What is Submandibular Gland?
- The submandibular gland, a pivotal component of the salivary system, stands as the second-largest salivary gland. Positioned beneath the floor of the mouth, it plays a crucial role in the production of saliva, contributing to approximately 65% of the unstimulated salivary secretion. This gland, in its anatomical context, is bilaterally located within the submandibular triangle, with each gland weighing around 15 grams in adult humans.
- In terms of its structural intricacies, the submandibular gland is bifurcated into superficial and deep lobes, separated by the mylohyoid muscle. The primary excretory duct of this gland, known as the Wharton duct, culminates in the oral cavity at the sublingual caruncle. This particular caruncle is a papilla situated medial to the sublingual gland and lateral to the frenulum linguae.
- Functionally, the submandibular gland is responsible for producing nearly 70% of saliva in an unstimulated state. However, upon stimulation, the dominance in saliva production shifts to the parotid gland. The gland’s secretions, a blend of serous and mucous salivary components, are indispensable for food lubrication during mastication. This not only facilitates effective swallowing but also aids in the digestion process.
- The gland’s functionality is further regulated by parasympathetic input it receives via the chorda tympani nerve. Historically referred to as the submaxillary glands, these paired glands have dimensions with an average length of 27 mm and a width of approximately 14.3 mm in adult humans.
- In conclusion, the submandibular gland, with its anatomical positioning and functional significance, remains vital for various oral and digestive processes. Its role in saliva production, both in stimulated and unstimulated states, underscores its importance in the human physiological system.

Definition of Submandibular Gland
The submandibular gland is one of the major salivary glands located beneath the floor of the mouth, responsible for producing a significant portion of saliva that aids in lubrication and digestion.
Anatomical Position of Submandibular Gland

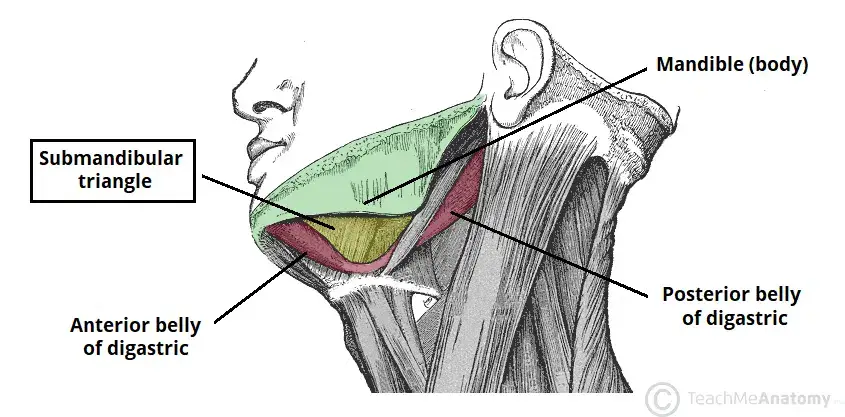
Situated within the anterior region of the submandibular triangle, the submandibular gland occupies a distinct anatomical position. The confines of this triangle are delineated as follows:
- Superior Boundary: The inferior aspect of the mandibular body.
- Anterior Boundary: The anterior segment of the digastric muscle.
- Posterior Boundary: The posterior segment of the digastric muscle.
This strategic positioning of the submandibular gland underscores its significance in the oral and digestive systems, facilitating its primary function of salivary secretion.
Structure of Submandibular Gland – Anatomical Structure
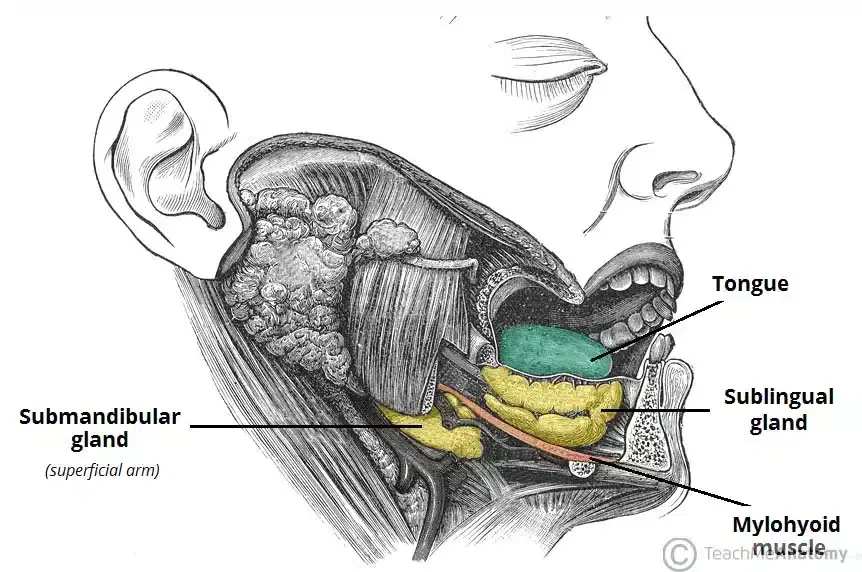
The submandibular gland, a pivotal component of the salivary system, boasts a unique and intricate anatomical structure. Comprising a pair of elongated, flattened hooks, the gland is bifurcated into two distinct arms: superficial and deep. These arms are strategically positioned in relation to the mylohyoid muscle, which the gland encircles.
- Superficial Arm: This constitutes the larger segment of the gland. It is partially situated inferior to the posterior half of the mandible, specifically within the submandibular fossa’s impression on its medial aspect. Notably, this arm remains outside the confines of the oral cavity.
- Deep Arm: This segment of the gland hooks around the posterior margin of the mylohyoid muscle, entering the oral cavity through a triangular aperture. It is positioned on the hyoglossus’s lateral surface, adjacent to the tongue’s root.
The gland’s secretions are channeled into the oral cavity via the submandibular duct, commonly referred to as Wharton’s duct. This duct, measuring approximately 5cm in length, originates anteromedially from the gland’s deep arm, navigating between the mylohyoid, hypoglossus, and genioglossus muscles. As it ascends, the duct culminates in 1-3 orifices on a sublingual papilla, known as the caruncle, situated at the lingual frenulum’s base.
Further delineating its structure:
- Superficial Lobe: This lobe encompasses the majority of the gland, with the mylohyoid muscle running beneath it.
- Deep Lobe: This is the more compact segment of the gland.
- Submandibular Duct: The secretions from the gland are first directed into this duct located in the deep lobe. They then circumvent the mylohyoid muscle’s posterior edge, advancing on its superior surface laterally. The lingual nerve intersects these excretory ducts, which eventually drain into the sublingual caruncles, alongside the major sublingual duct.
- Submandibular Gland Papilla: The terminal segment of the submandibular (Wharton’s) duct is found in the mouth’s floor, opening as the submandibular duct papilla’s orifice. The duct’s position and its ostium, ranging between 0.5–1.5 mm in width, are symmetric yet can vary, making the papillae occasionally difficult to identify. Based on their macroscopic appearance and a sialoendoscopic approach, four distinct types of submandibular gland papillae have been described: types A, B, C, and D.
In essence, the submandibular gland’s anatomical structure, with its distinct lobes and duct system, plays a pivotal role in salivary secretion, underscoring its significance in the human physiological system.
Microanatomy
The submandibular gland, an integral component of the salivary system, presents a complex microanatomy that facilitates its primary function of saliva secretion. Delving into its microscopic structure:
- Adenomeres and Acini: The larger lobes of the gland encompass smaller lobules, which in turn house adenomeres. These adenomeres are the fundamental secretory units of the gland. Each adenomere comprises one or more acini, which are minuscule cell clusters responsible for secreting their products into a designated duct. The cellular composition of these acini can be either serous or mucous, with the former being more predominant. Notably, certain mucous adenomeres are capped with serous demilunes, which are lysozyme-secreting serous cells arranged in a half-moon configuration.
- Classification: The submandibular gland’s microscopic anatomy and the arrangement of its secretory cells classify it as a branched tubuloacinar gland. Given the presence of both serous and mucous secretory cells, it is deemed a mixed gland. While the majority of the cells are serous in nature, the primary exudate is predominantly mucous. This gland is characterized by elongated striated ducts and shorter intercalated ducts.
- Functionality of Secretory Acinar Cells: The acinar cells within the submandibular gland exhibit specialized functions. The mucous cells, being the most active, predominantly produce saliva with a mucoid consistency. These cells secrete mucin, a component crucial for lubricating the food bolus, facilitating its passage through the esophagus. Concurrently, the serous cells synthesize salivary amylase, an enzyme instrumental in starch breakdown within the oral cavity. The submandibular gland’s acini, due to their heightened activity, contribute significantly to the overall salivary volume, with the parotid and sublingual glands accounting for the residual volume.
In essence, the submandibular gland’s microanatomy, with its intricate arrangement of adenomeres, acini, and specialized secretory cells, underscores its pivotal role in salivary secretion and oral digestion processes.
Relationship with Nerves
The submandibular gland, a key component of the salivary system, maintains a close anatomical association with three primary nerves: the lingual nerve, the hypoglossal nerve, and the marginal mandibular branch of the facial nerve. Understanding the intricate courses of these nerves provides insights into their functional interplay with the gland:
- Lingual Nerve: Originating laterally to the submandibular duct, the lingual nerve embarks on an anteromedial trajectory. It loops beneath the duct, culminating in multiple medial branches. These terminal branches ascend along the external and superior facets of the hypoglossus muscle. Functionally, they offer general somatic afferent innervation to the mucous membrane, covering the anterior two-thirds of the tongue.
- Hypoglossal Nerve: Positioned deep to the submandibular gland, the hypoglossal nerve courses superficially over the hyoglossus muscle while remaining deep to the digastric muscle. This nerve plays a pivotal role in tongue movement and function.
- Facial Nerve (Marginal Mandibular Branch): This nerve emerges from the anterior-inferior segment of the parotid gland near the jaw’s angle. It follows a path along the mandible’s margin, situated between the platysma muscle and the investing layer of the deep cervical fascia. As it progresses, it curves downward, passing inferiorly to the submandibular gland.
In essence, the submandibular gland’s intricate relationship with these principal nerves underscores the importance of understanding their anatomical interplay, especially in clinical contexts involving surgical interventions or diagnostic evaluations.
Blood supply, Lymphatic drainage and Nerve supply
Blood Supply: The submandibular gland derives its vascular supply primarily from the facial and lingual arteries. Specifically, the sublingual and submental arteries cater to the gland’s blood requirements. Venous drainage from the gland is facilitated by the common facial and lingual veins, ensuring efficient blood circulation within the glandular structure.
Lymphatic Drainage: Lymphatic vessels play a pivotal role in the gland’s immune defense and fluid balance. The lymphatics originating from the submandibular gland initially channel into the submandibular lymph nodes. Subsequent drainage is directed towards the jugulo-digastric lymph nodes, ensuring the efficient removal of waste products and immune surveillance.
Nerve Supply: The submandibular gland’s neural regulation is intricate, involving both the parasympathetic and sympathetic divisions of the autonomic nervous system.
- Parasympathetic Innervation: The superior salivatory nucleus provides the gland’s parasympathetic innervation. This is channeled via the chorda tympani, an offshoot of the facial nerve. Before reaching the gland, this nerve integrates with the lingual nerve, a branch of the trigeminal nerve, and subsequently synapses on the submandibular ganglion. Enhanced parasympathetic activity augments saliva secretion, vital for oral digestion and lubrication.
- Sympathetic Innervation: The sympathetic nervous system modulates the gland’s secretions by inducing vasoconstriction in the arteries supplying the gland. Elevated sympathetic activity diminishes the gland’s blood flow, leading to a reduction in the fluid volume of salivary secretions. This results in the secretion of mucous saliva enriched with enzymes. However, direct sympathetic nerve stimulation amplifies salivary enzymatic secretions. Collectively, while the volume of secretions is reduced, their enzymatic content is augmented by the combined effects of parasympathetic and sympathetic innervation.
Anatomical Relations: Positioned within the submandibular triangle, the gland is located posteroinferiorly to the mandible’s ramus and is nestled between the two muscular bellies of the digastric muscle.
Development: The submandibular gland’s embryological development commences later than the parotid glands, initiating towards the end of the sixth prenatal week. Originating bilaterally from epithelial buds in the sulcus surrounding the sublingual folds, these buds give rise to solid cords that branch and grow laterally to the developing tongue. These cords undergo further branching and canalization to form the ductal system. By the 12th week, the gland’s acini develop, with secretory activity commencing by the 16th week. Postnatal growth sees the formation of additional acini. The submandibular duct’s genesis is marked by the development of a linear groove lateral to the tongue, which eventually encloses to form the duct.
In summary, the submandibular gland’s intricate vascular, lymphatic, and neural networks underscore its significance in oral health and function.
Innervation
The submandibular gland, a pivotal salivary gland, is intricately regulated by both parasympathetic and sympathetic branches of the autonomic nervous system. These neural pathways play a crucial role in modulating the gland’s secretory functions.
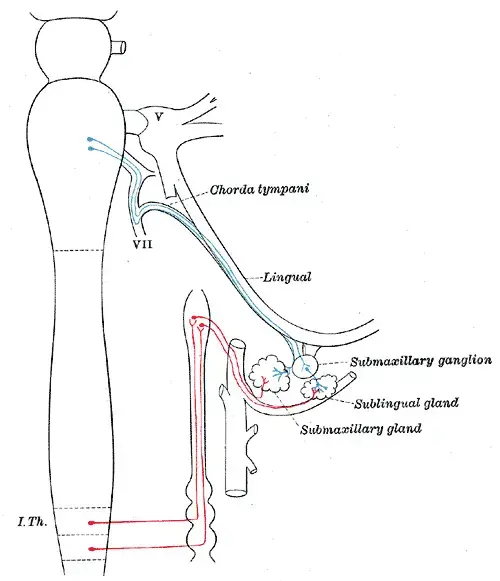
- Parasympathetic Innervation:
- The parasympathetic regulation of the submandibular gland is initiated at the superior salivatory nucleus. Pre-synaptic fibers from this nucleus traverse through the chorda tympani, a specialized branch of the facial nerve (CNVII). This nerve subsequently merges with the lingual branch of the mandibular nerve (CNViii). The synapse occurs at the submandibular ganglion, which is anchored by two delicate nerve filaments.
- The post-ganglionic fibers emerging from this synapse serve dual functions. Firstly, the secretomotor fibers directly stimulate the gland, prompting it to release its secretions. Secondly, vasodilator fibers accompany the arterial network, enhancing the blood supply to the gland. Consequently, heightened parasympathetic activity amplifies salivary secretion, ensuring optimal oral hydration and enzymatic activity.
- Sympathetic Innervation:
- The sympathetic regulation of the submandibular gland has its genesis at the superior cervical ganglion. From here, post-synaptic fibers, possessing vasoconstrictive properties, embark on a journey along a network of arteries. They form a plexus around the internal and external carotid arteries, proceed to the facial artery, and ultimately reach the submental arteries, granting them access to the gland.
- The primary role of sympathetic innervation is to modulate the gland’s blood flow. An upsurge in sympathetic activity induces vasoconstriction, curtailing the blood supply to the gland. This results in a reduction in the volume of salivary secretions. However, the saliva produced under such conditions is characterized by a higher mucous and enzymatic content, optimizing its lubricative and digestive properties.
In essence, the dual autonomic innervation of the submandibular gland ensures a dynamic balance between volume and composition of saliva, catering to the ever-changing physiological needs of the oral cavity.
Clinical Significance
The submandibular gland, an integral component of the salivary gland system, can be implicated in various clinical conditions, each bearing its unique pathophysiology and clinical presentation.
- Neoplasia: Tumors can arise in the submandibular gland, albeit they constitute a minor fraction (less than 2%) of all head and neck neoplasms. Notably, around half of these tumors are malignant in nature. The predominant malignancies identified are adenoid cystic and mucoepidermoid carcinomas. Furthermore, metastasis from primary head and neck cancers can target major salivary glands. The clinical presentation is often subtle, manifesting as an unremarkable swelling in the mouth’s floor or beneath the mandible, thereby complicating the diagnostic process. Comprehensive evaluation, encompassing imaging and biopsy, is pivotal. Treatment modalities range from surgical excision for benign entities to more aggressive interventions like neck dissection and radiation therapy for advanced or aggressive tumors.
- Sialolithiasis: This condition is characterized by the formation of salivary stones that obstruct the gland’s excretory duct. The genesis of these stones is intricately linked to salivary stasis and ductal inflammation. Clinically, these stones can induce glandular swelling and pain, especially during meals. The majority of these stones (80%-90%) are localized in the Wharton duct, originating from the submandibular gland. This predilection is attributed to the duct’s anatomical features and the gland’s secretion consistency.
- Sialadenitis: Inflammation of the salivary gland, termed sialadenitis, can be triggered by infections or obstructions. Bacterial agents, predominantly Staphylococci, or viruses like mumps are common culprits. In the context of the submandibular gland, the presence of salivary stones often underlies the inflammation. Clinical manifestations include fever, pain, and glandular swelling. Treatment is tailored to the etiology, with antibiotics being the mainstay for bacterial infections. In severe cases, especially when abscesses form, surgical intervention might be warranted.
- Sialadenosis: This benign condition is marked by a non-inflammatory enlargement of the submandibular glands. It is frequently observed in individuals with conditions linked to malnutrition, such as bulimia, diabetes, or advanced liver diseases. The underlying pathogenesis is believed to revolve around autonomic neuropathy, leading to the accumulation of secretory granules in the gland’s acinar cells, thereby disrupting its autonomic innervation.
In summary, the submandibular gland’s clinical significance is vast, with its involvement in a spectrum of conditions ranging from benign to malignant. A thorough understanding of its pathophysiology and clinical presentation is essential for timely diagnosis and effective management.
Tests of Submandibular Gland
The submandibular gland, a crucial component of the salivary system, may be affected by various conditions. To ascertain the nature and extent of these conditions, healthcare professionals employ a range of diagnostic tests and procedures.
- Sialolithiasis: For suspected cases of sialolithiasis, dental X-rays can often reveal the presence of salivary stones. Physical palpation of the affected area may be conducted if pain or swelling is reported. Advanced imaging techniques, such as computed tomography (CT) scans or ultrasounds, may be requisitioned to differentiate from other potential conditions. Therapeutically, initial interventions might include hydration, heat application, and massage. In cases where these conservative measures are ineffective, surgical removal of the stones via sialendoscopy might be necessitated.
- Sialadenitis: The diagnostic approach for sialadenitis typically commences with a physical examination. Further insights might be garnered through CT scans and ultrasounds. Treatment often involves antibiotics, with surgical drainage being a consideration for non-responsive infections. Concurrently, any contributing salivary stones might also be surgically excised.
- Sjögren’s Syndrome: For suspected Sjögren’s syndrome, blood tests are conducted to detect specific antibodies. Additional diagnostic measures might encompass eye examinations, glandular biopsies, and imaging techniques like sialometry and salivary scintigraphy. While there’s no definitive cure, management revolves around symptom alleviation.
- Xerostomia: In cases of xerostomia or dry mouth, a comprehensive physical examination is undertaken, followed by tests to exclude potential diseases or infections. Treatment primarily focuses on addressing the root cause, supplemented by symptom management strategies such as chewing gum and saliva substitutes.
- Salivary Gland Cancer: The diagnostic journey for salivary gland cancer starts with a meticulous physical examination of the mouth and facial region. If anomalies are detected, specialist consultations, possibly with an otolaryngologist, are recommended. A gamut of imaging techniques, including X-rays, CT scans, MRI, and PET scans, may be employed to scrutinize the glands for tumors. If tumors are identified, biopsies are conducted to ascertain their nature. Fine needle aspiration (FNA) biopsy involves extracting cells from the tumor for lab analysis. In instances where FNA yields insufficient cells, an incisional biopsy might be performed, wherein a portion of the tumor is excised for lab evaluation. If malignancy is confirmed, surgical removal of the tumor is typically advised, potentially supplemented by radiation or chemotherapy, especially if the cancer has metastasized.
In essence, the submandibular gland’s diagnostic procedures are multifaceted, tailored to the specific condition suspected, ensuring accurate diagnosis and optimal patient care.
Functions of Submandibular Gland
The submandibular gland is one of the major salivary glands in the human body, and it plays a vital role in the maintenance of oral health and the digestive process. Here are the primary functions of the submandibular gland:
- Saliva Production: The primary function of the submandibular gland is the production and secretion of saliva. This gland contributes to approximately 60-65% of the total salivary volume in the oral cavity.
- Digestion: The saliva produced by the submandibular gland contains digestive enzymes, most notably alpha-amylase. This enzyme initiates the breakdown of dietary starches into simpler sugars, beginning the digestive process even before food reaches the stomach.
- Lubrication: Saliva acts as a lubricant, facilitating the processes of chewing, swallowing, and speaking. It ensures that the oral mucosa and the food bolus remain moist, aiding in the smooth passage of food down the esophagus.
- Oral Health Maintenance: Saliva plays a crucial role in maintaining oral health. It helps neutralize acids produced by bacteria in the mouth, thereby preventing tooth decay. Additionally, the antimicrobial components in saliva help reduce the bacterial load in the oral cavity, preventing infections.
- Taste: Saliva aids in the dissolution of food particles, allowing them to come into contact with taste receptors on the tongue. Without saliva, the perception of taste would be hindered.
- Buffering Action: Saliva from the submandibular gland has a buffering capacity, helping to maintain the pH of the oral environment. This is essential in preventing demineralization of tooth enamel and promoting remineralization.
- Wound Healing: Saliva contains various growth factors and proteins that promote tissue repair and wound healing in the oral cavity.
- Protection: The mucous component of the saliva produced by the submandibular gland helps form a protective barrier on the oral mucosa, shielding it from potential irritants in food and drink.
In summary, the submandibular gland plays a multifaceted role in ensuring the proper functioning of the oral cavity and the initial stages of digestion. Its secretions are integral to maintaining oral health, aiding digestion, and ensuring the overall well-being of the oral environment.
Quiz
Which of the following is the primary function of the submandibular gland?
a) Production of hormones
b) Production and secretion of saliva
c) Production of mucus for the nasal cavity
d) Regulation of blood pH
[expand title=”Show answer” swaptitle=”Hide answer”] b) Production and secretion of saliva [/expand]
Approximately what percentage of the total salivary volume in the oral cavity is contributed by the submandibular gland?
a) 20-25%
b) 40-45%
c) 60-65%
d) 80-85%
[expand title=”Show answer” swaptitle=”Hide answer”] c) 60-65% [/expand]
Which enzyme, found in the saliva produced by the submandibular gland, initiates the breakdown of dietary starches?
a) Lipase
b) Protease
c) Alpha-amylase
d) Lactase
[expand title=”Show answer” swaptitle=”Hide answer”] c) Alpha-amylase [/expand]
Which of the following nerves is NOT closely associated with the submandibular gland?
a) Lingual nerve
b) Hypoglossal nerve
c) Facial nerve
d) Vagus nerve
[expand title=”Show answer” swaptitle=”Hide answer”] d) Vagus nerve [/expand]
Saliva from the submandibular gland plays a role in:
a) Neutralizing acids in the mouth
b) Increasing the bacterial load in the oral cavity
c) Promoting tooth decay
d) Drying out the oral mucosa
[expand title=”Show answer” swaptitle=”Hide answer”] a) Neutralizing acids in the mouth [/expand]
The submandibular gland is located in which anatomical region?
a) Parotid region
b) Sublingual region
c) Submandibular triangle
d) Buccal cavity
[expand title=”Show answer” swaptitle=”Hide answer”] c) Submandibular triangle [/expand]
Which component in saliva aids in the dissolution of food particles for taste perception?
a) Mucous
b) Enzymes
c) Growth factors
d) Antimicrobial agents
[expand title=”Show answer” swaptitle=”Hide answer”] a) Mucous [/expand]
Which of the following conditions is characterized by inflammation of the salivary gland due to infection or obstruction?
a) Sialolithiasis
b) Sialadenitis
c) Sjögren’s Syndrome
d) Xerostomia
[expand title=”Show answer” swaptitle=”Hide answer”] b) Sialadenitis [/expand]
The majority of salivary stones found in the Wharton duct originate from which gland?
a) Parotid gland
b) Sublingual gland
c) Submandibular gland
d) Buccal gland
[expand title=”Show answer” swaptitle=”Hide answer”] c) Submandibular gland [/expand]
Which of the following is NOT a treatment approach for Sjögren’s syndrome related to the submandibular gland?
a) Artificial saliva producers
b) Eye drops for dry eyes
c) Surgical removal of the gland
d) Specific dental care to prevent decay
[expand title=”Show answer” swaptitle=”Hide answer”] c) Surgical removal of the gland [/expand]
FAQ
What is the submandibular gland?
The submandibular gland is one of the major salivary glands responsible for producing and secreting saliva into the oral cavity. It is located beneath the lower jaw, in the submandibular triangle.
What is the primary function of the submandibular gland?
The primary function of the submandibular gland is to produce and secrete saliva, which aids in digestion, lubrication, and protection of the oral cavity.
How does the submandibular gland differ from other salivary glands?
The submandibular gland contributes to approximately 60-65% of the total salivary volume in the oral cavity, making it the second-largest salivary gland after the parotid gland.
What conditions can affect the submandibular gland?
Conditions such as sialolithiasis (salivary stones), sialadenitis (inflammation of the gland), and neoplasia (tumors) can affect the submandibular gland.
How is sialolithiasis treated in the submandibular gland?
Sialolithiasis, or salivary stones, can sometimes be managed with at-home treatments like hydration and massage. In cases where the stone doesn’t pass, surgical intervention may be necessary.
What are the symptoms of a submandibular gland infection?
Symptoms can include pain, swelling in the neck or under the jaw, fever, and a foul taste in the mouth.
How is the submandibular gland innervated?
The gland receives both parasympathetic and sympathetic innervation, which regulate its secretory functions.
Can the submandibular gland be removed?
Yes, in certain conditions where the gland is severely affected, such as recurrent infections or tumors, surgical removal (submandibulectomy) might be recommended.
How does the submandibular gland aid in digestion?
The saliva produced by the submandibular gland contains enzymes like alpha-amylase that initiate the breakdown of dietary starches, aiding in the digestive process.
What role does the submandibular gland play in oral health?
The saliva produced by the submandibular gland helps in neutralizing acids in the mouth, preventing tooth decay, and providing lubrication, which aids in speech and swallowing.
References
- Grewal JS, Jamal Z, Ryan J. Anatomy, Head and Neck, Submandibular Gland. [Updated 2022 Dec 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542272/
- Biology Dictionary. (Year). Title of the webpage. Retrieved from https://biologydictionary.net/submandibular-gland/
- Teach Me Anatomy. (Year). Title of the webpage. Retrieved from https://teachmeanatomy.info/head/organs/salivary-glands/submandibular/
- Wikipedia contributors. (Year). Submandibular gland. In Wikipedia, The Free Encyclopedia. Retrieved from https://en.wikipedia.org/wiki/Submandibular_gland
- Verywell Health. (Year). Title of the webpage. Retrieved from https://www.verywellhealth.com/submandibular-gland-5101463
- Kenhub. (Year). The submandibular gland. Retrieved from https://www.kenhub.com/en/library/anatomy/the-submandibular-gland