyphae.
- Typically have 5-50 conidial spores per chain of aerial hyphae.
- Examples: Streptomyces, Microdlobaspone, Sporoctilhya.
- Nocardiaceae:
- Members possess non-segmented hyphae.
- Examples: Nocardia, Pseudonocardia.
- Micromonosporaceae:
- Known for non-segmented conidia, which exist singly, in pairs, or in chains.
- Examples: Micromonospora, Thermonospora, Thermoactinomycetes, Actinobifida.
- Actinoplanaceae:
- Members feature sporangiospores and hyphae that range from 0.2-2.0 µm in width.
- Examples: Streptosporangium, Actinoplanes, Plasmobispora, Dactylosporangium.
- Dermatophilaceae:
- Characterized by hyphae that undergo fragmentation, leading to the formation of a large number of motile structures.
- Example: Geodermatophilus.
- Frankiaceae:
- These actinomycetes are strictly associated with the roots of non-leguminous plants and contribute to nitrogen fixation by forming root nodules.
- Example: Frankia.
- Actinomycetaceae:
- Members of this family lack true mycelium and are generally facultative anaerobes.
- Example: Actinomyces.
Pathogenesis of Actinomyces
Actinomyces species, typically part of the normal flora in the oral cavity, lower gastrointestinal tract, and female genital tract, play a crucial role in human infections when conditions allow. Though usually benign, these organisms can become pathogenic under certain circumstances.
- Role of Companion Bacteria:
- Actinomyces is often found alongside other bacteria in the body, including Bifidobacterium dentium, Actinobacillus actinomycetemcomitans, Eikenella corrodens, Haemophilus aphrophilus, Bacteroides, Fusobacterium, staphylococci, and anaerobic streptococci.
- These companion bacteria are considered copathogens, meaning they can enhance the virulence of Actinomyces, making infections more likely or severe.
- Infection Process:
- Once Actinomyces establishes an infection, the host’s immune system responds with intense inflammation.
- This inflammation often leads to suppurative granulomatous and fibrotic reactions, processes where the body forms a type of chronic inflammation that can result in tissue scarring.
- Infection spreads contiguously, meaning it typically moves directly into adjacent tissues and organs, rather than traveling through the bloodstream initially.
- Complications:
- As the infection progresses, it leads to the formation of draining sinus tracts, which are passages through the skin or mucous membranes filled with damaged tissue and pus.
- Bacteria from these tracts can enter the bloodstream, allowing the infection to disseminate to distant organs, potentially causing systemic complications.
Clinical Syndromes of Actinomyces
Actinomycosis, caused by Actinomyces species, is a subacute to chronic infection marked by contiguous spread, suppurative, and granulomatous inflammation. This condition leads to the formation of abscesses and sinus tracts that discharge characteristic sulfur granules (white to yellowish granules). Actinomycosis can present in various clinical forms, depending on the site of infection.
- Cervicofacial Actinomycosis:
- This is the most common manifestation, accounting for about two-thirds of cases.
- It typically follows oral surgery in patients with poor oral hygiene.
- Initially, a soft tissue swelling occurs in the perimandibular region.
- Over time, the infection spreads into adjacent tissues, forming fistulas.
- These fistulas discharge purulent material containing sulfur granules.
- If untreated, the infection can spread to the blood, and eventually to brain and orbit.
- Thoracic Actinomycosis:
- Responsible for 15–20% of actinomycosis cases.
- Often caused by aspiration of oropharyngeal secretions or occasionally by esophageal perforation.
- It can also spread from neck or abdominal lesions or via blood circulation from distant sites.
- Commonly presents as a pulmonary infiltrate or a mass in the lung.
- If left untreated, it can extend to the pleura, pericardium, and chest wall, forming multiple sinuses that discharge sulfur granules.
- Abdominal and Pelvic Actinomycosis:
- Accounts for 10–20% of reported actinomycosis cases.
- The ileocecal region is the most frequently affected.
- Initially, the infection appears as a slow-growing tumor.
- It spreads to involve abdominal organs, including the abdominal wall, forming draining sinuses.
- Pelvic actinomycosis is often associated with the long-term use of intrauterine contraceptive devices (IUDs).
- The infection typically spreads directly from the uterus to the pelvic region.
Epidemiology of Actinomyces
Actinomycosis, caused by Actinomyces species, is a bacterial infection found across the globe. Its prevalence varies depending on several factors, including environmental conditions, socioeconomic status, and specific risk behaviors.
- Geographic Distribution:
- Actinomycosis is a worldwide condition, present in both developed and developing countries.
- It is more commonly found in rural areas, particularly affecting farm workers who may have higher exposure to risk factors such as trauma or poor hygiene.
- Risk Factors:
- Poor dental hygiene is a significant risk factor, as it creates an environment conducive to the growth of Actinomyces in the oral cavity.
- Individuals from low socioeconomic backgrounds are more frequently affected, likely due to limited access to healthcare, hygiene, and preventive dental care.
- Gender and Age Distribution:
- Actinomycosis predominantly affects men, with a male to female ratio of 4:3.
- An exception is seen in pelvic actinomycosis, which is more common in women, especially those who have used intrauterine contraceptive devices for extended periods.
- The condition is most commonly reported in young and middle-aged adults, highlighting the age group most susceptible to this infection.
Laboratory Diagnosis of Actinomyces
The laboratory diagnosis of actinomycosis relies on detecting Actinomyces species in patient specimens, typically through microscopy and culture methods. The presence of characteristic sulfur granules plays a crucial role in confirming the diagnosis.
- Specimens for Diagnosis:
- Common specimens include sputum, bronchial secretions, discharges, and infected tissues.
- These samples often contain large numbers of sulfur granules, a key diagnostic feature of the infection.
- Sulfur granules can also be collected from dressings removed from draining sinus tracts.
- It is important to transport specimens immediately to the laboratory, ideally under anaerobic conditions, to preserve the integrity of the samples.
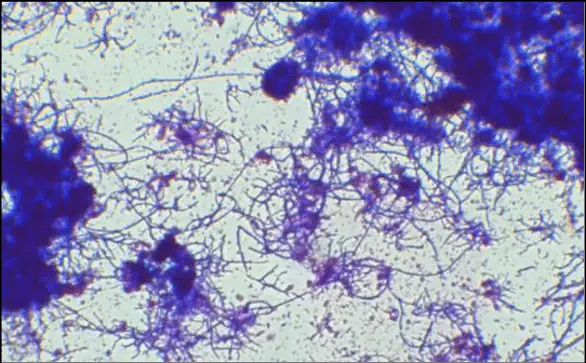
- Microscopy:
- The sulfur granules are typically white to yellow and vary in size, ranging from small specks to larger granules.
- These granules are carefully separated from pus or other specimens and collected from draining sinuses.
- The sulfur granules are then crushed between two slides and stained using either Gram or Ziehl–Neelsen staining methods, with 1% sulfuric acid used for decolorization.
- Under microscopic examination, Gram-positive hyphal fragments are seen, surrounded by a peripheral zone of swollen, club-shaped structures that radiate outward in a sunray appearance.
- These club-shaped structures are Gram-positive, acid-fast, and believed to be antigen complexes.
- Culture:
- Specimens containing sulfur granules or pus are cultured immediately under anaerobic conditions at 35–37°C for up to 14 days.
- The samples are inoculated on blood agar, BHI agar, and into thioglycollate broth for anaerobic incubation.
- The bacterium Actinomyces israelii produces large (0.5 mm), white, smooth, and lobulated colonies, often resembling a molar tooth after about 10 days of anaerobic incubation.
- Identification of the Bacteria:
- The colonies formed are identified using a combination of microscopy, biochemical reactions, direct fluorescent antibody tests, and gel immunodiffusion tests.
- The latter two tests are particularly useful for differentiating A. israelii from other species within the Actinomyces genus and from other filamentous anaerobes that may produce similar types of granules in tissues.
Treatment of Actinomyces
The treatment of actinomycosis primarily involves long-term antibiotic therapy, with high-dose penicillins or tetracyclines being the most commonly used medications.
- Antibiotic Therapy:
- Penicillins are typically the first-line treatment. High doses are administered over an extended period to effectively combat the infection.
- Tetracyclines can also be used as an alternative or in cases where penicillin is not suitable.
- Metronidazole, cotrimoxazole, sulfamethoxazole, and penicillinase-resistant penicillins like methicillin, oxacillin, and cloxacillin are not effective against Actinomyces species.
- Surgical Intervention:
- For more advanced or complicated cases of actinomycosis, surgical therapy is necessary.
- Surgical procedures may be required to remove infected tissue or to drain abscesses that do not respond to antibiotic treatment.
Prevention and Control of Actinomyces
Preventing and controlling actinomycosis primarily involves maintaining proper hygiene and addressing potential risk factors.
- Dental and Oral Hygiene:
- Regular and effective dental care is crucial in preventing actinomycosis.
- Good oral hygiene helps reduce the likelihood of infection, as the mouth is a common site for Actinomyces colonization.
- Regular brushing and flossing can prevent the buildup of plaque and the formation of abscesses that act as potential breeding grounds for the bacteria.
- Minimizing Risk Factors:
- Individuals with compromised health or weakened immune systems should take extra precautions.
- For farm workers or people in rural areas who may be more at risk, avoiding injuries to the skin or mucous membranes can reduce exposure to Actinomyces.
Economic Importance of Actinomycetes
Actinomycetes are crucial organisms with broad applications across industries, healthcare, agriculture, and environmental management. Their diverse roles make them economically significant in various sectors, from bioremediation to pharmaceutical production.
- Bioremediation:
- Actinomycetes break down complex carbohydrates such as chitin, cellulose, and hemicellulose.
- They are involved in degrading toxic compounds, playing an essential role in cleaning up the environment.
- Able to survive in harsh conditions, like high temperatures up to 50°C, which is vital for processes like composting.
- Biomedical Use:
- Actinomycetes produce some of the most well-known antibiotics:
- Tetracycline and erythromycin target bacterial ribosomes, helping treat respiratory infections.
- Vancomycin works on the bacterial cell wall of Streptococcus aureus, treating infections.
- Rifampicin targets RNA polymerase, aiding in the treatment of tuberculosis and leprosy.
- Adriamycin is used in cancer treatment.
- Amphotericin attacks fungal membranes with minimal side effects.
- Rapamycin is used in organ transplantation.
- Actinomycetes produce some of the most well-known antibiotics:
- Regulating Plant Growth:
- Actinomycetes in the soil produce phytohormones, extracellular enzymes, and bioactive compounds that enhance plant growth.
- These compounds help plants by:
- Protecting against phytopathogens and pests.
- Producing indole 3-acetic acid, siderophores, and solubilizing phosphate to promote plant health.
- Industrial Use:
- Actinomycetes are responsible for producing several key enzymes with wide industrial applications:
- Lipase in detergents and pharmaceuticals.
- Cellulases for the animal feed industry.
- Catalase in detergents.
- Amylase for use in food, textile, and paper industries.
- Chitinase for use in biochemical industries.
- Actinomycetes are responsible for producing several key enzymes with wide industrial applications:
- Agroactive Compounds:
- Actinomycetes are abundant in the rhizospheric zone of plants, where they produce agroactive compounds.
- They actively colonize plant roots, offering protection against pathogenic fungi and other harmful microorganisms.
- Frankia, an example, forms a symbiotic relationship with plants, promoting root nodule formation and contributing to nitrogen fixation.
- Preventing Biocorrosion:
- Actinomycetes produce secondary metabolites that serve as antimicrobial substances.
- These substances help prevent biocorrosion by attacking pathogenic and phytopathogenic microorganisms that contribute to corrosion.
- Biopesticide Use:
- Actinomycetes are effective biopesticides, targeting insects like Musca domestica and Culex quinquefasciatus.
- They eliminate up to 90% of insects at their larval and pupal stages.
- https://www.slideshare.net/ANKURKUMAR442/actinomycetes-234784559
- https://www.slideshare.net/kalpeshvaghela8/actinomycetes-178490069
- https://www.differencebetween.com/difference-between-actinomyces-and-actinomycetes/
- https://www.researchgate.net/figure/Actinomycetes-microorganisms-after-the-application-of-Gram-staining-400-fold_fig2_317132368
- https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2016.02149/full
- https://biologyreader.com/actinomycetes.html
- https://www.emnz.com/blogs/news/the-contribution-of-actinomycetes
- https://www.britannica.com/science/actinomycete
- https://www.slideshare.net/slideshow/actinomycetes-122126860/122126860
- https://en.wikipedia.org/wiki/Actinomycetota
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.