What is Wuchereria bancrofti?
- Wuchereria bancrofti is a parasitic nematode belonging to the group of filarial worms, which are primarily transmitted by mosquito vectors. It plays a significant role in the global burden of lymphatic filariasis, a debilitating condition that primarily affects the lymphatic system. Alongside Brugia malayi and Brugia timori, W. bancrofti is one of the three key species responsible for this disease.
- The distribution of Wuchereria bancrofti is notably extensive, with over 120 million individuals infected worldwide. The regions most affected include Central Africa, the Nile Delta, parts of South and Central America, and tropical areas of Asia, extending to southern China and the Pacific islands. This widespread prevalence highlights the public health significance of the parasite and its associated disease.
- Transmission of W. bancrofti occurs through the bite of infected mosquitoes, which act as vectors for the larvae. Once inside the human host, the larvae migrate to the lymphatic system, where they mature into adult worms. The presence of these adult worms can lead to a range of complications, primarily lymphatic filariasis, characterized by severe swelling of the limbs and genitals due to the accumulation of lymphatic fluid.
- Without timely and appropriate treatment, the infection can progress to more severe forms, including lymphatic damage and complications such as elephantiasis. In rare instances, W. bancrofti can also lead to tropical pulmonary eosinophilia, a condition marked by respiratory symptoms and elevated eosinophil counts in the blood.
- Although no commercially available vaccine exists to prevent Wuchereria bancrofti infection, effective treatment regimens utilizing antifilarial medications have shown high cure rates. The World Health Organization (WHO) has implemented the Global Program to Eliminate Lymphatic Filariasis, aiming to eradicate the disease as a public health concern. Initially set to achieve this goal by 2020, the program has faced challenges and setbacks in reaching its objectives.
- The study and management of Wuchereria bancrofti are crucial not only for individual health outcomes but also for broader public health initiatives. Understanding the lifecycle, transmission dynamics, and impact of this nematode is essential for developing effective control strategies and reducing the incidence of lymphatic filariasis globally.
Scientific classification
| Domain: | Eukaryota |
| Kingdom: | Animalia |
| Phylum: | Nematoda |
| Class: | Chromadorea |
| Order: | Rhabditida |
| Family: | Onchocercidae |
| Genus: | Wuchereria |
| Species: | W. bancrofti |
Hosts and Vectors of Wuchereria bancrofti
- Definitive Hosts:
- Humans serve as the definitive hosts for Wuchereria bancrofti. The adult worms reside in the lymphatic system of infected individuals, where they can live for several years, producing live offspring known as microfilariae.
- Unlike other filarial species, Wuchereria bancrofti does not have significant animal reservoirs. The presence of zoonotic filarial species, such as Brugia pahangi, is primarily noted in felids and certain primates, but these are of minimal epidemiological importance for Wuchereria bancrofti.
- Intermediate Hosts:
- The transmission of Wuchereria bancrofti occurs through various mosquito species, which act as intermediate hosts. The mosquitoes become infected when they take a blood meal from an infected human, ingesting microfilariae present in the bloodstream.
- The microfilariae then undergo several developmental stages within the mosquito, transforming into the infective third-stage (filariform) larvae. When the mosquito subsequently bites another human, these larvae are transmitted, initiating a new infection cycle.
- Vector Species:
- The vectors for Wuchereria bancrofti vary according to geographical distribution and include several genera of mosquitoes:
- Aedes spp.: These mosquitoes are known for their aggressive biting behavior and are prevalent in tropical and subtropical regions.
- Anopheles spp.: Although primarily recognized as malaria vectors, certain Anopheles species can also transmit Wuchereria bancrofti.
- Culex spp.: This genus is one of the most common vectors for Wuchereria bancrofti, especially in urban settings.
- Mansonia spp.: These mosquitoes are particularly associated with the transmission of lymphatic filariasis in specific geographic locations.
- Coquillettidia juxtamansonia: This lesser-known vector also plays a role in the transmission cycle of Wuchereria bancrofti in certain areas.
- The vectors for Wuchereria bancrofti vary according to geographical distribution and include several genera of mosquitoes:
- Geographical Variation in Transmission:
- The choice of mosquito vector can significantly influence the epidemiology of lymphatic filariasis. For instance, in regions where Aedes mosquitoes are prevalent, the transmission dynamics may differ from areas where Culex or Mansonia species dominate. Understanding these regional differences is critical for developing targeted vector control strategies.
- Impact on Disease Dynamics:
- The relationship between Wuchereria bancrofti and its mosquito vectors is vital for the persistence of lymphatic filariasis. Factors such as environmental conditions, mosquito breeding sites, and human behaviors all contribute to the transmission efficiency of this parasite.
- Therefore, effective control of the mosquito populations through measures such as habitat modification, insecticide use, and community education is essential in preventing the spread of Wuchereria bancrofti and reducing the incidence of lymphatic filariasis.
History and Distribution of Wuchereria bancrofti
Wuchereria bancrofti is a parasitic nematode responsible for lymphatic filariasis, a disease with historical significance dating back to ancient civilizations. The knowledge of filariasis, particularly its manifestations, has been documented for centuries, revealing the long-standing impact of this parasite on human health.
- Historical Context
- References to conditions resembling filariasis can be found in ancient texts. For instance, the Indian physician Sushrutha described elephantiasis, a severe manifestation of lymphatic filariasis, while Persian scholars like Rhazes and Avicenna also noted similar ailments.
- The term “Malabar leg” was introduced in 1709 by Clarke in Cochin, India, highlighting the painful swelling associated with the disease, primarily affecting the legs and genital regions.
- The discovery of the microfilariae, the larval stage of W. bancrofti, marked a significant milestone in the understanding of this parasite. Demarquay first observed these larvae in hydrocele fluid from a patient in Havana, Cuba, in 1863.
- The genus Wuchereria is named after the Brazilian physician Otto Wucherer, who documented the presence of microfilariae in chylous urine in 1868. Further contributions to the understanding of the life cycle of this nematode included Lewis’s demonstration of microfilariae in human blood in Calcutta in 1872.
- Key Discoveries
- In 1876, Bancroft provided the first comprehensive description of the adult female W. bancrofti, while the adult male was described later in 1888 by Bourne. These findings were pivotal in advancing the medical community’s understanding of the life stages of the parasite.
- Manson’s groundbreaking work in 1878 identified the Culex mosquito as a vector for W. bancrofti, marking the first recognition of insect transmission of a human disease. His follow-up studies in 1879 established the nocturnal periodicity of microfilariae in the peripheral blood, indicating specific times when the larvae are most prevalent, correlating with the feeding patterns of the mosquito vectors.
- Current Distribution
- Today, Wuchereria bancrofti is distributed across tropical and subtropical regions, particularly in sub-Saharan Africa, Southeast Asia, India, and various Pacific islands.
- Among these areas, India accounts for the largest number of filariasis cases. In India, endemic regions are predominantly found along coastal areas and riverbanks, though cases can arise in nearly all states, with the exception of the northwestern regions.
- The distribution of W. bancrofti is influenced by environmental factors conducive to mosquito breeding, including warm temperatures and high humidity. Such conditions facilitate the life cycle of the parasite, thereby increasing the risk of transmission and infection in human populations.
Habitat of Wuchereria bancrofti
This parasite relies on two distinct hosts to complete its life cycle: humans as the definitive host and female mosquitoes as the intermediate host.
- Definitive Host: Humans
- The adult W. bancrofti worms reside in the lymphatic system of human hosts.
- They are typically coiled within lymph nodes and lymphatic vessels, where they can obstruct lymphatic flow, leading to swelling and associated complications of lymphatic filariasis.
- Adult worms can remain viable for several years, contributing to a chronic infection that affects millions of people worldwide.
- Intermediate Hosts: Female Mosquitoes
- The transmission of W. bancrofti occurs through specific species of blood-feeding mosquitoes, primarily from the genera Culex, Aedes, and Anopheles.
- These mosquitoes serve as vectors that facilitate the life cycle of the parasite by ingesting microfilariae present in the blood of an infected human during a blood meal.
- Within the mosquito, the microfilariae undergo several developmental stages, transforming into infective larvae before being transmitted back to humans through subsequent bites.
- Microfilariae Habitat
- The larvae, known as microfilariae, circulate in the peripheral blood of infected individuals.
- Besides being found in the bloodstream, microfilariae may also appear in other body fluids, such as chylous urine and hydrocele fluid, indicating their mobility and adaptability within the host.
- Geographic Distribution
- Wuchereria bancrofti is endemic in tropical and subtropical regions across the globe, including Central Africa, the Nile Delta, parts of South and Central America, southern China, and the Pacific islands.
- The habitat conditions in these regions, including warm temperatures and high humidity, favor the survival and reproduction of the mosquito vectors, thereby facilitating the transmission of the parasite.
| Habitat Regions | tropical, freshwater |
| Terrestrial Biomes | rainforest |
| Aquatic Biomes | lakes and ponds, rivers and streams, temporary pools |
| Wetlands | marsh, swamp |
| Other Habitat Features | urban, suburban, agricultural |
Morphology of Wuchereria bancrofti
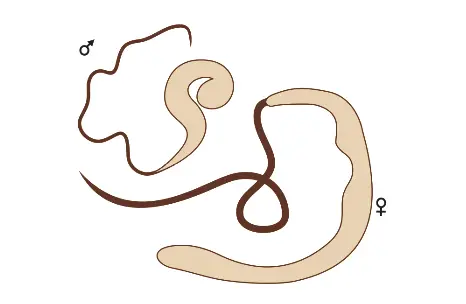
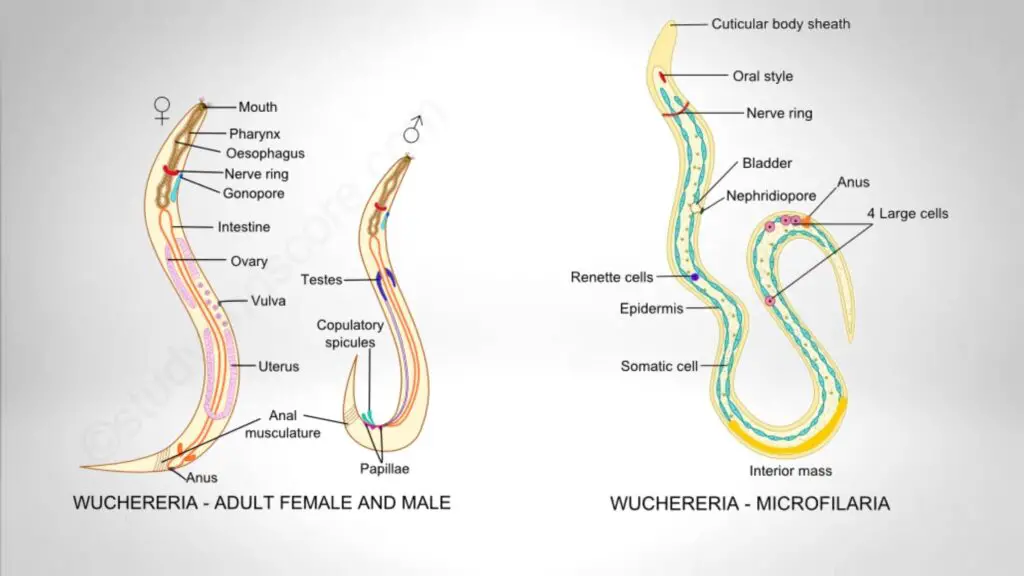
- Adult Worm Morphology
- Adult W. bancrofti worms are slender, whitish, and translucent, exhibiting a thread-like appearance.
- Size Differences: The female worm is notably larger than the male, measuring approximately 70 to 100 mm in length and 0.25 mm in diameter, compared to the male, which measures about 25 to 40 mm in length and 0.1 mm in diameter.
- End Morphology: The posterior end of the female worm is straight, while that of the male is curved vertically. The male’s posterior end also features two spicules of unequal length, which are important for mating.
- Location in Host: Adult worms typically reside in the lymphatic vessels and lymph nodes of the abdominal and inguinal regions. They may also be found in testicular tissues, often coiling together, which can obstruct lymphatic flow and contribute to the clinical manifestations of lymphatic filariasis.
- Reproductive Characteristics: The female is viviparous, meaning it directly releases sheathed microfilariae into the lymphatic system, from where they can enter the bloodstream. Adult worms can live for many years, potentially up to 10 to 15 years or longer within the host.
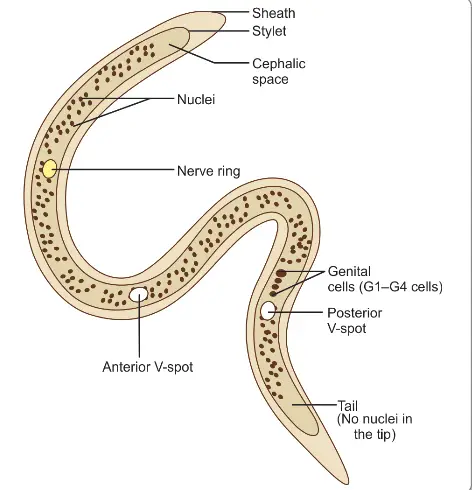
- Microfilariae Morphology
- The microfilariae are characterized by a colorless, translucent body, featuring a blunt head and a pointed tail. They measure approximately 250 to 300 μm in length and 6 to 10 μm in thickness.
- Sheath and Movement: Each microfilaria is enclosed within a hyaline sheath, which is longer than the embryo itself, allowing the microfilariae to move actively forwards and backwards within it.
- Structural Features:
- Cephalic Space: At the head end, there is a clear space devoid of granules known as the cephalic space. In W. bancrofti, this space is as long as it is wide, which can help distinguish it from other species such as Microfilaria malayi, where the cephalic space is longer than its breadth.
- Nerve Ring: Located in the anterior half, this oblique area is devoid of granules, indicative of the microfilaria’s nervous system.
- V-spots:
- The anterior V-spot marks the location of a rudimentary excretory system.
- The posterior V-spot serves as the cloaca or anal pore, while the genital cells are positioned anteriorly to this point.
- Internal Body Structures: The internal body of Manson extends from the anterior V-spot to the first genital cell, representing the rudimentary alimentary system.
- Tail Tip: In W. bancrofti, the tail tip lacks nuclei, serving as a distinguishing characteristic from Microfilaria malayi, which has two distinct nuclei at the tail tip.
- Lifespan and Periodicity
- Microfilariae do not multiply or develop further within the human body; if they are not ingested by a female mosquito, they typically die within 2 to 3 months. For effective transmission, a microfilarial density of at least 15 per drop of blood is necessary.
- Nocturnal Periodicity: In regions such as India and China, microfilariae exhibit nocturnal periodicity, meaning they circulate in the blood predominantly at night (between 10 PM and 4 AM). This pattern aligns with the nocturnal feeding habits of their mosquito vectors.
- Adaptability of Periodicity: The periodicity of microfilariae can adapt based on the sleeping patterns of their human hosts. Reports indicate that if host sleeping habits change over time, the microfilariae can shift their periodicity from nocturnal to diurnal.
- Variations in Other Regions: In the Pacific Islands and certain areas of the Malaysian archipelago, microfilariae may be non-periodic or diurnally sub-periodic, appearing in the bloodstream at all times with slight peaks in the late afternoon or evening, correlating with the local mosquitoes’ biting habits.
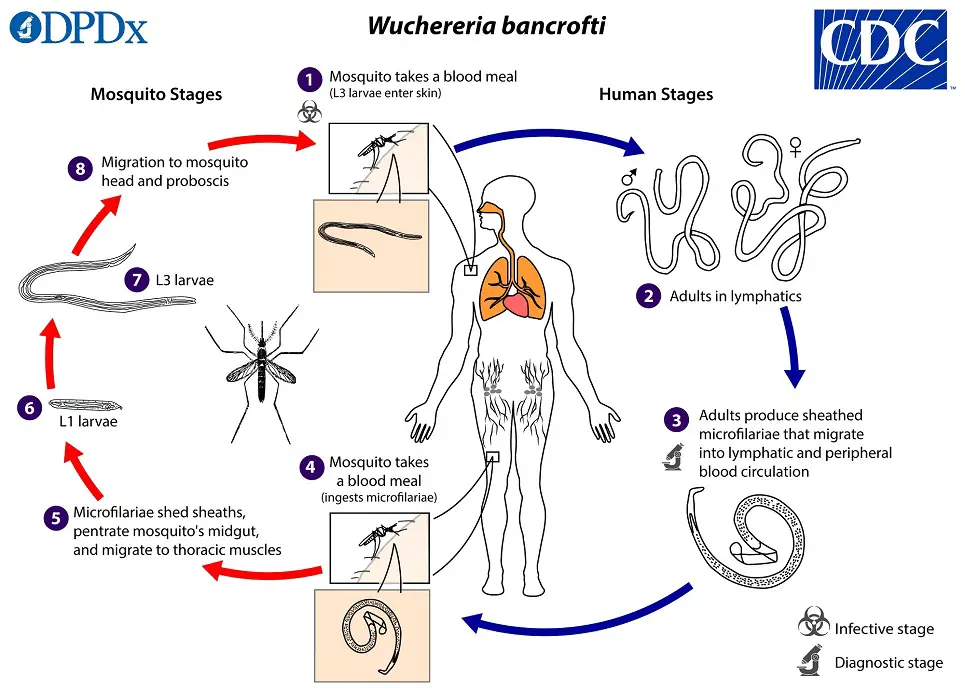
The life cycle of Wuchereria bancrofti
The life cycle of Wuchereria bancrofti, a parasitic roundworm responsible for lymphatic filariasis, involves two distinct hosts: humans, the definitive host, and female mosquitoes, the intermediate hosts. This complex cycle enables the parasite to thrive and perpetuate its transmission within affected populations. Understanding the stages of this life cycle is essential for recognizing how the disease spreads and for developing effective control measures.
- Hosts Involved
- Definitive Host: The primary host for W. bancrofti is humans. There are no known animal reservoirs for this parasite.
- Intermediate Host: Female mosquitoes of various species serve as the vectors for transmission, with Culex quinquefasciatus being the primary vector in India and much of Asia.
- Infective Form
- The actively motile third-stage filariform larva is the infective stage for humans.
- Transmission Process
- Humans acquire the infection through the bite of a mosquito that carries the filariform larvae.
- Development in Mosquito
- Intake of Microfilariae: When a vector mosquito feeds on an infected individual, it ingests microfilariae along with the blood meal.
- Exsheathing: Within 2 to 6 hours after ingestion, the microfilariae shed their sheaths and penetrate the stomach wall of the mosquito.
- Migration: The larvae then migrate to the thoracic muscles, undergoing further development over the next 4 to 17 hours.
- First-Stage Larva: After approximately 2 days, the larvae metamorphose into the first-stage larva, which is sausage-shaped and has a spiky tail, measuring between 125 to 250 μm by 10 to 15 μm.
- Second-Stage Larva: Within a week, the first-stage larva molts one or two times, growing larger to become the second-stage larva, measuring 225 to 325 μm by 15 to 30 μm.
- Third-Stage Filariform Larva: In another week, the larvae develop internal structures, becoming the elongated third-stage filariform larva, measuring 1,500 to 2,000 μm by 15 to 25 μm. This is the actively motile and infective form.
- Location in Mosquito: The infective larvae enter the proboscis sheath of the mosquito, where they remain until the mosquito feeds again.
- Extrinsic Incubation Period: The period from the ingestion of microfilariae to the development of the infective larvae in the proboscis sheath constitutes the extrinsic incubation period, which varies based on environmental conditions, such as temperature and humidity, and typically lasts between 10 to 20 days.
- Development in Humans
- Entry through Skin: When a mosquito with infective larvae feeds on a human, the larvae are deposited near the puncture site. They can enter through the puncture wound or directly penetrate the skin.
- Infective Dose: The exact number of larvae required for successful transmission is not well-defined, but it is estimated that a large number of infected mosquito bites—potentially around 15,000—are needed to ensure transmission to a human host.
- Migration to Lymphatic System: After penetrating the skin, the third-stage larvae enter the lymphatic vessels, typically moving to abdominal or inguinal lymph nodes, where they develop into adult forms.
- Development into Adults: Each larva develops into one adult worm (either male or female) without multiplication occurring at this stage. The adults take about six months to mature sexually.
- Reproduction: Gravid females release a significant number of microfilariae—up to 50,000 daily—which enter the bloodstream through the thoracic duct and pulmonary capillaries.
- Cycle Continuation: The microfilariae in circulation are then available to be ingested by another feeding mosquito, thus continuing the life cycle.
- Prepatent Period
- The period from the entry of the infective larvae into the human host until the first appearance of microfilariae in the bloodstream is known as the biological incubation period or prepatent period. This period generally lasts about 8 to 12 months.
- Clinical Incubation Period
- The clinical incubation period is defined as the time from the entry of infective larvae to the manifestation of clinical symptoms, which can vary widely but typically lasts between 8 to 16 months, although it may be longer in some cases.
Pathogenesis of Wuchereria bancrofti

The pathogenesis of Wuchereria bancrofti, the causative agent of bancroftian filariasis, illustrates a complex interplay between the parasite and the host’s immune response, leading to a range of clinical manifestations. This disease presents primarily in two forms: classical filariasis and occult filariasis. Understanding the underlying mechanisms that contribute to the pathogenesis of W. bancrofti is crucial for developing effective treatments and control strategies.
- Classical Filariasis
- Pathogenesis Mechanisms:
- Lymphatic Obstruction: The adult worms reside in the lymphatic vessels and lymph nodes, causing blockage either through mechanical obstruction or allergic inflammatory reactions to worm antigens and secretions.
- Immune Response: The affected lymph nodes and vessels become infiltrated with immune cells, including macrophages, eosinophils, lymphocytes, and plasma cells. This cellular infiltration is a response to the presence of the parasite.
- Vascular Changes: The inflammation leads to thickening of vessel walls and narrowing of lumens, resulting in lymph stasis and dilation of lymph vessels. This is compounded by the formation of granulomas around the worms, leading to scarring and, in some cases, calcification.
- Lymphatic Valve Damage: Inflammatory changes can also damage the valves in lymphatic vessels, worsening the stasis and leading to further complications.
- Fluid Leakage: Increased permeability of lymphatic vessel walls results in the leakage of protein-rich lymph into surrounding tissues, creating the characteristic hard pitting or brawny edema associated with the disease.
- Fibrosis Development: As fibroblasts invade the edematous tissues, fibrous tissue is laid down, contributing to non-pitting gross edema and eventually leading to elephantiasis.
- Recurrent Infections: Repeated acute bacterial infections complicate the clinical picture, exacerbating tissue damage and promoting chronicity.
- Pathogenesis Mechanisms:
- Clinical Manifestations:
- The spectrum of symptoms in classical filariasis includes:
- Asymptomatic Microfilaremia: Many infected individuals may remain asymptomatic yet harbor microfilariae in their blood.
- Acute Adenolymphangitis (ADL): Characterized by sudden high fever, inflammation of lymphatic vessels (lymphangitis), and local edema. The fever often lasts for 2 to 3 days, with red streaks visible under the skin indicating inflamed lymph vessels.
- Lymphadenitis: Inflammation and enlargement of lymph nodes, predominantly affecting inguinal and axillary regions.
- Lymphedema: Following recurrent episodes of lymphangitis, swelling begins around the ankles and can progress up the leg, eventually becoming hard and non-pitting over time.
- Hydrocele: A common manifestation due to obstruction of lymph vessels in the spermatic cord, leading to fluid accumulation that can be substantial.
- Lymphorrhagia: Rupture of lymphatic varices may lead to the release of lymph into surrounding tissues, resulting in conditions such as chyluria, chylous diarrhea, and chylothorax.
- Elephantiasis: A severe and delayed consequence of repeated lymphatic obstruction and edema, resulting in thickened skin, new tissue growth, and increased susceptibility to secondary infections.
- The spectrum of symptoms in classical filariasis includes:
- Occult Filariasis
- Pathogenesis Characteristics:
- Occult filariasis occurs primarily due to hypersensitivity reactions to microfilarial antigens, rather than direct lymphatic involvement.
- In this form, microfilariae are typically absent from the bloodstream due to destruction by host tissues.
- Clinical Manifestations:
- Massive Eosinophilia: Eosinophil counts can range from 30% to 80%, indicating a strong immune response.
- Hepatosplenomegaly: Enlargement of the liver and spleen is commonly observed.
- Pulmonary Symptoms: These can include dry nocturnal cough, dyspnea, and asthmatic wheezing.
- Additional Symptoms: Other reported manifestations include arthritis, glomerulonephritis, and thrombophlebitis.
- Meyers Kouwenaar Syndrome: This term is synonymous with occult filariasis, highlighting its unique characteristics compared to classical filariasis.
- Tropical Pulmonary Eosinophilia: A specific manifestation of occult filariasis often seen in endemic areas, featuring low-grade fever, pulmonary symptoms, and significantly elevated eosinophil counts.
- Pathogenesis Characteristics:
Laboratory Diagnosis of Wuchereria bancrofti
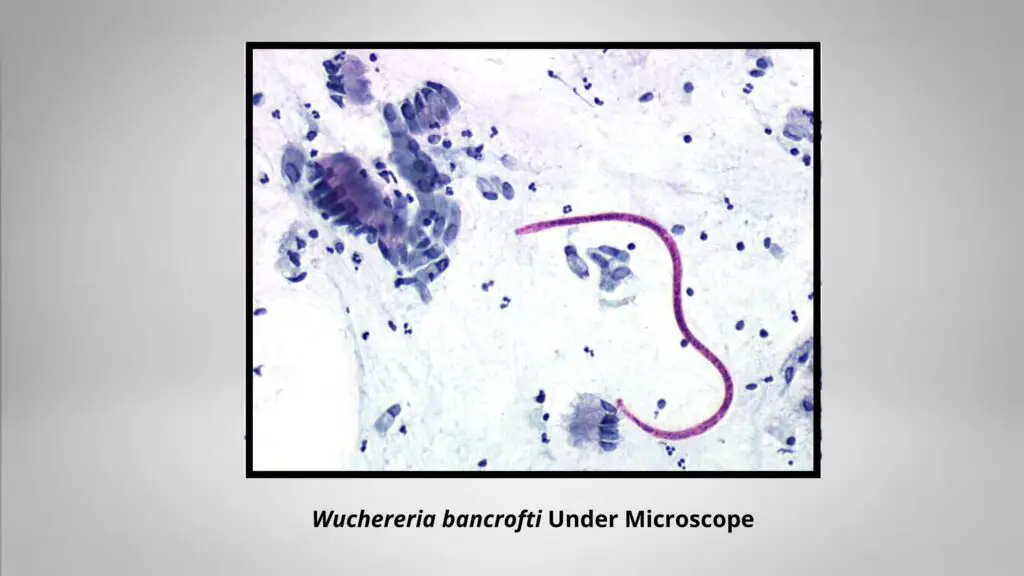
The laboratory diagnosis of Wuchereria bancrofti infection involves multiple diagnostic approaches, including microscopy, serological assays, and molecular techniques. These methods are essential for confirming the presence of the parasite in patients, especially those from endemic regions. Diagnosis hinges on the detection of microfilariae or the identification of antigens or antibodies associated with the parasite.
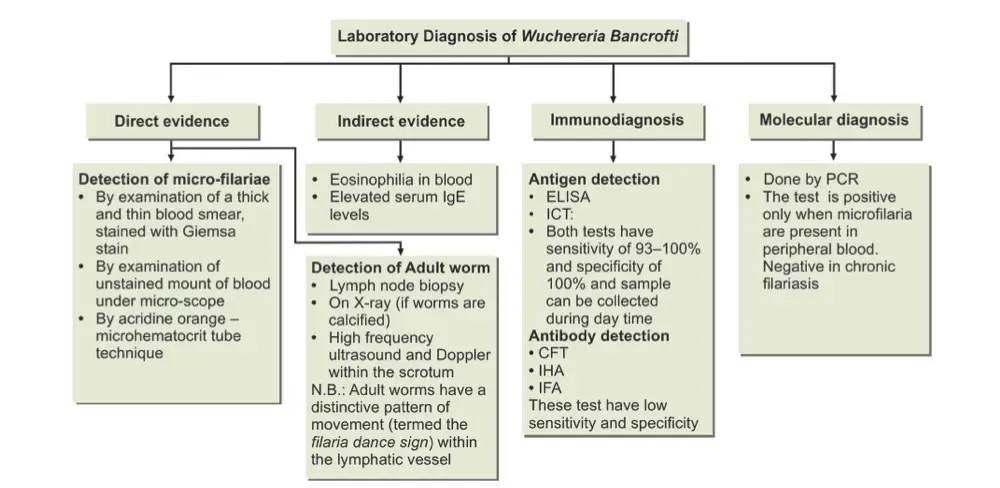
- Demonstration of Microfilariae:
- Specimen Collection: Peripheral blood is the main specimen for detecting microfilariae, although chylous urine, lymphatic exudates, and hydrocele fluid can also contain the parasite. In regions where nocturnally periodic W. bancrofti species are common, blood samples must be collected between 10 PM and 4 AM to capture peak microfilarial activity.
- Unstained and Stained Preparations:
- Unstained Films: These preparations allow visualization of motile microfilariae under a low-power microscope, interacting with red blood cells.
- Stained Films: A “thick and thin” smear is used, with the thick smear being dehemoglobinized and stained using Giemsa, Leishman, or polychrome methylene blue. The microfilariae are identified by their sheathed appearance, smooth body, and measurements of approximately 298 µm in length and 7.5-10 µm in diameter.
- Microfilaria Counts: A known volume of blood (typically 20-60 µm³) is taken with a micropipette, and the total number of microfilariae in the smear is counted.
- Concentration Techniques:
- Knott’s Concentration Technique: In this method, 1 mL of anticoagulated blood is mixed with 9 mL of 2% formalin, centrifuged, and the sediment is stained and examined microscopically for microfilariae.
- Nucleopore Filtration: Larger blood volumes (up to 5 mL) are passed through millipore or nucleopore filters (3 µm pore size). The membranes are examined for microfilariae, offering high sensitivity. This method can be done during the day, though it is more expensive and requires venipuncture.
- DEC Provocation Test: Diethylcarbamazine (DEC) can be administered to provoke the appearance of microfilariae in peripheral blood, allowing for sample collection shortly afterward.
- Other Specimens: Microfilariae may also be found in the centrifuged deposits of lymph, hydrocele fluid, or early morning urine. Typically, 10-20 mL of first morning urine is collected for examination.
- Biopsy:
- Although rarely used for diagnosis, adult worms may occasionally be observed in lymph node biopsies, providing a direct identification of the parasite.
- Skin Testing:
- An intradermal skin test using filarial antigens may trigger a hypersensitivity reaction. However, this test is not commonly employed due to its limited diagnostic value, with frequent false positives and negatives.
- Imaging Techniques:
- Ultrasonography: High-frequency ultrasonography with Doppler imaging can detect motile adult worms in the lymphatic vessels, often showing the “filaria dance sign.” This is especially useful for visualizing worms in the spermatic cord of infected males.
- Radiology: Occasionally, dead or calcified worms may be visible on X-rays. Additional imaging techniques, such as intravenous urography, retrograde pyelography, and lymphoscintigraphy, can reveal lymphatic system abnormalities.
- Serodiagnosis:
- Antibody Detection: Serological tests like indirect immunofluorescence assay (IFA) and immunodiffusion have been developed but lack the sensitivity and specificity required for routine diagnostic use.
- Detection of Circulating Antigen: Highly sensitive tests detect circulating filarial antigens (CFA) in recent infections. The TropBio test, a semi-quantitative sandwich ELISA, and the immunochromatographic filariasis card test (ICT) offer sensitivities of 93-100% and near-perfect specificity. Additionally, enzyme-linked immunosorbent assays (ELISA) are used to detect specific IgG4 antibodies against W. bancrofti antigens.
- Molecular Diagnostic Techniques:
- Polymerase chain reaction (PCR) can identify W. bancrofti DNA in blood samples, even when microfilariae are absent. PCR offers up to ten times greater sensitivity than conventional methods and maintains high specificity, making it a powerful tool for diagnosis.
- Indirect Evidence:
- Eosinophilia (an elevated number of eosinophils) is commonly seen in filarial infections, often ranging from 5-15%. Additionally, increased levels of serum IgE may be present, serving as indirect markers of infection.
Treatment of Wuchereria bancrofti
- Diethylcarbamazine (DEC): This medication is considered the cornerstone of treatment for lymphatic filariasis caused by Wuchereria bancrofti. It has both macrofilaricidal (affecting adult worms) and microfilaricidal (affecting microfilariae) properties. The recommended dosage is 6 mg/kg body weight administered orally for 12 consecutive days, culminating in a total of 72 mg of DEC per kg.
- Potential Reactions: Following DEC administration, patients may experience the Mazzotti reaction, which is a severe allergic response due to the rapid death of microfilariae. Symptoms can include fever, rash, and lymphadenopathy, necessitating careful monitoring post-treatment.
- Administration Strategies for DEC: The treatment approach to DEC can be categorized into three distinct strategies:
- Mass Therapy: This strategy involves the administration of DEC to nearly all individuals in a community, regardless of their infection status. Exemptions apply to children under two years old, pregnant women, and severely ill patients. In highly endemic regions, mass treatment helps to significantly reduce the prevalence of lymphatic filariasis. In some countries, DEC is given alone, while in others, it may be combined with albendazole or ivermectin to enhance efficacy.
- Selective Treatment: Under this approach, DEC is specifically administered to individuals who have tested positive for microfilariae. In India, this strategy is prevalent, focusing on identifying and treating human carriers of the parasite. The regimen typically mirrors that of mass therapy, with the same dosage and duration. This treatment should be repeated every two years in endemic areas to maintain control over transmission.
- DEC Medicated Salts: In certain regions, such as Lakshadweep Island, common salt has been fortified with 1–4 g of DEC per kg to facilitate control of filariasis. This method follows an initial reduction in prevalence through either mass or selective treatment and serves as a long-term preventive strategy.
- Ivermectin: Although Ivermectin can effectively kill microfilariae at a dosage of 200 µg/kg, it does not affect adult Wuchereria bancrofti worms. Consequently, it is not commonly used in India but has found application in African regions, where it aids in managing co-infections with other filarial species.
- Tetracyclines: This class of antibiotics plays a role in the treatment of filariasis by targeting the endosymbiotic bacteria, Wolbachia species, which are vital for the fertility of the adult worms. By inhibiting these bacteria, tetracyclines can reduce the reproductive capacity of Wuchereria bancrofti, leading to a gradual reduction in the worm population.
- Supportive Treatment Options: For chronic conditions, particularly those that result in physical deformities such as elephantiasis, complete eradication of the infection may not be feasible. Therefore, supportive care becomes essential. Strategies include:
- Elevating Affected Limbs: This can help reduce swelling and discomfort associated with lymphedema.
- Elastic Bandaging: Applying elastic bandages can aid in managing limb swelling and improving circulation.
- Local Foot Care: Maintaining hygiene and proper care of the affected areas can prevent secondary infections.
- Surgical Intervention: Procedures may be necessary for complications like hydrocele, where surgical correction can restore function and alleviate discomfort.
- Management of Chyluria: This condition can be addressed through bed rest, a high-protein diet while excluding fats, and continued use of DEC. In refractory cases, surgical options such as endoscopic sclerotherapy using silver nitrate may be employed.
Prophylaxis of Wuchereria bancrofti
- Eradication of the Vector Mosquito: The control of vector mosquitoes is critical in the prevention of Wuchereria bancrofti infections. The main strategies employed include:
- Antilarval Measures: Effective vector control requires the reduction or elimination of mosquito breeding sites. While ideal sanitation and wastewater disposal systems can significantly mitigate mosquito populations, these measures are often cost-prohibitive. Thus, current strategies in countries like India focus on urban areas and employ the following methods:
- Chemical Control: Various larvicides are utilized to target mosquito larvae before they can mature into adult mosquitoes. Commonly used chemicals include:
- Mosquito larvicidal oil: This type of oil targets mosquito larvae and reduces their ability to survive.
- Pyrosene oil: Known for its efficacy in larvicidal applications.
- Organophosphorous larvicides: Chemicals such as temephos and fenthion effectively disrupt the development of mosquito larvae.
- Removal of Aquatic Vegetation: The removal of Pistia, a water plant that provides habitat for specific mosquito species, particularly Mansonia mosquitoes, is essential in controlling the transmission of Brugian filariasis, a related condition caused by Brugia malayi.
- Chemical Control: Various larvicides are utilized to target mosquito larvae before they can mature into adult mosquitoes. Commonly used chemicals include:
- Antiadult Measures: To reduce adult mosquito populations, various insecticides have historically been used:
- DDT and Dieldrin: Although effective, these chemicals have seen a decline in efficacy due to widespread resistance among mosquito populations.
- Pyrethrum: Despite resistance concerns, pyrethrum is still effective as a space spray to target adult mosquitoes.
- Personal Prophylaxis: In addition to community-wide vector control measures, individual protective strategies are crucial. These include:
- Use of Mosquito Nets: Insecticide-treated nets provide a barrier against mosquito bites during the night, significantly reducing transmission risk.
- Application of Mosquito Repellents: Repellents containing DEET or other effective ingredients help protect individuals from mosquito bites when outside.
- Antilarval Measures: Effective vector control requires the reduction or elimination of mosquito breeding sites. While ideal sanitation and wastewater disposal systems can significantly mitigate mosquito populations, these measures are often cost-prohibitive. Thus, current strategies in countries like India focus on urban areas and employ the following methods:
- Detection and Treatment of Carriers: Identifying and treating individuals who harbor Wuchereria bancrofti is another pivotal aspect of prophylaxis. The recommended treatment involves:
- Diethylcarbamazine (DEC): The standard dosage is 6 mg/kg of body weight administered orally for 12 consecutive days. This regimen aims to reduce the microfilariae load in carriers, consequently decreasing the potential for further transmission.
- Screening Initiatives: Regular screening programs in endemic areas are essential for early detection of microfilaria-positive individuals, ensuring timely treatment and reducing the reservoir of infection within the community.
Factors Affecting the Transmission of Filarial Worm
The transmission of the filarial worm Wuchereria bancrofti, which causes lymphatic filariasis, is notably less efficient compared to other vector-borne diseases like malaria or dengue. This is due to various factors that limit its spread through mosquito vectors. Understanding these factors is crucial for developing effective control strategies.
- Number of ingested microfilariae:
- Unlike some parasites, microfilariae do not multiply within the mosquito’s body. Therefore, the quantity of larvae (L3 stage) that a mosquito can eventually transmit is determined by how many microfilariae it initially ingests. This inherent limitation restricts the potential transmission rate.
- Longevity of mosquito:
- The development of the filarial worm from microfilariae to the infective L3 stage takes approximately 12 to 14 days. Therefore, only mosquitoes that live longer than this—typically more than 15 to 20 days—can contribute to the transmission cycle. Mosquitoes that die prematurely are unable to transmit the filarial worm, thus reducing overall transmission potential.
- Release of microfilariae:
- Upon biting a human host, mosquitoes do not directly inject L3 larvae into the bloodstream. Instead, the larvae are deposited on the skin near the puncture wound. They must then find their way into the bite wound to enter the human body. This indirect mode of entry adds an additional barrier, reducing the efficiency of transmission.
- Biting rate of the mosquito:
- The rate at which mosquitoes bite humans directly impacts the transmission of microfilariae. A higher biting rate increases the likelihood of a mosquito ingesting microfilariae from an infected host, which in turn raises the probability of subsequent transmission to other humans.
- Prevalence of disease:
- The spread of filarial disease in a population depends on how many individuals are carrying a significant density of circulating microfilariae in their peripheral blood. The more infected individuals there are in a community, the greater the chances of mosquitoes acquiring and spreading the parasite.
- Impact on mosquitoes:
- High numbers of microfilariae in the blood meal can be harmful to the mosquito. As the microfilariae develop inside the mosquito, they may damage the mosquito’s gut and thoracic muscles. The emergence of L3 larvae from the flight muscles can cause severe physical damage, impairing the mosquito’s ability to fly and potentially leading to its death. This reduces the number of mosquitoes capable of transmitting the filarial worm.
- Environmental conditions:
- Transmission of filarial worms is also heavily influenced by environmental factors such as rainfall, temperature, humidity, and soil type. These conditions affect the breeding sites of mosquitoes and their overall survival. Favorable environmental conditions promote mosquito longevity and increase the potential for transmission, while unfavorable conditions can disrupt the life cycle of both the mosquito and the parasite.
Key points of Wuchereria bancrofti
- Morphological Characteristics:
- The adult Wuchereria bancrofti is a white, thread-like nematode with a smooth cuticle and tapering ends.
- Female worms are viviparous, producing live offspring known as microfilariae. These microfilariae are colorless, sheathed, and exhibit a distinctive morphology with a tail-tip free of nuclei. Additionally, they are motile, allowing for movement through the bloodstream.
- Life Cycle and Hosts:
- The definitive host for Wuchereria bancrofti is humans, where the adult worms reside in the lymphatic system.
- The intermediate host is the mosquito, primarily Culex quinquefasciatus (also known as C. fatigans).
- Microfilariae do not multiply in humans; instead, when ingested by a vector mosquito during a blood meal, they undergo several developmental stages. Within the mosquito, they develop into the third-stage (filariform) larvae, which are the infective form capable of transmission to humans.
- Microfilarial Periodicity:
- The microfilariae display nocturnal periodicity, meaning they are predominantly found in the peripheral blood between 10 PM and 4 AM. This pattern assists in diagnosis as blood samples collected during these hours are more likely to contain microfilariae.
- Pathogenesis:
- The adult worms induce lymphatic obstruction, leading to mechanical blockages in the lymphatic system. This blockage can trigger various allergic manifestations in the host.
- Clinical Features:
- In the early stage of infection, individuals may experience fever, malaise, urticaria (hives), and fugitive swelling.
- As the disease progresses to the chronic stage, symptoms can become more severe, including lymphadenitis (inflammation of lymph nodes), lymphangiovarix (enlargement of lymph vessels), chyluria (presence of lymphatic fluid in urine), hydrocele (swelling of the scrotum), and elephantiasis (severe swelling of the limbs or genitals).
- Another notable complication is tropical pulmonary eosinophilia, which occurs as a hypersensitivity reaction to filarial antigens.
- Diagnosis:
- Diagnosis of Wuchereria bancrofti infection typically involves demonstrating the presence of microfilariae in peripheral blood or chylous urine.
- Other diagnostic methods include identifying adult worms through biopsy, employing imaging techniques such as Doppler ultrasound and X-rays, and using serological tests to detect filarial antigens and antibodies.
- Treatment Options:
- The drug of choice for treating Wuchereria bancrofti infections is Diethylcarbamazine (DEC), which targets both adult worms and microfilariae.
- Ivermectin is also used in some cases, particularly in regions where it is indicated for co-infections.
- Supportive treatment may be necessary for managing chronic complications, and surgical intervention might be required in cases like hydrocele or severe lymphedema.
- Paniker’s Textbook of Medical Parasitology
- https://www.cdc.gov/parasites/lymphaticfilariasis/gen_info/index.html
- https://animaldiversity.org/accounts/Wuchereria_bancrofti/
- https://www.cdc.gov/dpdx/lymphaticfilariasis/index.html
- https://en.wikipedia.org/wiki/Wuchereria_bancrofti
- https://www.cdc.gov/dpdx/lymphaticfilariasis/index.html
- http://www.antimicrobe.org/new/b141.asp
- https://www.msdsonline.com/resources/sds-resources/free-safety-data-sheet-index/wuchereria-bancrofti/
- https://thebiologynotes.com/wuchereria-bancrofti-habitat-morphology-and-life-cycle/
- https://www.onlinebiologynotes.com/wuchereria-bancrofti-morphology-life-cycle-and-epidemiology/