Viral Spread
- After replication at the point of entry, the virus particles may remain in situ or expand to different tissues.
- The local spread of the infection within the epithelium happens when the virus is released and infects adjacent cells. The infections are typically controlled by the physical limitations of the tissue, and are managed by the inherent immune and innate defenses.
- A condition that extends beyond the original location of infection is known as disseminated.
- If multiple organs are infected the condition is referred to as systemic.
- To allow an infection to spread beyond its primary site, the physical as well as immune barrier must be broken.
- After crossing the epithelium virus particles travel to through the basement membrane. The integrity of this structure can be compromised by epithelial cell death and inflammation.
- Under the basement membrane lie sub-epithelial tissues. These are where the virus interacts with the lymphatic system, as well as the phagocytes. They all play a significant role in the elimination of foreign particles however they can also disseminate the virus from the location of infection.
- One of the most effective ways to avoid local host defenses and encouraging spreading throughout an organism is dispersal of viral particles by mucosal cells that are polarized at the surface.
- Virion can be released from the apical layer or from the basolateral surface or both.
- After replication, the virus is released by the apical surfaces is released outside the host. This directional release aids in the dispersal of a variety of newly replicated enteric viruses into the stool (e.g. Poliovirus, for instance).
- Contrary to this, virus particles that have been released from the basolateral surfaces of epithelial cells have been pushed away from the protective layers that protect the interior of the lumenal surfaces. This is an important factor in determining the nature of the infection.
- In general, viruses that are released in apical membranes create a isolated or restricted infection.
- The release of viruses in the basal membrane allows access to tissues underneath and can facilitate the spread of viruses throughout the body.
Hematogenous Spread
- Viruses that break out of local defenses and cause a disseminated infection typically enter into the circulation of blood (hematogenous spreading).
- The virus particles can get into the bloodstream through capillaries. They can do this by replicating in endothelial cells or by inoculation via the bite of a vector.
- When they are in bloodstream, viruses can infiltrate virtually every cell within the body of the patient.
- Hematogenous spread occurs with the creation of new replicated particles at the entry point are released into extracellular fluids. These fluids may be absorbed by the lymphatic system in the local system.
- Lymphatic capillaries are significantly better permeable than circulatory capillaries, making it easier for viruses to enter. When lymphatic vessels connect together with the system of venous viruses in lymph are free to access the bloodstream.
- The lymphatic system the lymph nodes are where virions travel and then meet lymphocytes of the immune system.
- The pathogenesis of viral infections arising directly from infected cell types of the immune system (e.g. measles virus, human immunodeficiency virus) can be initiated in this manner.
- Certain viruses multiply in lymphoid cells that are infected, and the progenitors are released into blood plasma.
- The lymphoid cells infected by the infection can also be able to migrate from the lymph node local into distant parts of the circulatory system.
- The term”viremia” refers to the presence of virus particles that are infectious in the blood.
- These virions can be found in blood or within cells that are infected, such as lymphocytes. Active viremia results from the replication of viruses, while passive viremia occurs after virus particles have been introduced into bloodstream without viral replication at the point where they enter (injection of an infection suspension of virus into the vein).
- Progeny viruses released into blood following first replication on the point of entry form primary viremia.
- The quantity of virus particles in primary viremia is typically minimal. However, the disseminated infection that results is usually extensive, and release significantly greater amounts of viruses.
- The delay in the appearance of a higher level of infectious virus in blood is known as secondary viremia.
- The two stages of viremia were first identified in the classic mousepox studies. Viemias can be used to diagnose and are able to observe the progression of an infection. However, they also pose practical challenges.
- Infections are often spread accidentally throughout the population when blood pooled from thousands of people is used for direct reasons of therapeutic use (transfusions) or for the purpose of generating protein therapeutics (e.g. Gamma globulin, gamma globulin as well as blood-clotting proteins).
Neural Spread
- Many viruses are spread from the site of infection via the local nerve endotheles.
- For specific viruses (e.g. the rabies viruses and the alpha herpesviruses) neuronal spread is the primary aspect of their cause of action.
- Other viruses (e.g. the poliovirus, poliovirus and Reovirus) invading nervous systems is not as frequent a divergence from their place of replication as well as their final destination.
- Certain viruses (e.g. the mumps virus, the human immunodeficiency and measles virus) can be able to replicate in the brain but they are spread through the hematogenous pathway. Since protein synthesis does not occur in the processes that extend neurons, viruses need to be carried over large distances to reach the site of replication.
- There is evidence that shows that viruses are transported into the affected neuron via cells, however viral proteins could aid in the path of spread.
- A neurotropic virus may cause neural cell damage; the infection can occur through the spread of hematogenous or neural viruses that begins from a peripheral location.
- A neuroinvasive virus may enter Central Nervous System (spinal cord or brain) by infecting an external area.
- A neurovirulent virus may cause neuronal tissue damage which manifests itself as neurological symptoms , and sometimes death.
Examples:
- Herpes simplex virus is very low neuroinvasiveness in the central nervous system however, it has high neurovirulence. It will always infiltrate into the peripheral nervous system, but seldom enters into the Central Nervous System. If it does, results are often serious, if they are not fatal.
- The Mumps virus is highly neuroinvasive however it has low neurovirulence. The majority of infections result in inflammation into the nervous system central however, neurological diseases are mild.
- The Rabies virus exhibits high neuroinvasiveness as well as high levels of neurovirulence. It rapidly affects nerves in the peripheral system, and expands to the central nerve system. It is 100% lethal in the absence of antiviral therapy within a short time after the infected.
Organ Invasion of Virus
- After virions have entered the bloodstream and disperse away from the source the next replication is dependent on the invasion of new cells and tissues.
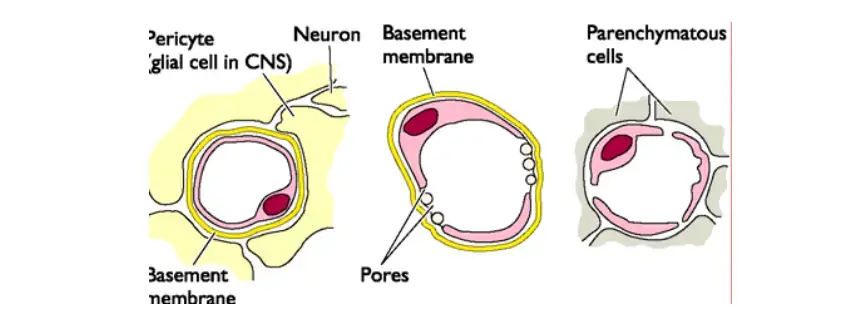
- Three major kinds of blood-tissue junctions offer pathways for tissue invasion such as; capillary, venule, and sinusoid.
- In some viral infections that are systemic the rashes develop when the virions are released from blood vessels. Different kinds of skin lesions develop.
- Papules and macules appear when inflammation is present in the dermis. the infection being contained in or close to the blood vessel bed.
- The formation of pustules and the appearance of vesicles occurs as viruses travel from capillaries to the surface layer of skin.
- The destruction of cells caused by viral replication can be the most common reason for lesions.
The Liver, Spleen, Bone Marrow, and Adrenal Glands
- These tissues are distinguished through the existence of sinusoids lining them with macrophages.
- These macrophages, also known as the reticuloendothelial system function to cleanse blood and to remove foreign particles.
- They usually provide a means for entry into different tissues. For instance viruses that affect the liver are usually absorbed through the blood.
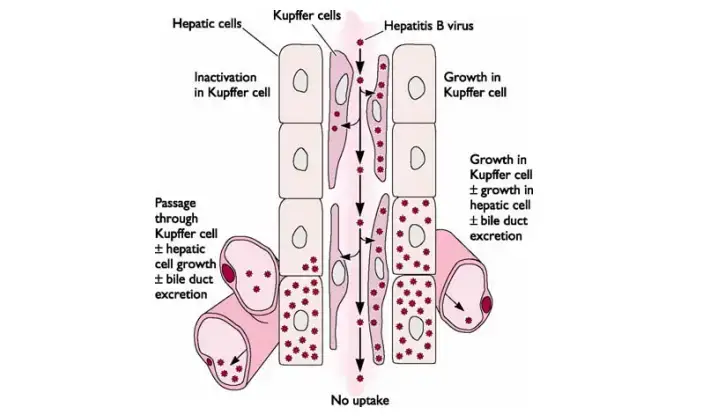
- In the presence of viruses in blood is always a trigger for the infecting that causes the development of Kupffer cells, which are macrophages that line the sinusoids of the liver.
- The virus can be transcytosed between Kupffer and endothelial cell lines without replication in order to reach the liver cells.
- In addition, viruses can grow within Kupffer and endothelial cells , and eventually infect liver cells that surround them. The combination of both causes can trigger inflammation and necrosis of the liver tissue, which is known as Hepatitis.
Central Nervous System, Connective Tissue, and Skeletal and Cardiac Muscle
- Within these tissue types, the capillary endothelial cells are usually not infected and are protected by a thick basement membrane.
- A great deal of study has been given to studying how viruses enter the brain through blood.
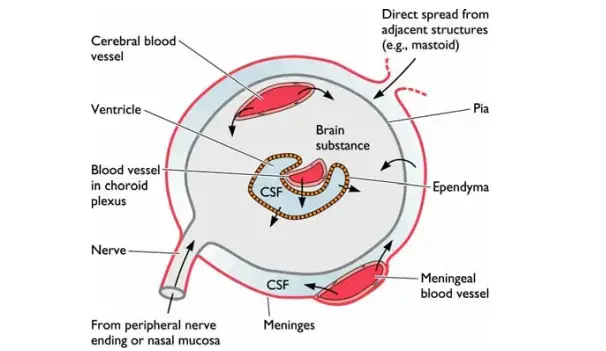
- In a variety of well-defined areas of the brain the capillary epithelium has been infenestrated, while the basement membrane appears thin. The most vascularized areas include the choroid and plexus.
- Certain viruses (e.g. Mumps virus, and certain types of togaviruses) traverse the capillary epithelium, and then enter the choroid plexus’ stroma and then enter the epithelium to the cerebrospinal fluid via transcytosis or replication, and controlled release. Once they’re in the cerebrospinal liquid the viruses infect ventricles’ ependymal cell layers and then invade the brain tissue.
- Other viruses can directly infect, or even be carried across the capillary epithelium (e.g. picornaviruses as well as togaviruses).
- Certain viruses can cross the endothelium inside the lymphocytes, monocytes, or both (e.g. measles virus and human immunodeficiency virus). A higher degree of permeability in the local capillary endothelium , caused by, for instance, certain hormones can allow virus entry into the spinal cord and brain.
The Renal Glomerulus, Pancreas, Ileum, and Colon
- In order to enter the tissues without sinusoids, viruses first attach to the endothelial cell lining capillaries or venules. These are the areas in the venules, where blood flow is at its lowest while the capillaries’ walls the thinnest.
- After blood-borne virus have been able to stick to the vessel’s wall, they may infiltrate quickly the renal glomerulus pancreas, the ileum, or colon, because the endothelial cells that form the capillaries have been Fenestrated (with “windows” between cells and loosely joined) that allow the virus, or the cells infected by virus to enter the surrounding tissues (e.g. for example, for example, poliovirus).
- Certain viruses (e.g. herpes simplex yellow fever, herpes simplex, and measles virus) traverse the endothelium being carried by lymphocytes or monocytes through a process known as diapedesis.
The Fetus
- For a female who is pregnant the viremia can lead to infections of the fetus in development.
- The basement membrane not as mature in the fetus. infection may result from an invasion of the placental tissues and later the fetal tissues. Infected cells in circulation, such as monocytes could get into the bloodstream of the fetus.
- The virus can also be passed to the newborn during birth or during breast-feeding.