Hey, in this article I will discuss the complement pathway which is one of the easiest pathways. Basically, This complement pathway helps to kill microorganisms by antibodies or phagocytosis.
The complement pathway has been accomplished in three main ways, which I have discussed step by step below. Believe me, if you understand the first step (the classical path) of the complementary path, you will not face any problem in the next two paths.
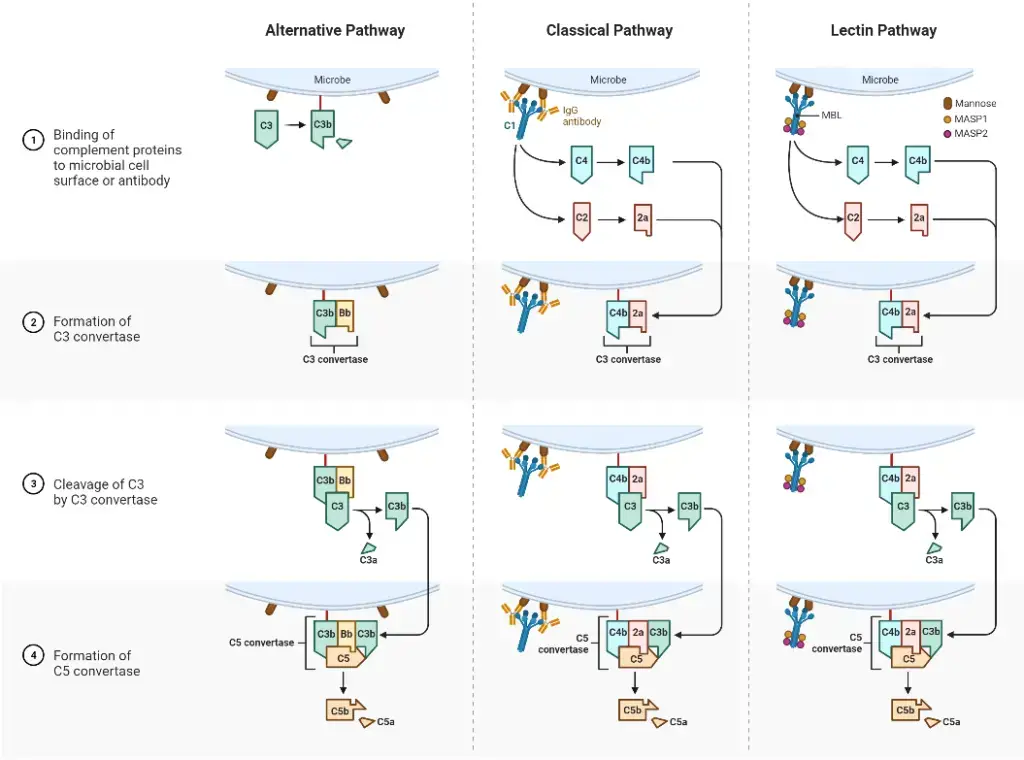
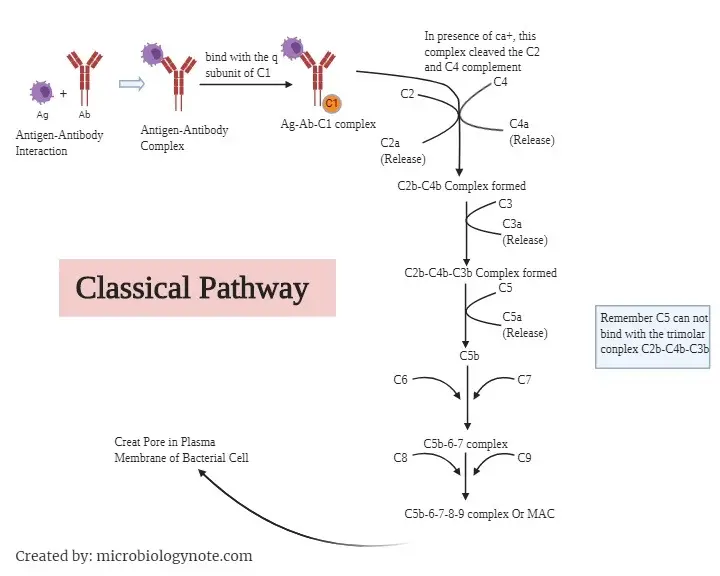
I have provided pictures where you can read each step of the complementary pathway by following them. Otherwise, it will go over your head.
What is the Complement Pathway?
The complement pathway is a complex process which helps in the elimination or inhibition of microbes by enhancing (complement) the killing ability of antibodies and phagocytic cells. The complement pathway is a part of the innate immune system.
The complement pathway is made up of over 30 heat-labile Complement proteins, which are found in human blood plasma. These proteins are synthesized by the liver, intestinal mucosa, spleen, and macrophages. After synthesis, they circulate in an inactive form in plasma and tissue fluids.
These 30 heat-labile proteins are, C1,C2,C3,C4,C5, C6, C7, C8, C9 in addition to factor B, factor D, factor H, factor I, and proteins, peptides.
After activation of these complement proteins, they inhibit the microbes by the lysis of cell membranes, phagocytosis, and inflammation. These complement proteins are enhanced phagocytosis, by opsonization.
Opsonization is a Greek term, where “opson” means “to prepare victims for”. Opsonization refers to, coats the microorganisms or inanimate particles with serum components, thereby preparing them for recognition and ingestion by phagocytic cells, which helps in the clearance of pathogens by phagocytic cells.
The complement pathway acts in a cascade fashion, which means the activation of one component in the complement pathway resulting in the activation of the next components.
The complement system was first observed in 1888 by George Nuttall in a sheep’s blood serum. He found that sheep blood serum had a killing activity against the causing agent of anthrax, but the killing activity of sheep’s blood serum disappeared when he heated the blood.
Later, in 1891, 1894 several laboratory experiments were conducted, which gave the same result. In 1899, Paul Ehrlich first renamed those heat-sensitive proteins as “complement.”
Activation of the Complement Pathway
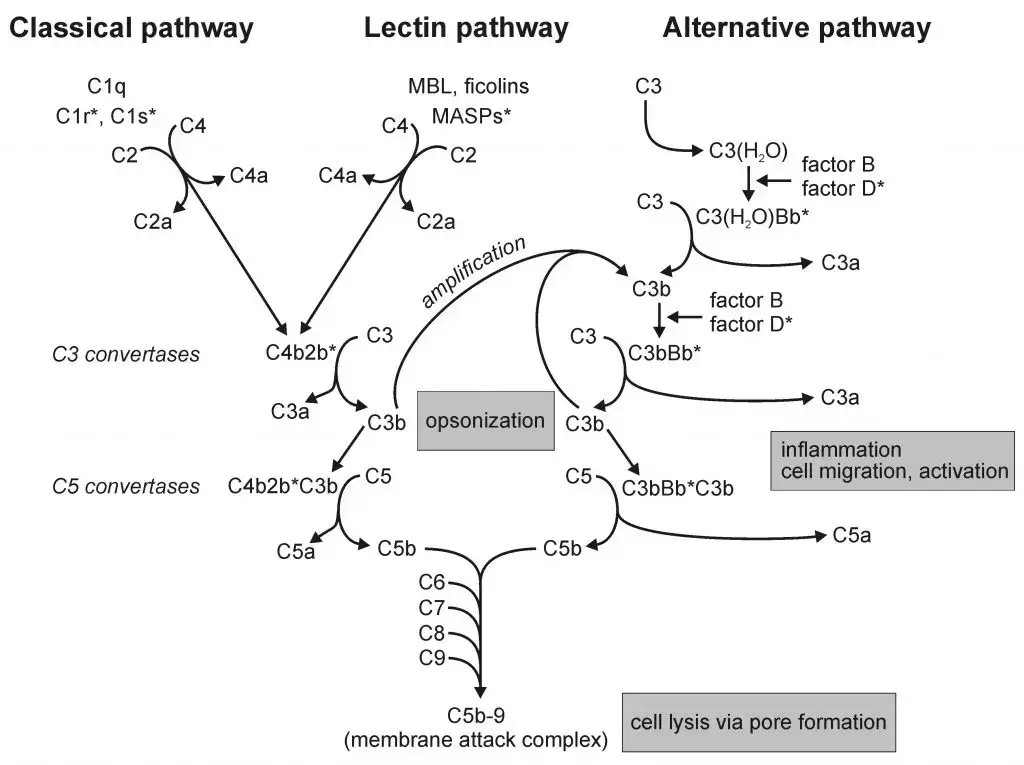
The activation of the complement pathway is accomplished by these three pathways;
- The Classical Pathway
- The Alternative Pathway
- The Mannose-Binding Lectin Pathways
1. The Classical Pathway
- Activation of classical pathways is initiated by the interaction between antibody and antigen interaction.
- Then it is also activated by some viral membranes, C reactive proteins, bacterial lipopolysaccharides, and trypsin like protease such as plasmin.
- After the formation of the antibody-antigen complex, they combine with the q-Subunit of C1 complement component, and form a complex called Antibody-antigen-C1 complex or C1-Ab-Ag. The C1 complement component consists of three subunits, such as C1q, C1r, and C1s. (These 3 subunits normally remain bonded with each other in plasma, by calcium-dependent bonds to form a loose trimolecular Complex called recognition unit or C1qrs).
- Normally C1 complement components bind with the Fc portion of IgM and IgG antibody molecules which is Already bonded with the surface antigens of the cell.
- In the presence of calcium ions, this trimolecular complex (C1-Ab-Ag) which already formed in the previous step will cleave C2 and C4 complement components into Large subunit (C2b and C4b) and small subunit (C2a and C4a) with the help of its convertase activity.
- As a result it will lead to the binding of the large portion (C2b and C4b) of C2 and C4 molecules and form a bimolecular complex called C2b-C4b, with the release of smaller molecules (C2a and C4a).
*Remember, C2,C4,C3, molecules consist of two subunits called large subunits, which is denoted by C2b,C4b, C3b and small subunits denoted by C2a, C3a, C4a.
- Newly formed this bimolecular complex C2b-C4b, has a trypsin-like proteolytic activity. Now this bimolecular complex Cleaved the C3 complement into larger C3b and smaller C3a compounds.
- C2b-C4b Complex combines with the C3b and forms a Trimolecular Complex called C3b-C2b-C4b complex, hence C2b-C4b complex cleaves the C3 therefore it is called C3-convertase.
- The complex C3b-C2b-C4b cleave the C5 complement into larger C5b and smaller C5a compounds, therefore C3b-C2b-C4b is called C5 convertase.
- C6 and C7 rapidly bind to C5b and form a trimolecular Complex called C5b-6-7.
- C5b-6-7 contains an unstable membrane binding site, once this complex is bound to a membrane it becomes stable.
- Then the C8 and C9 complement bind to C5b-6-7 Complex and form C5b-6-7-8-9 complex, which is called MAC or membrane attack complex.
- This MAC creates a pore in the plasma membrane of the target cell, which leads to cosmetic lysis of the cell.
2. The Alternative Pathways
- Initiation of the alternative pathway of complement activation is independent of antibody-antigen interactions.
- The alternative pathway seems to protect the body against microbes before immunoglobulin has been produced against them. After the serum Ig titre rises, this pathway is largely replaced by the classical pathway.
- The alternative pathway started with cleavage of C3 into smaller fragment c3a and larger fragments c3b by a blood enzyme.
- These fragments are produced at a slow rate and do not carry out the next step, however when c3b binds to lipopolysaccharide of bacterial outer membrane it becomes stable.
- A protein in blood termed factor B, is cleaved into two fragments such as one larger fragment or Bb and one smaller fragment called Ba, with the help of factor D.
- After that the large fragment (Bb) of factor B combines with the large fragment (C3b) of C3 and forms a complex called C3b-Bb.
- Then the C3b-Bb complex again Cleaved the C3 complement into larger c3b and smaller c3a components .
- After that the complex C3b-Bb binds with the C3b, and forms a trimolar complex C3b-Bb-3b. Hence, C3b-Bb complex cleaved the C3, therefore it is called C3-convertase.
- The trimolar complex C3b-Bb-3b, cleaves the C5 into larger C5b and Smaller C5a components, therefore C3b-Bb-3b complex is called C5-convertase.
- C6 and C7 rapidly bind to C5b, and form a trimolar complex C5b-6-7 that possesses an unstable membrane binding site, once this complex is bound to a membrane it becomes stable.
- Then the C8 and C9 complement bind to C5b-6-7 Complex and form C5b-6-7-8-9 complex, which is called MAC or membrane attack complex.
- This MAC creates a pore in the plasma membrane of the target cell, which leads to cosmetic lysis of the cell.
3. The Mannose-Binding Lectin Pathways
- The lectin pathway activates C3 convertase by using a Lectin.
- Lectin is a special protein that binds to specific carbohydrates.
- When macrophages ingest viruses, bacteria and other foreign material they release the cytokines.
- These cytokines stimulate liver cells to secrete mannose-binding protein (MBP), a lectin for mannose.
- Mannose binding proteins bind to many pathogens. Because Mannose is the major component of the bacterial cell walls and Virus envelopes.
- This lectin activates the complement pathway two ways;
A. After binding to the surface it can Trigger the alternative pathway directly. These Mannose binding protein-antigen (MBP-Ag) complexes cleaved the C3 complement into larger C3b and smaller C3a components. Now Complex MBP-Ag binds with the C3b and from a trimolar complex Mannose binding protein-antigen-C3b or MBP-Ag-C3b.
B. In addition, if MBP is bound to the MBP-associated serine esterase and forms a complex called MBP-MASP. Then, It will activate the classical complement pathway. The MBP- MASP Complex claved the C2 and C4 complement.
After the activation of the classical pathway it leads to the formation of MAC, which then lysis the bacterial cell wall.
*Remember all these three pathways lead to the same result, formation of MAC protein.
Functions or Immune Effects of the Complement Pathway
Once the complement pathway is activated, then it leads to these following activities;
- Immune Adherence: C3b and c4b promote phagocytosis by adherence of the antigen on the surface of the phagocytic cell.
- Chemotactic Action: C5a as well as C5b-6-7 Complex causes chemotaxis of neutrophil leukocytes towards the antigen. As a result it causes infiltration and aggregation of neutrophils in the affected tissue.
- Respiratory Burst in Leukocytes: C5a stimulates oxidative metabolism in leukocytes to produce the respiratory breast.
- Anaphylactic and inflammatory effects: Small components such as C3a, C2a and C5b which were released from the complement pathway act as anaphylatoxins. These small components act on mast cells and basophils to Trigger the release of anaphylactic and inflammatory chemicals which produce anaphylaxis and inflammation to help body immunity.
- Membrane Lesion and Complements: The membrane attack complex (MAC) can cause lysis of bacterial cells enclosed by lipoprotein envelope, viruses, platelets and many animal cells such as lymphocytes and erythrocytes.
- Opsonization: C3b binds to the immune complex or coated on the surface of pathogens, and activates phagocytic cells. These proteins bind to specific receptors on the phagocytic cells to get engulfed.
Deficiencies of the Complement Pathway
The deficiencies of complements can cause recurrent mild or serious bacterial infections, autoimmune disease, or episodes of angioedema (a painless, but often dramatic, swelling under the skin, or swelling in the intestines, which can be extremely painful).
A list of potential complement-related problems include renal disease, vasculitis (blood vessel inflammation) and age-related macular degeneration.
The treatment of the disease obtained from the Complement Deficiencies is at an early stage at the moment but more treatments should be obtained in the near future.
1. Deficiencies in the Classical Pathway Components
- The Deficiencies of C1q, C1r, C1s or C4 in classical pathways can lead to the development of systemic lupus erythematosus (SLE) or rheumatoid arthritis (RA).
- The C2 deficiency is found in SLE patients as compared to healthy controls. It is also found in young children with recurrent infections, primarily upper respiratory infections with Streptococcus pneumoniae or similar organisms.
- The CP control protein, C1-Inh deficiency can cause Hereditary angioedema (HAE) disease.
2. Deficiencies of the Lectin Pathway Components
- It was determined that deficiencies of MBL are very common, found in approximately 5-30% of all individuals.Therefore, its absence alone cannot be a cause of serious immunodeficiency. It is important to stress that the finding of low or absent MBL does not indicate that the cause for an individual’s infections has been found and that the diagnostic process must continue until the correct diagnosis is determined.
3. Deficiencies of the Alternative Pathway
- The deficiency of Factor D is very rare in alternative pathways, but it can cause serious infections.
- There is only one unconfirmed report of this Factor B deficiency.
- Properdin deficiency can increase the risk of bacterial infection of the Neisseria family of organisms.
- The deficiency of factor H can cause the uncontrolled activation of the AP and depletion of C3 occurs.
Reference
- Joanne Willey , Linda Sherwood , Christopher J. Woolverton, Prescott’s Microbiology
- https://teachmephysiology.com/immune-system/innate-immune-system/complement-system/
- https://www.britannica.com/science/complement-immune-system-component
- https://en.wikipedia.org/wiki/Complement_system
- https://primaryimmune.org/about-primary-immunodeficiencies/specific-disease-types/complement-deficiencies
nice information